Abstract
Purpose
Exacerbation-associated health-related quality of life (HRQoL) in patients with severe and very severe chronic obstructive pulmonary disease (COPD) is ill-defined. This study describes patterns, HRQoL, and the work productivity impact of COPD-related moderate and SEV exacerbations in patients with SEV/VSEV COPD, focusing on the chronic bronchitis subtype.
Patients and methods
A US sample of SEV and VSEV COPD patients with recent moderate or SEV exacerbation was recruited. Along with the demographic and clinical data collected from medical records, patients reported on exacerbation frequency, health-related quality of life (HRQoL) (using the St George’s Respiratory Questionnaire for COPD [SGRQ-C] and the European Quality of Life-5 Dimensions [EQ-5D]™ index), and work productivity and activity impairment (using the Work Productivity and Activity Impairment Questionnaire – Specific Health Problem [WPAI-SHP]). The HRQoL-related impacts of exacerbation frequency, time since exacerbation, and last exacerbation severity were evaluated via linear regressions.
Results
A total of 314 patients (190 SEV/124 VSEV, mean age =68.0 years, 51% male, 28% current smokers) were included. In the previous 12 months, patients reported an average of 1.8 moderate exacerbations and 0.9 SEV exacerbations. Overall, 16% of patients were employed and reported a high percentage of overall work impairment (42.4% ± 31.1%). Activity impairment was positively associated with recent exacerbation severity (SEV 64.6% ± 26.8% versus moderate 55.6% ± 28.2%) (P=0.006). The HRQoL was significantly worse for SEV versus VSEV COPD (EQ-5D: 0.62 ± 0.23 versus 0.70 ± 0.17, respectively, and SGRQ-C: 70.1 ± 21.3 versus 61.1 ± 19.0, respectively) (P<0.001). Worse current HRQoL was reported by patients with a SEV versus moderate recent exacerbation (EQ-5D: 0.63 ± 0.21 versus 0.70 ± 0.20, respectively) (P=0.003); SGRQ-C: 70.3 ± 19.9 versus 61.7 ± 20.1, respectively (P<0.001). One additional exacerbation in the previous 12 months was associated with a 2.4-point SGRQ-C increase and a 0.02-point EQ-5D index decrease.
Conclusion
The severity and frequency of COPD-related moderate/SEV exacerbations in SEV and VSEV COPD patients were positively associated with poor HRQoL and work productivity and activity impairment.
Introduction
Chronic obstructive pulmonary disease (COPD) is a slowly progressive condition affecting approximately 24 million adults in the United States, an estimated 50% of whom are undiagnosed.Citation1 Affected patients suffer from frequent and recurrent exacerbations, which are defined by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) as events in the course of COPD, characterized by acute changes in patients’ baseline dyspnea, cough, and/or sputum exceeding ordinary day-to-day variations and which may warrant changes to medication.Citation2 Accordingly, COPD exacerbations are associated with rapid decline in lung function and physical activity, increased risk of hospitalization and mortality,Citation3,Citation4 deterioration in health-related quality of life (HRQoL), and substantial financial burden.Citation3,Citation5,Citation6
Previous studies have noted the impact of increasing disease severity on HRQoL,Citation7–Citation10 that patients experiencing an exacerbation have worse HRQoL versus patients with stable disease,Citation11 and that HRQoL deteriorates with frequent exacerbations.Citation12 However, further evidence of the real-world impact of exacerbations on HRQoL and work impairment in actively-treated COPD patients is essential, particularly for high risk severe and very severe COPD patients.Citation13 Of note, there have been no published analyses comparing the effects of varying levels of exacerbation severity among severe and very severe COPD patients.
To this end, the objective of this study was to describe COPD exacerbation burden in terms of exacerbation frequency and severity, HRQoL, and impact on work productivity, in patients with severe or very severe COPD, with a focus on the chronic bronchitis subtype, and to explore the relationship between exacerbation frequency/severity and patients’ HRQoL and work productivity.
