Abstract
Background
The Danish National Patient Registry (DNPR) is one of the world’s oldest nationwide hospital registries and is used extensively for research. Many studies have validated algorithms for identifying health events in the DNPR, but the reports are fragmented and no overview exists.
Objectives
To review the content, data quality, and research potential of the DNPR.
Methods
We examined the setting, history, aims, content, and classification systems of the DNPR. We searched PubMed and the Danish Medical Journal to create a bibliography of validation studies. We included also studies that were referenced in retrieved papers or known to us beforehand. Methodological considerations related to DNPR data were reviewed.
Results
During 1977–2012, the DNPR registered 8,085,603 persons, accounting for 7,268,857 inpatient, 5,953,405 outpatient, and 5,097,300 emergency department contacts. The DNPR provides nationwide longitudinal registration of detailed administrative and clinical data. It has recorded information on all patients discharged from Danish nonpsychiatric hospitals since 1977 and on psychiatric inpatients and emergency department and outpatient specialty clinic contacts since 1995. For each patient contact, one primary and optional secondary diagnoses are recorded according to the International Classification of Diseases. The DNPR provides a data source to identify diseases, examinations, certain in-hospital medical treatments, and surgical procedures. Long-term temporal trends in hospitalization and treatment rates can be studied. The positive predictive values of diseases and treatments vary widely (<15%–100%). The DNPR data are linkable at the patient level with data from other Danish administrative registries, clinical registries, randomized controlled trials, population surveys, and epidemiologic field studies – enabling researchers to reconstruct individual life and health trajectories for an entire population.
Conclusion
The DNPR is a valuable tool for epidemiological research. However, both its strengths and limitations must be considered when interpreting research results, and continuous validation of its clinical data is essential.
Introduction
As the role of routine computerized health data in epidemiological research is growing,Citation1 there is a need to examine their strengths and limitations.Citation2,Citation3 Typical shortcomings of such data include limited linkage possibilities, incomplete temporal or geographic coverage, restriction to selected patient groups, and lack of systematic follow-up.Citation4–Citation7 Among the examples, the Dutch nationwide hospital registry has been in operation since 1963, but personal records are anonymized, and therefore not linkable to other data sources.Citation4 Also, the United Kingdom’s Clinical Practice Research Datalink has recorded detailed information on both diagnoses and prescriptions in primary care since 1987 but covers only part of the population and lacks information on patients who leave participating practices.Citation8 In the United States, the collection of routine health data is restricted to specific age groups (eg, Medicare beneficiaries),Citation6 income groups (eg, Medicaid beneficiaries),Citation6 professions (eg, the Veterans Affairs),Citation7 or members of private insurance plans (eg, Kaiser Permanente),Citation9 often without the possibility of linkage or long-term follow-up.
In the Nordic countries, government-funded universal health care, combined with the tradition of record-keeping and individual-level linkage, has led to establishment of extensive networks of interlinkable longitudinal population-based registries covering entire nations.Citation10,Citation11 Patient registries with complete nationwide coverage and individual-level linkage potential have existed in Finland since 1969,Citation12 in Sweden since 1987,Citation13 in Iceland since 1999,Citation14 and in Norway since 2008.Citation15,Citation16
The Danish National Patient Registry (DNPR) is one such population-based administrative registry, which has collected data from all Danish hospitals since 1977 with complete nationwide coverage since 1978.Citation17–Citation19 An epidemiologist setting out to use the DNPR must be familiar with the strengths and limitations of its data. Many studies have validated algorithms for identifying health events in the DNPR, but the reports are fragmented and no overview exists. Herein, we review the content and data quality of the DNPR and its potential as a research tool in epidemiology.
Setting
Denmark had 5,580,516 inhabitants in 2012, excluding inhabitants of Greenland and the Faroe Islands.Citation20 Although these areas are part of the Kingdom of Denmark, they are not covered by the DNPR. Since 2007, the Danish healthcare system has had three administrative levels:Citation10,Citation21 1) the state, responsible for legislation, national guidelines, surveillance, and health financing through the Ministry of Health; 2) the regions (n=5), responsible for delivery of primary and hospital-based care; and 3) the municipalities (n=98), responsible for a broad range of welfare services, including school health, child dental treatment, home care, primary disease prevention, and rehabilitation.
The Danish National Health Service provides tax-supported health care for the entire Danish population.Citation10,Citation21 Redistributionist taxation finances ~85% of overall health care costs, including access to general practitioners (GPs), hospitals, outpatient specialty clinics, and partial reimbursement of prescribed medications.Citation21 Of note, outpatient specialty clinics include contacts from hospital-based (ambulatory) specialty clinics but not from private practice specialists or GPs. Patients’ out-of-pocket expenditures cover the remaining costs of medication and dental care.Citation21 Except in emergencies, GPs (including on-call GPs) provide referrals to hospitals and specialists.Citation21 Approximately 4,100 GPs and 4,600 dentists, as well as physiotherapists, chiropractors, and home nurses, work in the primary health care sector.Citation21
The Danish Civil Registration System is a key tool for epidemiological research in Denmark.Citation20,Citation22 This nationwide registry of administrative information was established on April 2, 1968.Citation20 It assigns a unique ten-digit Civil Personal Register (CPR) number to all persons residing in Denmark, allowing for technically easy, cost-effective, and exact individual-level record linkage of all Danish registries.Citation20 The Danish Civil Registration System, which tracks and continuously updates information on migrations and vital status, permits long-term follow-up with accurate censoring at emigration or death.Citation20
DNPR overview
History
In the early 1970s, most nonpsychiatric hospitals in Denmark established computerized Patient Administrative Systems (PASs).Citation1 Initially, individual hospitals collected varying information. To ensure standardized data collection, the Danish Health and Medicines Authority developed a protocol for data collection, in which the unit of observation was the hospital discharge record of an individual patient.Citation23 In 1976, all Danish counties (formerly the main administrative level, replaced by regions in 2007) were requested to submit these data to a central national hospital registry, which formed the basis for the DNPR (Danish, Landspatientregisteret).Citation23 This registry was established in 1977 and achieved complete nationwide coverage in 1978.Citation24
Since its establishment, different names have been used in the literature for the DNPR. Commonly used English terms include the Danish National Hospital Register,Citation18 Danish National Health Registry,Citation19 Danish National Patient Register,Citation17 Danish Hospital Discharge Registry,Citation25 and Danish National Registry of Patients.Citation1 The official English name, as it appears in the registry declaration by the Danish Health and Medicines Authority, is the Danish National Patient Registry, DNPR. This term therefore will be used in this review.
Aims
The official aims of the DNPR are presented in .Citation26 The primary aim is continuous monitoring of hospital and health services utilization for the Danish Health and Medicines Authority, thus providing a tool for health care planning.Citation26 The registry is also increasingly used to monitor the occurrence of diseases and use of treatments,Citation27 for quality assurance in the hospital sector,Citation28 and for medical research. Since 2002, the DNPR has served as the basis for paying public and private hospitals via the Diagnosis-Related Group system.Citation29,Citation30 The registry also collects data for other health registries, including the Danish Psychiatric Central Research Register since 1995,Citation31 the Register of Legally Induced Abortions since 1995,Citation32 the Medical Birth Registry since 1997,Citation33 and the Danish Cancer Registry since 2004.Citation34
Table 1 Aims of the Danish National Patient Registry
Updates
DNPR data are updated continuously.Citation35 Each regional PAS is required by law to submit standardized data to the DNPR at least monthly, but in practice does so weekly or, for some hospitals, daily. As regional PASs may collect more information than is reportable to the DNPR, the contents of the PASs and the DNPR are overlapping but not identical. The overlapping data are referred to as the common content. The Danish Health and Medicines Authority reports all changes in the common content in its annual report – Common content for basic registration of hospital patients – which includes separate sections for usersCitation36 and developers.Citation37 An overview of the registry’s content and structure is also available online.Citation26
Reporting to the DNPR became compulsory in 2003 for private hospitals and private outpatient specialty clinics, excluding private practice specialists and GPs.Citation38,Citation39 Private practice specialists are only obliged to report activities that are not covered by the health insurance scheme (Danish, Sygesikringen). Despite their increasing share in the health sector, the 249 private hospitals and clinics in Denmark generated only 2.2% of the total hospital activity in 2010.Citation40 Registration of care provided by the private sector is mandatory, regardless of whether the referring hospital is public or private, whether out-of-pocket payments are involved, or whether patients are covered by a private health insurance.Citation38,Citation39 However, the reporting from private hospitals and clinics is generally considered incomplete.Citation17,Citation41
DNPR content
Type of data
The content of the DNPR is structured, with each variable having a finite number of possible values.Citation36,Citation37 Information reported to the DNPR includes administrative data, diagnoses, treatments, and examinations ().Citation26
Table 2 Content of the Danish National Patient Registry
Administrative data include personal and admission data. The personal data include patients’ CPR numbers and municipality and region of residence. The admission data include hospital and department codes, admission type (acute or nonacute), patient contact type (inpatient, outpatient, or emergency department [ED]), referral information, contact reason, and dates of admission and discharge.
Diagnoses associated with each hospital contact are registered in the DNPR as one primary diagnosis and, when relevant, secondary diagnoses.Citation36 The primary diagnosis is the main reason for the hospital contact. Secondary diagnoses supplement the primary diagnosis by identifying other relevant diseases related to the current hospital contact, eg, underlying chronic diseases.Citation26,Citation36 An exception (since 2009) is brain death (code: R991), which is registered as a diagnosis secondary to the primary underlying condition leading to brain death.Citation36 In addition to primary and secondary diagnoses, the registry records referral, temporary, procedure-related, and supplementary diagnoses (). The discharging physician registers all diagnoses at the time of hospital discharge or at the end of an outpatient contact. However, outpatient and inpatient psychiatric contacts with long-term attendance are reported at least monthly.Citation36 ED contacts are registered as completed hospital contacts, regardless of whether patients are transferred to another hospital department.Citation36
Treatments include information on surgery, other treatments (eg, invasive procedures, mechanical ventilation, dialysis, cancer treatments, and psychotherapy), anesthesia, and intensive care ().
Examinations include radiological procedures and other examinations (). The attending physician/surgeon registers treatment and examination codes immediately following their completion. Thus, each treatment and examination is assigned to its own exact date, independent of the dates of admission and discharge.
