Abstract
Background
Few studies have examined changes in the pain experience of patients with COPD and predictors of pain in these patients.
Objectives
The objectives of the study were to examine whether distinct groups of COPD patients could be identified based on changes in the occurrence and severity of pain over 12 months and to evaluate whether these groups differed on demographic, clinical, and pain characteristics, and health-related quality of life (HRQoL).
Patients and methods
A longitudinal study of 267 COPD patients with very severe COPD was conducted. Their mean age was 63 years, and 53% were females. The patients completed questionnaires including demographic and clinical variables, the Brief Pain Inventory, and the St Georges Respiratory Questionnaire at enrollment, and 3, 6, 9, and 12 months follow-up. In addition, spirometry and the 6 Minute Walk Test were performed. Latent class analysis was used to identify subgroups of patients with distinct pain profiles based on pain occurrence and worst pain severity.
Results
Most of the patients (77%) reported pain occurrence over 12 months. Of these, 48% were in the “high probability of pain” group, while 29% were in the “moderate probability of pain” group. For the worst pain severity, 37% were in the “moderate pain” and 39% were in the “mild pain” groups. Females and those with higher body mass index, higher number of comorbidities, and less education were in the pain groups. Patients in the higher pain groups reported higher pain interference scores, higher number of pain locations, and more respiratory symptoms. Few differences in HRQoL were found between the groups except for the symptom subscale.
Conclusion
Patients with COPD warrant comprehensive pain management. Clinicians may use this information to identify those who are at higher risk for persistent pain.
Introduction
Pain is a common symptom in patients with COPD, but there is a high variation in the estimates of both the occurrence and the severity of pain in individuals with COPD.Citation1–Citation5 Across two studies,Citation1,Citation6 the occurrence of pain ranged from 34% to 53% in patients with moderate COPD, from 24% to 31% in those with severe COPD, and from 16% to 42% in those with very severe COPD. Similarly, between 21% and 96% of COPD patients report pain with severity scores in the moderate to severe range.Citation1–Citation5
While cross-sectional studies provide insights about pain in COPD patients, only three studies have evaluated longitudinal changes in pain occurrence and severity.Citation7–Citation9 In a community sample of COPD patients,Citation7 46% reported pain at enrollment and 48% after two years. In another study,Citation8 the occurrence of pain was 74% before hospitalization and decreased to 54% two weeks after discharge. Finally, in a sample of COPD patients admitted to hospice,Citation9 82% had pain on admission and 28% had pain control within 24 hours. Across these three studies,Citation7–Citation9 16%–31% of the patients reported mild pain and 20%–63% reported moderate to severe pain. While these findings suggest that pain persists in COPD patients, none of these studies evaluated for changes in the occurrence and severity of pain and in patients at different stages of their disease. Therefore, longitudinal studies are needed to characterize changes over time in the occurrence and severity of pain in COPD patients in various stages of the disease.
Eight studies evaluated the relationships between demographic and clinical characteristic and pain in COPD patients.Citation1,Citation2,Citation6,Citation10–Citation14 While no sex and age differences were found in two studies,Citation13,Citation14 in other studies females had a higher prevalence of pain.Citation1 Moreover, younger patients reported more severe pain.Citation2,Citation10 Regarding the relationships between pain and body mass index (BMI) and comorbidities, previous findings are inconclusive. While three studies found no association between pain and BMI,Citation10,Citation13,Citation14 other studies of COPD patients found that pain was associated with higher BMI,Citation12 as well as with a higher number of comorbidities.Citation6,Citation12 While no associations were found between lung function or smoking and pain in two studies,Citation6,Citation10 in a recent studyCitation1 patients with better lung function reported more severe pain. In addition, COPD patients with pain had lower levels of physical function.Citation12
Health-related quality of life (HRQoL) provides insights into the disease as well as patients’ health status.Citation15–Citation18 Three studies have evaluated the relationship between pain and HRQoL in patients with COPD.Citation6,Citation13,Citation19 One studyCitation6 found a significant association between pain occurrence and respiratory symptoms, while another study found a significant association between pain occurrence and pain severity, and overall health status,Citation13 by contrast, in another studyCitation19 no association was found between worst pain severity and overall health status.
