Abstract
Background
Despite the availability of national and international guidelines, evidence suggests that chronic obstructive pulmonary disease (COPD) treatment is not always prescribed according to recommendations. This study evaluated the current management of patients with COPD using a large UK primary-care database.
Methods
This analysis used electronic patient records and patient-completed questionnaires from the Optimum Patient Care Research Database. Data on current management were analyzed by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) group and presence or absence of a concomitant asthma diagnosis, in patients with a COPD diagnosis at ≥35 years of age and with spirometry results supportive of the COPD diagnosis.
Results
A total of 24,957 patients were analyzed, of whom 13,557 (54.3%) had moderate airflow limitation (GOLD Stage 2 COPD). The proportion of patients not receiving pharmacologic treatment for COPD was 17.0% in the total COPD population and 17.7% in the GOLD Stage 2 subset. Approximately 50% of patients in both cohorts were receiving inhaled corticosteroids (ICS), either in combination with a long-acting β2-agonist (LABA; 26.7% for both cohorts) or a LABA and a long-acting muscarinic antagonist (LAMA; 23.2% and 19.9%, respectively). ICS + LABA and ICS + LABA + LAMA were the most frequently used treatments in GOLD Groups A and B. Of patients without concomitant asthma, 53.7% of the total COPD population and 50.2% of the GOLD Stage 2 subset were receiving ICS. Of patients with GOLD Stage 2 COPD and no exacerbations in the previous year, 49% were prescribed ICS. A high proportion of GOLD Stage 2 COPD patients were symptomatic on their current management (36.6% with modified Medical Research Council score ≥2; 76.4% with COPD Assessment Test score ≥10).
Conclusion
COPD is not treated according to GOLD and National Institute for Health and Care Excellence recommendations in the UK primary-care setting. Some patients receive no treatment despite experiencing symptoms. Among those on treatment, most receive ICS irrespective of severity of airflow limitation, asthma diagnosis, and exacerbation history. Many patients on treatment continue to have symptoms.
Introduction
Chronic obstructive pulmonary disease (COPD) is a complex disease characterized by pulmonary as well as extrapulmonary effects. As airflow limitation poorly relates to other important clinical outcomes in COPD, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2014 strategy advocates a combined assessment to estimate current symptoms and future risk of exacerbations ().Citation1 In the UK, the National Institute for Health and Care Excellence (NICE) also recommends a multidimensional assessment to guide treatment of COPD.Citation2
In COPD, pharmacologic therapy is used to reduce symptoms, reduce frequency and severity of exacerbations, and improve health status and exercise tolerance.Citation1 Bronchodilator medications are central to the pharmacologic management of COPD.Citation1 Short-acting bronchodilators are used for immediate relief from symptoms; one or more long-acting bronchodilators (long-acting β2-agonists [LABAs] or long-acting muscarinic antagonists [LAMAs]) are recommended for long-term maintenance therapy in patients with moderate-to-severe COPD.Citation1–Citation3 Combining bronchodilators of different pharmacologic classes has the potential to improve efficacy, without increasing the risk of side effects, compared with increasing the dose of a single bronchodilator.Citation1,Citation4–Citation7
Whilst inhaled corticosteroids (ICS) are the cornerstone of asthma management, their role in COPD remains controversial.Citation8–Citation11 In COPD, the role of ICS is primarily to reduce the risk of exacerbations.Citation12 Evidence from subset analyses of large clinical trials indicates the efficacy of LABA/ICS in patients with moderate or severe COPD,Citation13 but the benefit due to the ICS component appears small compared with that of the LABA component.Citation11,Citation12 Further, the use of ICS has been associated with local and systemic side effects, including skin thinning and easy bruising,Citation12 oral candidiasis,Citation12,Citation13 increased risk of pneumonia,Citation12–Citation15 osteoporosis, early onset diabetes, cataracts,Citation12 and tuberculosis.Citation16
The GOLD 2014 strategy recommends the addition of a second bronchodilator in symptomatic patients with moderate airflow limitation, reserving the use of ICS, in addition to a maintenance therapy with a LABA, and/or a LABA and a LAMA, for patients with severe or very severe airflow limitation and/or two or more exacerbations per year.Citation1 In line with GOLD, national guidelines such as those developed by NICE recommend ICS in addition to a LABA as first choice in patients with severe airflow limitation (forced expiratory volume in 1 second [FEV1] <50% of predicted) and recurrent exacerbations and/or breathlessness.Citation2 However, there is evidence to suggest that treatment is not always prescribed according to GOLD recommendations or other national guidelines,Citation9,Citation17–Citation22 resulting in a substantial proportion of patients being treated with ICS unnecessarily and unduly exposed to the risk of serious side effects.