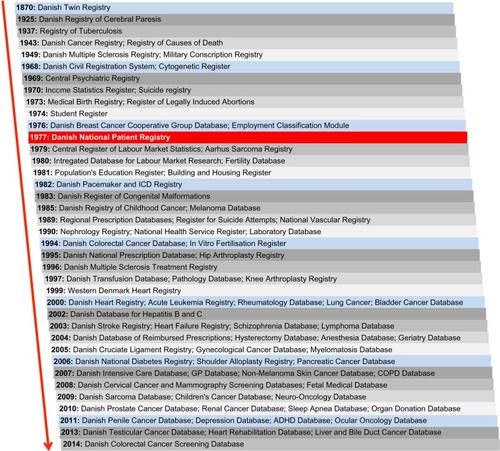
Changes in content over time
Initially, the DNPR recorded information on all inpatient contacts only at nonpsychiatric (somatic) Danish departments,Citation23 whereas psychiatric inpatient contacts were recorded in the Psychiatric Central Research Register from 1969 to 1995, after which it was merged with the DNPR.Citation31 Registration of somatic outpatient contacts started in 1994 but was not complete (including the counties of Ribe, Ringkøbing, and Copenhagen) until 1995. Thus, since 1995, all psychiatric inpatient, psychiatric and somatic outpatient, and ED contacts in Denmark have also been reported to the DNPR.Citation23
The personal data reported to the DNPR have remained unchanged since the registry’s establishment in 1977,Citation36 but over time changes have been made to the admission data, diagnoses, treatments, and examinations.Citation35
For the admission data, the first change occurred in 1987, whereby registration of patient contacts, referral information, and type of discharge was simplified (). Changes have been made almost annually thereafter, gradually expanding the registry’s content as shown in . The most recent changes to the admission data concerned type of admission and patient contact (). As of January 1, 2014, ED patients are no longer registered separately as “patient contact type 3” but instead as acute outpatients (ie, “admission type 1” and “patient contact type 2”), whereas other outpatients are registered as nonacute outpatients (ie, “admission type 2” and patient contact type 2). Thus, a patient contact in the DNPR was defined as an inpatient contact from 1977 through 1994; an inpatient, outpatient, or ED contact from 1995 through 2013; and as an inpatient or outpatient contact thereafter.
Figure 1 Timeline for the content and classification systems in the Danish National Patient Registry.
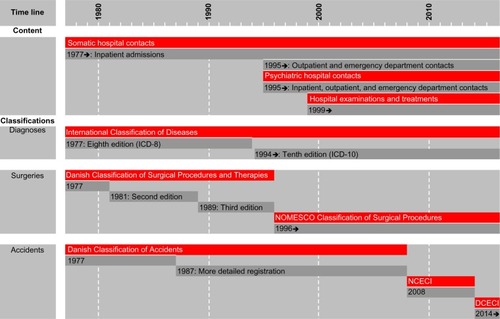
Table 3 Time line for patient contact and admission types in the Danish National Patient Registry
For diagnoses, it was originally possible to register up to 19 secondary diagnoses (ie, a maximum of 20 diagnoses per contact). Since 1995, the maximum number of recordable secondary diagnoses has increased to 99 in 1995–1998, 999 in 1999–2002, and 9,999 thereafter. Although in practice this means that there is no upper limit to the number of recordable secondary diagnoses, only the first 18 secondary diagnoses are subject to reimbursement by the Danish National Health Service.Citation42 Since the adaption of the tenth revision of the International Classification of Diseases (ICD-10) in 1994, 23% of hospital contacts have had one or more secondary diagnoses recorded. The median number of secondary diagnoses per contact in this period was 1 (interquartile range: 1–2 diagnoses).
Surgeries have been reported to the DNPR since 1977. Starting in 1999, diagnostic examinations and treatments were included.Citation26,Citation35 It became mandatory to report on many medical treatments in 2001 (including cardiac, respiratory, kidney, and cancer treatments) and on radiological examinations in 2002. The results of examinations are not included in the DNPR (). Thus, the DNPR records when a patient undergoes magnetic resonance imaging, colonoscopy, biopsy, etc, but the findings are not registered explicitly. In some cases, however, findings may implicitly be inferred from the recorded diagnoses (eg, when an ulcer diagnosis follows procedure coding for gastroscopy).
Number of patient contacts
During 1977–2012, the cumulative Danish population numbered 8,342,199 persons. During this period, 8,085,603 distinct persons were registered in the DNPR at least once. Among these, 7,268,857 (90%) persons were registered with an inpatient contact, 5,953,405 (74%) persons with an outpatient contact, and 5,097,300 (63%) persons with an ED contact. When excluding the unspecific Z-codes (factors influencing health status and contact with health services), the numbers of persons registered with inpatient, outpatient, and ED contacts were 4,610,123, 4,995,365, and 4,792,298, respectively. The distribution of all hospital contacts according to ICD category and patient contact type is shown in . The 25 most common ICD-10 diagnoses for each patient contact type are provided in .
Table 4 Number of patients registered in the Danish National Patient Registry according to disease categories and patient contacts, 1977–2012Table Footnotea
Table 5 The 25 most common ICD-10 diagnoses at the four-digit level in the Danish National Patient Registry, according to patient contact type, 1994–2012Table Footnotea
Classification systems
The SKS browser
The classifications used in the DNPR are provided in the Health Care Classification System (Danish, Sundheds-væsenets Klassifikations System [SKS]).Citation43 The SKS is a collection of international, Nordic, and Danish classifications.Citation43 SKS codes contain up to ten alphanumeric characters, the first being a letter representing a primary group, following a monohierarchical classification system.Citation43 Thus, diagnoses are registered under “D”, surgery under “K”, other treatments under “B”, anesthesia under “N”, and examinations under “U” or “ZZ” ().Citation36
To facilitate the search for SKS codes, the Danish National Health and Medicines Authority maintains a user-friendly SKS browser (),Citation44 searchable by code, by free text, or by browsing. Searching for acute myocardial infarction codes can be done by entering “DI21” or by typing the Danish or Latin term in a full phrase (akut myokardieinfarkt) or a partial phrase (eg, infarctus myo).Citation44 Manual browsing requires clicking the main group “Classification of diseases” (group D), then “Diseases of the cardiovascular system” (I), then “Ischemic heart disease” (I20–I25), and finally “Acute myocardial infarction” (I21). The SKS browser does not include historical codes,Citation44 but these are available online elsewhere.Citation45
Figure 2 User interface of the Danish Health Care Classification System (SKS browser).
Abbreviation: SKS, Sundhedsvæsenets Klassifikations System.
Changes over time
Over time, the DNPR has adopted different classification systems for diagnoses, surgeries, and accidents (), whereas the classification systems for radiological procedures and in-hospital medications have remained unchanged since their introduction into the DNPR.Citation26,Citation36
Diagnoses were classified according to the ICD-8 until the end of 1993 and the ICD-10 thereafter. The three-digit ICD-8 codes were used in a modified Danish version (with two supplementary digits), which explains in part why ICD-9 coding was never introduced in Denmark. Coding granularity improved in 1994 through introduction of the five-digit ICD-10 codes. Although the DNPR follows the current international standards for disease classification, the ICD-10 version used in Denmark often does not allow for identification of certain clinical details, such as disease severity. Supplementary codes (eg, the so-called “TUL” codes) sometimes allow for anatomical precision, eg, to identify location of a thrombosis or surgery site in right/left or upper/lower extremity, but these codes are used inconsistently. Sometimes, ABC extensions are added to specific diagnostic codes, eg, atrial fibrillation (I489B) and flutter (I489A), making the Danish version of the ICD-10 more detailed than the international ICD-10 but less detailed than the clinical modification of the ICD-10 (ICD-10-CM), which is not used in Denmark.Citation46
Surgeries were coded according to the three consecutive editions of the Danish Classification of Surgical Procedures and Therapies, from 1977 to 1995.Citation47 Since 1996, surgical procedures have been coded according to the Danish version of the Nordic Medico-Statistical Committee Classification of Surgical Procedures.Citation48
Accidents have been coded using the Danish Classification of Accidents. A detailed registration was introduced in 1987. The latest version of the classification, the Nordic Classification of External Causes of Injury, also included suicide attempts and violence.Citation26 It was adopted in 2008 and used until a new Danish Classification of External Causes of Injury was incorporated in the SKS, in 2014.Citation36,Citation37 Although closely related to the Nordic classification in structure, the new Danish classification facilitates a simpler registration of external causes of injury.
Radiological procedures (without results) are coded according to the Danish Classification of Radiological Procedures (UX codes). This classification system follows the general principles used for registration of treatments in the SKS.Citation36
In-hospital medication use (without dispensed dose or route of administration) is registered using different modules consistent with the Anatomical Therapeutic Chemical (ATC) classification system. Data on in-hospital medical treatment are not commonly used in research, except for drugs exclusively administered at hospitals, eg, fibrinolysis or cancer/immune-modulating treatments such as antibody, radiation, cytostatic, and biological therapies (). These drugs are primarily registered with a SKS treatment code, but their ATC codes can also be used as supplemental codes (eg, fibrinolysis is covered by SKS code BOHA1 and ATC code B01AD).
Data quality
Measurements of data quality
The two most common measures of data quality are validity and completeness.Citation49 By validity we refer to the extent to which a variable measures the intended construct.Citation49 The positive predictive value (PPV) of registration is the most frequently reported measure of the validity of records in the DNPR. It is defined as the proportion of patients registered with a disease who truly have the disease and is usually estimated using medical record review as the reference standard to confirm the presence of disease.Citation49 The term reference standard is used here, as medical record is not always considered the gold standard in validation studies, although one must assume that it is a better representation of the truth than the registry record.
Completeness refers to the proportion of true cases of a disease that is correctly captured by the registry.Citation49 Completeness can be measured in relation to either all individuals in the general population with a specific disease or all patients admitted/treated for the specific disease. Completeness is largely determined by the registry’s sensitivity and depends on the amount of missing data.Citation49 Since no complete reference source exists, it is difficult to estimate the overall completeness of registry data relative to the general population. Data completeness depends on hospitalization patterns and diagnostic accuracy. Thus, conditions such as nonfatal myocardial infarction or hip fracture, which should always lead to a hospital encounter, are registered consistently in the DNPR. In contrast, lifestyle risk factors (overweight, smoking, excessive alcohol consumption, and physical inactivity) and conditions as hypertension or uncomplicated diabetes are often treated by GPs and are thus not completely registered.