In several studies,Citation1,Citation10,Citation11,Citation20–Citation22 the authors commented that the occurrence, severity, and risk factors for pain in patients with COPD were rather heterogeneous. Although two studies reported changes over time in the occurrence and severity of pain,Citation7,Citation8 neither of these studies evaluated demographic and clinical characteristics, and HRQoL associated with this variability. These limitations highlight the need for additional research on changes in and characteristics associated with the occurrence and severity of pain in patients with COPD. Therefore, the purposes of the present study were to examine whether distinct groups of COPD patients could be identified based on changes in self-reports of pain occurrence and severity over 12 months and to evaluate whether these groups differed on a number of demographic, clinical, and pain characteristics, as well as HRQoL.
Patients and methods
Patients, settings, and study procedures
This longitudinal study is a follow-up study of 267 COPD patients (ClinicalTrials.gov identification: NCT1016587).Citation1 In brief, patients were enrolled from three outpatient clinics and one referral hospital in the Norwegian Health Region Southeast from December 2009 until October 2012. A research nurse explained the purpose of the study at enrollment, and written informed consent was obtained from all patients. The inclusion criteria were >18 years of age; diagnosed with moderate (grade II), severe (grade III), or very severe (grade IV) COPD according to the Global Initiative for Chronic Obstructive Lung disease (GOLD);Citation23 able to read and understand Norwegian; and had no cognitive impairments. The patient’s cognitive function was assessed by the nurse during the enrollment process. Exclusion criteria were receiving ongoing treatment for a pulmonary infection, COPD exacerbation, or cancer diagnosis at enrollment.
A total of 363 patients were asked to participate in this study. Of these, 16 did not meet the inclusion criteria and 55 declined to participate. Of the 292 patients who wanted to participate, eight withdrew from the study and 17 did not return the questionnaire at enrollment. The final sample for this study consisted of 267 patients (response rate 76.9%). To evaluate for the changes in pain occurrence and severity, patients completed questionnaires at enrollment (n=267), and at three (n=234), six (n=225), nine (n=202), and 12 (n=202) months after enrollment.
This study was approved by the privacy ombudsman at Oslo University Hospital, and recommended by the Regional Committees for Medical and Health Research Ethics (reference no S-09102a).
Instruments
Patients completed all of the self-report questionnaires. Research nurse reviewed the patients’ medical records for clinical data.
Demographic and clinical characteristics
At enrollment, patients provided information on age, sex, education, and cohabitation. The research nurse collected data on BMI, smoking history, and number of years since diagnosis of COPD. Pack-years smoking was calculated as the average number of cigarettes smoked per day divided by 20 and multiplied by the total number of years smoking.Citation24
Comorbidity
Comorbidities were assessed using the Self-Administered Comorbidity Questionnaire (SCQ-19),Citation25 which includes 16 common and three optional medical conditions. Patients were asked to indicate whether they had the comorbid condition (yes/no), if they received treatment for it (yes/no), and whether it limited their activities (yes/no). The SCQ total score can range from 0 to 57. A higher score indicates a more severe comorbidity profile.Citation25 The SCQ-19 has well-established validity and reliability with patients with chronic medical conditions.Citation25
Pain
Pain occurrence, worst pain severity, pain inference, and number of pain locations were examined using the Brief Pain Inventory (BPI).Citation26 Patients were asked to indicate whether they generally were bothered by pain (yes/no). If they were generally bothered by pain, they rated worst pain severity using a numeric rating scale (NRS) that ranged from 0 (no pain) to 10 (worst pain imaginable). In addition, patients rated how much pain interfered with general activity, mood, walking ability, normal work and housework, relations with other people, sleep, enjoyment of life using a NRS that ranged from 0 (does not interfere) to 10 (completely interferes). A total interference score was calculated as the mean of these seven items. Total number of pain locations was calculated using a body outline diagram. The body outline diagram is divided into 30 different areas. Each area that was marked was counted and summed to create the total number of pain locations. Scores could range from 0 to 30.Citation27 The Norwegian version of BPI has satisfactory validity and reliability and sensitivity to change in longitudinal studies.Citation28,Citation29 The BPI was used in studies of COPD patients.Citation1,Citation10–Citation13,Citation22
HRQoL
The St George’s Respiratory Questionnaire (SGRQ) during the last three months was used to evaluate the overall HRQoL.Citation30 The total SGRQ score can range from 0 to 100, with higher scores indicating lower HRQoL.Citation30,Citation31 The SGRQ is a valid and reliable measure of HRQoL in patients with COPD.Citation32–Citation34
Lung function
At enrollment, patients underwent a spirometry. Data were collected on forced expiratory volume in one second (FEV1) and forced vital capacity (FVC), and predicted values were calculated according to the guidelines of the European Respiratory Society.Citation35 FVC, FEV1, and FEV1 as a percentage of the predicted value (FEV1% predicted) were used as measures of lung function. Disease severity was classified using the GOLD guidelinesCitation23 and was graded as mild (FEV1 ≥80% predicted), moderate (FEV1 50%–79% predicted), severe (FEV1 30%–49% predicted), or very severe (FEV1 <30% predicted).
