Abstract
Background
The diagnosis of COPD is not always consistent with the Global Initiative for Chronic Obstructive Lung Disease (GOLD) strategy in daily clinical practice, especially in primary care. This study aimed to estimate the overall COPD prevalence and severity, to identify differences between newly and previously diagnosed patients, and to evaluate the potential COPD overtreatment in a smoking population attending a primary care spirometry surveillance program.
Methods
A study was conducted in 10 primary health care centers of Central Greece during a 7-month period. Eligible participants were aged ≥40 years and were either current smokers or exsmokers.
Results
A total of 186 subjects were included (68% males, mean age 62.3±12.6 years, mean life-time tobacco exposure 50 pack-years). COPD prevalence was 17.8%, identified to be higher in elderly males. Forty-two percent of the COPD group were newly diagnosed patients, who were of younger age, current smokers, presented with less dyspnea and better health status, and mainly appeared with mild-to-moderate disease. Interestingly, 61.4% of non-COPD and 85.7% of newly diagnosed COPD individuals had been using inhaled medication under primary care provider’s prescription without ever undergoing spirometry or further evaluation by a pulmonologist; thus, the phenomena of COPD overdiagnosis and missed diagnosis came into the spotlight. Moreover, only 26.3% of known COPD patients were properly medicated according to GOLD guidelines, while half of them were inappropriately treated with triple inhaled therapy.
Conclusion
We reported a significant prevalence of COPD in smoking population attending this spirometry program. A remarkable proportion of COPD patients were undiagnosed and made case finding worthwhile. Underutilization of spirometry in the diagnosis and management of COPD as well as general practitioners’ nonadherence to the GOLD treatment guidelines was confirmed by our data. These findings highlight the need for a major overhaul and culture change in primary care settings of Central Greece.
Introduction
COPD is a chronic respiratory disorder that currently represents a major public health concern worldwide.Citation1 It is a major cause of morbidity and mortality at international level, and it has been identified as the third leading cause of death globally.Citation2,Citation3 The hallmark of COPD is the presence of airflow obstruction that is not fully reversible, and spirometry is essential for the definite diagnosis of the disease.Citation4
Respiratory symptoms – such as cough, sputum production, and dyspnea – may precede the development of airflow limitation by many years; yet significant airflow obstruction may develop without symptoms.Citation5 Estimates of global COPD prevalence rates vary widely, most likely because of methodological differences between studies.Citation6 The prevalence of spirometry-defined COPD in adults was estimated to be 10% based on the international Burden of Obstructive Lung Diseases (BOLD) survey.Citation7 In Greece, the prevalence of COPD was estimated to range between 3.5% and 18.4%.Citation5,Citation8–Citation10
Primary care physicians (PCPs) play a crucial role in detecting and managing COPD, since they manage the vast majority of patients in the early stages of the disease.Citation4–Citation6,Citation8,Citation11,Citation12 However, the diagnosis of COPD by PCPs is not always consistent to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines in daily clinical practice, mainly because of underuse of spirometry in primary health care (PHC) settings.Citation5,Citation11,Citation13–Citation18 As a result, COPD is a disease that is largely underestimated and underdiagnosed.Citation5,Citation11 In the USA and Europe, the rate of underdiagnosis varies greatly with the highest estimates reaching up to 86%.Citation13–Citation15 Similarly, in Greece, the percentage of undiagnosed COPD patients in the PHC is really high,Citation5,Citation11,Citation16–Citation18 with the study of Spyratos et alCitation11 reporting that 52.6% of COPD cases are undiagnosed. In contrast, overdiagnosis of the disease, a rather common situation in PHC because, again, of nonuse of spirometry or insufficient training of GPs in the interpretation of pulmonary function tests (PFTs), leads to subsequent unnecessary drug overprescription that increases significantly the already high economic burden of diseaseCitation11 as shown previously.Citation19 In particular, PHC is the gateway to the health system and is expected to resolve up to 85% of health demands as well as to offer comprehensive care coordinated with the other levels of health care.Citation20
The aims of the present study were to estimate the overall prevalence and severity of COPD as well as the fraction of already diagnosed and treated COPD patients in a smoking population attending PHC settings in Central Greece, to identify differences between newly and previously diagnosed COPD patients, and to evaluate potential overtreatment in primary care COPD patients.
Methods
The study was conducted in 10 randomly selected PHC centers in urban, suburban, and rural areas in Thessaly, Central Greece, during a 7-month period (May 2016–November 2016). All subjects were aged >40 years, current smokers or exsmokers, resided near a PHC setting, and were willing to participate in a spirometry surveillance program. Exclusion criteria included no smoking history, a history of lower or upper respiratory infection or antibiotic treatment within the last month, an operative procedure or acute myocardial infarction within last 3 months, and inability to perform spirometry. The potentially eligible participants were selected and screened by PCPs (case-finding program). The study was approved by the Ethics Committee of the University Hospital of Larissa, and all subjects provided written informed consent.
Study design
A survey questionnaire was completed for each participant. The questionnaire included questions on smoking status, occupational exposure, chronic respiratory symptoms (cough, sputum, wheezing, and dyspnea), history of respiratory infections, comorbidities, and history of inhaled medication received during the last 3 years. Additionally, clinical COPD questionnaire (CCQ), COPD assessment test (CAT), and modified Medical Research Council (mMRC) dyspnea scale were completed by all participants. The CCQ was used to assess health-related quality of life (HRQoL). CAT was used to measure the impact of COPD on a person’s life and mMRC dyspnea scale to quantify how shortness of breath causes disability. Smoking status was categorized in the following two terms: 1) former smokers included adults who have smoked at least 100 cigarettes in their lifetime but who had quit smoking for at least 12 months and 2) current smokers included adults who have smoked 100 cigarettes in their lifetime and currently smoke cigarettes every day (daily) or some days (nondaily). Smoking status for all subjects was measured in pack-years of cigarette smoking (pys).
