Abstract
Objective
Breast cancer is the most common cancer among women worldwide. The Nordic countries have relatively high survival, but Denmark has a lower survival than neighboring countries. A breast cancer screening program was introduced in 2007 and 2008 in the northern and central regions of Denmark respectively. We aimed to examine possible changes in survival of Danish breast cancer patients in central and northern Denmark in the period 1998–2009.
Materials and methods
From the northern and central Denmark regions, we included all women (n = 13,756) with an incident diagnosis of breast cancer, as recorded in the Danish National Registry of Patients during the period January 1, 1998 through December 31, 2009. We calculated age-stratified survival and used Cox proportional hazard regression to estimate mortality rate ratios (MRRs) for all breast cancer patients.
Results
Median age was 62 years (21–102 years). The overall 1-year survival improved steadily over the period from 90.9% in 1998–2000 to 94.4% in 2007–2009, corresponding to a 1-year age adjusted MRR of 0.68 in 2007–2009 compared with the reference period 1998–2000. We estimated the 5-year survival to improve from 70.0% in 1998–2000 to 74.7% in 2007–2009, corresponding to a 5-year age adjusted MRR of 0.82 in 2007–2009 compared with the reference period 1998–2000. For middle-aged women (50–74 years) 1-year survival increased from 92.8% in 1998–2000 to 96.6% in 2008–2009, and 5-year survival was expected to increase from 73.9% in 1998–2000 to 80.2% in 2007–2009. Among younger women (15–49 years) and elderly women (>75 years), 1-year survival and 5-year predicted survival did not change over the two time periods.
Conclusion
Survival of breast cancer patients has improved in Denmark over the period 1998–2009, and this change was most distinct in women aged 50–74 years. Survival improved even before the implementation of a formal breast cancer screening program.
Introduction
Breast cancer accounts for a substantial proportion of the cancer burden in women, with an estimated 1.4 million new cases per year and more than 450,000 breast cancer-related deaths per year worldwide.Citation1 In Denmark, breast cancer accounted for 29% of all incident cancers and 16% of all cancer deaths among women in the period 1999–2003.Citation1
Despite increasing survival in the Nordic countries, Denmark still has a deficit compared with the other Nordic countries. In 2005–2007, Denmark had a 3.0% lower 1-year and 6.1% lower 5-year survival than Sweden.Citation2–Citation4 Prompted by the general lower cancer survival in Denmark compared with neighboring countries, National Cancer PlansCitation5 were introduced in 2002 and 2005, respectively, aiming to improve survival of cancer patients.Citation6
Breast cancer treatment in Denmark is standardized in programs formed by the Danish Breast Cancer Cooperative Group (DBCG). These programs have changed over the last decade towards a more widespread use of sentinel node technique and breast conserving surgery with adjuvant radiotherapy,Citation7 prolonged use of tamoxifen, and introduction of aromatase inhibitors.Citation8 Use of chemotherapy has improved with anthracyclines and/or taxanes, and most recently, in 2006, anti-HER2-therapy with trastuzumab according to the biomarker profile has been added to the programs.Citation8,Citation9 The beneficial effect of these treatments on survival has been documented in randomized controlled trials,Citation10,Citation11 and data from the DBCG database have, during the period 1977–2006, shown an increase in 5-year survival in Danish breast cancer patients from 65% to 81%.Citation12
A breast cancer mammographic screening program was introduced in 2007 and 2008 in the northern and central regions of Denmark, respectively and may influence survival. Numerous investigations have proven a 25%–30% increased survival after introduction of screening programs in other countries.Citation13–Citation15
We used population-based registries in northern and central Denmark to examine changes in the mortality and survival of breast cancer patients of all ages between 1998 and 2009.
Material and methods
We conducted this study in the central and the northern Denmark regions, with a total population of 1.8 million persons. The National Health Service provides tax-supported health care for all inhabitants of Denmark, guaranteeing free treatment in hospitals. Virtually no breast cancer patients were treated in private hospitals during the study period.Citation16
Identification of breast cancer patients
Through the Danish National Registry of Patients (DNRP), we identified all women resident in the northern or central regions of Denmark who had their first breast cancer diagnosis recorded in a hospital within one of the two regions over the period January 1, 1998 through December 31, 2009. The DNRP contains information about all admissions from nonpsychiatric hospitals in Denmark since 1977 and outpatient data from 1995.Citation17 This registry includes information on civil registration number, dates of admission and discharge, surgical procedure(s) performed, and up to 20 diagnoses from each hospital contact. Since 1994, diagnoses have been classified according to the International Classification of Diseases 10th edition (ICD-10). The ICD codes used to identify breast cancer were ICD-10 C50.x.