Overall data quality
After receiving data from the hospitals, the DNPR automatically checks for missing codes, incorrect digits, errors in CPR numbers, and inconsistencies between diagnoses and sex.Citation24 In case of errors, the records are returned to the source hospital for correction.Citation24
The Danish Health and Medicines Authority has examined the PPVs of personal data, admission data, and diagnoses in the DNPR three times, using medical record review as the reference standard.Citation24,Citation50,Citation51 The first such validation was performed in 1980 as a pilot study of 1,000 randomly sampled discharges from a single hospital (Hillerød Hospital).Citation50 The study concluded that the validity of primary diagnoses in the DNPR was not sufficient for research.Citation50 The secondary study validated 1,094 random discharges from a 1990 nationwide sample and found high overall correlation between admission and discharge data in the DNPR and medical records.Citation24 The proportion of incorrect registrations was 1.4% for admission type, 8.1% for contact reason, 0.8%–8.7% for accident registration (lowest for work-related accidents), 14.8% for the “referral to” variable, and 1.5% for date of discharge. The “referral from” data were incorrect among 11.5% of nonacute patients. However, due to differing guidelines for reporting this variable, there was considerable regional variation in its validity. In the study, diagnoses and surgical procedures were categorized according to five clinical specialties covering 85% of all nonpsychiatric discharges (). A comparison of various primary diagnoses showed correct categorization at the five-digit level for 73% of all cases, increasing to 83% when alternative diagnoses were accepted. Substantial variation was observed between different clinical specialties, with the lowest PPV for medical diagnoses (66%) and the highest PPV for diagnoses associated with orthopedic surgery (83%). For all specialties, the proportion of correct diagnoses increased substantially when the comparison was made at the three-digit rather than at the five-digit level. It increased even further when secondary diagnoses were also included (). The third validation study included 420 random discharges from a nationwide sample in 2003 and focused only on admission and discharge data.Citation51 The proportion of incorrect registrations in this sample was 3% for admission type and 8% for referral type. Data on admission/discharge dates, hospital/department codes, and CPR numbers were accurate.Citation51
Table 6 Summary results from the Danish Health and Medicines Authority’s evaluation of diagnoses in the Danish National Patient Registry in 1990 according to clinical specialties
Systematic review of validated variables
The data quality of individual variables in the DNPR has been examined on an ad hoc basis.Citation25,Citation52–Citation164 To provide researchers with an overview of such studies, we performed a systematic review, aiming to create a bibliography of validated administrative data, diagnoses, treatments, and examinations in the DNPR.
shows a flowchart for the review process, including the search strategy. We searched MEDLINE (PubMed) and the Danish Medical Journal (http://ugeskriftet.dk/udgivelser) using the Danish and the various English names for the DNPR. One author (MS) screened titles and abstracts, and when necessary the full-text papers, for inclusion in the bibliography. Because validation is often a secondary study aim and therefore not highlighted in titles, abstracts, or keywords of papers, even a comprehensive systematic search cannot identify all relevant papers. We therefore also searched the reference lists of the retrieved papers for potentially relevant articles. Finally, we included additional studies known to us beforehand. We included all studies written in English or Danish, regardless of characteristics, such as publication status or year.
Two authors (MS and SAJS) independently extracted the following data from all included papers: patient contact type (inpatient, outpatient, or ED), diagnosis type (primary vs secondary), codes/algorithms used, measure of validity (PPV/negative predictive value), measure of completeness (sensitivity/specificity), the reference standard used, and results (absolute numbers, proportions, and confidence intervals [CIs]). Any disagreements were resolved by consensus. When patient contact, diagnosis type, or codes were not specified, we contacted the corresponding authors for this information. Unspecified patient type included most often both in- and outpatient diagnoses. Unspecified diagnosis type included most often both primary and secondary diagnoses. Unconfirmed data were categorized as not available (n/a). We used extracted information as well as more detailed information from selected studies to illustrate the use of various algorithms over time and to discuss methodological considerations, in particular information bias.
Our review showed that several different methods had been used to calculate CIs for proportions. Moreover, studies varied with respect to the number of decimal points reported for CIs, while some studies failed to report CIs. To permit direct comparisons among study results, we recalculated all proportions based on the absolute numbers provided in the papers. We used Wilson’s score methods to calculate CIs with one decimal point precision.Citation165 When lack of absolute numbers precluded recalculations, we presented the results as reported in the original reference.
We identified 114 papers, validating 1–40 codes/algorithms each and 253 in total. The bibliography of validated variables is provided in . The variables are listed in the table according to the SKS coding (ie, ICD-10 codes for diagnoses and Nordic Medico-Statistical Committee codes for surgeries) and within each variable according to study period. Recalculation of all proportions reported was possible for 89% (102/114) of all studies.
We found that the PPVs of the reported diagnoses in the DNPR ranged from below 15%Citation137 to 100%.Citation58,Citation97 Some of this variation (both intervariable and intravariable variation) may result from different reference standards used. The majority of variables were examined in cross-sectional studies using medical record review as the reference standard. However, several other reference standards have also been used, including patient interviews,Citation84,Citation146 clinical registries,Citation32,Citation57,Citation78,Citation89,Citation142 the Danish Cancer Registry,Citation59,Citation60,Citation64,Citation67 a military conscription research database,Citation116 the Clinical Laboratory Information System Database,Citation72,Citation73,Citation114 the Danish National Pathology Registry and Data Bank,Citation120 the hospital pharmacy systems,Citation160 the Danish prescription registries,Citation79,Citation83 GP verification,Citation75 radiology reports,Citation111,Citation118 and autopsy reports.Citation110,Citation141 Our review revealed variation in study settings and calendar year. The study setting is important to consider, as the PPV depends on the prevalence of disease and therefore on the data’s department of origin. Thus, restriction to specialized departments, eg, rheumatology departments when examining the validity of a rheumatoid arthritis diagnosis, likely results in higher PPVs.Citation126 Similarly, the calendar year may affect the quality of variables, given the continuous improvement in diagnostic criteria and procedures used. As examples, the validation studies indicate a temporal increase in the PPV of ulcer disease (from 84% during 1997–2001Citation119 to 98% during 1998–2007Citation58) and of myocardial infarction (from 92% during 1979–1980,Citation100 94% during 1982–1991,Citation99 to almost 100% during 1996–2009Citation97). Improvements in variable completeness over time have also been documented for, eg, bacteremia (from 4.4% in 1994,Citation25 25.1% in 2000,Citation55 to 35.1% in 2011Citation55).
We found that the definition of a disease in registry data is not always based on ICD codes alone but may require algorithms that combine a diagnosis with admission data (eg, admission type, patient contact, and department specialty), other diagnostic specification (such as primary vs secondary diagnoses), procedures, in-hospital medical treatment (eg, chemotherapy), prescription use, previous medical history (to identify incident events), time since first diagnosis or metastasis (to identify recurrent events), pathology data (for tumor genotypes),Citation166 or other registry data (eg, laboratoryCitation167 and cancer dataCitation34). As an example, a validation study of recurrent venous thromboembolism tested different algorithms based on the inpatient vs outpatient diagnoses, presence or absence of an ultrasound or computed tomography (CT) scan during admission, and postdischarge anticoagulant drug use.Citation112 Based on the results of that study, a case of venous thromboembolism recurrence was defined as an inpatient diagnosis of deep venous thrombosis or pulmonary embolism recorded >3 months after the incident venous thromboembolism event among patients with an ultrasound or CT scan performed during admission (PPV =79%).Citation112 An algorithm for colorectal cancer recurrences combines metastasis and chemotherapy codes in the DNPR with cancer recurrence codes in the Danish National Pathology Registry (PPV =86%; sensitivity =95%).Citation61
Lack of completeness of the DNPR in capturing certain conditions can sometimes be compensated by data linkage to other routine registries. Diabetes can be identified from at least one outpatient dispensation record for insulin or an oral antidiabetic drug (in the Danish prescription registriesCitation168) and/or by an inpatient or outpatient hospital diagnosis of type 1 or type 2 diabetes in the DNPR.Citation76 Recent studies have supplemented the algorithm with data on glycosylated hemoglobin A1c level of ≥6.5% from the Clinical Laboratory Information System Database, increased specificity by excluding metformin-treated patients with polycystic ovarian syndrome,Citation169 and differentiated type 1 and type 2 diabetes using information on age at diagnosis combined with insulin monotherapy.Citation76
The large variation in data validity found in our review underscores the need to validate diagnoses and treatments before using DNPR data for research. Furthermore, validation studies may need updates, as newer diagnostic criteria and procedures may differ from those used in older validation studies.
DNPR as a research tool
Health events
Potential uses of the DNPR, according to study design, are presented in . Patient cohorts of interest may be identified, along with their medical history and outcomes. Thus, the DNPR may provide data on diseases,Citation170,Citation171 treatments,Citation172 and diagnostic examinations as exposures. Seasonal variation as an exposure has also been examined.Citation173
Table 7 Use of the Danish National Patient Registry according to study design
Furthermore, the DNPR allows for identification of disease occurrence in the general population (risk studies),Citation174 where the exposure information could originate from other data sources involving primary or secondary data collection, eg, military conscription cohortsCitation175 or population-based health surveys such as the Danish Health Examination Survey,Citation176 the “How Are You?” study,Citation177 the Danish Diet, Cancer and Health study,Citation178 the Soon Parents cohort,Citation179 the Glostrup Population Studies,Citation180 and the Copenhagen City Heart study.Citation181 Extraordinary long-term follow-up (>35 years) for lifestyle-associated diseases is feasible.Citation175
Using techniques similar to that in risk studies, the DNPR can be used to study outcomes in well-defined patient groups (eg, diagnostic examinations,Citation182 recurrence,Citation112 and complicationsCitation183) and prognostic factors.Citation170 These patient groups may be identified from the DNPR itself, other registries, or surveys. Most recently, the DNPR has also been used to gather long-term follow-up data for randomized controlled trials using clinically driven outcome detection.Citation184 The automated event-detection feature of the DNPR allows for large, low-cost randomized trials that reflect daily clinical practice, cover a broad range of patients and end points, and include lifelong follow-up.Citation183,Citation185–Citation187 As with cohort studies, DNPR data may be used to identify exposures and cases/outcomes in case– control studiesCitation112,Citation188,Citation189 and ecological studiesCitation182 ().
Health care planning
The administrative data related to each patient contact allow for studies of health care utilization and how health care planning may affect patient outcomes. As an example, admission rates for the most common medical conditions in Denmark have been found to be higher during the regular office hours than during the weekend hours.Citation190 However, admissions during the weekend hours have been associated with higher mortality rates (weekend nighttime hours > weekend daytime hours > weekday out-of-hours > weekday office hours).Citation190
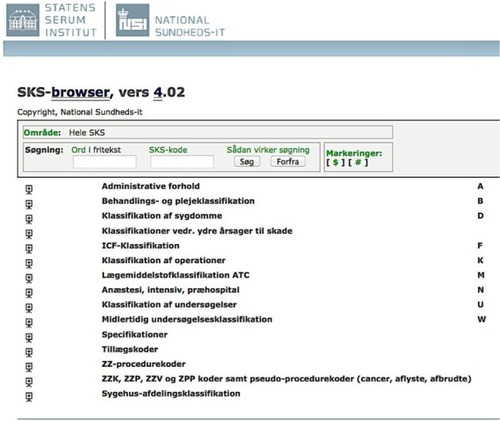
Record linkage
The availability of patient-identifiable data in the DNPR makes it technically easy to link to other Danish data sources using the CPR number.Citation20 Because Denmark’s registries are numerous and far reaching even by the high standards of the Nordic countries,Citation22,Citation191 additional information on, eg, cancer staging,Citation34 laboratory test results,Citation167 general practice utilization,Citation192 socioeconomic data,Citation193–Citation196 prescription use,Citation197 all-cause mortality,Citation20 and cause-specific mortalityCitation198 can easily be obtained to supplement the DNPR. shows the time line for the DNPR relative to selected administrative and clinical registries in Denmark, illustrating the potential for record linkage by calendar year. As shown, nationwide data can be obtained on, eg, all twins in Denmark since 1870 (the Danish Twin Registry),Citation199 specific causes of death since 1943 (the Danish Register of Causes of Death),Citation198 detailed cancer diagnoses since 1943 (the Danish Cancer Registry),Citation34 migration and vital status since 1968 (the Danish Civil Registration System),Citation20 personal income since 1970 (the Income Statistics Registry),Citation195 labor market statistics and health services since 1980 (the Integrated Database for Labour Market ResearchCitation193 and Danish National Health Service Register),Citation192 education since 1981 (the Population’s Education Register),Citation194 prescribed medications since 1995 (the Danish National Prescription Registry),Citation168 and patient tissue samples and blood transfusions since 1997 (the Danish National Pathology Registry and Blood Transfusion Databases).Citation166 The Danish clinical registries constitute the infrastructure of the National Clinical Quality Databases and the Danish Multidisciplinary Cancer Groups.Citation200 The clinical registries contain information about individual patients used for quality improvement, research, and surveillance purposes.Citation200 Linkage to one or more of the current 69 clinical registries thus provides detailed information on a range of procedures (eg, hip arthroplasty and hysterectomy) and diseases (eg, heart failure, stroke, diabetes, and various malignant diseases; ).Citation200,Citation201 Finally, individual-level linkage to data from randomized controlled trials, population surveys, and epidemiologic field studies is possible as previously described.