Material and methods
This study combined a retrospective observational chart review with a cross-sectional patient survey, to assess patients who had been diagnosed with severe or very severe COPD and who had experienced a moderate or severe exacerbation within 3 months prior to data collection. The medical charts of enrolled patients were reviewed to collect clinical/medical-related information, and then all patients were surveyed to collect matched data on HRQoL and work productivity. This study was conducted in compliance with the Health Insurance Portability and Accountability Act of 1996Citation14 and was exempted from patient consent by New England Institutional Review Board.
Study design
Data collection (from recruitment of the first physician through completion of the last documents) occurred between November 23, 2011 and March 30, 2012.
Physician selection
A stratified random quota sample of 100 physicians (with a target of equal representation by pulmonologists and primary care physicians drawn in equal proportions from the four major census regions of the United States) were identified from a national database provided by F1rstMark, Inc. (Campton, NH, USA) and recruited via telephone. The physicians were screened to ensure that they were currently managing/treating severe and/or very severe COPD patients (as defined by GOLD guidelines)Citation15 and that they were willing to comply with study instructions.
Patient selection
From among all adults (>40 years old) who had been diagnosed with severe or very severe COPD for ≥12 months prior to their most recent visit, had a chronic productive cough for ≥3 months, and who experienced ≥1 moderate or severe exacerbation (based on the American Thoracic Society/European Respiratory Society-proposed categories for COPD exacerbation severity)Citation16 within the previous 3 months, each included physician was asked to randomly select up to four adults from his/her practice, using patient birth month and day as the selection criteria, with a randomly chosen starting point for birth month/day that varied across sites.
Data collection instruments
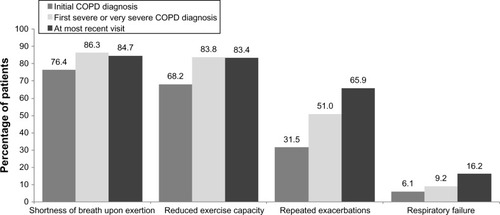
A patient case report form was developed to abstract the clinical/medical information from the patient medical record, and a physician practice profile form was also completed by the physician to profile the treatment site/clinical practice. Patient interview data were collected via a computer-assisted telephone interview technique. Alternatively, patients were also provided the option of completing a paper and pencil version of the instrument. The data elements collected from the physicians’ practice profile forms, patients’ medical charts, and patient surveys are summarized in .
Figure 1 Data elements collected within the study.
Outcomes
The key outcomes included the frequency of exacerbations in the previous 12 months, patient-reported HRQoL, and patient-reported work productivity and impairment.
COPD severity
Spirometry readings and COPD symptoms were collected at the initial COPD diagnosis, at the initial diagnosis of severe/very severe COPD, and at the most recent visit. Patient severity was classified based on the physician report at the time of the diagnosis of severe/very severe COPD or at their most recent visit (maximum value observed). Physicians were provided with the following references for diagnosing COPD severity based on spirometry readings (consistent with GOLD guidelines):Citation15 mild = forced expiratory volume in 1 second/forced vital capacity (FEV1/FVC) <0.7 and FEV1 ≥80% predicted; moderate = FEV1/FVC <0.7 and 50% ≤ FEV1 <80% predicted; severe = FEV1/FVC <0.7 and 30% ≤ FEV1 <50% predicted; and very severe = FEV1/FVC <0.7 and FEV1 <30% predicted; however, they were not restricted to using only spirometry-based definitions (ie, they could base their severity rating on other factors beyond spirometry). Patients’ worst severity was measured based on the maximum level of physician-reported severity attained at their most recent visit or at their initial diagnosis of severe/very severe COPD.
Exacerbations
Exacerbation severity was classified as mild (increase in respiratory symptoms controllable by an increase of usual medication), moderate (requiring treatment with systemic steroids and/or antibiotics), or severe (requiring hospitalization or a visit to the emergency department), consistent with the American Thoracic Society/European Respiratory Society proposed categories for COPD exacerbation severity.Citation16 The number of moderate and severe exacerbations occurring within the previous 12 months was collected from both patients’ medical charts (primary source) and by direct patient report (secondary source). Patients also directly reported the number of mild exacerbations experienced in the previous 12 months. Chart data were used to classify a patient’s most recent exacerbation as moderate or severe.