The objective of this study was to evaluate the current management of patients with COPD using real-life data generated in the UK primary-care setting. The study also includes a subset analysis of patients with moderate airflow limitation (FEV1 ≥50–<80% predicted) as defined by NICE 2010 guidelines, which corresponds to GOLD Stage 2.Citation23 This population forms the majority of patients treated in primary care, and is therefore relevant in this analysis of prescribing patterns of UK general practitioners.
Methods
Data for patients with a diagnosis of COPD were extracted from the Optimum Patient Care Research Database (OPCRD) on May 20, 2013. Only data for patients with a COPD diagnosis (quality and outcomes framework diagnostic code),Citation24 1 year of practice data prior to last data extraction and no leaving date, spirometry supportive of COPD diagnosis within 5 years of data extraction, and last data extraction date after 2009 were included in this retrospective analysis. Data from patients younger than 35 years at diagnosis were excluded.
The OPCRD is a quality-controlled, longitudinal, primary-care, respiratory-focused database containing anonymous data from general practices in the UK. The OPCRD has been approved by Trent Multicentre Research Ethics Committee for clinical research use (approval reference 10/H0405/3). The database combines routine data from electronic patient records with linked patient-reported data collected using disease-specific questionnaires. Routine clinical data, including patient demographics, standard COPD comorbidities, exacerbation history, modified Medical Research Council (mMRC) score,Citation1 and current therapy, were extracted from primary-care practice management systems. In addition, a proportion of patients with relevant disease codes were invited to complete validated disease assessment questionnaires, sent via a secure mailing house, containing questions to calculate COPD Assessment Test (CAT)Citation25 and mMRC scores. Questionnaire data were added to the database anonymously. The mMRC questionnaire and CAT are provided in the supplementary materials ( and ).
Data were analyzed according to GOLD groupCitation26 and presence or absence of a concomitant asthma diagnosis. In a subset of patients with moderate airflow limitation,Citation2,Citation23 data were also analyzed by exacerbation history (moderate and severe exacerbation rate), mMRC score, and CAT score. mMRC scores were taken both from routine data (ie, abstracted from the medical record) and patient questionnaires, with the most recent scores taking precedence. CAT scores were obtained from patient questionnaires. GOLD groups were calculated with mMRC rather than CAT scores, unless specified otherwise.
Moderate and severe COPD exacerbations were defined as unscheduled hospital admission/emergency hospital attendance for COPD (definite code) or lower respiratory-related events (ie, with a lower respiratory read code), or lower respiratory illnesses treated with antibiotics and/or acute use of oral steroids. Exacerbation rates were calculated for the year prior to most recent data extraction. Events were considered to be the result of the same exacerbation and only counted once if any of the three elements (hospitalization, oral steroid prescription, or lower respiratory tract infection consultation) occurred within 2 weeks of another.
Results
Patient selection
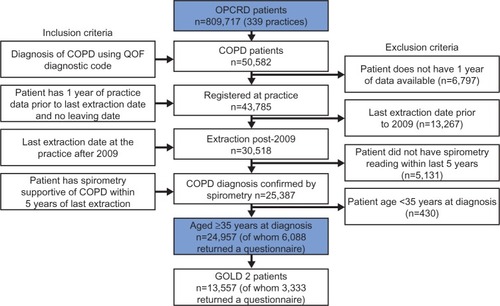
Data from 50,582 patients with COPD were extracted from 339 practices. Among these patients, 24,957 (49.3%) met the inclusion criteria and were included in the analysis (). Out of all the patients included in the analysis, 12,967 (52.0%) were sent questionnaires, which were returned by 6,088 patients (46.9%). The GOLD Stage 2 subset included 13,557 patients; 7,055 were sent a questionnaire, and 3,333 (47.2%) returned the questionnaire.