Survival
Since 1968, the Central Office of Civil Registration has assigned a unique 10-digit personal identification number to all Danish citizens.Citation18 This number, unique to each Danish resident, is used in all Danish registries, allowing unambiguous individual-level data linkage. From the Civil Registration System we also obtained information on vital status (dead or alive), date of death, and residence for all cancer patients.
Statistical analysis
We followed each patient from date of cancer diagnosis until emigration, death, or June 25, 2010, whichever came first. To visualize crude survival we constructed Kaplan– Meier curves, stratified according to period of diagnosis (1998–2000, 2001–2003, 2004–2006, and 2007–2009). We estimated 1-, 3-, and 5-year survival. In the latter periods we estimated 3- and 5-year survival using a hybrid analysis in which we included the actual survival for as long as possible and then estimated the conditional probability of surviving thereafter based on the corresponding survival experience of patients in the previous period (ie, using a period analysis technique).Citation19 To compare all-cause mortality over time, we used Cox proportional hazard regression analysis, with 1998–2000 as the reference period to estimate 1-, 3-, and 5-year mortality rate ratios (MRRs) and corresponding 95% confidence intervals (CIs), adjusting for age group (15–49 years, 50–74 years, and >75 years).
Analyses were performed using SAS (v 9.2; SAS Institute, Inc, Cary, NC).
Results
A total of 13,756 women had incident breast cancer during the period 1998–2009, with a median age of 62 years (range 21–102 years). The descriptive data are presented in and .
Figure 1 Survival curves for women with breast cancer, according to year of diagnosis, northern Denmark, 1998–2009.
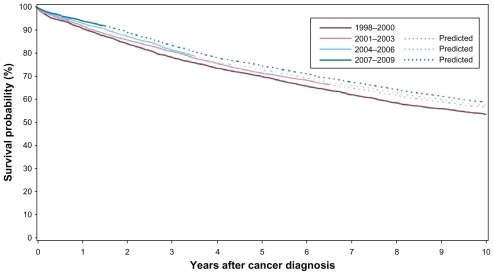
Table 1 Cumulative survival and crude and adjusted MRRs, and associated 95% confidence intervals, for breast cancer patients diagnosed in northern Denmark, 1998–2009
The annual number of women with incident breast cancer nearly doubled in the end of our study period, from a total of 962 in 1998 to 1758 in 2009. In 1998–2006, around 58% of newly diagnosed breast cancer patients were in the age group 50–74 years. However, in 2007–2009, women aged 50–74 years constituted 70.1% of all newly diagnosed breast cancer patients (see ).
Table 2 Survival and associated 95% confidence intervals in women with breast cancer, according to age and year of diagnosis for breast cancer patients diagnosed in northern Denmark, 1998–2009
The 1-year overall survival improved gradually from 90.9% in 1998–2000 to 94.4% in 2007–2009 ( and ), corresponding to an unadjusted 1-year MRR of 0.61 (95% CI: 0.51–0.73) in 2007–2009 compared with 1998–2000. After adjustment for age, the MRR was 0.68 (95% CI: 0.56–0.79). The 5-year survival was 70.0% in 1998–2000 and was predicted to be 74.7% in 2007–2009. This yielded an adjusted 5-year MRR of 0.79 (95% CI: 0.72–0.87) ( and ).
Among women aged 50–74 years, the 1-year survival increased from 92.8% in 1998–2000 to 96.6% in 2007–2009, and the 5-year predicted survival increased from 73.9% in 1998–2000 to 80.2% in 2007–2009 (). In women aged 15–49 years and more than 75 years both 1- and 5-year survival remained virtually unchanged during the study period; in the youngest women, the 1-year survivals were 97.0%–97.9%, and 5-year survival/predicted survivals were 86.6%–87.6%. In the elderly, the 1-year survival was 81.3%–81.1%, and 5-year survival was 46.5%–45.9% ().
Discussion
In this population-based cohort study including nearly 14,000 breast cancer patients diagnosed between 1998 and 2009, we found that survival after breast cancer diagnosis gradually increased over the entire period. The 1-year mortality decreased more than 30%, and the 5-year mortality was predicted to decrease by 20%. In the end of our study period, however, the annual number of women diagnosed with breast cancer nearly doubled.