Physical function
Physical function was evaluated using the 6 Minute Walk Test (6MWT).Citation36,Citation37 Distance covered was measured to the closest meter. A greater distance indicates better physical function. The 6MWT has satisfactory validity and reliability in COPD patients.Citation37,Citation38
Data analysis
In this study, patients who indicated that they were generally bothered by pain or who completed information on two of the four dimensions of the BPI (ie, intensity, location, interference, relief)Citation26 were categorized into the pain group.
The profile for pain across five assessments was evaluated. Because trajectory for pain across the assessments was complex, latent class analysis (LCA) for the occurrence rates, and latent profile analysis (LPA) for the severity ranges were performed rather than growth mixture modeling.Citation39–Citation42 To accommodate expected serial covariation over time, covariances between adjacent assessments were included in the model (ie, baseline with three months, three months with six months, etc.). Patients who did not report pain at any of the five measurements were classified as the no pain group. These patients were not included in the LCA or LPA. Separate analyses were done for pain occurrence (LCA) and severity (worst pain; LPA) to identify groups of patients (ie, latent classes) with distinct pain experiences over the five assessments.
Estimation was carried out with full information maximum likelihood (FIML) with standard errors and a chi-square test that are robust to non-normality and non-independence of observations (estimator = multiple linear regression analysis). Model fit was evaluated using the Bayesian Information Criterion (BIC), entropy, the Vuong Lo Mendell Rubin (VLMR) likelihood ratio test for the K vs K-1 model, and latent class sizes (percentages) that were large enough to be reliable.Citation43,Citation44 Missing data were accommodated with the use of FIML and the Expectation Maximization algorithm.
Mixture models such as LPA are known to produce solutions at local maxima. Therefore, our models were fit with from 1,000 to 2,400 random starts. This approach ensured that the selected model was replicated many times and not due to a local maximum. The LPAs were conducted using Mplus Version 7.2.Citation43
After identifying the latent class solution that best fits the data for each outcome, the patients who did not report pain at any of the five assessments were added in the subsequent analyses as the no pain group. Differences in demographic and clinical characteristics as well as HRQoL among the pain groups were evaluated using analysis of variance, chi-square tests, or Kruskal–Wallis tests using SPSS version 21.Citation45 A p-value of <0.05 was considered statistically significant. Multiple comparisons of differences between groups were Bonferroni adjusted.
Results
Patient characteristics
Of the 267 patients in this study, 52.8% were females, with a mean age of 63.2 (SD 9.0, range 37–84) years. A total of 24% were current smokers. The mean numbers of years since the diagnosis of COPD was 7.6 (SD 6.3, range 0–35). In addition, 31.1% of the patients had moderate COPD, 22.8% had severe COPD, while 46.1% had very severe COPD. Characteristics of the participants at enrollment are summarized in .
Table 1 Characteristics in the total sample at enrollment into the study (n=267)
LCA for pain occurrence
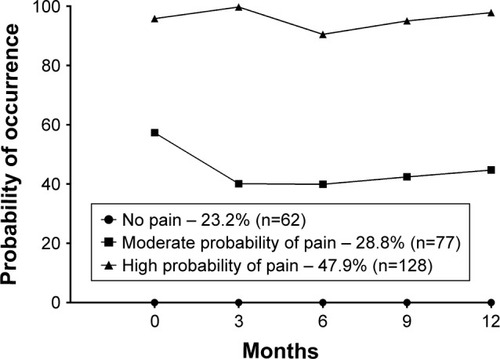
After removing patients who did not report any occurrence of pain across the five assessments, the LCA was performed. A 2-class solution fits the data best. The 2-class solution was selected because the BIC was smallest for the 2-class solution, the VLMR was significant for the 2-class but not for the 3-class solution, and because one of the classes in the 3-class solution was too small (14 cases, or 7% of the sample examined in the latent profile models) to be reliable ().