Spirometry procedure
Spirometry test was performed with a dry spirometer (Spirolab, MIR, Rome, Italy) according to American Thoracic Society (ATS) recommendations.Citation21 Calibration checks were performed every morning, before the beginning of the spirometry program. Spirometry testing was performed by physicians who had undergone a special training program. Forced expiratory maneuvers were repeated until three reproducible acceptable tests were obtained and the best. Forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), and FEV1/FVC ratio were recorded. An acceptable maneuver was defined as follows: 1) an explosive start (no hesitation or sigmoid curve) with a back-extrapolation volume <150 mL, 2) the maneuver was performed with a maximal inspiration and expiration, 3) no glottis closure or cessation of airflow occurred during the maneuver, 4) no coughs (particularly during the first second), inspirations during the trace or evidence of leaks, and 5) the maneuver met the end-of-test criteria (exhaling for ≥6 seconds with <50 mL being exhaled in the last 2 seconds).Citation22 A bronchodilator reversibility test with 400 µg of salbutamol was performed in all patients with obstructive spirometry. Obstructive spirometry was defined as an FEV1/FVC of <0.70 in accordance with GOLD guidelines.Citation23 A positive response to bronchodilators was defined as an increase in the FEV1 of 200 mL and 12% from the prebronchodilator value (baseline value).Citation24
Fractional exhaled nitric oxide (FeNO) measurement
FeNO concentration in exhaled breath was also measured for all subjects. The FeNO levels were measured using a nitric oxide analyzer (NoBreath; Bedfont Scientific Ltd, Maidstone, UK). The testing standards for FeNO followed the guidelines recommended by the ATS and the European Respiratory Society.Citation25
Diagnosis of COPD
After the completion of the study questionnaire, the measurement of FeNO, and spirometry test, all participants were evaluated by respiratory physicians who established the diagnosis of COPD. The presence of COPD was assessed based on medical history, clinical symptoms, and spirometry results. Classification of COPD was based on the postbronchodilator FEV1 (%) according to GOLD guidelines (Stage I/mild COPD, FEV1 ≥80%; Stage II/moderate COPD, 50%≤ FEV1 <80%; Stage III/severe COPD, 30%≤ FEV1 <50%; Stage IV/very severe COPD, FEV1 ≤30% or FEV1 <50% with respiratory failure).Citation23,Citation26 Patients with COPD were also allocated into four groups by GOLD (GOLD Groups A, B, C, and D) according to 2016 and 2017 GOLD guidelines.Citation23,Citation26 Additionally, for participants with known COPD, an extra questionnaire regarding COPD and exacerbation history was completed. COPD patients were also asked whether they had previously received a chest X-ray (CXR). In terms of the differentiation between COPD and asthma, asthma diagnosis was based on participants’ medical history (presence of symptoms from childhood or adolescence and/or seasonal distribution) and the presence of significant reversibility of airway obstruction on spirometry according to GINA guidelines (improvement in the FEV1 of >12% and 200 mL from the baseline spirometry).Citation27 Patients with asthma were included in the analysis as non-COPD patients.
Statistical analyses
Data were analyzed using the statistical program SPSS 22 (IBM Corporation, Armonk, NY, USA). Quantitative variables were presented as mean with standard deviation (SD), and qualitative variables are presented as frequencies with percentages. Chi-square test was used to explore any associations between qualitative variables. To identify differences between two independent groups when the dependent variable was either ordinal or continuous, unpaired t-tests or Mann–Whitney U tests were used for normally and skewed data, respectively. Differences between more than two unrelated groups were tested by one-way analysis of variance (ANOVA). A result was considered statistically significant when the P-value was <0.05.
Results
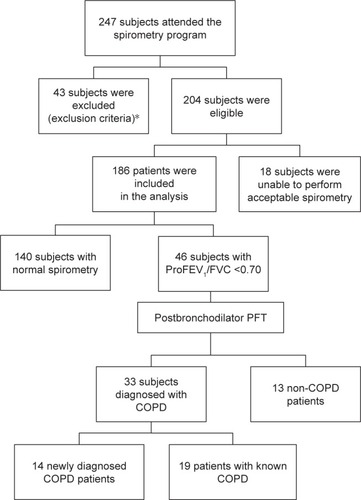
Study flowchart is presented in . At baseline, 247 subjects were enrolled and screened, but only 204 subjects fulfilled inclusion criteria. Of the 204 eligible participants, 186 participants performed an acceptable spirometry and were included in the analysis. From the subjects included, 46 individuals presented with a prebronchodilator FEV1/FVC ratio of <0.70. Thirty-three individuals had a postbronchodilator FEV1/FVC of <70% and diagnosed with COPD. The rest of the 13 subjects were either diagnosed with asthma or in cases with a response that improved postbronchodilator FEV1/FVC >70% but did not meet the spirometric and/or clinical criteria for asthma diagnosis, referral for further specialized investigations was recommendedCitation26 (further evaluation of asthma–COPD overlap). This group was included in the analysis as non-COPD patients.
Figure 1 Flowchart of the study selection process.
Abbreviation: PFT, pulmonary function test.
The demographic and clinical characteristics of 186 subjects enrolled into the study are presented in . Of the 186 subjects, 68.3% of them were males with a mean age of 62.3±12.6 years. At least one comorbid condition was reported in 82% of the sample, with the most common being arterial hypertension (44.6%); 82.3% had at least one respiratory symptom (dyspnea, cough, sputum, and/or wheezing); and 67.2% of all participants reported that they had been medicated with inhalers for different time periods during the last 3 years, with the combination of LABA/inhaled corticosteroid (ICS) being the most prescribed treatment (24.2%).