Demographics
The mean age of the total COPD population was 71.4 years; the majority of patients were <75 years of age (59.7%), male (53.0%), and ex-smokers (56.2%) (). The distribution of patients according to GOLD stages was 15.8% in Stage 1, 54.3% in Stage 2, 24.6% in Stage 3, and 5.3% in Stage 4. Based on degree of airflow limitation, symptoms (mMRC score), and history of exacerbations, the 23,294 (93.3%) patients with known mMRC score were identified as being in GOLD Group A (39.2%), Group B (20.0%), Group C (19.0%), or Group D (21.7%). Of the patients in the high-risk groups, C and D, 57.6% and 59.2%, respectively, were categorized as high risk based on severity of airflow limitation and not exacerbation history. The use of CAT score to assess symptoms resulted in a different distribution, with 13.4%, 46.1%, 4.6%, and 35.9% of the 5,882 (23.6%) patients with known CAT score classified as Group A, B, C, or D, respectively. There were no major demographic differences across GOLD groups in terms of age, sex, and smoking status (). The prevalence of comorbidities was similar across GOLD groups, except for ischemic heart disease, which was more prevalent in patients in Groups B and D (). The combined percentage of overweight and obese patients was higher in Group B than in any other GOLD group.
Table 1 Patient demographics for the total COPD population split by GOLD group
Demographic characteristics of patients with GOLD Stage 2 COPD were similar to those of patients in the total COPD population (). The mean age was 70.9 years and 52.2% of patients were male. The majority of patients (54.7%) were ex-smokers. The most frequently occurring comorbidities in patients with GOLD Stage 2 COPD were the same as in the total COPD population. Patients with known GOLD groups (n=12,730) were identified as being in Group A (55.0%), Group B (29.6%), Group C (8.4%), or Group D (7.1%) based on mMRC score. Patients (n=3,227) were classified as being in Group A (18.7%), Group B (67.2%), Group C (2.0%), or Group D (12.2%) when symptoms were assessed using CAT score.
Table 2 Patient demographics for the GOLD Stage 2 population split by GOLD group
Demographic characteristics of patients who were responders and nonresponders to the study questionnaires are illustrated in the supplementary materials () for total COPD population and GOLD Stage 2 subset. Overall, patients who returned the questionnaire, as compared with those who did not, tended to be slightly older (72.4 versus 70.5 years) and were more likely to be male (56.1% versus 52.5%) and ex-smokers (61.7% versus 52.1%) but less likely to be current smokers (24.7% versus 33.8%); differences in GOLD group categorization were minor. A similar pattern was evident for patients categorized at GOLD Stage 2 who did, versus did not, return the questionnaire ().
Clinical characteristics
Of the patients in the total COPD population, 61.0% had no exacerbations and 16.9% had two or more moderate or severe exacerbations in the year prior to data extraction. The majority of patients with no exacerbations were in Group A (45.4%), while 25.9% of patients were classified as being in Groups C or D based on severity of airflow limitation (). Of the patients with exacerbations in the year prior to data extraction, 57.2% were in Groups C or D.
Figure 2 Distribution of GOLD groups in patients without and with moderate and severe exacerbations in the year prior to data extraction for total COPD population (A) and GOLD Stage 2 subset (B).
Abbreviations: COPD, chronic obstructive pulmonary disease; GOLD, Global Initiative for Chronic Obstructive Lung Disease.
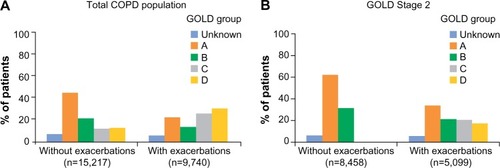
Patients with GOLD Stage 2 COPD displayed similar clinical characteristics to those in the overall cohort in terms of total exacerbation rate. In the GOLD Stage 2 subset, 62.4% of patients had no exacerbations and 15.4% had two or more moderate or severe exacerbations in the year prior to data extraction. Of the patients with no exacerbations, 62.3% were classified as being in Group A and 31.5% were classified as being in Group B. The majority of patients with exacerbations in the year prior to data extraction were in Group A (34.0%; ). However, 38.5% of patients were classified as being in Groups C or D and experienced two or more exacerbations in the year previous to data extraction, despite having moderate airflow limitation.