Table 2 Latent class profile analysis solutions and fit indices for the 1-class through 3-class solutions for probability of occurrence of pain and severity of worst pain
As shown in , 62 patients (23.2%) did not report any pain across the five assessments (ie, no pain group). The largest group of patients (n=128; 47.9%), with the highest pain occurrence rates, was named the “high probability of pain” group. The second largest group (n=77; 28.8%) was named the “moderate probability of pain” group.
Differences in demographic and clinical characteristics and HRQoL among the pain occurrence groups
As shown in , compared to the “no pain” group, patients in the “high probability of pain” group were more likely to be female; were less likely to have a university education; had a higher BMI; had a higher FEV1% predicted; and were less likely to have very severe COPD. In addition, these patients reported a higher number of comorbidities and a higher total SCQ score, and were more likely to report heart disease, headache, depression, osteoarthritis, back and neck pain, and disease of muscle and connective tissue. Compared to the “no pain” group, patients in the “moderate probability of pain” group reported a higher number of comorbidities and were more likely to report back and neck pain. Compared to the “moderate probability of pain” group, patients in the “high probability of pain” group reported more pain locations and a higher pain interference score. For the SGRQ symptom component, patients in the “high probability of pain” group had a significantly higher score than the patients in the “no pain” group. In addition, there was a significant difference in the SGRQ total score, but no significant pairwise group differences were found.
Table 3 Differences in demographic and clinical characteristics, and health-related quality of life among the three latent pain groups based on probability of occurrence of pain
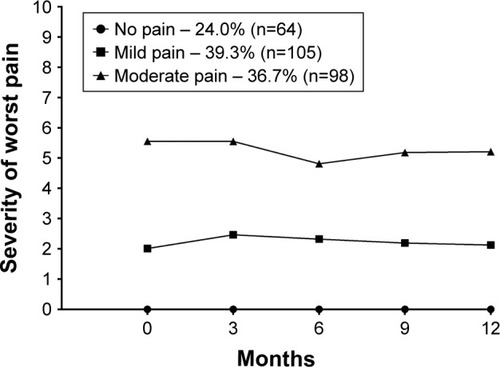
LPA for worst pain severity
After removing patients who did not report any severity ratings for pain across the five assessments, the LPA of worst pain scores was performed. Again, a 2-class solution fits the data best. The 2-class solution was selected because the VLMR was significant for the 2-class but not for the 3-class solution and one of the classes in the 3-class solution was too small (9 cases, or 4% of the sample examined in the latent profile models) to be reliable (). In addition, although the BIC was slightly larger for the 2-class solution compared to the 3-class solution, the difference was trivial (3,091.61 compared to 3,090.77).Citation46,Citation47 Therefore, the 3-class solution did not provide a better fit than the 2-class solution using the BIC as a criterion.
As shown in , 64 patients (24.0%) reported worst pain scores of 0 across the five assessments (ie, no pain group). The largest group of patients (n=105, 39.3%) reported worst pain scores in the mild range (ie, mild pain group). The second largest group (n=98, 36.7%) reported worst pain scores in the moderate range (ie, moderate pain group).
Differences in demographic and clinical characteristics and HRQoL among the worst pain severity groups
As shown in , compared to the “no pain” group, patients in the “moderate pain” group were more likely to be female, were less likely to have a university education, had a higher BMI, had a higher FEV1 (liters) and FEV1% predicted, and were less likely to have very severe COPD. In addition, these patients reported a higher number of comorbidities and a higher SCQ score. They were more likely to report heart disease, headache, osteoarthritis, back and neck pain, and disease of muscle and connective tissue. Compared to the “no pain” group, the patients in the “mild pain” group reported a higher number of comorbidities, had a higher SCQ score, and were more likely to report back and neck pain. Compared to the “mild pain” group, patients in the “moderate pain” group reported more pain locations and higher pain interference score. There was a significant difference in SGRQ symptoms score (p=0.047), but no significant pairwise group difference was found.
Table 4 Differences in demographic and clinical characteristics, and health-related quality of life among the three latent pain groups based on ratings of severity of worst pain
Discussion
The present study is the first to identify specific groups of patients with COPD who are characterized by distinct trajectories of pain based on reports of occurrence and severity over a 12-month period. Using LCA, two distinct groups of pain could be identified among those COPD patients who reported pain, one with high probability and one with moderate probability of pain. A similar pattern was found when severity scores were used in the LPA. When analyzing the occurrence of pain, we found that 77% of the patients had pain at least once during the five assessments done over one year. Of these, 29% of the patients were in the “moderate probability of pain” group and 48% were in the “high probability of pain” group. Moreover, when analyzing pain severity, we found that the overall percentage of patients with pain scores in the mild and moderate range was 76%. This finding is higher than the 38% found in terminally ill COPD patients.Citation5 Taken together, our findings suggest that persistent pain is a significant problem for COPD patients.