Methodological considerations
Methodological considerations related to the internal validity of cohort studies conducted within the DNPR are summarized subsequently and in . We also address the special methodological problems that relate to studies of temporal health trends.
Table 8 Methodological considerations related to the internal validity of cohort studies conducted with data from the Danish National Patient Registry
Precision
The nationwide coverage since 1978 provides sample sizes that permit studies of rare diseases, disease complications, and effects in subgroups of patients (effect modification and interactions). Of note, very rare diseases may still be difficult to study because of the relatively small size of the Danish population.Citation202
Selection bias
Appropriate population-based study designs can reduce selection biases in cohort studies for three reasons. First, the Danish population has a relatively stable and homogeneous demography with regard to race and religion. Second, the universal health care system (and small private hospital sector)Citation40 prevents selection bias arising from selective inclusion of specific hospitals, health insurance systems, income levels, or age groups. Third, virtually complete follow-up of all patients (with no unrecorded dropouts) is possible because the Danish Civil Registration System records vital status and migrations on a daily basis.Citation20 Still, the cohort represented in the DNPR is only unselected for diseases that always require hospital treatment. For diseases that can be treated in general practice, cases included in the DNPR to some degree represent a selected patient group, with either high severity of the disease in question (eg, herpes zoster infections, obesity, diabetes, and hypertension) or severe comorbidity leading to a lower threshold for hospital admission compared with patients without comorbidity (eg, pneumonia in transplant patients vs in young otherwise healthy adults).
Information bias
Although it is obvious that registration and retrieval of patient information from the DNPR must be based on correct SKS codes, this task is not always easy. The SKS includes many codes that might not be mutually exclusive from a clinical point of view. For many diagnoses, it is thus necessary to be aware of potential differences in registration practice among hospital departmentsCitation24 and over time.Citation122,Citation170,Citation203
Before engaging in extensive retrieval and analysis of data, it is therefore important to consult clinicians from the relevant specialty to learn about current and previous coding practices. As an example, atrial fibrillation and atrial flutter have separate codes at the four-digit level. However, a large proportion of all diagnoses for atrial fibrillation or flutter are registered as “not elsewhere specified” (Danish, uden nærmere specifikation). Since ~95% of all I48 codes correspond to atrial fibrillation and only 5% to atrial flutter,Citation104 use of the unspecified code will increase the sensitivity of the DNPR-based definition of atrial fibrillation but reduce its specificity. Hence, DNPR studies on risk of atrial fibrillation are often limited by considering atrial fibrillation and flutter as one disease entity.Citation174 Another example is ICD-10 diagnoses of stroke (I60–I64). Approximately one-third of the cases are registered as unspecified stroke (I64),Citation204 and among these, two-thirds are ischemic strokes.Citation91 Inclusion of unspecified diagnoses will increase sensitivity but reduce specificity of stroke subtypes.
The introduction of the Diagnosis-Related Group system in 2002Citation29,Citation30 regarding payment to public hospitals may have resulted in more complete registration. However, it may also have affected coding practices for some diseases and certain types of treatments. Private hospitals and clinics are potential sources of underreporting.Citation40 Although it has been mandatory for private health care providers to report all activities since 2003, and the Danish Health and Medicines Authority runs information campaigns to promote registration,Citation38 registration from private hospitals and clinics remains incomplete.Citation17,Citation41 Private hospitals offer services paid by taxes due to the rules of “free hospital choice” or as part of an agreement with a region, as well as services paid privately either by insurance companies or private parties.Citation21,Citation40 Services paid for by private parties have the highest degree of incomplete registration.
In contrast to validity, the completeness of diagnoses is often higher in the DNPR than in the clinical registries.Citation89,Citation100,Citation164,Citation205,Citation206 This higher completeness is expected since many clinical registries receive data from the DNPR. Another reason is that the law requires the national clinical registries to cover only 90% of patients with a given condition.Citation207 Moreover, the degree of completeness varies among and within clinical registries over time.Citation164,Citation208
Confounding
Nonrandomized studies are susceptible to confounding by known and unknown factors.Citation209 Therefore – irrespective of data source – the potential for confounding always needs to be addressed in the study design or analysis. The DNPR provides an opportunity to obtain information on many potential confounders, particularly comorbidities.Citation58,Citation210 The possibility of identifying such covariables from patients’ history of hospital encounters (back to 1977) rather than short-fixed historical windows may also result in less biased estimates.Citation211 Still, it should be kept in mind that incomplete registration of some diagnoses and missing data on other characteristics (eg, lifestyle risk factorsCitation212) may leave substantial residual and unmeasured confounding.
Temporal health trends
As data in the DNPR currently span almost four past decades, the registry is a unique data source to monitor long-term temporal trends in use of diagnostic procedures (eg, cardiac CT angiography),Citation164 treatments (eg, use of implantable cardioverter-defibrillators),Citation213 and disease incidence (eg, myocardial infarction).Citation27,Citation170 Related particularly to disease incidence, however, a number of methodological problems must be considered.
First, the DNPR only covers patients with disease episodes associated with hospital contact and thus not necessarily the total number of patients with a given disease (as described previously).
Second, lack of information on deaths occurring outside the hospital among persons with no previous hospital contact for a given disease may lead to underestimation of both the disease incidence and the disease-specific mortality. This problem is particularly important for acute critical events such as myocardial infarction.Citation170 Still, it should be noted that a person is not considered legally dead in Denmark before a physician has confirmed clear signs of death. Thus, all patients dying in an ambulance or otherwise arriving at a hospital with no signs of life are also admitted and registered in the DNPR (even when no resuscitation is attempted at the hospital). Data linkage to the Danish Register of Causes of DeathCitation198 may help to provide a more complete picture of the incidence of acute fatal events not included in the DNPR.Citation170
Third, it may be difficult – or even impossible – to identify incident diagnoses of chronic diseases in older patients because of immigration or the lack of hospital data before 1977. Thus, events occurring prior to 1977 are left censored if individuals are enrolled in a study and left truncated if they are not.Citation214 On the other hand, the DNPR enables reconstruction of individual life and health trajectories of persons born in 1977 or later.
Fourth, defining incidence by “the first occurrence of the disease in the registry” leads to overestimation of incidence in the period immediately following the initiation of the DNPR, after initiation of a screening program, or after introduction of new registry codes, due to misclassification of “backlogged” prevalent cases as incident cases. Because this problem decreases with the passage of time after 1977 or with the number of screening rounds, a “washout period” before identification of incident cases may reduce the error. This source of error is less important when examining diseases of short duration, such as infections. The transition from ICD-8 to ICD-10 in 1994 and inclusion of outpatients and ED diagnoses in 1995 may similarly introduce artifacts in long-term incidence trends. Exemplifying this problem, the incidence of alcoholic cirrhosis showed no clear trend for men or women of any age from 1988 to 1993 but apparently increased by 32% in 1994 and by an additional 10% when including outpatient and ED visits.Citation122
Fifth, changes in classification systems and diagnostic criteria and use of more sensitive diagnostic methods over time (diagnostic drift) may hamper the interpretation of secular trends in incidence. As an example, a transient increase in the observed rate of hospitalization with myocardial infarction in Denmark between 2000 and 2004 was likely attributable not to the true increase of occurrence but to new diagnostic criteria introduced in 2000, which included troponin as the main diagnostic biomarker.Citation170,Citation215 Similar time-trend biases have been observed for the incidence of primary liver cancerCitation203 and advanced stages of lung cancer, the latter leading to an apparent improvement over time in stage-specific prognosis.Citation216
Data access
The Danish Health and Medicines Authority has established guidelines for releasing data from the DNPR. Implementing the European Union Data Protection Directive (Directive 95/46/EC) on the protection of individuals with regard to the processing of personal data and on the free movement of such data, the Danish Act on Processing of Personal Data provides the legal basis for private and public institutions to obtain individually identifiable health data for research purposes.Citation217 This Act protects against abuse of such data and thus balances the privacy rights of individuals and the society’s need for quality research. In order to access data from the DNPR, researchers have to apply to Research Service (Danish, Forskerservice).Citation26,Citation218 Use of any health data also requires project-specific permission from the Danish Data Protection Agency,Citation217 and, in many cases, additional permission from the Danish Health and Medicines Authority to link data from various registries.Citation26 The Danish Data Protection Agency specifies safety precautions for data processing and also sets cancellation deadlines, ensuring that data traceable to individuals will not be stored longer than required to complete a project. As well, it is necessary to obtain permission from the Danish Health and Medicines Authority and the chief physician from relevant hospital departments to retrieve medical record files for validation of DNPR data.Citation219
Conclusion
The DNPR is a valuable tool for epidemiological research, providing longitudinal registration of diagnoses, treatments, and examinations, with complete nationwide coverage since 1978. Denmark’s constellation of universal health care, routine and long-standing registration of life and health events, and the possibility of exact individual-level linkage impart virtually unlimited research possibilities onto the DNPR. At the same time, varying completeness and validity of the individual variables underscore the need for validation of its clinical data before using the registry for research.
Author contributions
MS conceived the study idea, designed the study, and wrote the initial draft. MS reviewed the literature on the registry content together with JLS; study examples together with HTS; and previous validation studies together with SAJS. HTS obtained data permissions and LP collected the data and carried out the descriptive analyses. All authors contributed to data analysis, drafting and critical revision of the paper, and agree to be accountable for all aspects of the work.
Acknowledgments
The study was approved by the Danish Data Protection Agency (record number 1-16-02-1-08). Author HTS was supported by the Program for Clinical Research Infrastructure (PROCRIN) established by the Lundbeck Foundation and the Novo Nordisk Foundation, and the Department of Clinical Epidemiology’s Research Foundation. The funding sources had no role in the design, conduct, analysis, or reporting of the study.
Supplementary materials
Figure S1 Flowchart for the systematic review of validation studies.