Table 1 Demographic and clinical characteristics of study participants (N=186)
Of the 186 subjects, 121 (65.1%) subjects were current smokers and 65 (34.9%) subjects were exsmokers. The mean estimated life-time tobacco exposure was 59±48 pys for exsmokers and 45±30 pys for active smokers (P=0.142). A male predominance was detected in both groups (81.5% in exsmokers vs 61.2% in active smokers, P=0.004). Furthermore, exsmokers were older than active smokers (68.83±12.44 vs 58.83±11.26 years, respectively, P<0.001). Exsmokers reported significant dyspnea (mMRC ≥2) compared to current smokers (30.8 vs 17.4%, respectively, P=0.035) with no differences in the prevalence of other respiratory symptoms (cough, sputum, and wheezing). Both groups had a high rate of cardiac comorbidities. However, exsmokers had more cardiac comorbidities as compared to active smokers (81.5 vs 62%, respectively, P=0.006), especially suffered from coronary heart disease (75.4 vs 53.7%, P=0.007) and arterial hypertension (56.9 vs 38%, P=0.013). Exsmokers had lower proFEV1 values as compared to current smokers (2,192±958 vs 2,558±750 mL, P=0.005), as well as lower FEV1/FVC ratio (63.82±22.89 vs 78.04±18.96, P=0.027). No differences were detected in FeNO values (P=0.228) or reversibility (P=0.743) between two groups.
COPD was diagnosed in 33 of the 186 participants providing a COPD prevalence of 17.8% in the study population. COPD group was constituted of 57.6% (19/33) exsmokers and 42.4% (14/33) active smokers. COPD diagnosis was associated with older age (71±10.3 vs 60.5±12.3 years, P<0.001), male predominance (93.9 vs 62.7%, P<0.001), higher CAT (10.5±7.6 vs 6.7±6.9, P=0.003), and mMRC scores (P=0.002) as well as sputum production (P=0.008). Furthermore, the mean FeNO value was significantly higher in the COPD group compared to that in the non-COPD group (11.68±13.76 vs 7.25±7.82 ppb, P=0.019). In , comparisons of demographic and clinical characteristics of COPD vs non-COPD groups are presented.
Table 2 Comparisons of COPD and non-COPD groups
Newly diagnosed COPD patients represented 42.4% of the COPD group. Newly diagnosed patients were younger (66±10 vs 75±9 years, P=0.009), predominantly current smokers (64.3 vs 35.7%, P=0.029), presented with lower mMRC scores (mMRC ≥2: 21.4 vs 57.9%, P=0.036) compared to the known COPD individuals. Moreover, they had lower total and functional CCQ scores (P=0.033 and 0.013, respectively). One of the five (3/14) newly diagnosed COPD groups included asymptomatic smokers, representing 1.6% of the study participants. Known COPD patients represented 57.6% of COPD group (19/33). Comparisons of demographic and clinical characteristics between newly diagnosed and known COPD patients are presented in .
Table 3 Comparisons of newly diagnosed and known COPD patients
COPD patients were asked whether they had ever undergone chest imaging by general practitioners (GPs). In known COPD patients, CXRs were previously performed on 60% of them, mainly for ruling out alternative diagnoses and comorbid conditions. Regarding newly diagnosed COPD patients, none of them had ever undergone a spirometry and 40% of them had a CXR previously performed.
Moreover, 93.9% of all COPD individuals reported that they had received inhaled medication over the last 3 years. Notably, 61% of healthy individuals and 85.7% of newly diagnosed patients reported that they had been medicated with inhalers for various time periods under the guidance of GPs. None of them was referred for further diagnostic assessment by a specialist or spirometry testing according to patients’ self-reports.
The majority of COPD patients were classified into risk groups A and B. Depending on GOLD system, a rise in the proportion of COPD patients classified in groups A and B was observed (from 75.8% according to 2016 GOLDCitation23 classification to 84.8% according to the latest established classificationCitation26) as presented in . Furthermore, 85.7% of newly diagnosed patients were in the mild-to-moderate stage of disease and were classified into Stages I and II. Similarly, we observed an increasing proportion of early-stage newly diagnosed COPD patients when they were reclassified according to 2017 GOLD system (from 85.7% to 92.8% according to old and new GOLD guidelines,Citation23,Citation26 respectively) (). Moreover, differences in treatment compliance according to GOLD group were observed. Specifically, we found that only 47.4% of known COPD patients received proper medication according to 2016 GOLD guidelinesCitation23 and only 26.3% of known COPD patients received proper medication according to latest treatment guidelines.Citation26 Overall, 68.4% of known COPD patients were medicated with ICSs and approximately half of them were being inappropriately treated with triple inhaled therapy ().
To this end, summarizes demographics and clinical characteristics of all COPD patients according to different GOLD stages (I–IV) and different GOLD groups (A–D). We found that COPD patients in GOLD Stage III/IV had significantly higher total CCQ score than early-stage patients, as expected. Finally, taking into account GOLD grouping according to 2016Citation23 and 2017Citation26 GOLD definition, we found that Groups B and D had more dyspnea and higher mMRC, CAT, and total CCQ scores compared to Groups A and C, as also expected (). It is worth mentioning that none of the subjects was allocated to 2017 GOLD Group C. This is in accordance to 2017 GOLD update,Citation26 which reported that Group C is consistently the least prevalent group.