In addition, we found that those who reported pain had less severe COPD as measured by FEV1% predicted. These findings are consistent with a previous study that found that patients with moderate COPD reported a higher pain prevalence rate and worse pain severity scores than patients with severe or very severe disease.Citation3 There may be several explanations for this somewhat unexpected finding. One potential explanation is that patients with more severe COPD are more likely to report respiratory phenomena (eg, chronic cough, sputum production, breathlessness, wheezing)Citation10,Citation48,Citation49 that are experienced as more severe and distressing than pain.
Despite the fact that the patients with higher probability of pain occurrence had less severe COPD as measured by FEV1% predicted, they reported more respiratory symptoms. This finding is consistent with a previous study.Citation20 In addition, in a qualitative studyCitation22 it was found that COPD patients described their pain as “tying up their body” making it impossible to breathe, which in turn resulted in increased pain. This finding may be a confirmation of the notion that the sensation of pain and respiratory symptoms may be related.Citation50
Regarding the specific descriptions of pain, our study showed that painful conditions including headache, heart diseases, osteoarthritis, back and neck pain, rheumatoid arthritis, and diseases of muscle and connective tissue were reported in relatively high percentages of patients in the two highest pain groups compared to the no pain groups. This finding is consistent with previous research.Citation51 It is conceivable that some of these conditions may be causally related to the COPD. Headache may result from chronic hypoxemia.Citation52 In addition, osteoporosis-related vertebral fractures are common in COPDCitation53 and the resulting pain is often reported to be severe.Citation54,Citation55 Moreover, the high rates of back and neck pain in the COPD patients could be explained by changes in respiratory function and remodeling of the thorax often associated with COPD.Citation56,Citation57 The main muscles of respiration are the diaphragm and the intercostal muscles.Citation58 However, in patients with COPD, a range of muscles located in the neck (ie, sternocleidomastoid, scalene muscles, pectoralis major and minor) and back (erector spinae and levatores costarum) are overused,Citation59 which may lead to increased pain.Citation56,Citation57 Also, there is evidence to suggest that the systemic inflammation associated with COPD may contribute to the sensation of pain.Citation8,Citation51 Finally, the back and neck pain may be related to a higher BMI.Citation11,Citation13 The BMIs of the patients in the “high probability of pain” (ie, 24–29) and “moderate pain” (ie, 25–29) groups are classified as overweight by the World Health Organization.Citation60 Moreover, being overweight is associated with increased pain in the elderly,Citation61 as well as with a number of painful musculoskeletal conditions (eg, osteoarthritis, and neck back, hip and knee pain).Citation62,Citation63
Additional factors are associated with reports of pain in patients with COPD. Compared to the “no pain” group, patients in the “high probability of pain” and “moderate pain” groups were more likely to be female, to report depression, and to have only a primary school education. Of note, painful musculoskeletal disorders (eg, back and neck pain, osteoarthritis) are more common in females.Citation64–Citation66 In addition, population-based studies,Citation67,Citation68 as well as previous studies of COPD patients,Citation2,Citation69 found that females and depressed patients report higher occurrence and severity of pain. The reasons for this association are not clear. However, evidence suggests that sex differences in pain occurrence and severity may be explained by differences in sex steroid hormones.Citation70 While causal association between depression and pain is not clear, it may be of interest that the same neurological mechanisms are involved in the perception of both depression and pain.Citation71,Citation72 Finally, why the occurrence and severity of pain was associated with a lower level of education is not clear, but our finding is consistent with a previous study.Citation73
Limitations
Some limitations need to be acknowledged. The exact etiologies for the pain and the use of pain medications were not evaluated. Our observations suggest that a detailed characterization of the causes of and treatment for pain should be evaluated in future studies. A further limitation of this study is that approximately 50% of our patients had very severe COPD and were recruited from a tertiary referral hospital. Hence, the results from the present study may not generalize to all COPD patients. Strengths of the study include its high response rate and the large sample of COPD patients evaluated, particularly those COPD patients in the more severe stages of the disease.Citation6,Citation11,Citation13
Conclusion and clinical implications
Our study demonstrates a high occurrence of pain in COPD patients and that this pain persists over time and is often associated with certain comorbidities. The results from this study suggest that more effective interventions are needed to manage pain in COPD patients, particularly among the overweight and poorly educated women in the milder disease groups of COPD. Clinicians may be able to use this information to identify patients who are at higher risk for more severe and persistent pain.