In the total COPD population, among patients with a known mMRC score, the mean (standard deviation [SD]) mMRC score was 1.5 (1.0); 40.9% of patients had an mMRC score of 1 and 41.7% had a score ≥2. In the GOLD Stage 2 subset, among patients with a known mMRC score, the mean (SD) mMRC score was 1.3 (1.0); 43.7% of patients had an mMRC score of 1 and 36.6% had a score ≥2. Among patients who returned a questionnaire and had a known CAT score, the mean (SD) CAT score was 17.1 (9.0) in the total COPD population and 16.3 (8.9) in the GOLD Stage 2 subset. Of the patients with a known CAT score, 79.0% and 76.4% had a CAT score ≥10 in the total COPD population and in the GOLD Stage 2 subset, respectively.
Current management
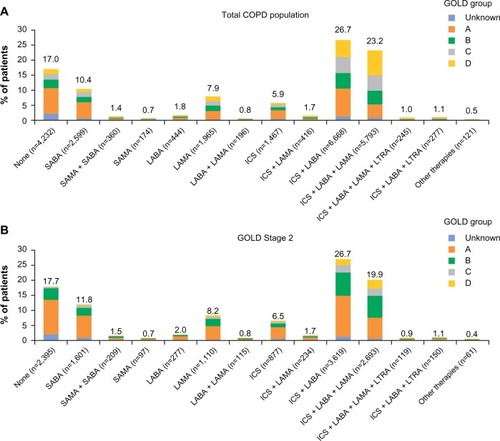
A similar proportion of patients in the total COPD population (n=24,957) and GOLD Stage 2 subset (n=13,557) were not receiving pharmacologic treatment for COPD (17.0% and 17.7%, respectively; ). Approximately 50% of patients in the total COPD population and GOLD Stage 2 subset were receiving ICS (), either in combination with a LABA (26.7% for both cohorts) or in combination with a LABA and a LAMA (23.2% and 19.9%, respectively). In both cohorts, ICS + LABA combinations were the most frequently used treatment in Groups A and B (). Of the total COPD population, 9.3% and 5.1% of Group A and B patients were receiving ICS + LABA. Of the patients with GOLD Stage 2 COPD, 13.5% and 7.6% of Group A and B patients, respectively, were given ICS + LABA. A small proportion of patients across all GOLD groups were using LABA or LAMA monotherapy in the total COPD population (1.8% and 7.9%, respectively) and GOLD Stage 2 subset (2.0% and 8.2%; ).
Figure 3 Current management for total COPD population (A) and GOLD Stage 2 subset (B) by GOLD groups.
Abbreviations: COPD, chronic obstructive pulmonary disease; GOLD, Global Initiative for Chronic Obstructive Lung Disease; ICS, inhaled corticosteroids; LABA, long-acting β2-agonist; LAMA, long-acting muscarinic antagonist; LTRA, leukotriene receptor antagonist; SAMA, short-acting muscarinic antagonist; SABA, short-acting β2-agonist.
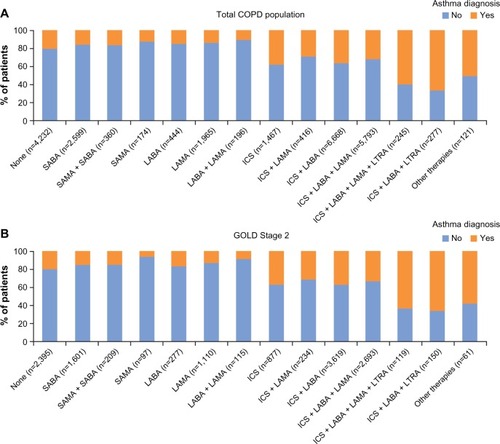
Current management was analyzed based on the presence or absence of a concomitant asthma diagnosis. Of the patients without a concomitant diagnosis of asthma in the total COPD population (n=17,930) and GOLD Stage 2 subset (n=9,814) 53.7% and 50.2%, respectively, were receiving ICS. Among ICS-containing regimens, ICS + LAMA, ICS + LABA, and ICS + LABA + LAMA were the most frequently used treatment options (total COPD population: 70.7%, 63.9%, and 68.1%, respectively; GOLD Stage 2 subset: 68.8%, 63.2%, and 67.5%, respectively; ).
Figure 4 Current management by concomitant asthma diagnosis for total COPD population (A) and GOLD Stage 2 subset (B).