Table 4 Demographics and clinical characteristics of all COPD patients according to different GOLD stages (I–IV) and different 2017 GOLD COPD groups (A–D)
Discussion
The prevalence of COPD among smokers aged 40 years or older, attending this surveillance program, was 17.8%. Only one-half of COPD patients had already been diagnosed and treated; thus, underdiagnosis and missed diagnosis of COPD patients are a concern. We found that newly diagnosed COPD patients were of younger age, current smokers, and less symptomatic; the majority appeared to have COPD of mild and moderate airflow limitation. Remarkably, gaps seem to exist in the implementation of evidence-based guidelines for managing COPD in PHC. First, the phenomenon of COPD overdiagnosis followed by overtreatment came into spotlight, since 61.4% of non-COPD subjects were probably misdiagnosed with COPD and medicated without ever performing spirometry to confirm the diagnosis. Furthermore, a great proportion of newly diagnosed COPD patients (85.7%) had been using inhaled medication under PCPs’ prescription without ever undergoing spirometry. Finally, more convincingly, we found that only 26.3% of previously known COPD patients were properly medicated according to 2017 GOLD treatment guidelines, while half of them were inappropriately treated with triple inhaled therapy.
Generally, smoking population participated in this PHC spirometry surveillance program viewed mainly the profile of a male current smoker. The male predominance may be explained by the low smoking habit of females in Greece,Citation9,Citation28 especially in rural and suburban areas.Citation5 Gender-related differences do also exist in COPD patients in Greece. A study conducted in Thessaly (Central Greece) reported that females comprised only 12.5% of COPD patients.Citation5
In addition, in this study, different clinical profile was detected among current smokers and exsmokers. Current smokers were younger than exsmokers, which is consistent to published data.Citation29,Citation30 However, quitters had higher mean estimated life-time tobacco exposure and reported significantly more dyspnea (mMRC ≥2) and cardiac comorbidities, especially coronary heart disease and arterial hypertension, compared to active smokers. There is abundant evidence that respiratory effects and health sequences associated with cigarette smoke increase motivation to quit smoking.Citation31 Furthermore, it has previously been described that smoking-associated symptoms such as sputum production and dyspnea might not be completely reversible.Citation32
Notably, approximately two-thirds (67.2%) of all study participants reported that they had been treated with inhaled medication over the last 3 years – especially LABA/ICS combination – without ever undergoing PFTs or further evaluation by a pulmonologist. Spyratos et alCitation11 consistently documented that GPs prescribe drugs based on patients’ symptoms, clinical examination, and smoking history without using spirometry for the confirmation of the respiratory disease. Without COPD determination and proper classification, GPs blindly treat an obstructive pulmonary disease, usually by the prescription of LABA/ICS, in order to “cover” all COPD stages or bronchial asthma.Citation11 Moreover, our findings are in agreement with those observed in another Greek study, reporting that LABA/ICS combination was the most frequent medication prescribed, followed by LAMA.Citation33
Further analysis of various types of drugs used showed that approximately half of the study participants were medicated with inhalers, while the prevalence of COPD in this particular population was 17.8%. Hence, we can speculate that patients may be too often misdiagnosed with COPD and then overtreated. However, we were not able to reliably verify the accuracy of participants’ self-reported diagnoses. It is worth mentioning in this context that 55.4% of the current costs for COPD medication were found to be wasted to overdiagnosis and overtreatment in Greece.Citation11
In this article, we reported a significant proportion of COPD patients being diagnosed by the implementation of a PHC-based spirometry program. The reported COPD prevalence rate of our study was obviously limited by a small sample size; however, it is comparable to that found in previously published larger studies.Citation5,Citation9,Citation11 In detail, Spyratos et alCitation11 reported a COPD prevalence of 10.7% in PHC, and Minas et alCitation5 found a prevalence of 18.4% in PHC settings of Thessaly (Central Greece) – in a study conducted before the Greek crisis onset (from January 2006 to June 2007), and included 15 PHC centers in Central Greece. Similarly, in the study of Tzanakis et al,Citation9 COPD prevalence was recorded to be 15.1% in males living in rural areas.
Specifically, we found a remarkable proportion of newly diagnosed patients, yet COPD remains grossly undiagnosed in PHC by GPs. The large proportion of undiagnosed COPD cases in a PHC is a silent scourge.Citation4,Citation5,Citation11,Citation16 Herein, however, the rate of newly diagnosed COPD cases observed was lower than previously reported at PHC level, even though only high-risk smokers were screened. Specifically, two-fifths (42.4%) of COPD patients were classified as newly diagnosed, in comparison with two other studiesCitation8,Citation11 that reported higher proportions of newly diagnosed COPD patients (69% and 52.6%, respectively).Citation8,Citation11 Crucially, in support of our strategy, offering spirometry to subjects with tobacco/occupational exposure and at least one respiratory symptom was found to be a very effective screening strategy as more than one-third of participants with airway obstruction could be detected.Citation34,Citation35 Other studies indicated that in those with risk factors such as >20 pack-years of smoking, the diagnostic yield for COPD is relatively high and spirometry should be considered as a method of early case finding.Citation35,Citation36 Screening in high-risk smoking groups is also supported by GOLD 2017 guidelines.Citation26
Regarding further evaluation of known COPD, we found that CXR is a diagnostic tool for GP, which is mostly used in cases of established COPD. Generally, it has been reported that GPs tend to perform more CXRs than PFTs. Nonetheless, according to established guidelines, CXR is only valuable in excluding alternative diagnoses or identifying significant comorbidities,Citation26 as it is usually abnormal in patients with severe COPD but may not show changes in up to one-half of patients with mild and moderate COPD.Citation37,Citation38
We documented high proportions of undiagnosed patients with COPD in the early stages of the disease, which is in accordance with previous studies.Citation39–Citation41 Moreover, in our study, we found that newly diagnosed COPD patients were of younger age, current smokers, and presented with fewer symptoms. These findings are consistent with previously published data too.Citation5
Although current clinical practice guidelines recommend against screening for COPD in asymptomatic individuals,Citation23,Citation42,Citation43 there are several studies that have revealed a high prevalence of COPD among smokers with minimal or no symptoms.Citation44 In our study, the group of asymptomatic smokers with COPD represented 1.6% of the study participants and 21% of those who had COPD. These findings are in accordance with a previous studyCitation37 showing that the prevalence of COPD in asymptomatic smokers has been 1.5% when considering the whole group of smokers and 7% when considering the group of nonsymptomatic smokers.Citation44