Acknowledgments
We want to thank all the patients and clinicians who contributed to this study, especially the research nurses Gunilla Solbakk, Mari-Ann Øvreseth and Britt Drægni.
Disclosure
The authors report no conflicts of interest in this work.
References
- ChristensenVLHolmAMKongerudJOccurrence, characteristics, and predictors of pain in patients with chronic obstructive pulmonary diseasePain Manag Nurs201617210711827095390
- JanssenDWoutersEParraYStakenborgKFranssenFPrevalence of thoracic pain in patients with chronic obstructive pulmonary disease and relationship with patient characteristics: a cross-sectional observational studyBMC Pulm Med2016164727052199
- van Dam van IsseltEFGroenewegen-SipekamaKHSpruitvan EijkMPain in patients with COPD: a systematic review and meta-analysisBMJ Open201449e005898
- LeeALHarrisonSLGoldsteinRSBrooksDPain and its clinical associations in individuals with COPD: a systematic reviewChest201514751246125825654647
- WyshamNGCoxCEWolfSPKamalAHSymptom burden of chronic lung disease compaed with lung cancer at time of refferral for palliative care consultationAnn Am Thorac Soc20151291294130026161449
- BentsenSBRustøenTMiaskowskiCDifferences in subjective and objective respiratory parameters in patients with chronic obstructive pulmonary disease with and without painInt J Chron Obstruct Pulmon Dis2012713714322419861
- WalkeLMByersALTinettiMEDubinJAMcCorkleRFriedTRRange and severity of symptoms over time among older adults with chronic obstructive pulmonary disease and heart failureArch Intern Med2007167222503250818071174
- PantilatSZO’RiordanDLDibbleSLLangfeldCSLongituidinal assessment of symptom severity among hospitalized elders diagnosed with cancer, heart failure, and chronic obstructive pulmonary diseaseJ Hosp Med20127756757222371388
- RomemATomSEBeaucheneMBabingtonLScharfSMRomenAPain management at the end of life: a comparative study of cancer, dementia, and chronic obstructive pulmonary diseasePalliat Med201529546446925680377
- BorgeCRWahlAKMoumTAssociation of breathlessness with multiple symptoms in chronic obstructive pulmonary diseaseJ Adv Nurs201066122688270020825511
- HajGhanbariBHolstiLRoadJDRiedDWPain in people with chronic obstructive pulmonary disease (COPD)Respir Med20121067998100522531146
- HajGhanbariBGarlandSJRoadJDReidWDPain and physical performance in people with COPDRespir Med2013107111692169923845881
- BorgeCRWahlAKMoumTPain and quality of life with chronic obstructive pulmonary diseaseHeart Lung2011403E90E10121444112
- HajGhanbariBYamabayashiCGarlandSJRoadJDReidWDThe relationship between pain and comorbid health conditions in people with chronic obstructive pulmonary diseaseCardiopulm Phys Ther J20142512535
- AndersonKLBurckhardtCSConceptalization and measurement of quality of life as an outcome variable for health care intervention and researchJ Adv Nurs199929229830610197928
- CazzolaMMacNeeWMartinezFJAmerican Thoracic SocietyEuropean Respiratory Society Task Force on outcomes of COPDOutcomes for COPD pharmacological trials: from lung function to biomarkersEur Respir J200831241646818238951
- WilkeSJanssenDJWoutersEFScholsJMFranssenFMSpruitMACorrelations between disease-specific and generic health status questionnaires in patients with advanced COPD: a one-year observational studyHealth Qual Life Outcomes2012109822909154
- Wood-DauphnieeSAssessing quality of life in clinical research: from where have we come and where are we going?J Clin Epidemiol199952435536310235176
- BentsenSBMiaskowskiCRustoenTDemographic and clinical characteristics associated with quality of life in patients with chronic obstructive pulmonary diseaseQual Life Res201423399199823999743
- BentsenSBRustoenTMiaskowskiCPrevalence and characteristics of pain in patients with chronic obstructive pulmonary disease compared to the Norwegian general populationJ Pain201112553954521549316
- JanssenDJSpruitMAUszko-LencerNHScholsJMWoutersEFSymptoms, comorbidities, and health care in advanced chronic obstructive pulmonary disease or chronic heart failureJ Palliat Care Med2011146735743