Health-related quality of life
HRQoL data were collected via patient interview, using both a generic (European Quality of Life-5 DimensionsCitation17 [EQ-5D]™); and a disease-specific (St George’s Respiratory Questionnaire for COPDCitation20 [SGRQ-C]) instrument. The EQ-5D measures five single-item dimensions (Mobility, Self-Care, Usual Activities, Pain/Discomfort, and Anxiety/Depression), each with three levels of response (no, some, or extreme problems).Citation17 The reliability, validity, and responsiveness of this measure in COPD has been previously established.Citation18 Patients were asked to answer the EQ-5D items twice: once to rate their health on the day of the interview using the standard frame of reference for the EQ-5D and then, using a modified version of the EQ-5D that asked the patients to recall their health status during their last moderate or severe exacerbation. These responses were converted into utilities using the United States algorithm.Citation19
The SGRQ-C is an adaptation of the SGRQ that was designed specifically to focus on COPD patients and their unique symptom profile.Citation20 The SGRQ-C provides a total score and also, component scores for Symptoms, Activities, and Impacts, each of which ranges from 0 to 100, with directionality such that higher scores reflect worse HRQoL.
Work productivity
The Work Productivity and Activity Impairment Questionnaire – Specific Health Problem (WPAI-SHP)Citation21 was used to measure work and activity impairment in COPD patients, with a 7-day recall period. The WPAI-SHP was previously used within a COPD population and found to have “good to acceptable” ease of completion in 83% of subjects.Citation10
The WPAI-SHP consists of six items designed to measure work and activity impairment during the previous 7 days. The first question asks whether subjects are currently employed; if yes, questions 2 to 5 ask the subjects for the number of hours missed from work because of problems associated with the disease and the extent to which the problem affected their productivity while they were working (from “no effect on my work” to “completely prevented me from working”) during the previous 7 days. In addition to measuring work productivity, the WPAI-SHP questionnaire (the last question) asks patients about the extent to which their condition limits them in the performance of regular non-job-related daily activities. The WPAI-SHP outcomes are expressed as impairment percentages, with higher numbers indicating greater impairment and less productivity.
Statistical analyses
Outcomes were described and compared across COPD severity levels (severe or very severe) and by the severity of patients’ most recent exacerbation (moderate or severe), which by design occurred within 3 months of survey completion. Chi-squared tests were used for bivariate comparisons of the categorical variables (eg, exacerbation rates) and one-way analysis of variance (ANOVA) for continuous variables. All tests assumed a two-sided significance level of 0.05.
Pearson correlations between the severity and frequency of exacerbations reported in the previous 12 months, HRQoL, and WPAI-SHP scores were calculated in order to explore the relationship between exacerbations and HRQoL. Furthermore, multiple linear regressions evaluated the impact of the total number of exacerbations in the previous year, the time since exacerbation, and the severity of the last exacerbation as per the SGRQ-C total scores and EQ-5D index, controlling for COPD severity, age, and race ethnicity.
Results
A total of 99 physicians (45 pulmonologists/54 primary care physicians) recruited 314 COPD patients for the study (190 severe/124 very severe). Among the recruited patients, 205 (65.3%) and 109 (34.7%) had recently experienced a moderate or a severe exacerbation, respectively, and 40 patients (12.7%) were experiencing an exacerbation at the time that the survey was completed.
Patient demographics
The patients were predominantly white (86.6%), 51.3% male, with mean ± standard deviation age of 68.0 ± 9.6 years, and almost all patients were current (27.7%) or former (66.6%) smokers (). There were no significant differences in patient demographics, at the time of survey, between patients with severe versus very severe COPD or between patients with a moderate versus severe last exacerbation.
Table 1 Patient characteristics
COPD history, symptoms, and treatment
The average duration from the time of COPD diagnosis to the time of patients’ most recent physician visit was 6.4 ± 5.2 years (5.9 ± 4.9 for severe COPD; 7.2 ± 5.6 for very severe COPD). At their most recent visit, patients had been diagnosed with severe or very severe COPD for 3.7 ± 3.4 years.