Abbreviations: COPD, chronic obstructive pulmonary disease; GOLD, Global Initiative for Chronic Obstructive Lung Disease; ICS, inhaled corticosteroids; LABA, long-acting β2-agonist; LAMA, long-acting muscarinic antagonist; LTRA, leukotriene receptor antagonist; SAMA, short-acting muscarinic antagonist; SABA, short-acting β2-agonist.
GOLD Stage 2 subset analyses
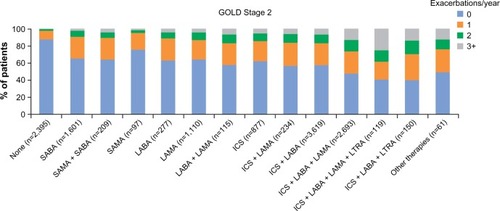
Additional analyses were conducted in the GOLD Stage 2 subset. illustrates current management by moderate and severe exacerbation rate. Among patients who experienced no exacerbations (n=8,458) or one exacerbation (n=3,006) in the year prior to extraction, 49.0% and 64.1%, respectively, were receiving ICS, either alone or in combination with long-acting bronchodilators. Of those patients receiving no treatment, 87.3% experienced no exacerbations in the year prior to data extraction, while of those patients receiving triple therapy (ICS + LABA + LAMA or ICS + LABA + leukotriene receptor antagonist) or quadruple therapy (ICS + LABA + LAMA + leukotriene receptor antagonist), more than 50% experienced one or more exacerbations in the year prior to extraction ().
Figure 5 Current management by moderate and severe exacerbation rate in the year prior to data extraction for the GOLD Stage 2 subset.
Abbreviations: GOLD, Global Initiative for Chronic Obstructive Lung Disease; ICS, inhaled corticosteroids; LABA, long-acting β2-agonist; LAMA, long-acting muscarinic antagonist; LTRA, leukotriene receptor antagonist; SAMA, short-acting muscarinic antagonist; SABA, short-acting β2-agonist.
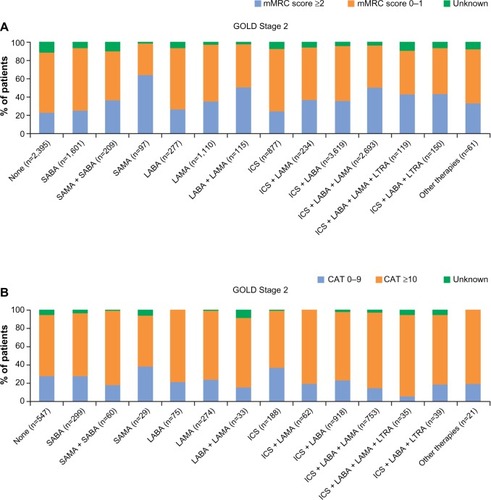
Further, current management in the GOLD Stage 2 subset was analyzed based on mMRC and CAT scores to evaluate the proportion of patients experiencing symptoms while on treatment. An mMRC score ≥2 was recorded for 22.7% of patients receiving no treatment, 35.4% of patients receiving LAMA monotherapy, and 35.6% and 50.2% of patients receiving ICS + LABA and ICS + LABA + LAMA, respectively (). A CAT score ≥10 was recorded for 66.7% of patients receiving no treatment, 74.5% of patients on LAMA monotherapy, and 74.4% and 81.9% of patients receiving ICS + LABA and ICS + LABA + LAMA, respectively ().
Figure 6 Current management by mMRC score (A) and CAT score (B) for the GOLD Stage 2 subset.
Abbreviations: CAT, COPD Assessment Test; COPD, chronic obstructive pulmonary disease; GOLD, Global Initiative for Chronic Obstructive Lung Disease; ICS, inhaled corticosteroids; LABA, long-acting β2-agonist; LAMA, long-acting muscarinic antagonist; mMRC, modified Medical Research Council; LTRA, leukotriene receptor antagonist; SAMA, short-acting muscarinic antagonist; SABA, short-acting β2-agonist.
Discussion
The present study, one of the largest to evaluate real-life treatment patterns of COPD in the UK, indicates that COPD is often not managed in primary care according to the most recent recommendations and guidelines. In our analysis, a substantial proportion of patients with COPD did not receive any treatment despite experiencing symptoms or a history of exacerbations. Among patients receiving treatment, ICS were prescribed to patients irrespective of severity of airflow limitation, exacerbation history, and asthma diagnosis.