It is well established that COPD is most prevalent in older adults and males with more comorbidities which is also in accordance with our results.Citation24,Citation45–Citation49 A previous study from our group found that 87.7% of COPD patients report at least one comorbid condition.Citation19 FeNO levels in COPD are conflictual, but it seems that smoking habits and disease severity are the most important factors influencing FeNO levels in COPD patients.Citation50,Citation51 However, we found no significant difference in FeNO levels between ex- and current smokers or between COPD and non-COPD individuals in contradiction to previous studies.Citation50,Citation51
Finally, differences in treatment compliance according to stage of COPD were observed according to 2016 GOLD guidelines,Citation23 a phenomenon was emphasized more taking into account the most recently published GOLD guidelines.Citation26 In other words, COPD patients in GOLD Grades A and B were frequently overtreated according to both versions of GOLD guidelines. Analogous results were obtained by Papala et alCitation52 who identified an overtreatment in all GOLD grades. Spyratos et alCitation11 also previously reported that only 45% of the subjects were treated according to GOLD guidelines in PHC and 53.1% of the cases were overtreated. As far as corticosteroid use is concerned, we found that approximately half of the known COPD patients were inappropriately treated with triple inhaled therapy. ICS use in early stages of disease was also documented in the study of Tzovaras et al.Citation53
Achieving the optimal management of COPD in PHC is a major challenge. Taken together, our findings strongly suggest that GPs usually prescribe treatment without the use of spirometry and/or without taking into account the severity of airway obstruction. The limited access to spirometry in PHC in Greece remains strongly evident.Citation5 Other causes of COPD misdiagnosis are as follows:Citation54 1) due to the threshold of 0.70 used for defining COPD, leading to underdiagnosis in younger patients and overdiagnosis in older patients;Citation54 2) errors made in PHC due to GP’s lack of awareness of COPD;Citation54–Citation59 3) errors linked to the spirometry test such as technological errors;Citation54,Citation59–Citation61 4) differential diagnoses, which causes diagnostic confusion; and finally 5) patient-related factors such as the absence of obvious respiratory symptoms.Citation54,Citation62 Given the underdiagnosis and no refreshment in PHC, both highlighted by our study, in combination with the absence of obvious respiratory symptoms, COPD is often established at a late stage. Thus, symptomatic patients may be referred to a specialist only in severe cases, which is associated with increased COPD disease burden, comorbidities, and costs. Interestingly, it has been reported that opportunities to diagnose COPD earlier are missed for 85% of patients during the 5-year period preceding actual diagnosis.Citation63 To facilitate implementation of the guidelines, several actions are needed, such as additional resources, further training for professionals, and improved organizational structure for interprofessional collaboration and patient education.Citation64
Regarding limited resources, the medical supply short-ages reflect the unfolding humanitarian crisis of the country.Citation65 A study conducted at the beginning of economic recession revealed major shortages in rural PHC equipment as only 4.6% of rural doctors had spirometers available for clinical use.Citation66 Consequently, the treatment begins without formal assessment of lung function; the diagnosis is therefore unconfirmed. In fact, spirometry changed the physician’s clinical impressions and treatments for approximately one-third of cases.Citation20,Citation67–Citation69 Another major point is that Greece presents high variability in the distribution of pulmonologists, and therefore, significantly different rates may be observed among regions independently of population risk factors.Citation70 Many PHCs are located in the remote areas where access to specialists is limited. Patients living in these areas are usually of old age, and transportation is difficult for them; thus, GPs depend on their experience to diagnose COPD.Citation65,Citation70
Moreover, in PHC settings of Greece, there is a lack of training and feedback for diagnostic spirometry by GPs, and both constitute major barriers to its use.Citation11 Despite numerous guidelines for COPD management, studies conducted both in Greece and globally have consistently shown underutilization of spirometry in COPD diagnosisCitation71–Citation75 and deviations from optimal pharmacological treatment. In other words, gaps exist in the implementation and uptake of evidence-based guidelines for managing COPD in PHC.Citation76 Providing a theory-driven and evidenced-based COPD intervention is a research and a clinical practice priority. Raising awareness of COPD among PCPs requires a two-pronged approach: education and empowerment.Citation77 Effective forms of continuing medical education (CME) and questionnaires about the treatment and diagnosis guidelines are important tools to improve guideline adherence and implementation.Citation78
Additionally, PCPs play a central role in the multidisciplinary team involved in the diagnosis and treatment of patients with COPD. They play a key role to persuade community members to seek medical care from specialists alerting them to the risk factors and symptoms that they should recognize, in order to seek medical attention at an earlier stage in the disease process.Citation77–Citation79 Better valuing of preventative medicine will help increase the motivation and effectiveness of PHC. Screening and case-finding strategies as well as validated questionnaires in identified casesCitation80 are the tools in achieving the goal of early diagnosis in COPD.Citation26
Access to care and continuity of care are essential for improved quality and greater treatment efficiency to be achieved;Citation81 however, their implementation in the context of management of major diseases, such as COPD, diabetes mellitus, and coronary heart disease, is a matter of continual scholarly debate. Barriers to health care access emerged as one of the main negative consequences of austerity in Greece, as the proportion of Greek adults who reported unmet health care needs more than doubled in just 5 years, with 12.2% of the respondents citing cost as the main reason for not receiving proper treatment or diagnostic tests.Citation82–Citation84
Our study presents several limitations. First, the research was limited by a small sample size. Even though we aimed to have a larger sample size, the actual response rate was much lower. The use of a larger sample would improve future studies. Second, a significant limitation of our study lies in the subject selection based on the population attending PHCs. Current smokers and subjects with respiratory symptoms were more likely to attend PHC. Moreover, the enrolled subjects were selected mainly by local GPs; therefore, younger and/or asymptomatic smokers were not easily recruited for the study. These limitations may have influenced the reported prevalence of COPD in our population. Moreover, we aimed mainly at smokers of rural and suburban areas. This may further account for the higher number of male participants, since they represent the vast proportion of smokers in rural and suburban areas of Greece. Therefore, these limitations limit the generalizability of our findings to the general Greek population.