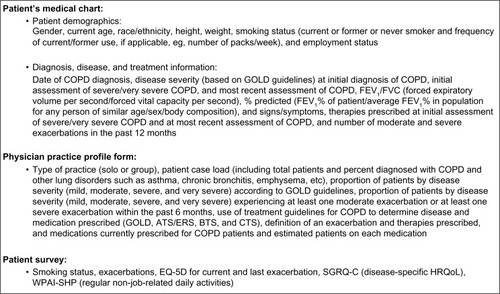
The most frequently observed symptoms for COPD patients at their most recent visit were shortness of breath upon exertion (84.7%) and reduced exercise capacity (83.4%) (). Patients were treated with a mean of 3.8 ± 1.2 medications, with inhaled corticosteroids (83.8%), short-acting beta agonists (83.1%), long-acting beta agonists (81.8%), and long-acting anticholinergics (74.2%) being most frequently prescribed. In addition, 65.4% patients who had recently experienced a moderate exacerbation and 85.3% who had experienced a severe exacerbation were on oxygen therapy.
Exacerbations
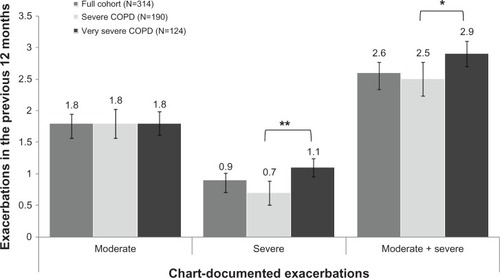
Severe COPD patients were more likely to have their last exacerbation be moderate (70.5% moderate versus 29.5% severe exacerbations), while very severe patients were more evenly divided between moderate and severe exacerbations (57.3% versus 42.7%). Based on the chart documentation, the patients had experienced an average of 2.6 ± 0.16 moderate (requiring systemic corticosteroid or antibiotic treatment) or severe (requiring an emergency room [ER] visit or hospitalization) exacerbations in the previous 12 months, with a total of 556 moderate exacerbations (mean length 10.7 ± 8.4 days) and 273 severe exacerbations (mean length 9.7 ± 5.8 days) recorded. Patients with very severe COPD had experienced significantly more severe exacerbations in the previous 12 months versus severe COPD patients (mean 1.1 ± 0.19 versus 0.7 ± 0.14) (P<0.01). (). The majority of patients (65%) also reported experiencing two or more mild exacerbations that may only have required an increase in the use of their maintenance medications, with a mean estimate of 7.2 ± 25.8 per year.
Figure 3 Mean exacerbations in the previous 12 months among COPD patients enrolled in the study.
Abbreviation: COPD, chronic obstructive pulmonary disease.
The majority (63.4%) of moderate exacerbations were treated with both oral corticosteroids and antibiotics. Among the patients whose most recent exacerbation was severe, 17.4% were treated through an ER visit alone, 24.8% were treated on an inpatient basis, 49.5% started in the ER but resulted in a hospitalization, and nine patients (8.3%) had no hospitalization or ER visit, based on the physician report. The patients who had experienced ≥1 additional exacerbation in the previous 12 months reported having a mean of 15 weeks since their previous exacerbation ().
Table 2 Exacerbation characteristics, by COPD severity and severity of last exacerbation
HRQoL
The mean observed SGRQ-C Symptoms, Activities, and Impact scores were 70.6 ± 19.0, 78.0 ± 21.9, and 54.7 ± 24.8, respectively, indicating a high level of impairment of quality of life due to COPD in these patients. Those whose most recent exacerbation was severe (versus moderate) had significantly higher Symptoms (73.6 ± 17.2 versus 69.1 ± 19.8) (P<0.05), Activity (83.6 ± 18.3 versus 75.1 ± 23.0) (P=0.001), and Impact (61.3 ± 25.9 versus 51.2 ± 23.5) (P<0.001) scores (). Patients with very severe COPD also had higher Symptoms, Activities, and Impact scores compared with patients with severe COPD (all P≤0.001). Significant differences on the SGRQ-C Symptoms, Activities, and Impact scores were seen based on the time since last exacerbation (P<0.001 for current versus <1 month, versus 1–2 months, and versus >2 months post exacerbation), with worse scores seen among patients currently experiencing exacerbation (total score: 69.8 ± 17.0; Symptoms score: 74.7 ± 17.0; and Impacts score: 60.4 ± 21.3). The SGRQ-C total scores were also significantly higher in patients whose recent exacerbation was severe versus moderate (70.3 ± 19.9 versus 61.7 ± 20.1) (P<0.001), in patients with very severe versus severe COPD (70.1 ± 21.3 versus 61.1 ± 19.0) (P<0.001), and in patients experiencing an exacerbation at the time of study versus those who were >2 months post exacerbation (69.8 ± 17.0 versus 54.6 ± 20.6) (P<0.001). The SGRQ-C total scores were significantly worse for patients who had experienced three or more exacerbations (69.5 ± 18.7) compared with patients with one (57.8 ± 20) or two (62.9 ± 21.8) exacerbations in the previous year (P<0.001). The SGRQ-C total scores were positively correlated with the number of patient-reported severe (r=0.33, P<0.001), chart-recorded severe (r=0.27, P<0.001), and total number of moderate and severe (r=0.27, P<0.001) exacerbations in the previous year. When controlling for age, race/ethnicity, and COPD severity, the severity of the last exacerbation, the time since the last exacerbation, and the total number of moderate or severe exacerbations in the previous 12 months were all significant predictors of the SGRQ-C total scores ().