Notes: The literature search was performed on July 20, 2015 using the following search string in 1) PubMed: “Danish National Patient Registry” OR “Danish National Registry of Patients” OR “Danish National Hospital Register” OR “Danish National Health Registry” OR “Danish National Patient Register” OR “Danish Hospital Discharge Registry” OR “Danish National Hospital Registry” OR “Danish Hospital Registers”; and 2) the Danish Medical Journal: “Landspatientregisteret”.
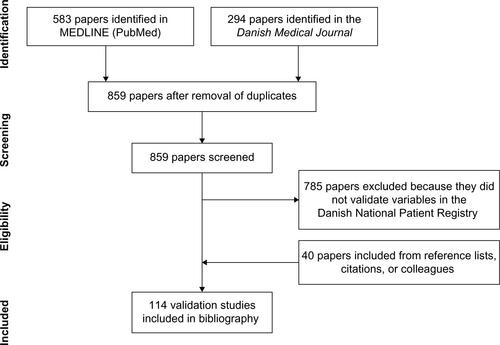
Table S1 Bibliography of validated administrative data, diagnoses, treatments, and examinations in the Danish National Patient Registry
Disclosure
The authors report no conflicts of interest in this work.
References
- SørensenHTRegional administrative health registries as a resource in clinical epidemiology: a study of options, strengths, limitations and data quality provided with examples of useInt J Risk Saf Med199710112223511270
- SorensenHTSabroeSOlsenJA framework for evaluation of secondary data sources for epidemiological researchInt J Epidemiol19962524354429119571
- BenchimolEISmeethLGuttmannAThe Reporting of studies Conducted using Observational Routinely-collected health Data (RECORD) StatementPLoS Med20151210e100188526440803
- PHARMOThe Dutch Hospital Database Available from: http://www.pharmo.nl/pharmo-databases/hospitalisationslmrAccessed April 1, 2015
- García-RodríguezLAPérez GutthannSUse of the UK general practice research database for pharmacoepidemiologyBr J Clin Pharmacol19984554194259643612
- LichtmanJHLeifheit-LimsonECGoldsteinLBCenters for medicare and medicaid services medicare data and stroke research: goldmine or landmine?Stroke201546259860425593137
- BoykoEJKoepsellTDGazianoJMHornerRDFeussnerJRUS department of veterans affairs medical care system as a resource to epidemiologistsAm J Epidemiol2000151330731410670556
- HerrettEGallagherAMBhaskaranKData resource profile: clinical practice research datalink (CPRD)Int J Epidemiol201544382783626050254
- National Cancer InstitutePharmacoepidemiology and Healthcare Databases Available from: http://epi.grants.cancer.gov/pharm/pharmacoepi_db/Accessed June 24, 2015
- Health Statistics for the Nordic Countries 2014Nordic Medico-Statistical Committee2014102
- OlsenJBassoOSørensenHTWhat is a population-based registry?Scand J Public Health1999271787810847676
- SundRQuality of the Finnish hospital discharge register: a systematic reviewScand J Public Health201240650551522899561
- LudvigssonJFAnderssonEEkbomAExternal review and validation of the Swedish national inpatient registerBMC Public Health201111145021658213
- GudbjornssonBThorsteinssonSBSigvaldasonHRofecoxib, but not celecoxib, increases the risk of thromboembolic cardiovascular events in young adults – a nationwide registry-based studyEur J Clin Pharmacol201066661962520157701
- HelsedirektoratetNorsk pasientregister Available from: http://www.helsedirektoratet.no/kvalitet-planlegging/norsk-pasientregisternpr/innhold-og-kvalitet/Sider/default.aspxAccessed April 1, 2015
- Office of the Auditor General of NorwayRevisjonsrapport om kvaliteten på de medisinske kodingene i helseforetakene som grunnlag for innsatsstyrt finansiering. I: Riksrevisjonens kontroll med forvaltningen av statlige selskaper for 2008 Dokument 322009–2010 Vedlegg 5Oslo2009
- LyngeESandegaardJLReboljMThe Danish national patient registerScand J Public Health2011397 Suppl303321775347
- AndersenTFMadsenMJorgensenJMellemkjoerLOlsenJHThe Danish national hospital register. A valuable source of data for modern health sciencesDan Med Bull199946326326810421985
- NickelsenTNData validity and coverage in the Danish National Health Registry. A literature review [in Danish: Datavaliditet og dækningsgrad i Landspatientregisteret. En litteraturgennemgang]Ugeskr Laeger20021641333711810794
- SchmidtMPedersenLSørensenHTThe Danish civil registration system as a tool in epidemiologyEur J Epidemiol201429854154924965263
- Ministry of Interior and Health. Health Care in Denmark2008 Available from: http://tyskland.um.dk/de/~/media/Tyskland/German-site/Documents/Reise%20und%20Aufenthalt/Health%20Care%20in%20Denmark.pdfAccessed October 8, 2015
- FrankLEpidemiology. When an entire country is a cohortScience200028754622398239910766613
- Danish Health and Medicines AuthorityThe Danish National Patient Registry Through 25 Years: 1977–20022003Copenhagen Report 21
- Danish Health and Medicines AuthorityEvaluation of the Danish National Patient Registry 1990 Hospital Statistics II57Copenhagen1993
- MadsenKMSchønheyderHCKristensenBNielsenGLSørensenHTCan hospital discharge diagnosis be used for surveillance of bacteremia? A data quality study of a Danish hospital discharge registryInfect Control Hosp Epidemiol19981931751809552185
- eSundhedDocumentation of the Danish National Patient Registry Available from: http://www.esundhed.dk/dokumentation/Registre/Sider/Register.aspx#Pc980378f70f74dd890a9bdb3d00abd5a_2_340iT0Accessed April 1, 2015
- Department of Clinical Epidemiology, Aarhus University Hospital, DenmarkAUDEO – Program for Disease Epidemiology and Outcomes Available from: http://www.audeo.dk/sygdomsmonitorering.aspxAccessed April 1, 2015
- LidegaardØVestergaardCHHammerumMSQuality monitoring based on data from the Danish National Patient Registry. [in Danish: Kvalitetsmonitorering ud fra data i Landspatientregisteret]Ugeskr Laeger2009171641241519208329
- The Diagnosis Related Group (DRG) SystemBeretning om DRG-SystemetThe National Audit Office of DenmarkCopenhagen2011 in Danish
- The Diagnosis Related Group (DRG) system and the Danish Ambulant Grouping System (DAGS) Available from: http://www.drg.dkAccessed April 1, 2015
- MorsOPertoGPMortensenPBThe Danish psychiatric central research registerScand J Public Health2011397 Suppl545721775352
- KrebsLJohansenAMTHelweg-LarsenKIndberetning af prokerede aborter i 1994: En sammenligning mellem data i registret over Legalt Provokerede Aborter og LandspatientregistretUgeskr Laeger199715911160716119092143
- KnudsenLOlsenJThe Danish medical birth registryDan Med Bull19984533203239675544
- GjerstorffMLThe Danish cancer registryScand J Public Health2011397 Suppl424521775350
- Danish Health and Medicines AuthorityChanges in the reporting to the Danish National Patient Registry, 2000–2015 [in Danish: Ændringer til indberetning til Landspatientregisteret]2015
- Danish Health and Medicines AuthorityFællesindhold for basisregistrering af sygehuspatienter – Vejledningsdel [Common Content for Basic Registration of Hospital Patients 2014 – Instruction Part]22nd ed2014Copenhagen [Report no 6]. Danish
- Danish Health and Medicines AuthorityCommon Content for Basic Registration of Hospital Patients 2014 – Technical Part (in Danish: Fællesindhold for basisregistrering af sygehuspatienter – Teknisk del)23nd ed2013Copenhagen Report 6
- Danish Health and Medicines AuthorityBekendtgørelse om lægers anmeldelse til Sundhedsstyrelsens Landspatientregister af patienter behandlet på private sygehuse eller klinikker2003Copenhagen Notification no 986
- Danish Health and Medicines AuthorityBekendtgørelse om lægers anmeldelse til Sundhedsstyrelsens Landspatientregister af patienter behandlet på private sygehuse eller klinikker2007Copenhagen Notification no 1073
- Danish Health and Medicines AuthorityPrivate hospital activity 2006–2010 [In Danish: Aktivitet på private sygehuse 2006–20102011 Available from: http://sundhedsstyrelsen.dk/publ/Publ2011/DOKS/AktivitetPrivateSygehuse/AktvitetPrivateSygehuse2006-10.pdfAccessed April 1, 2015
- PolitikenLack of control with private hospitals. [in Danish: Hul i kontrollen med privathospitaler]2008 Available from: http://pol.dk/565165Accessed August 1, 2015
- Personal CorrespondenceSundhedsdokumentation Sektor for National Sundhedsdokumentation og ForskningDenmark201412
- National Health ITSundhedsvæsenets Klassifikations System (SKS) Available from: http://www.ssi.dk/sksAccessed October 1, 2015
- National Health ITSKS-Browser Available from: http://www.medinfo.dk/sks/brows.phpAccessed April 1, 2015
- The reference as indicated is correct (free access as guest user), thus with the updated date the please change the reference to: National Health ITHistorical SKS Codes Available from: ftp://filer.sst.dk/filer/sks/data/skscomplete/Accessed October 1, 2015
- Centers for Disease Control and PreventionInternational Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) Available from: http://www.cdc.gov/nchs/icd/icd10cm.htmAccessed April 1, 2015
- Danish Health and Medicines AuthorityDanish Classification of Surgical Procedures and Therapies1st, 2nd, 3rd edCopenhagen, DenmarkDanish Health and Medicines Authority1973, 1980, 1988
- The Nordic Medico-Statistical Committee (NOMESCO) Classification of Surgical Procedures Available from: http://nowbase.org/Publikationer/~/media/Projekt%20sites/Nowbase/Publikationer/NCSP/NCSP%201_14.ashxAccessed April 1, 2015
- BaronJASørensenHTSoxHCJrClinical epidemiologyOlsenJSaracciRTrichopoulosDTeaching Epidemiology: A Guide for Teachers in Epidemiology, Public Health and Clinical Medicine4th ed444462OxfordOxford University Press2015
- JürgensenHJFrølundCGustafsenJMosbechHGuldhammerBMosbechJRegistration of diagnoses in the Danish national registry of patientsMethods Inf Med19862531581643736436
- Division of Health Planning at C. F. Møller on behalf of The Danish National Board of HealthProject concerning data quality in The Danish National Patient Registry in Danish: Projekt vedrørende datakvalitet i Landspatientregistret2004
- Vest-HansenBRiisAHChristiansenCFRegistration of acute medical hospital admissions in the Danish national patient registry: a validation studyClin Epidemiol2013512913323658498
- Holland-BillLXuHSørensenHTPositive predictive value of primary inpatient discharge diagnoses of infection among cancer patients in the Danish national registry of patientsAnn Epidemiol20142485937597.e1e1825084702
- SørensenHTHansenIEjlersenESchønheyderHCHamburgerHSabroeSIdentification of cases of meningococcal disease: data quality in two Danish population-based information systems during a 14-year periodInt J Risk Saf Med19957317918923511794
- GradelKONielsenSLPedersenCDanish Collaborative Bacteraemia Network (DACOBAN)Danish Observational Registry of Infectious Syndromes (DORIS)Low completeness of bacteraemia registration in the Danish national patient registryPLoS One2015106e013168226121584