The main strength of our study is the population-based design with a well defined catchment area and virtually complete follow-up, which minimizes the potential for selection bias. The use of data from the DNRP allowed for analyses updated to recent calendar years; however, the codes from the DNRP may not be entirely accurate. A previous Danish study conducted in northern Denmark compared ovarian cancer diagnoses recorded in the DNRP with similar data from the Danish Cancer Registry. The completeness of ovarian cancer diagnoses in the DNRP was 96%, and the positive predictive value was 87%.Citation20 Thus, we cannot rule out some misclassification of our patients, and if the positive predictive value increased over the study period this may have influenced our estimates. However, we find it likely that women without a breast cancer diagnosis have a better survival than women with a breast cancer diagnosis. Therefore, we do expect improved predictive values to result in decreased survival. Our study has other limitations worth addressing. We do not have information on cancer stage, tumor size, hormone receptor status, choice of medical treatment, comorbidity, or lifestyle; all of which have an impact on breast cancer outcome.Citation12,Citation21 Mortality trends among younger women with breast cancer could likely almost entirely be driven by breast cancer and its treatment, while mortality among older women is probably influenced by comorbidity. The improved survival among 50–74-year-old women in our study could thus to some extent be explained by improved survival in this age category in the general population. We are, however, unable to address the impact of these factors on the change we observed in breast cancer survival.
The weakness of the hybrid analysis design is that it may not be as accurate as directly observed survival. However, since we based our predictions on the survival experience in the previous period of our study, we expect our predictions to be conservative estimates of the increased survival among women with breast cancer.
Our finding of an improved breast cancer survival in central and northern Denmark extends the findings by Coleman et alCitation3 based on data from the Danish Cancer Registry that relative 1- and 5-year survival improved during the period 1995–2007 and Mouridsen et alCitation12 who based their study on data from the DBCG and similarly found an increased survival during the period 1977–2006. Mouridsen et al report an overall 5-year survival of 81% in 2002–2006, which is higher than the 5-year survival of 73% we found in 2004–2006. The DBCG is not entirely complete, as the registration earlier on of patients, who were not operated, was very limited, and this may explain differences in survival.
Several factors may explain the increase in survival that we observed. One possibility is changes in diagnostic procedures leading to earlier diagnosis. Breast cancer screening was introduced in our regions and offered to all women aged 50–69 years biennially in 2007 and 2008Citation16 and may explain the nearly two-fold increase in the annual number of breast cancers in that period. If this increase in breast cancer incidence mainly occurred in tumors which were less aggressive than tumors detected outside screening programs, survival in the latest period may be affected by length time bias.Citation22 Since the aim of screening is to detect cancers at an earlier stage,Citation16 survival will also be prolonged even without change in time of death (lead time bias). However, we also observed improvement in survival before the screening program was implemented. Thus other factors must be involved.
The technical quality of diagnostic imaging with digital mammography, high resolution ultrasound, stereotactic biopsies, and adjunct MRI mammography has improved over the yearsCitation23–Citation26 so cancers could be detected at an earlier stage, even before the introduction of the screening program.
However, the treatment of breast cancer in Denmark during our study period has changed towards treatment by specialized breast surgeons working in multidisciplinary teams in centralized units with a higher volume of patients than just a few years ago.Citation27 This specialization might have contributed to the improved survival.Citation9 More widespread use of standardized treatment following the DBCG protocols may also have had an important impact on the improved survival.Citation12 These treatment changes include extended indications of adjuvant treatment with chemotherapy, endocrine treatment, biological treatment, and radiation therapy for smaller tumors, lower disease grades, and different age categories.Citation8
In conclusion, survival among breast cancer patients has improved in Denmark over the time period 1998–2009, and this change was most pronounced in women aged 50–74 years. Introduction of a screening program in the last part of our study period might have contributed to these findings, but improvement of survival was also observed in the first part of our study period before the screening program was implemented. This could thus reflect changes in adjuvant treatment.
Disclosure
The authors report no conflicts of interest in this work.