Table 3 HRQoL and work productivity by COPD severity and severity of last exacerbation
Table 4 Predictors of SGRQ-C total scores and EQ-5D index
With a trend similar to the SGRQ-C scores, the EQ-5D indices for current health illustrated significantly worse health for patients recently experiencing a severe versus moderate exacerbation (0.627 ± 0.210 versus 0.698 ± 0.197, respectively) (P<0.01), for patients who had very severe versus severe COPD (0.623 ± 0.234 versus 0.707 ± 0.174, respectively) (P<0.001), and for patients who had experienced three or more exacerbations in the previous year (0.638 ± 0.212) versus two exacerbations (0.684 ± 0.204) versus one exacerbation (0.727 ± 0.175) (P<0.01) (). The EQ-5D indices for current HRQoL were most robustly correlated with the total number of chart-recorded moderate and severe exacerbations (r=−0.21, P<0.001) and patient-reported severe exacerbations (r=−0.34, P<0.001) in the previous 12 months.
When patients thought back to their last exacerbation, their EQ-5D scores averaged 0.552 (±0.283), with greater disutility in patients with very severe COPD versus severe COPD (0.494 ± 0.312 versus 0.590 ± 0.256, respectively) (P<0.01), for patients whose last exacerbation (for which they were providing the utility estimate) was severe versus moderate (0.471 ± 0.313 versus 0.595 ± 0.257, respectively) (P<0.001), and for patients who had experienced a higher frequency of exacerbations the previous year (three or more exacerbations: 0.520 ± 0.282, two exacerbations: 0.552 ± 0.306, one exacerbation: 0.610 ± 0.254). Of note, estimates for utilities during previous exacerbation were consistent with those provided for current health among the patients who were currently experiencing exacerbation (0.599 ± 0.220). When controlling for age, race/ethnicity, and COPD severity, the EQ-5D indices increased with time since exacerbation, decreased for each additional moderate/severe exacerbation in the previous year, and were higher for severe versus very severe COPD ().
Employment and work productivity
Overall, 50 (15.9%) respondents were employed at the time of survey, and employment status differed significantly by COPD severity (very severe COPD: 13 [10.5%] versus severe COPD: 37 [19.5%]) (P<0.033) but not by the severity of the most recent exacerbation. Among the employed respondents, an average of 9.0% ± 19.1% of work time was missed due to COPD, and patients estimated 38.8% ± 28.2% impairment while at work, for an estimated 42.4% ± 31.1% overall work impairment. Among all respondents, those who had recently experienced a severe exacerbation versus a moderate exacerbation had significantly more activity impairment (72.0% ± 22.4% versus 51.3% ± 28.1%) (P<0.001), as did patients whose COPD was very severe versus severe (66.5% ± 29.0% versus 53.6% ± 26.2%) (P<0.001). Significant activity impairment was also seen among patients with higher documented exacerbations in the previous year (three or more exacerbations: 64.3 ± 24.9, two exacerbations: 59.0 ± 28.9, and one exacerbation: 48.3 ± 29.6) (P<0.001). Work impairment was worse among patients experiencing an exacerbation at the time of survey (75.3% ± 8.9%), with scores improving over time (P=0.010).