Conclusion
Our study reported a significant prevalence of COPD in 10 PHC settings in Central Greece and emphasized the crucial role of presymptomatic control in PHC. A remarkable proportion of COPD patients were undiagnosed and made case finding worthwhile. The phenomenon of missed diagnosis and overtreatment in certain individuals also came into spotlight. Moreover, appropriate COPD treatment should be a part of current health care agenda. The majority of our findings match perfectly with the global estimations and observations of previous Greek studies, indicating that no refreshment in primary care is a scourge at general practice. Undoubtedly, COPD affects Greeks with significant economic impact, which profoundly deteriorated by persistent errors in COPD management. Higher index of suspicion for the presence of COPD in high-risk smoking groups, wider use of spirometry, and PCPs’ CME should be a priority in order to tackle the scourge of COPD in primary care.
Author contributions
ES, OSK, KD, and KIG were involved in the acquisition of data and drafting of the manuscript. OSK especially participated in drafting the article and revising it critically for important intellectual content. All authors read and approved the final manuscript. This article has not been presented or published elsewhere.
Acknowledgments
The authors wish to thank the following respiratory physicians for their active participation in the spirometry program: Zoe Daniil, Irini Gerogianni, Theodora Kerenidi, Eleni Karetsi, Andreas Dimoulis, Ilias Karametos, Foteini Malli, Aggeliki Psatha, Foteini Bardaka, Layla Sicha, Charalabos Varsamas, Stylianos Boutlas, and Spyridon Ladias. The authors especially thank the following PCPs for their cooperation and the identification of high-risk individuals: Iliana Kerani, Dimitrios Kanatas, Vasileios Xamos, Vasileios Delezos, Violeta Roka, Maria Papala, Vasileios Gizlis, Fani Sarigianni, and Ioannis Antonopoulos.
Disclosure
The authors report no conflicts of interest in this work.
References
- Dal NegroRWTognellaSTosattoRDionisiMTurcoPDonnerCFCosts of chronic obstructive pulmonary disease (COPD) in Italy: the SIRIO study (social impact of respiratory integrated outcomes)Respir Med200810219210117881206
- Dal NegroRWBonadimanLTurcoPTognellaSIannazzoSCosts of illness analysis in Italian patients with chronic obstructive pulmonary disease (COPD): an updateClinicoecon Outcomes Res2015715315925834458
- LozanoRNaghaviMForemanKGlobal and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010Lancet201238098592095212823245604
- KonstantikakiVKostikasKMinasMComparison of a network of primary care physicians and an open spirometry programme for COPD diagnosisRespir Med2011105227428120663655
- MinasMHatzoglouCKaretsiECOPD prevalence and the differences between newly and previously diagnosed COPD patients in a spirometry programPrim Care Respir J201019436337020532466
- WelteTVogelmeierCPapiACOPD: early diagnosis and treatment to slow disease progressionInt J Clin Pract201569333634925363328
- BuistASVollmerWMMcBurnieMAWorldwide burden of COPD in high- and low-income countries. Part I. The burden of obstructive lung disease (BOLD) initiativeInt J Tuberc Lung Dis200812770370818544191
- MinasMKoukosiasNZintzarasEKostikasKGourgoulianisKIPrevalence of chronic diseases and morbidity in primary health care in central Greece: an epidemiological studyBMC Health Serv Res20101025220799979
- TzanakisNAnagnostopoulouUFiladitakiVChristakiPSiafakasNPrevalence of COPD in GreeceChest2004125389290015006947
- SichletidisLTsiotsiosIGavriilidisAPrevalence of chronic obstructive pulmonary disease and rhinitis in northern GreeceRespiration200572327027715942296
- SpyratosDChlorosDMichalopoulouDSichletidisLEstimating the extent and economic impact of under and overdiagnosis of chronic obstructive pulmonary disease in primary careChron Respir Dis201613324024626965221
- SpyratosDChlorosDSichletidisLDiagnosis of chronic obstructive pulmonary disease in the primary care settingHippokratia2012161172223930052
- PeñaVSMiravitllesMGabrielRGeographic variations in prevalence and under diagnosis of COPD: results of the IBERPOC multicentre epidemiological studyChest2000118498198911035667
- RudolfMThe reality of drug use in COPD: the European perspectiveChest20001172 Suppl29S32S10673471
- StangPLydickESilbermanCKempelAKeatingETThe prevalence of COPD: using smoking rates to estimate disease frequency in the general populationChest20001175 Suppl 2354S359S10843976
- KotrogianniFMalliFGourgoulianisKIUnderdiagnosis of respiratory diseases during an economic downturn and the need for spirometry as a screening testJ Bras Pneumol201339225425523670515
- AlexopoulosECMalliFMitsikiEBaniaEGVarounisCGourgoulianisKIFrequency and risk factors of COPD exacerbations and hospitalizations: a nationwide study in Greece (Greek Obstructive Lung Disease Epidemiology and health ecoNomics: GOLDEN study)Int J Chron Obstruct Pulmon Dis2015102665267426715845
- MinasMVerrou-KatsarouIMystridouPApostolidouEHatzoglouCGourgoulianisKITwo-year mortality of patients with COPD in primary health care: an observational studyInt J Gen Med2012581582223055771
- StafylaEKerenidiTGerogianniIGeitonaMDaniilZGourgoulianisKIThe pharmacological cost of COPD during Greek economic crisisInt J Chron Obstruct Pulmon Dis20171246146628203069
- PartridgeMREnhancing the diagnosis and management of COPD in primary careMultidiscip Respir Med2014916225516797