- SøgaardKKThomsenRWSchønheyderHCSøgaardMPositive predictive values of the international classification of diseases, 10th revision diagnoses of Gram-negative septicemia/sepsis and urosepsis for presence of Gram-negative bacteremiaClin Epidemiol2015719519925709502
- ObelNReinholdtHOmlandLHEngsigFSørensenHTHansenA-BERetrivability in the Danish national hospital registry of HIV and hepatitis B and C coinfection diagnoses of patients managed in HIV centers 1995–2004BMC Med Res Methodol200882518439245
- ThygesenSKChristiansenCFChristensenSLashTLSørensenHTThe predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish national registry of patientsBMC Med Res Methodol2011118321619668
- OsterlindAJensenOMEvaluation of cancer registration in Denmark in 1977. Preliminary evaluation of cancer registration by the Cancer Register and the National Patient Register [in Danish: Evaluering af cancerregistreringen i Danmark 1977. En praeliminaer evaluering af cancerregisterets og landspatientregisterets registrering af cancertilfaelde]Ugeskr Laeger198514731248324884060314
- HelqvistLErichsenRGammelagerHJohansenMBSørensenHTQuality of ICD-10 colorectal cancer diagnosis codes in the Danish national registry of patientsEur J Cancer Care (Engl)201221672272722510213
- LashTLRiisAHOstenfeldEBErichsenRVybergMThorlacius-UssingOA validated algorithm to ascertain colorectal cancer recurrence using registry resources in DenmarkInt J Cancer201513692210221525307704
- KjaergaardJClemmensenIHStormHHValidity and completeness of registration of surgically treated malignant gynaecological diseases in the Danish national hospital registryJ Epidemiol Biostat20016538739211822728
- DrljevicABorreMEhrensteinVNguyen-nielsenMHøyerMQuality of venous thromboembolism diagnoses among prostate cancer patients in the Danish national registry of patientsClin Epidemiol2014635135725328419
- GammelagerHChristiansenCFJohansenMBBorreMSchoonenMSørensenHTQuality of urological cancer diagnoses in the Danish national registry of patientsEur J Cancer Prev201221654555122433631
- JensenAØNørgaardMYongMFryzekJPSørensenHTValidity of the recorded international classification of diseases, 10th edition diagnoses codes of bone metastases and skeletal-related events in breast and prostate cancer patients in the Danish national registry of patientsClin Epidemiol2009110110820865091
- EhrensteinVHernandezRKMaegbaekMLValidation of algorithms to detect distant metastases in men with prostate cancer using routine registry data in DenmarkClin Epidemiol2015725926525914556
- NørgaardMSkriverMVGregersenHPedersenGSchønheyderHCSørensenHTThe data quality of haematological malignancy ICD-10 diagnoses in a population-based hospital discharge registryEur J Cancer Prev200514320120615901987
- KjaergaardJClemmensenIHThomsenBLStormHHValidity of diagnoses of and operations for nonmalignant gynecological conditions in the Danish national hospital registryJ Clin Epidemiol200255213714211809351
- NielsenEHLindholmJLaurbergPUse of combined search criteria improved validity of rare disease (craniopharyngioma) diagnosis in a national registryJ Clin Epidemiol201164101118112621463925
- GregersenHLarsenCHaglundAMortensenRAndersenNFNørgaardMData quality of the monoclonal gammopathy of undetermined significance diagnosis in a hospital registryClin Epidemiol2013532132624009431
- AndersenGSToftdahlDNielsenPEStrandgaardSLundJOPheochromocytoma in Denmark 1977–1981 [in Danish: Faeokromocytom i Danmark 1977–1981]Ugeskr Laeger198614847310931133810901
- ZalfaniJFrøslevTOlsenMPositive predictive value of the international classification of diseases, 10th edition diagnosis codes for anemia caused by bleeding in the Danish national registry of patientsClin Epidemiol2012432733123236255
- Ben GhezalaIArendtJFErichsenRPositive predictive value of the diagnosis coding for vitamin B12 deficiency anemia in the Danish national patient registerClin Epidemiol2012433333823271924
- HedenKEKJensenAØFarkasDKNørgaardMValidity of a procedure to identify patients with chronic idiopathic thrombocytopenic purpura in the Danish national registry of patientsClin Epidemiol2009171020865080
- KristensenJKDrivsholmTBCarstensenBSteding-JensenMGreenAValidation of methods to identify known diabetes on the basis of health registers [in Danish: Validering af metoder til identifikation af erkendt diabetes på basis af administrative sundhedsregistre]Ugeskr Laeger2007169181687169217532878
- ThomsenRWHundborgHHLervangH-HJohnsenSPSørensenHTSchønheyderHCDiabetes and outcome of community-acquired pneumococcal bacteremia: a 10-year population-based cohort studyDiabetes Care2004271707614693969
- AtladóttirHOPedersenMGThorsenPAssociation of family history of autoimmune diseases and autism spectrum disordersPediatrics2009124268769419581261
- SvenssonJMarinelliKEisingSLandspatientregisteret over for et specialespecifikt register for diabetes i barnealderen?Ugeskr Laeger2007169212217227658
- NielsenGLSørensenHTPedersenABSabroeSAnalyses of data quality in registries concerning diabetes mellitus – A comparison between a population based hospital discharge and an insulin prescription registryJ Med Syst19962011108708487
- DalJSkouNNielsenEHPedersenLJoergensenJOLAcromegaly according to the Danish national registry of patients: how valid are ICD diagnoses and how do patterns of registration affect the accuracy of registry data?Clin Epidemiol2014629529925210475
- LundJOAndersenGSToftdahlDStrandgaardSNielsenPEPrimary aldosteronism (Conn’s syndrome) in Denmark 1977–1981 [in Danish: Primaer aldosteronisme (Conn’s syndrom) i Danmark 1977–1981]Ugeskr Laeger198614847311531183810903
- RasmussenNHThomsenRWRasmussenHHSøgaardMValidity of diagnostic coding for undernutrition in hospitalsClin Nutr2015 Epub ahead of print
- Holland-BillLChristiansenCFUlrichsenSPRingTJørgensenJOLSørensenHTValidity of the international classification of diseases, 10th revision discharge diagnosis codes for hyponatraemia in the Danish national registry of patientsBMJ Open201444e004956
- PhungTKTAndersenBBHøghPKessingLVMortensenPBWaldemarGValidity of dementia diagnoses in the Danish hospital registersDement Geriatr Cogn Disord200724322022817690555
- KioumourtzoglouM-ASealsRMHimmerslevLGredalOHansenJWeisskopfMGComparison of diagnoses of amyotrophic lateral sclerosis by use of death certificates and hospital discharge data in the Danish populationAmyotroph Lateral Scler Frontotemporal Degener2015163–422422925946516
- WermuthLLassenCFHimmerslevLOlsenJRitzBValidation of hospital register-based diagnosis of Parkinson’s diseaseDan Med J2012593A439122381086
- RugbjergKRitzBKorboLMartinussenNOlsenJHRisk of Parkinson’s disease after hospital contact for head injury: population based case-control studyBMJ2008337a249419074944
- GreeneNLassenCFRugbjergKRitzBReproductive factors and Parkinson’s disease risk in Danish womenEur J Neurol20142191168e6824750445
- MasonKThygesenLCStenagerEBrønnum-HansenHKoch-HenriksenNEvaluating the use and limitations of the Danish national patient register in register-based research using an example of multiple sclerosisActa Neurol Scand2012125321321721699500
- ChristensenJVestergaardMOlsenJSideniusPValidation of epilepsy diagnoses in the Danish national hospital registerEpilepsy Res2007752–316217017624737
- KrarupL-HBoysenGJanjuaHPrescottETruelsenTValidity of stroke diagnoses in a National register of patientsNeuroepidemiology200728315015417478969
- JohnsenSPOvervadKSørensenHTTjønnelandAHustedSEPredictive value of stroke and transient ischemic attack discharge diagnoses in the Danish national registry of patientsJ Clin Epidemiol200255660260712063102
- DjurhuusBDSkyttheAFaberCEValidation of the cholesteatoma diagnosis in the Danish national hospital registerDan Med Bull20105710A415921040678
- SchmidtMJohannesdottirSALemeshowSObesity in young men, and individual and combined risks of type 2 diabetes, cardiovascular morbidity and death before 55 years of age: a Danish 33-year follow-up studyBMJ Open201334e002698
- NielsenHWTüchsenFJensenMVValiditeten af diagnosen essentiel hypertension i LandspatientregistretUgeskr Laeger199615821631678553488
- JoensenAMJensenMKOvervadKPredictive values of acute coronary syndrome discharge diagnoses differed in the Danish national patient registryJ Clin Epidemiol200962218819418722087
- ColomaPMValkhoffVEMazzagliaGEU-ADR ConsortiumIdentification of acute myocardial infarction from electronic healthcare records using different disease coding systems: a validation study in three European countriesBMJ Open201336e002862
- Stratifed analyses of the positive predictive values were kindly provided by Albert Marni JoensenDepartment of Cardiology, Aalborg University HospitalAalborg, Denmark2014
- MadsenMDavidsenMRasmussenSAbildstromSZOslerMThe validity of the diagnosis of acute myocardial infarction in routine statistics: a comparison of mortality and hospital discharge data with the Danish MONICA registryJ Clin Epidemiol200356212413012654406
- MadsenMBallingHEriksenLSThe validity of the diagnosis of acute myocardial infarction in two registries: the Heart Registry compared to the National Patient Registry [in Danish: Validiteten af diagnosen akut myokardieinfarkt i to registre: Hjerteregistret sammenlignet med Landspatientregistret]Ugeskr Laeger199015253083142301079
- SeverinsenMTKristensenSROvervadKDethlefsenCTjønnelandAJohnsenSPVenous thromboembolism discharge diagnoses in the Danish national patient registry should be used with cautionJ Clin Epidemiol201063222322819595569
- LarsenTBJohnsenSPMøllerCILarsenHSørensenHTA review of medical records and discharge summary data found moderate to high predictive values of discharge diagnoses of venous thromboembolism during pregnancy and postpartumJ Clin Epidemiol200558331631915718123
- IngemanAAndersenGHundborgHHJohnsenSPMedical complications in patients with stroke: data validity in a stroke registry and a hospital discharge registryClin Epidemiol2010251320865097
- RixTARiahiSOvervadKLundbye-ChristensenSSchmidtEBJoensenAMValidity of the diagnoses atrial fibrillation and atrial flutter in a Danish patient registryScand Cardiovasc J201246314915322397620
- FrostLAndersenLVVestergaardPHustedSMortensenLSTrend in mortality after stroke with atrial fibrillationAm J Med20071201475317208079
- FrostLVestergaardPAlcohol and risk of atrial fibrillation or flutter: a cohort studyArch Intern Med2004164181993199815477433