The WPAI-SHP productivity loss was strongly correlated with the total number of chart-reported moderate exacerbations in the previous year (r=0.52, P<0.001). Similarly, the total number of chart-documented severe exacerbations in the previous year was positively correlated with the activity impairment domain of the WPAI-SHP (r=0.21, P<0.001). When assessing the association of work productivity to QoL, the EQ-5D indices for current health were strongly correlated with activity impairment (r =−0.54, P<0.001) and productivity loss (r=−0.50, P<0.001). The SQRQ-C total score had a moderate to strong correlation with almost all domains of the WPAI-SHP (presenteeism [r=0.48, P<0.001]; activity impairment [r=0.70, P<0.0001]; and productivity loss [r=0.47, P<0.0001]).
Discussion
The results of this study indicate that exacerbations significantly impact HRQoL and work productivity in severe and very severe COPD patients with chronic productive cough. Patients with severe and very severe COPD who recently experienced an exacerbation continued to experience diminished HRQoL, illustrating a lasting impact beyond the time of exacerbation. The findings from this study add to the growing evidence defining the exacerbation-associated burden in severe and very severe COPD patients.
The mean of 2.6 exacerbations per patient per year that was observed in this study was higher than that documented in previous studies.Citation5,Citation9 Thus, this study population allowed us to examine the burden of exacerbations in this highly severe population.
Overall, the mean SGRQ-C total scores found in this study were higher than those previously reported by Jones et al,Citation11 based on a European cross-sectional study of patients being treated in primary care settings, stratified by disease severity. While Jones et alCitation11 reported mean scores of 50.2 ± 18.6 versus 58.6 ± 17.7 for severe versus very severe COPD, respectively, the patients in the present study had mean scores over 10 points higher (61.1 ± 19.0 versus 70.1 ± 21.3 for severe versus very severe, respectively). However, there were differences in the study population as compared to that of the current study, particularly that few participants in Jones et alCitation11 had recently experienced an exacerbation, while all patients in the current population were either currently exacerbating or had recently had an exacerbation. The EQ-5D indices from the present study for severe (0.707 ± 0.174) and very severe (0.623 ± 0.234) COPD patients were quite similar to those previously reported in a review of the use of the EQ-5D in COPD.Citation18 The utility estimates derived in the present study for severe exacerbations were lower than those observed by Menn et al,Citation22 who examined health state utilities in severe COPD patients hospitalized for exacerbations and found a EQ-5D utility of 0.62 at admission and of 0.84 at discharge. This could also be due to differences in the underlying COPD severity of the patients studied, as it was also found that very severe patients reported lower utilities during their last exacerbation as compared with severe COPD patients.
Beyond statistical significance, differences in HRQoL scores can also be compared in terms of clinical significance. For example, one study reported a mean minimally important difference (MID) of 0.074 for the EQ-5D, based on data from eleven longitudinal studies.Citation23 Using this difference, there was a clinically important difference between the EQ-5D scores reported for patients’ current health as compared with their health during their last exacerbation; between the current and last exacerbation scores, by COPD severity; between the patients who had experienced one, two, or three or greater exacerbations in the previous year; and in the EQ-5D index for last exacerbation by whether that exacerbation was moderate or severe. For the SGRQ-C, the MID is 4 units.Citation24,Citation25 Using this value, there were clinically significant differences between the severe and very severe patients, between patients whose last exacerbation was moderate versus severe, and between the patients who had experienced one versus two versus three or more exacerbations in the previous year, for all SGRQ-C summary scores.
There is mixed evidence in the literature regarding the relationship between exacerbations and HRQoL. In a study conducted by Seemungal et alCitation9 examining the effect of exacerbations on HRQoL in patients with FEV1 <70% predicted, the SGRQ total and component scores were significantly worse in patients who had frequent exacerbations, and frequent exacerbations in the previous year were a predisposing factor to future frequent exacerbations (odds ratio =5.5 for the frequent versus infrequent group, P=0.001). In contrast, in a 2-year follow-up study conducted by Miravitlles et al,Citation5 exacerbations had no effect on HRQoL in severe COPD patients, but significant impairment in HRQoL of patients with moderate COPD was observed. The present findings suggest a relationship between exacerbation frequency and the SGRQ-C score, with a 2.4-unit increase in scores for each additional moderate/severe exacerbation, but this could be partially attributable to the proximity between the patients’ most recent exacerbation and the SGRQ-C measurement.