- American Thoracic SocietyStandardization of spirometry, 1994 updateAm J Respir Crit Care Med19951523110711367663792
- MooreVCSpirometry: step by stepBreathe20128232240
- The Global Initiative for Chronic Obstructive Lung Disease (GOLD) [homepage on the Internet]Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease (updated 2016) Available from: http://www.goldcopd.org/Accessed May 23, 2017
- Global Initiative for Asthma [homepage on the Internet]Pocket guide of asthma management and preventionA pocket guide for health professionals – updated 2017 Available from: http://ginasthma.org/Accessed May 23, 2017
- American Thoracic Society; European Respiratory SocietyATS/ERS recommendations for standardized procedures for the online and offline measurement of exhaled lower respiratory nitric oxide and nasal nitric oxide, 2005Am J Respir Crit Care Med2005171891293015817806
- The Global Initiative for Chronic Obstructive Lung Disease (GOLD) [homepage on the Internet]Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease (2017 report) Available from: http://www.goldcopd.org/Accessed July 10, 2017
- KarachaliouFKostikasKPastakaCBagiatisVGourgoulianisKIPrevalence of sleep-related symptoms in a primary care population – their relation to asthma and COPDPrim Care Resp J2007164222228
- PapaioannouAIBaniaEAlexopoulosECMitsikiEMalliFGourgoulianisKISex discrepancies in COPD patients and burden of the disease in females: a nationwide study in Greece (greek obstructive lung disease epidemiology and health ecoNomics: GOLDEN study)Int J Chron Obstruct Pulmon Dis2014920321324600217
- NozawaDFrankenRARibeiro KdeCPereiraACSprovieriSRGolinVComparative study of smokers, ex-smokers, and nonsmokers who have experienced myocardial infarctionArq Bras Cardiol200381658959114963608
- SahgerDCercekBCannonCPHow do smokers differ from non smokers in their response to trombolisis (The TIMI-4 trial)Am J Cardiol1995752322367832129
- CaponnettoPPolosaRCommon predictors of smoking cessation in clinical practiceRespir Med200810281182119218586479
- RushDChanges in respiratory symptoms related to smoking in a teenage population: the results of two linked surveys separated by one yearInt J Epidemiol197652173178955767
- SouliotisKKaniCPapageorgiouMLionisDGourgoulianisKUsing big data to assess prescribing patterns in greece: the case of chronic obstructive pulmonary diseasePLoS One2016115e015496027191724
- UlrikCSLøkkeADahlRTOP study group: early detection of COPD in general practiceInt J Chron Obstruct Pulmon Dis2011612312721407825
- HillKGoldsteinRSGuyattGHPrevalence and underdiagnosis of chronic obstructive pulmonary disease among patients at risk in primary careCMAJ2010182767367820371646
- López VarelaMVMontes de OcaMReyAPUMA TeamDevelopment of a simple screening tool for opportunistic COPD case finding in primary care in Latin America: the PUMA studyRespirology20162171227123427319305
- MullerNLCoxsonHChronic obstructive pulmonary disease. 4: imaging the lungs in patients with chronic obstructive pulmonary diseaseThorax20025798298512403883
- DewarMCurryRWChronic obstructive pulmonary disease: diagnostic considerationsAm Fam Physician200673466967616506711
- VandevoordeJVerbanckSGijsselsLEarly detection of COPD: a case finding study in general practiceRespir Med2007101352553016908127
- BednarekMMaciejewskiJWozniakMKucaPZielinskiJPrevalence, severity and underdiagnosis of COPD in the primary care settingThorax20086340240718234906
- LlordésMJaénAAlmagroPPrevalence, risk factors and diagnostic accuracy of COPD among smokers in primary careCOPD201512440441225474184
- Guirguis-BlakeJMSengerCAWebberEMMularskiRAWhitlockEPScreening for chronic obstructive pulmonary disease: evidence report and systematic review for the US Preventive Services Task ForceJAMA2016315131378139327046366
- QaseemAWiltTJWeinbergerSEAmerican College of Physicians; American College of Chest Physicians; American Thoracic Society; European Respiratory SocietyDiagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory SocietyAnn Intern Med2011155317919121810710
- SansoresRHVelázquez-UncalMPérez-BautistaOLVillalba-CalocaJFalfán-ValenciaRRamírez-VenegasALPrevalence of chronic obstructive pulmonary disease in asymptomatic smokersIntern J COPD201520151023572363
- WaatevikMSkorgeTDOmenaasEBakkePSGulsvikAJohannessenAIncreased prevalence of chronic obstructive pulmonary disease in a general populationRespir Med201310771037104523680166
- SharifiHMasjediMREmamiHInterim report from burden of obstructive lung disease (BOLD Study) in Tehran: prevalence and risk factors of chronic obstructive pulmonary diseaseTanaffos2014133613
- HalldinCNDoneyBCHnizdoEChanges in prevalence of chronic obstructive pulmonary disease and asthma in the US population and associated risk factorsChron Respir Dis2015121476025540134
- LandisSHMuellerovaHManninoDMContinuing to confront COPD international patient survey: methods, COPD prevalence, and disease burden in 2012–2013Int J Chron Obstruct Pulmon Dis2014959761124944511
- AdeloyeDBasquillCPapanaAChanKYRudanICampbellHAn estimate of the prevalence of COPD in Africa: a systematic analysisCOPD2015121718124946179
- SterkPJde GouwHWRicciardoloFLRabeKFExhaled nitric oxide in COPD: glancing through a smoke screenThorax199954756556710377197
- MalerbaMRadaeliAOliviniAExhaled nitric oxide as a biomarker in COPD and related comorbiditiesBiomed Res Int2014201427191824719850