NICE recommends a LABA/ICS combination for patients with severe airflow limitation (FEV1 <50% predicted) and/or persistent exacerbations/breathlessnessCitation2 whereas the GOLD 2014 strategy document currently recommends LABA/ICS combinations for patients in Groups C and D.Citation1 The only exception to these recommendations on the use of ICS is for patients with overlap phenotype of asthma and COPD, in whom ICS are indicated.Citation9 Notably, a considerable proportion of patients in GOLD Groups A and B (mild-to-moderate airflow limitation and low risk of exacerbations) in the total COPD population, as well as in the GOLD Stage 2 subset, were using ICS in combination with long-acting bronchodilators; conversely, only a small proportion of these patients were treated exclusively with long-acting bronchodilators, either as mono- or combination therapy. Consistent with this finding, approximately half of the patients who had not experienced an exacerbation in the year prior to data extraction were receiving ICS. The majority of patients without a concomitant diagnosis of asthma were also being treated with ICS, suggesting that ICS were overprescribed. In the total COPD population, 17% of patients were not receiving pharmacologic treatment for COPD. This is greater than the proportion of adults diagnosed with diabetes who have been reported to not use recommended oral medications or insulin (approximately 13%),Citation27 but is lower compared with other chronic diseases such as multiple sclerosis and hypertension in which between one-third and two-thirds of patients have been reported to receive no approved treatment for their conditions.Citation28–Citation31
Our findings are supported by several studies analyzing the adherence to recommendations and guidelines for the management of COPD. Recently, data from a retrospective study revealed that most patients with COPD use ICS, irrespective of airflow limitation and exacerbation rate.Citation32 In addition, data from the Adelphi Respiratory Disease Specific Programme® (Adelphi, Macclesfield, UK), a multinational, cross-sectional market-research survey that generates data from current clinical practice, showed that a high proportion of low-risk patients are treated with a LABA/ICS.Citation33 Studies in other European countries have also shown a tendency for ICS to be prescribed outside of current recommendations in COPD, indicating that poor adherence to treatment guidelines among primary-care physicians is widespread.Citation9,Citation20,Citation22,Citation34–Citation37
Several factors can contribute to this disconnect between current real-life practice and evidence-based treatment recommendations. Two studies assessing the management of COPD in the US recently highlighted several barriers to implementing GOLD recommendations in primary care.Citation38,Citation39 One important barrier identified by Perez et alCitation38 was poor familiarity with GOLD recommendations, which was found to be associated with nonadherence to specific recommendations on ICS and long-acting bronchodilators. Further, the study by Salinas et alCitation39 found that physicians who have difficulty assessing response to therapy were less likely to adhere to recommendations on long-acting bronchodilator use. As suggested by the authors of the study, this may be because long-acting bronchodilators produce subtle but meaningful improvements, which can be difficult for physicians to recognize.Citation39 Moreover, physicians may not recognize a benefit of therapy in individual patients who have infrequent exacerbations, as decreased frequency of exacerbations is an important measure of the efficacy of inhaled therapies. Indeed, in our study, 61% of the total population did not experience an exacerbation in the preceding year, including many patients classified as being in Groups C and D. This makes the assessment of treatment benefit difficult for all severities of COPD.
Difficulties in distinguishing between asthma and COPD in adults with airways disease, or in establishing when these two conditions coexist, could also play an important role. The CADRE (COPD and asthma diagnostic/management reassessment) study among UK primary-care practices found a high rate of misdiagnosis among adults with airways disease, with a tendency to overdiagnose asthma and underdiagnose COPD.Citation40 A high proportion of patients diagnosed with asthma (54.3%) and mixed disease (45.4%) had their diagnosis changed, with the majority of them diagnosed with COPD after review. These findings indicate a lack of precision in diagnosing the ‘chesty’ patient in primary care. Data from Spanish practices also confirm the difficulty of accurately diagnosing COPD in primary care. Primary-care physicians using clinical criteria and spirometry had difficulty reaching a diagnosis for up to 20% of patients with chronic respiratory symptoms who were taking inhaled medication.Citation37 The misdiagnosis of respiratory disease may lead to inadequate treatment and overuse of ICSCitation21,Citation22,Citation37 particularly for patients with COPD.