- LohneVHeerHCAndersenMMiaskowskiCKongerudJRustoenTQualitative study of pain in patients with chronic obstructive pulmonary diseaseHeart Lung2010393225234
- GOLDGlobal strategy for the diagnosis, management and prevention of chronic obstructive pulmonary diseasePortland, ORGlobal Initiative for Chronic Obstructive Lung Disease2017
- LarssonKKOL – Kronisk Obstruktiv Lungsjukdom2nd edLundStudentlitteratur2006 Swedish
- SanghaOStuckiGLiangMHFosselAHKatzJNThe self administered comorbidity questionnaire: a new method to assess comorbidity for clinical and health services researchArthritis Rheum200349215616312687505
- CleelandCSRyanKMPain assessment: global use of the Brief Pain InterventoryAnn Acad Med Singapore19942321291388080219
- PuntilloKPain in the Critically Ill: Assessment and ManagementGaithersburg, MDAspen Publishers1991
- KlepstadPLogeJHBorchgrevinkPCMendozaTRCleelandCSKaasaSThe Norwegian Brief Pain Inventory Questionnaire: translation and validation in cancer pain patientsJ Pain Symptom Manage200224551752512547051
- TanGJensenMPThornbyJIShantiBFValidation of the Brief Pain Inventory for chronic nonmalignant painJ Pain20045213313715042521
- JonesPWQuirkFHBaveystockCMThe St George’s Respiratory QuestionnaireRespir Med199185Suppl B25351759018
- JonesPWSt. George’s Respiratory Questionnaire: MCIDCOPD200521757917136966
- BarrJTSchumacherGEFreemanSLeMoineMBakstAWJonesPWAmerican translation, modification, and validation of the St. George’s Respiratory QuestionnaireClin Ther20002291121114511048909
- EngströmCPPerssonLOLarssonSSullivanMReliability and validity of the Swedish version of the St George’s Respiratory QuestionnaireEur Respir J199811161669543271
- FerrerMAlonsoJPrietoLValidity and reliability of the St. George’s Respiratory Questionnaire after adaptation to a different language and culture: the Spanish exampleEur Respir J199696116011668804932
- QuanjerPHTammelingGJCotesJEPedersenOFPeslinRYernaultJCLung volums and forced ventilatory flows. Report working party standardization of lung function tests European community for steel and coal. Official statment of the European respiratory societyEur Respir J Suppl1993165408499054
- ButlandRJPangJGrossERWoodcockAAGeddesDMTwo-, six-, and twelve-minute walking tests in respiratory diseaseBr Med J (Clin Res Ed)1982284632916071608
- GuyattGHSullivanMJThompsonPJThe 6-minute walk: a new measure of exercise capcity in patients with chronic heart failureCan Med Assoc J198513289199233978515
- SolwaySBrooksDLacasseYThomasSA qualitative systematic overview of the measurement properties of functional walk test used in cardiorespiratory domainChest2001119125627011157613
- GeiserCData Analysis with MplusNew York, NYGuilford Press2012
- JungTWickramaKASAn introduction to latent class growth analysis and growth mixture modelingSoc Personal Psychol Compass20082302317
- MuthènBSecond-generation structural equation modeling with a combination of categorical and continuous latent variables: new opportunities for latent-class growth modelingColinsLMSayerAGNew Methods for the Analysis of ChangeWashington, DCAmerican Psychological Association2001291322
- MuthèLPersonal Communication, Mplus Product SupportLos AngelesCA. Muthèn & Muthèn2014
- MuthenLMuthenBMplus User’s Guide7th edLos Angeles, CAMuthen & Muthen19982014
- NylundKAsparouhovTMuthenBDeciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation studyStruct Equ Model200714535569
- SPSSIBM SPSS for Windows (version 21)Armonk, NYSPSS, Inc2016
- MuthènBMplus Discussion: Latent Variable Mixture Modelling: Latent Transition Analysis (LTA) Available from: http://www.statmodel.com/discussion/messages/13/278.htmlAccessed August 31, 2010
- MuthènBMplus Discussion: Using BIC for SEM Available from: http://www.statmodel.com/discussion/messages/11/5682.htmlAccessed July 14, 2010
- BentsenSBHenriksenAHWentzel-LarsenTHanestadBRWahlAKWhat determines subjective health status in patients with chronic obstructive pulmonary disease: importance of symptoms in subjective health status of COPD patientsHealth Qual Life Outcomes2008611519094216