In addition to the HRQoL burden of COPD, work productivity and the ability to perform usual activities also suffer, particularly among severe and very severe COPD patients who have recently experienced an exacerbation. The impact of COPD on work productivity was consistent with a recent analysis of the 2009 National Health and Wellness Survey, which found that employed adults with COPD reported significantly lower work productivity (34.04% overall work impairment).Citation26
Several limitations of this study should be noted. The results will be most generalizable to similar patient populations, that is, patients with severe or very severe COPD within the US population, who have recently experienced a moderate to severe exacerbation. Even though random selection criteria were utilized, study designs such as ours are predisposed to selection bias. For example, the physicians in this study included those patients who could be contacted and were willing to participate, and they may have differed from those patients who did not wish to participate. Also, the participating physicians did not have the same number of patients, and some of the results may possibly be over- or underrepresented by patients from a particular practice.
Given that patients were recruited through their physicians, our patient population would exclude patients who otherwise would have met inclusion criteria, but who were not being actively treated. The patients who participated in this study were those who were still living, were not lost to follow-up, were successfully contacted, and who agreed to participate in the interview. The health status and profile of these patients may therefore differ from the US COPD population otherwise meeting the inclusion criteria. It should be noted that the utilities that were provided for the HRQoL during the patients’ last exacerbation were gathered using a modified time frame for the EQ-5D (eg, recalling back to the last exacerbation) and may have been subject to recall bias and as such, should be interpreted with caution. However, the time since last exacerbation did not appear to influence patients’ EQ-5D index score for their last exacerbation, which provides some confidence that the time elapsed between the exacerbation and the patient’s response was not a significant predictor of the patients’ EQ-5D index value for their last exacerbation. This would suggest that the recall bias with patient-reported outcomes was limited in our study, since the patient-reported outcomes were robust to time since exacerbation.
Despite these limitations, this study adds to the literature regarding the treatment of exacerbations and exacerbation-related HRQoL measured in severe to very severe COPD patients, for which there is limited previous information. A sampling methodology was used to select a sample of patients with severe and very severe COPD patients from all regions of the United States and who were treated by both pulmonologists and primary care physicians. By combining chart-reported information about exacerbations and their treatment, which may be more precise and allows for the capture of more precise data on clinical severity, with patient reported outcomes, a more complete picture of the patients’ experience is provided. These results can help to quantify the burden associated with severe and very severe COPD and provide inputs (in terms of utilities) for future economic models of treatments aimed to reduce exacerbation frequency in these types of COPD patients.
Conclusion
In conclusion, the burden of severe and very severe COPD patients is particularly high in patients who have recently experienced an exacerbation. These patients were also very likely to have experienced at least one additional moderate to severe exacerbation in the previous year, which contributes to poor HRQoL and impairs patients’ ability to be productive and undertake normal activities. Avoiding exacerbations not only avoids the HRQoL decrement attributable to the first exacerbation, but may also reduce HRQoL impact on subsequent exacerbations. Interventions aiming to further reduce exacerbation occurrences will likely have a strong impact on COPD patients’ HRQoL.
Acknowledgments
This study was funded by Forest Research Institute.
Disclosure
Assistance with the editing and formatting of the manuscript for submission by Prescott Medical Communications Group (Chicago, IL, USA) was made possible by funding from Forest Research Institute (Jersey City, NJ, USA), a wholly owned subsidiary of Forest Laboratories, Inc. (New York, NY, USA).
Caitlyn T Solem, Lavanya Sudharshan, and Xin Gao are employees of Pharmerit International and were paid consultants to Forest Research Institute in the development and execution of this study and manuscript. Cynthia Macahilig and Monica Katyal are employees of Medical Data Analytics and were paid consultants to Forest Research Institute for conducting the survey and for data collection. Shawn X Sun is an employee of Forest Research Institute, the sponsor of this study. The authors report no other conflicts of interest in this work.