References
- FerlayJShinHRBrayFFormanDMathersCParkinDMfor GLOBOCAN 2008 Cancer Incidence and Mortality WorldwideIARC CancerBase No 10 [Internet]Lyon, FranceInternational Agency for Research on Cancer2010 Available at: http://globocan.iarc.fr/factsheets/cancers/breast.aspAccessed February 23, 2011
- TryggvadottirLGislumMBrayFTrends in the survival of patients diagnosed with breast cancer in the Nordic countries 1964–2003 followed up to the end of 2006Acta Oncol201049562463120429724
- ColemanMPFormanDBryantHCancer survival in Australia, Canada, Denmark, Norway, Sweden, and the UK, 1995–2007 (the International Cancer Benchmarking Partnership): an analysis of populationbased cancer registry dataLancet2011377976012713821183212
- StormHHKejsAMEngholmGTrends in the overall survival of cancer patients diagnosed 1964–2003 in the Nordic countries followed up to the end of 2006: the importance of case-mixActa Oncol201049571372420491527
- AndersenJSHansenSWThe cancer plan. Political will – professional formationUgesk Laeger20021642228852889 Danish
- StormHHGislumMEngholmGCancer survival before and after initiating the Danish Cancer Control planUgesk Laeger20081703930653069 Danish
- AhernTPLarssonHGarneJPCronin-FentonDPSorensenHTLashTLTrends in breast-conserving surgery in Denmark, 1982–2002Eur J Epidemiol200823210911417987392
- MøllerSJensenMBEjlertsenBThe clinical database and the treatment guidelines of the Danish Breast Cancer Cooperative Group (DBCG); its 30-years experience and future promiseActa Oncol200847450652418465317
- SkinnerKAHelsperJTDeapenDYeWSpostoRBreast cancer: do specialists make a difference?Ann Surg Oncol200310660661512839844
- Early Breast Cancer Trialists’ Collaborative Group (EBCTCG)Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trialsLancet200536594721687171715894097
- ClarkeMCollinsRDarbySEffects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trialsLancet200536695032087210616360786
- MouridsenHTBjerreKDChristiansenPJensenMBMøllerSImprovement of prognosis in breast cancer in Denmark 1977–2006, based on the nationwide reporting to the DBCG RegistryActa Oncol200847452553618465318
- OlsenAHNjorSHVejborgIBreast cancer mortality in Copenhagen after introduction of mammography screening: cohort studyBMJ2005330748522015649904
- HellquistBNDuffySWAbdsalehSEffectiveness of populationbased service screening with mammography for women ages 40 to 49 years: evaluation of the Swedish Mammography Screening in Young Women (SCRY) cohortCancer2011117471472220882563
- NystromLAnderssonIBjurstamNFrisellJNordenskjoldBRutqvistLELong-term effects of mammography screening: updated overview of the Swedish randomised trialsLancet2002359931090991911918907
- ChristiansenPMøllerSBjerreKDKvalitetsindikatorrapport for brystkræft, 20092010115
- AndersenTFMadsenMJorgensenJMellemkjoerLOlsenJHThe Danish National Hospital Register. A valuable source of data for modern health sciencesDan Med Bull199946326326810421985
- PedersenCBGotzscheHMollerJOMortensenPBThe Danish Civil Registration System. A cohort of eight million personsDan Med Bull200653444144917150149
- BrennerHRachetBHybrid analysis for up-to-date long-term survival rates in cancer registries with delayed recording of incident casesEur J Cancer200440162494250115519525
- TetscheMSNorgaardMSkriverMVAndersenESLashTLSorensenHTAccuracy of ovarian cancer ICD-10 diagnosis in a Danish population-based hospital discharge registryEur J Gynaecol Oncol200526326627015991523
- PattersonRECadmusLAEmondJAPierceJPPhysical activity, diet, adiposity and female breast cancer prognosis: a review of the epidemiologic literatureMaturitas201066151520097494
- AutierPBoniolMCaution needed for country-specific cancer survivalLancet201137797609910121215872
- SchuellerGRiedlCCMallekRImage quality, lesion detection, and diagnostic efficacy in digital mammography: full-field digital mammography versus computed radiography-based mammography using digital storage phosphor platesEur J Radiol200867348749617890036
- SkaanePStudies comparing screen-film mammography and full-field digital mammography in breast cancer screening: updated reviewActa Radiol200950131419037825
- Utzon-FrankNVejborgIvon Euler-ChelpinMLyngeEBalancing sensitivity and specificity: Sixteen year’s of experience from the mammography screening programme in Copenhagen, DenmarkCancer EpidemiolJanuary 142011 [Epub ahead of print]
- MoyLEliasKPatelVIs breast MRI helpful in the evaluation of inconclusive mammographic findings?Am J Roentgenol2009193498699319770320
- KromanNChristiansenPHussainZBKehletHBreast cancer surgery in DenmarkUgeskr Laeger20101724128362839 Danish20961504