- PapalaMKerenidiNGourgoulianisKIEveryday clinical practice and its relationship to 2010 and 2011 GOLD guideline recommendations for the management of COPDPrim Care Respir J201322336236423989678
- TzovarasNZKouloumentaVNGourgoulianisKIThe economic impact of late detection of COPD in general practiceChest2005127141241315654012
- HangaardSHelleTNielsenCHejlesenOKCauses of misdiagnosis of chronic obstructive pulmonary disease: a systematic scoping reviewRespir Med2017129638428732838
- AkhtarRWilsonAA comparison of spirometry in general practice and a pulmonary function laboratoryPrim Care Respir J200514421522016701728
- AlbersMSchermerTMolemaJDo family physicians’ records fit guideline diagnosed COPD?Fam Pract2009262818719228813
- StrongMGreenAGoyderEAccuracy of diagnosis and classification of COPD in primary and specialist nurse-led respiratory care in Rotherham, UK: a cross-sectional studyPrim Care Respir J2014231677324477772
- LucasAESmeenkFJSmeeleIJvan SchayckOPDiagnostic accuracy of primary care asthma/COPD working hypotheses, a real life studyRespir Med201210681158116322682550
- WaltersJAHansenECJohnsDPBlizzardELWaltersEHWood-BakerRA mixed methods study to compare models of spirometry delivery in primary care for patients at risk of COPDThorax200863540841418024537
- BoltonCEIonescuAAEdwardsPHFaulknerTAEdwardsSMShaleDJAttaining a correct diagnosis of COPD in general practiceRespir Med200599449350015763457
- EnrightPLShould we keep pushing for a spirometer in every doctor’s office?Respir Care201257114615322222133
- AkamatsuKYamagataTKidaYTanakaHUedaHIchinoseMPoor sensitivity of symptoms in early detection of COPDCOPD20085526927318972274
- van WeelCTowards earlier diagnosis of COPDLancet Respir Med20142424824924717614
- LundellSTistadMRehnBWiklundMHolmnerÅWadellKBuilding COPD care on shaky ground: a mixed methods study from Swedish primary care professional perspectiveBMC Health Serv Res201717146728693473
- RachiotisGKourousisCKamilarakiMSymvoulakisEKDouniasGHadjichristodoulouCMedical supplies shortages and burnout among greek health care workers during economic crisis: a pilot StudyInt J Med Sci201411544244724688306
- OikonomidouEAnastasiouFDervasDRural primary care in Greece: working under limited resourcesInt J Qual Heal Care2010224333337
- JoseBPCamargosPACruz FilhoAACorrea RdeADiagnostic accuracy of respiratory diseases in primary health unitsRev Assoc Med Bras201460659961225650863
- MapelDWDalalAAJohnsonPBeckerLHunterAGA clinical study of COPD severity assessment by primary care physicians and their patients as compared to spirometryAm J Med2015128662963725595469
- CelliBRRecommendations for the early diagnosis of COPD: the AIMAR viewMultidiscip Respir Med2015101625729573
- MitsikiEBaniaEVarounisCGourgoulianisKIAlexopoulosECCharacteristics of prevalent and new COPD cases in Greece: the GOLDEN studyInt J Chron Obstruct Pulmon Dis2015101371138226229456
- DavisKJLandisSHOhYMContinuing to Confront COPD International Physician Survey: physician knowledge and application of COPD management guidelines in 12 countriesInt J Chron Obstruct Pulmon Dis201510395525565799
- BourbeauJSebaldtRJDayAPractice patterns in the management of chronic obstructive pulmonary disease in primary practice: the CAGE studyCan Respir J2008151131918292848
- GlaabTVogelmeierCHellmannABuhlRGuideline-based survey of outpatient COPD management by pulmonary specialists in GermanyInt J Chron Obstruct Pulmon Dis2012710110822371651
- HernandezPBalterMSBourbeauJChanCKMarciniukDDWalkerSLCanadian practice assessment in chronic obstructive pulmonary disease: respiratory specialist physician perception versus patient realityCan Respir J20132029710523616966
- PriceDWestDBrusselleGManagement of COPD in the UK primary-care setting: an analysis of real-life prescribing patternsInt J Chron Obstruct Pulmon Dis2014988990425210450
- LiangJAbramsonMJZwarNInterdisciplinary model of care (RADICALS) for early detection and management of chronic obstructive pulmonary disease (COPD) in Australian primary care: study protocol for a cluster randomised controlled trialBMJ Open201779e016985
- VoelkelNFRaising awareness of COPD in primary careChest20001175 Suppl 2372S375S10843979
- SandelowskyHKrakauIModinSStällbergBNagerACase method in COPD education for primary care physicians: study protocol for a cluster randomised controlled trialTrials20171819728449709
- MulvaleGEmbrettMRazaviSD“Gearing Up” to improve interprofessional collaboration in primary care: a systematic review and conceptual frameworkBMC Fam Pract2016178327440181
- SpyratosDHaidichABChlorosDMichalopoulouDSichletidisLComparison of three screening questionnaires for chronic obstructive pulmonary disease in the primary careRespiration2017932838928052294
- KoponenAMSimonsenNSuominenSQuality of primary health care and autonomous motivation for effective diabetes self-management among patients with type 2 diabetesHealth Psychol Open201741205510291770718128567300
- KyriopoulosIIZavrasDSkroumpelosAMylonaKAthanasakisKKyriopoulosJBarriers in access to healthcare services for chronic patients in times of austerity: an empirical approach in GreeceInt J Equity Healt20141354
- ZavrasDZavrasAIKyriopoulosIIKyriopoulosJEconomic crisis, austerity and unmet healthcare needs: the case of GreeceBMC Health Serv Res20161630927460938
- FilippidisFTGerovasiliVMillettCTountasYMedium-term impact of the economic crisis on mortality, health-related behaviours and access to healthcare in GreeceSci Rep201774642328393903