References
- ManninoDMBuistASGlobal burden of COPD: risk factors, prevalence, and future trendsLancet2007370958976577317765526
- VestboJHurdSSAgustíAGGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med2013187434736522878278
- AnzuetoALeimerIKestenSImpact of frequency of COPD exacerbations on pulmonary function, health status and clinical outcomesInt J Chron Obstruct Pulmon Dis2009424525119657398
- GillissenAGlaabTLewisMBuhlRWorthHStatistical analysis of chronic obstructive pulmonary disease exacerbations in clinical studies: expectations and limitationsJ Physiol Pharmacol200960Suppl 5S7S11
- MiravitllesMFerrerMPontAIMPAC Study GroupEffect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: a 2 year follow up studyThorax200459538739515115864
- ToyELGallagherKFStanleyELSwensenARDuhMSThe economic impact of exacerbations of chronic obstructive pulmonary disease and exacerbation definition: a reviewCOPD20107321422820486821
- LlorCMolinaJNaberanKCotsJMRosFMiravitllesMEVOCA study groupExacerbations worsen the quality of life of chronic obstructive pulmonary disease patients in primary healthcareInt J Clin Pract200862458559218266710
- Rutten-van MölkenMPOostenbrinkJBTashkinDPBurkhartDMonzBUDoes quality of life of COPD patients as measured by the generic EuroQol five-dimension questionnaire differentiate between COPD severity stages?Chest200613041117112817035446
- SeemungalTADonaldsonGCPaulEABestallJCJeffriesDJWedzichaJAEffect of exacerbation on quality of life in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med19981575 Pt 1141814229603117
- StåhlELindbergAJanssonSAHealth-related quality of life is related to COPD disease severityHealth Qual Life Outcomes200535616153294
- JonesPWBrusselleGDal NegroRWPatient-centred assessment of COPD in primary care: experience from a cross-sectional study of health-related quality of life in EuropePrim Care Respir J201221332933622885563
- NiewoehnerDEThe impact of severe exacerbations on quality of life and the clinical course of chronic obstructive pulmonary diseaseAm J Med200611910 Suppl 1S38S45
- HurstJRVestboJAnzuetoASusceptibility to exacerbation in chronic obstructive pulmonary diseaseNew Engl J Med2010363121128113820843247
- Health Information Privacy [webpage on the Internet]Washington, DCUS Department of Health & Human Services Available from: http://www.hhs.gov/ocr/privacy/hipaa/understanding/index.htmlAccessed October 10, 2013
- RabeKFHurdSAnzuetoAGlobal Initiative for Chronic Obstructive Lung DiseaseGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med2007176653255517507545
- CelliBRMacNeeWATS/ERS Task ForceStandards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paperEur Respir J200423693294615219010
- BrooksREuroQol: the current state of playHealth Policy1996371537210158943
- PickardASWilkeCJungEPatelSStavemKLeeTAUse of a preference-based measure of health (EQ-5D) in COPD and asthmaRespir Med2008102451953618180151
- SzendeALeidyNKStåhlESvenssonKEstimating health utilities in patients with asthma and COPD: evidence on the performance of EQ-5D and SF-6DQual Life Res200918226727219105049
- MeguroMBarleyEASpencerSJonesPWDevelopment and validation of an improved, COPD-specific version of the St George Respiratory QuestionnaireChest2007132245646317646240
- ReillyMCZbrozekASDukesEMThe validity and reproducibility of a work productivity and activity impairment instrumentPharmacoeconomics19934535336510146874
- MennPWeberNHolleRHealth-related quality of life in patients with severe COPD hospitalized for exacerbations – comparing EQ-5D, SF-12 and SGRQHealth Qual Life Outcomes201083920398326
- WaltersSJBrazierJEComparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6DQual Life Res20051461523153216110932
- JonesPWInterpreting thresholds for a clinically significant change in health status in asthma and COPDEur Respir J200219339840411936514
- JonesPWSt George’s Respiratory Questionnaire: MCIDCOPD200521757917136966
- DiBonaventuraMdPaulose-RamRSuJThe impact of COPD on quality of life, productivity loss, and resource use among the elderly United States workforceCOPD201291465722292597