- BlindermanCDHomelPBillingsJATennstedtSPortenoyRKSymptoms, distress and quality of life in patients with advanced chronic obstructive pulmonary diseaseJ Pain Symptom Manage200938111512319232893
- LansingRWGracelyRHBanzetRBThe multiple dimensions of dys-pnea: review and hypothesesRespir Physiol Neurobiol20091671536018706531
- RobertsMHMapelDWHartryAvonWorleyAThomsonHChronic pain and pain medication use in chronic obstructive pulmonary disease. A cross-sectional studyAnn Am Thorac Soc201310429029823952846
- OzgeAOzgeCKaleagasiHYalinOUnalOOzgürESHeadache in patients with chronic obstructie pulmonary disease: effects of chronic hypoxaemiaJ Headache Pain200671374316408153
- BiskobingDMCOPD and osteoporosisChest2002121260962011834678
- Fahrleitner-PammerALangdahlBLMartinFFracture rate and back pain during and after discontinuation of teriapide: 36-month data from the European Forseo Observational Study (EFOS)Osteoporos Int201122102709271921113576
- LeeJSongJHootmanJMObesity and other modifiable factors for physical inactivity measured by accelerometer in adults with knee osteoarthritisArthritis Care Res (Hoboken)2013651536122674911
- O’SullivanPBBealesDJChanges in pelvic floor and diaphragm kinematics and respiratory patterns in subjects with sacroiliac joint pain following a motor learning intervention: a case seriesMan Ther200712320921816919496
- KapreliEVourazanisEBillisEOldhamJAStrimpakosNRespiratory dysfunction in chronic neck pain patients. A pilot studyCephalagia2009297701710
- MartiniFNathJBartholomewEFundamentals of Anatomy and Physiology9th edSan Francisco, CABenjamin Cummings2012
- Orozco-LeviMStructure and function of the respiratory muscles in patients with COPD: impariment or adaptation?Eur Respir J Suppl20034641s51s14621106
- WHOObesity and overweight2016 Available from: http://www.who.int/mediacentre/factsheets/fs311/en/Accessed July 04, 2016
- McCarthyLHBigalMEKatzMDerbyCLiptonRBChronic pain and obesity in elderly people: results from the Einstein aging studyJ Am Geriatr Soc200957140341019278395
- PlotnikoffRKarunamuniNLytvyakEOsteoarthritis prevalence and modifiable factors: a population studyBMC Public Health2015151195120526619838
- DeereKCClinchJHollidayKObesity is a risk factor for musculoskeletal pain in adolescents: findings from a population-based cohortPain201215391932193822805779
- StenbergGLundquistAFjellman-WiklundAAhlgrenCPatterns of reported problems in women and men with back and neck pain: similarities and differencesJ Rehabil Med201446766867524909233
- KingeJMKnudsenAKSkirbekkVVollsetSEMusculoskeletal disorders in Norway: prevalence of chronicity and use of primary and specialist health care servicesBMC Musculoskelet Disord2015167525887763
- PaanalahtiKHolmLWMagnussonCCarrollLNordinMSkillgateEThe sex-specific interrelationship between spinal pain and psychological distress across time in the general population. Results from the Stock-holm Public Health StudySpine J20141491928193524262854
- BreivikHCollettBVentafriddaVCohenRGallacherDSurvey of chronic pain in Europe: prevalence, impact on daily life, and treatmentEur J Pain200610428733316095934
- RustøenTWahlAKHanestadBRLerdalAPaulSMiaskowskiCPrevalence and characteristics of chronic pain in the Norwegian general populationEur J Pain20048655556515531224
- Di MarcoFVergaMReggenteMAnxiety and depression in COPD patients: the roles of gender and disease severityRespir Med2006100101767177416531031
- de KruijfMStolkLZillikensMCLower sex hormone levels are associated with more chronic musculoskeletal pain in community-dwelling elderly womenPain201615771425143127331348
- De PeuterSVan DiestILemaigreVVerledenGDemedtsMVan den BerghODyspnea: the role of psychological processesClin Psychol Rev200424555758115325745
- GatchelRJPengYBFuchsPNPetersMLTurkDCThe biopsychosocial approach to chronic pain: scientific advances and future directionsPsychol Bull2007133458162417592957
- MundalIBjørngaardJHNilsenTINichollBIGraweRWForsEALong-term changes in musculoskeletal pain sites in the general population: the HUNT studyJ Pain201617111246125627578444