- MardSNielsenFEPositive predictive value and impact of misdiagnosis of a heart failure diagnosis in administrative registers among patients admitted to a university hospital cardiac care unitClin Epidemiol2010223523921042557
- KümlerTGislasonGHKirkVAccuracy of a heart failure diagnosis in administrative registersEur J Heart Fail200810765866018539522
- WildenschildCMehnertFThomsenRWRegistration of acute stroke: validity in the Danish stroke registry and the Danish national registry of patientsClin Epidemiol20136273624399886
- GaistDVaethMTsiropoulosIRisk of subarachnoid haemorrhage in first degree relatives of patients with subarachnoid haemorrhage: follow up study based on national registries in DenmarkBMJ2000320722814114510634731
- TuckuvieneRKristensenSRHelgestadJChristensenALJohnsenSPPredictive value of pediatric thrombosis diagnoses in the Danish national patient registryClin Epidemiol2010210712220865109
- SchmidtMCannegieterSCJohannesdottirSADekkersOMHorvath-PuhoESørensenHTStatin use and venous thromboembolism recurrence: a combined nationwide cohort and nested case-control studyJ Thromb Haemost20141281207121524818818
- LidegaardØNielsenLHSkovlundCWSkjeldestadFELøkkegaardERisk of venous thromboembolism from use of oral contraceptives containing different progestogens and oestrogen doses: Danish cohort study, 2001–9BMJ2011343d6423d642322027398
- StensballeLGKristensenKNielsenJAabyPDiagnosis coding in the Danish national patient registry for respiratory syncytial virus infectionsScand J Infect Dis2005371074775216191894
- ThomsenRWLangePHellquistBValidity and underrecording of diagnosis of COPD in the Danish national patient registryRespir Med201110571063106821320769
- JensenAØNielsenGLEhrensteinVValidity of asthma diagnoses in the Danish national registry of patients, including an assessment of impact of misclassification on risk estimates in an actual datasetClin Epidemiol20102677220865105
- MothGVedstedPSchiøtzPONational registry diagnoses agree with medical records on hospitalized asthmatic childrenActa Paediatr200796101470147317727688
- SøgaardMKornumJBSchønheyderHCThomsenRWPositive predictive value of the ICD-10 hospital diagnosis of pleural empyema in the Danish national registry of patientsClin Epidemiol20113858921386977
- LassenAHallasJde MuckadellOBSComplicated and uncomplicated peptic ulcers in a Danish county 1993–2002: a population-based cohort studyAm J Gastroenterol2006101594595316573778
- FonagerKSørensenHTRasmussenSNMøller-PetersenJVybergMAssessment of the diagnoses of Crohn’s disease and ulcerative colitis in a Danish hospital information systemScand J Gastroenterol19963121541598658038
- VestbergKThulstrupAMSørensenHTOttesenPSabroeSVilstrupHData quality of administratively collected hospital discharge data for liver cirrhosis epidemiologyJ Med Syst199721111209172066
- JepsenPVilstrupHSørensenHTAlcoholic cirrhosis in Denmark – population-based incidence, prevalence, and hospitalization rates between 1988 and 2005: a descriptive cohort studyBMC Gastroenterol200881318261240
- ErichsenRStrateLSørensenHTBaronJAPositive predictive values of the international classification of disease, 10th edition diagnoses codes for diverticular disease in the Danish national registry of patientsClin Exp Gastroenterol2010313914221694857
- FloydAPedersenLNielsenGLThorladcius-UssingOSørensenHTSecular trends in incidence and 30-day case fatality of acute pancreatitis in North Jutland County, Denmark: a register-based study from 1981–2000Scand J Gastroenterol200237121461146512523598
- MajholmBBartholdyJChristoffersenJKEngbækJMøllerAMPoor agreement between data from the National patient registry and the Danish patient insurance associationDan Med J2012596A443022677234
- PedersenMKlarlundMJacobsenSSvendsenAJFrischMValidity of rheumatoid arthritis diagnoses in the Danish national patient registryEur J Epidemiol200419121097110315678789
- FriisSMellemkjaerLMcLaughlinJKConnective tissue disease and other rheumatic conditions following breast implants in DenmarkAnn Plast Surg1997391189229085
- JensenMVTüchsenFErhverv og diskusprolaps i lænden [Lumbar disc prolapse]Ugeskr Laeger19951571115191523 Danish7725550
- GammelagerHSværkeCNoerholtSEValidity of an algorithm to identify osteonecrosis of the jaw in women with postmenopausal osteoporosis in the Danish national registry of patientsClin Epidemiol2013526326723946670
- GammelagerHErichsenRAntonsenSPositive predictive value of the international classification of diseases, 10th revision, codes to identify osteonecrosis of the jaw in patients with cancerCancer Epidemiol201236438138322534488
- EhrensteinVGammelagerHSchiødtMEvaluation of an ICD-10 algorithm to detect osteonecrosis of the jaw among cancer patients in the Danish national registry of patientsPharmacoepidemiol Drug Saf201524769370025974710
- SchmidtLDamsgaardMTNielsenJMAn evaluation of the national patient register. A study of validity of some abortion diagnosesUgeskr Laeger198915151347834822609461
- LohseSRFarkasDKLohseNValidation of spontaneous abortion diagnoses in the Danish national registry of patientsClin Epidemiol2010224725021152251
- KlemmensenÅKOlsenSFØsterdalMLTaborAValidity of preeclampsia-related diagnoses recorded in a national hospital registry and in a postpartum interview of the womenAm J Epidemiol2007166211712417556761
- KristensenJLanghoff-RoosJSkovgaardLTKristensenFBValidation of the Danish birth registrationJ Clin Epidemiol19964988938978699210
- Langhoff-RoosJRasmussenSDanish Health and Medicines Authority. [Validering af Landspatientregistret (LPR) mhp. obstetrisk forskning og kvalitetssikring]Copenhagen2003
- DevantierAKjerJJThe national patient register – a research tool? [in Danish: Landspatientregistret – et forskningsredskab?]Ugeskr Laeger199115375165172000668
- ThygesenSKOlsenMChristiansenCPositive predictive value of the infant respiratory distress syndrome diagnosis in the Danish national patient registryClin Epidemiol2013529529823976865
- MaimburgRDBechBHBjerreJVOlsenJMøller-MadsenBObstetric outcome in Danish children with a validated diagnosis of kernicterusActa Obstet Gynecol Scand20098891011101619639464
- AgergaardPHebertABjerreJSørensenKMOlesenCOstergaardJRChildren diagnosed with congenital cardiac malformations at the national university departments of pediatric cardiology: positive predictive values of data in the Danish national patient registryClin Epidemiol20113616621386975
- JepsenBJepsenPJohnsenSPEspersenGTSørensenHTValidity of diagnoses of cardiac malformations in a Danish population-based hospital-discharge registryInt J Risk Saf Med20061827781
- LarsenHNielsenGLBendsenJFlintCOlsenJSørensenHTPredictive value and completeness of the registration of congenital abnormalities in three Danish population-based registriesScand J Public Health2003311121612623519
- JensenMSSnerumTMOlsenLHAccuracy of cryptorchidism diagnoses and corrective surgical treatment registration in the Danish national patient registryJ Urol201218841324132922902026
- PedersenLSkriverMVNørgaardMSørensenHTMaternal use of loratadine during pregnancy and risk of hypospadias in offspringInt J Med Sci200631212516575420
- GravholtCHJuulSNaeraaRWHansenJMorbidity in Turner syndromeJ Clin Epidemiol19985121471589474075
- VestergaardMObelCHenriksenTBThe Danish national hospital register is a valuable study base for epidemiologic research in febrile seizuresJ Clin Epidemiol2006591616616360562
- LauridsenMDGammelagerHSchmidtMNielsenHChristiansenCFPositive predictive value of international classification of diseases, 10(th) revision, diagnosis codes for cardiogenic, hypovolemic, and septic shock in the Danish national patient registryBMC Med Res Methodol20151512325888061
- SørensenHTNielsenJONissenINielsenJHead injuries. I. An epidemiological study based on 596 patients over a 4-year period [in Danish: Kranietraumer. I. En epidemiologisk undersøgelse baseret på 596 patienter i en 4 års periode]Ugeskr Laeger1987149106806833576741
- HougaardKKjaersgaard-AndersenPKuurERegistration under the diagnosis of traumatic hip luxation in the national registry [in Danish: Landspatientregisterets registrering under diagnosen traumatisk hofteluksation]Ugeskr Laeger199215440274727481413210
- SørensenHTNielsenBOstergaard NielsenJAnaphylactic shock occurring outside hospitalsAllergy19894442882902735517
- LangeJPedersenABTroelsenADo hip prosthesis related infection codes in administrative discharge registers correctly classify periprosthetic hip joint infection?Hip Int2015 Epub ahead of print
- McLaughlinJKOlsenJHFriisSMellemkjaerLFraumeniJFRe: breast implants, cancer, and systemic sclerosisJ Natl Cancer Inst19958718141514167658505
- HolteKBay-NielsenMUtzonJStøckelMFunch-JensenPKehletHOperation for gastroøsofageal refluks i Danmark 1997–1999Ugeskr Laeger2001163415658566111665467
- HarboeKMAnthonsenKBardramLValidation of data and indicators in the Danish cholecystectomy databaseInt J Qual Health Care200921316016819304994
- JespersenCGBorreMNørgaardMValidity of the recorded codes of gonadotropin-releasing hormone agonist treatment and orchiectomies in the Danish national patient registryClin Epidemiol2012414514922942650
- MøllerCKehletHUtzonJOttesenBSHysterectomy in Denmark. An analysis of postoperative hospitalisation, morbidity and readmissionUgeskr Laeger200216439453912380398
- OttesenMValidity of the registration and reporting of vaginal prolapse surgery [in Danish: Validitet af kodning og indberetning ved vaginal prolapskirurgi]Ugeskr Laeger2009171640440819208327
- LassPLilholtJThomsenLLundbye-ChristensenSEnevoldsenHSimonsenOHThe quality of diagnosis and procedure coding in Orthopaedic surgery Northern Jutland [in Danish: Kvaliteten af diagnose- og procedurekodning i Ortopaedkirurgi Nordjylland]Ugeskr Laeger2006168484212421517147947
- AndersenLVMortensenLSLindholtJSFaergemanOHennebergEWFrostLCompleteness and positive predictive value of registration of upper limb embolectomy in the Danish national vascular registryClin Epidemiol20091273220865084
- Blichert-HansenLNielssonMSNielsenRBChristiansenCFNørgaardMValidity of the coding for intensive care admission, mechanical ventilation, and acute dialysis in the Danish national patient registry: a short reportClin Epidemiol2013591223359787
- LundJLFrøslevTDeleuranTValidity of the Danish national registry of patients for chemotherapy reporting among colorectal cancer patients is highClin Epidemiol2013532733424039450
- NielssonMSErichsenRFrøslevTTaylorAAcquavellaJEhrensteinVPositive predictive values of the coding for bisphosphonate therapy among cancer patients in the Danish national patient registryClin Epidemiol2012423323622977313
- HaerskjoldAHenriksenLWaySThe Danish national prescription registry in studies of a biological pharmaceutical: palivizumab – validation against two external data sourcesClin Epidemiol2015730531226056490
- NielsenLHNørgaardBLTilstedHHThe Western Denmark cardiac computed tomography registry: a review and validation studyClin Epidemiol20157536425657592
- BrownLDCaiTTDasGuptaAInterval estimation for a binomial proportionStat Sci200116101117
- ErichsenRLashTLHamilton-DutoitSJBjerregaardBVybergMPedersenLExisting data sources for clinical epidemiology: the Danish national pathology registry and data bankClin Epidemiol20102515620865103
- GrannAFErichsenRNielsenAGFrøslevTThomsenRWExisting data sources for clinical epidemiology: the clinical laboratory information system (LABKA) research database at Aarhus university, DenmarkClin Epidemiol2011313313821487452
- KildemoesHWSørensenHHallasJThe Danish national prescription registryScand J Public Health2011397 Suppl384121775349
- ChristiansenCJohansenMChristensenSO’BrienJMTønnesenESørensenHPreadmission metformin use and mortality among intensive care patients with diabetes: a cohort studyCrit Care2013175R19224018017
- SchmidtMJacobsenJBLashTLBøtkerHESørensenHT25 year trends in first time hospitalisation for acute myocardial infarction, subsequent short and long term mortality, and the prognostic impact of sex and comorbidity: a Danish nationwide cohort studyBMJ2012344e35622279115
- SørensenHTMellemkjærLSteffensenFHOlsenJHNielsenGLThe risk of a diagnosis of cancer after primary deep venous thrombosis or pulmonary embolismN Engl J Med199833817116911739554856
- RoosNPWennbergJEMalenkaDJMortality and reoperation after open and transurethral resection of the prostate for benign prostatic hyperplasiaN Engl J Med198932017112011242469015
- FrostLVukelic AndersenLMortensenLSDethlefsenCSeasonal variation in stroke and stroke-associated mortality in patients with a hospital diagnosis of nonvalvular atrial fibrillation or flutter. A population-based study in DenmarkNeuroepidemiology200626422022516645321
- SchmidtMChristiansenCFMehnertFRothmanKJSørensenHTNon-steroidal anti-inflammatory drug use and risk of atrial fibrillation or flutter: population based case-control studyBMJ2011343d345021727167
- SchmidtMBøtkerHEPedersenLSørensenHTComparison of the frequency of atrial fibrillation in young obese versus young nonobese men undergoing examination for fitness for military serviceAm J Cardiol2014113582282624406109
- ChristensenAIEkholmOGlümerCThe Danish national health survey 2010. Study design and respondent characteristicsScand J Public Health201240439139722786925
- Center for Public Health and Quality Improvement, Central Denmark RegionHow Are You? Available from: http://www.cfk.rm.dk/om-cfk/projektsite/hvordan-har-du-det/om-undersogelsen/Accessed October 1, 2015
- TjønnelandAOlsenABollKStudy design, exposure variables, and socioeconomic determinants of participation in diet, cancer and health: a population-based prospective cohort study of 57,053 men and women in DenmarkScand J Public Health200735443244117786808
- MikkelsenEMHatchEEWiseLARothmanKJRiisASørensenHTCohort profile: the Danish web-based pregnancy planning study – ‘Snart-Gravid’Int J Epidemiol200938493894318782897
- OslerMLinnebergAGlümerCJørgensenTThe cohorts at the research centre for prevention and health, formerly ‘the Glostrup population studies’Int J Epidemiol201140360261020338891
- SchnohrPJensenGLangePScharlingHThe Copenhagen city heart study. Østerbroundersøgelsen: tables with data from the third examination 1991–1994Eur Heart J Suppl20013suppl HH1H83
- HjertholmPFenger-GrønMVestergaardMVariation in general practice prostate-specific antigen testing and prostate cancer outcomes: an ecological studyInt J Cancer2015136243544224905402
- ChristiansenEHJensenLOThayssenPScandinavian Orga-nization for Randomized Trials with Clinical Outcome (SORT OUT) V investigatorsBiolimus-eluting biodegradable polymer-coated stent versus durable polymer-coated sirolimus-eluting stent in unselected patients receiving percutaneous coronary intervention (SORT OUT) V: a randomised non-inferiority trialLancet2013381986766166923374649
- ThuesenLJensenLOTilstedHHEvent detection using population-based health care databases in randomized clinical trials: a novel research tool in interventional cardiologyClin Epidemiol2013535736124068874
- SlothADSchmidtMRMunkKCONDI InvestigatorsImproved long-term clinical outcomes in patients with ST-elevation myocardial infarction undergoing remote ischaemic conditioning as an adjunct to primary percutaneous coronary interventionEur Heart J201435316817524031025
- NielsenPHMaengMBuskMDANAMI-2 InvestigatorsPrimary angioplasty versus fibrinolysis in acute myocardial infarction: long-term follow-up in the Danish acute myocardial infarction 2 trialCirculation2010121131484149120308618
- JespersenCMAls-NielsenBDamgaardMCLARICOR Trial GroupRandomised placebo controlled multicentre trial to assess short term clarithromycin for patients with stable coronary heart disease: CLARICOR trialBMJ20063327532222716339220
- PedersenATLidegaardØKreinerSOttesenBHormone replacement therapy and risk of non-fatal strokeLancet19973509087127712839357407
- AndersenBSOlsenJOral contraception and factor V Leiden mutation in relation to localization of deep vein thrombosisThromb Res19989041911949692618
- Vest-HansenBRiisAHSørensenHTChristiansenCFOut-of-hours and weekend admissions to Danish medical departments: admission rates and 30-day mortality for 20 common medical conditionsBMJ Open201553e006731e006731
- ThygesenLCErsbøllAKDanish population-based registers for public health and health-related welfare researchScand J Public Health2011397 Suppl81021775344
- AndersenJSOlivariusNDFKrasnikAThe Danish national health service registerScand J Public Health2011397 Suppl343721775348
- Statistics DenmarkThe Integrated Database for Labour Market Researc [In Danish: Den Integrerede Database for Arbejdsmarkeds-forskning]201316 Available from: http://www.dst.dk/da/Statistik/Publikationer/VisPub.aspx?cid=20698Accessed April 1, 2015
- JensenVMRasmussenAWDanish education registersScand J Public Health2011397 Suppl919421775362
- BaadsgaardMQuitzauJDanish registers on personal income and transfer paymentsScand J Public Health2011397 Suppl10310521775365
- ChristensenGThe building and housing registerScand J Public Health2011397 Suppl10610821775366
- JohannesdottirSAHorvath-PuhoEEhrensteinVSchmidtMPedersenLSørensenHTExisting data sources for clinical epidemiology: the Danish national database of reimbursed prescriptionsClin Epidemiol2012430331323204870
- Helweg-LarsenKThe Danish register of causes of deathScand J Public Health2011397 Suppl262921775346
- HarvaldBHaugeGKyvikKOChristensenKSkyttheAHolmNVThe Danish twin registry: past and presentTwin Res20047431833515193163
- Databasernes fællessekretariatInformation on the Danish Clinical Registries Available from: http://www.rkkp.dk/in-english/Accessed August 1, 2015
- The Danish e-Health PortalDescription of all Danish Clinical Registries (in Danish) Available from: http://www.sundhed.dk/sundhedsfaglig/kvalitet/kliniske-kvalitetsdatabaser/Accessed August 1, 2015
- NørgaardMJensenAØEngebjergMCLong-term clinical outcomes of patients with primary chronic immune thrombocytopenia: a Danish population-based cohort studyBlood2011117133514352021263148
- AndersonIBSørensenTIPrenerAIncrease in incidence of disease due to diagnostic drift: primary liver cancer in Denmark, 1943–1985BMJ199130267744374402004170
- SchmidtMHováth-PuhóEChristiansenCFPetersenKLBøtkerHESørensenHTPreadmission use of nonaspirin nonsteroidal anti-inflammatory drugs and 30-day stroke mortalityNeurology201483222013202225378670
- ToppMLanghoff-RoosJUldallPValidation of a cerebral palsy registerJ Clin Epidemiol1997509101710239363036
- AndersenTFMadsenMLoftAValidity of surgical information from the Danish National Patient Registry with special attention to the analysis of regional variations in hysterectomy rates [in Danish: Regionale variationer i anvendelse af hysterektomi]Ugeskr Laeger198714936242024223450055
- GreenADanish clinical databases: an overviewScand J Public Health2011397 Suppl687121775356
- IngeholmPDanish National Colorectal Cancer Database. National Database for Colorectal Cancer. Annual Report 20112012
- SørensenHTLashTLRothmanKJBeyond randomized controlled trials: a critical comparison of trials with nonrandomized studiesHepatology20064451075108217058242
- PetersenKEJohnsenNFOlsenAThe combined impact of adherence to five lifestyle factors on all-cause, cancer and cardiovascular mortality: a prospective cohort study among Danish men and womenBr J Nutr2015113584985825690300
- BrunelliSMGagneJJHuybrechtsKFEstimation using all available covariate information versus a fixed look-back window for dichotomous covariatesPharmacoepidemiol Drug Saf201322554255023526818
- LidegaardØLøkkegaardEJensenASkovlundCWKeidingNThrombotic stroke and myocardial infarction with hormonal contraceptionN Engl J Med2012366242257226622693997
- SchmidtMPedersenSBFarkasDKThirteen-year nationwide trends in use of implantable cardioverter-defibrillators and subsequent long-term survivalHeart Rhythm20151292018202725937527
- CainKCHarlowSDLittleRJBias due to left truncation and left censoring in longitudinal studies of developmental and disease processesAm J Epidemiol201117391078108421422059
- AlpertJSThygesenKAntmanEBassandJPMyocardial infarction redefined – a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarctionJ Am Coll Cardiol200036395996910987628
- FeinsteinARSosinDMWellsCKThe Will Rogers phenomenon. Stage migration and new diagnostic techniques as a source of misleading statistics for survival in cancerN Engl J Med198531225160416084000199
- Danish Data Protection AgencyThe Danish Act on Processing of Personal Data Available from: http://www.datatilsynet.dk/english/the-danish-data-protection-agency/introduction-to-the-danish-data-protection-agency/Accessed February 1, 2015
- Danish Health and Medicines AuthorityForskerservice Available from: http://www.ssi.dk/Sundhedsdataogit/Forskerservice.aspxAccessed April 1, 2015
- Danish Health and Medicines AuthorityVideregivelse af patientjournal oplysninger Available from: http://sundhedsstyrelsen.dk/da/sundhed/behandling-og-rettigheder/patientjournaloplysningerAccessed April 1, 2015