The burden of symptoms reported by patients, which affects the physician-perceived severity of the disease, could also have a considerable impact on treatment choices. Physicians may evaluate disease as more or less severe based on their overall clinical judgment rather than guidelines. Physicians may, therefore, be more willing to prescribe treatments outside of recommendations when confronted by symptomatic patients, resulting in ICS being prescribed for reasons other than severity of airflow limitation or exacerbation risk. Indeed, a recent study of prescription drugs from UK general practices suggests that over 37% of COPD patients were overtreated (ie, according to GOLD 2009 recommendations) and, of those, 96% were overtreated with ICS.Citation41 As shown by our data, a substantial proportion of GOLD Stage 2 patients in the UK are symptomatic on treatment, irrespective of their current management. In line with our findings, studies have suggested that many patients with moderate COPD may remain symptomatic despite LAMA monotherapyCitation42–Citation44 or LABA/ICS treatment.Citation45 Interestingly, our analysis suggests that use of CAT, compared with mMRC, increased the number of patients in more symptomatic groups (Groups B and D), potentially because the CAT assessment considers not only dyspnea, but also other COPD symptoms and health status. This difference in GOLD group distribution depending on whether the mMRC score or CAT score is used highlights the difficulty facing primary-care physicians when making treatment decisions in real-life practice and illustrates how guidelines may only provide limited assistance.
It is important to note that in some cases the discordance between the current treatment recommendations and real-life clinical practice may be because of individual patients’ needs and comorbidities. Indeed, the NICE guidelines state that, “Treatment and care should take into account patients’ needs and preferences.”Citation2 In addition, our study provides a snapshot of current practice and may reflect therapy that has been long-standing and perceived as ‘effective’ by both the patient and physician. Thus, in some cases, depending on individual factors, it may be reasonable for patients to continue with existing therapy despite the updated treatment recommendations.
The baseline demographic and disease characteristics of the patients analyzed in our study provide interesting insights. The prevalence of cigarette smoking (approximately 30% in both the total COPD population and GOLD Stage 2 subset) is rather high considering that smoking cessation is the single most important intervention for all COPD patients who continue to smoke and has the greatest capacity to influence the natural history of the disease.Citation1 The prevalence of anxiety or depression was also approximately 30% in both study populations. This may be expected to influence treatment outcomes because depression, in particular, is associated with poor compliance and negatively impacts on smoking cessation.Citation46 The proportion of patients with a history of pneumonia increased steadily from GOLD Groups A (6.2%) through D (11.9%), which is as expected and supports the reliability of GOLD Group categorization in the study. The majority of patients in Groups C and D were classified in these groups based on their severity of airflow limitation rather than exacerbation history, which is in accordance with the findings of other cohort studies.Citation47
Although it is often reported that most COPD patients remain undiagnosed until their disease progresses to severe stages (FEV1 <50% predicted),Citation48–Citation50 in our study more than 50% of patients with spirometry-confirmed COPD had GOLD Stage 2 disease. This is consistent with other retrospective cohort studies in the UK. A recent analysis of a large database of primary-care COPD patients from 80 general practices across the UK showed that GOLD Stage 2 disease was present in 52% of patients.Citation51 In an analysis of primary-and secondary-care data pooled from the OPCRD and the General Practice Research Database, 45% of patients with FEV1 data available had GOLD Stage 2 disease.Citation52 The proportion of patients with a lesser degree of airflow obstruction at the time of COPD diagnosis increased over the 20-year study period, which may be due to increased use of diagnostic spirometry and recent COPD policy and practice guidance aimed to improve COPD diagnosis.Citation52
Several study limitations must be considered when interpreting our results. As this is a retrospective analysis, it is not possible to conclude whether the treatment patterns are a response to symptoms or whether the symptoms show lack of response to treatment. Further, data on adherence have not been analyzed, so it cannot be established whether the presence of symptoms in patients on treatment is owing to inadequate disease control as a result of suboptimal treatment or poor adherence to prescribed medications, or both. The analyses using CAT scores were conducted in a subset of patients because, unlike mMRC scores that were determined from questionnaire data or patient records, CAT scores could only be calculated from patient questionnaires, which were not available for all patients. Potential differences between the characteristics of patients who returned questionnaires and those who did not cannot be discounted as a possible source of bias.
In summary, this analysis of UK prescribing patterns indicates that COPD management choices do not usually follow GOLD recommendations and NICE guidelines, in particular those relating to the use of ICS and long-acting bronchodilators, which results in a substantial proportion of patients not being treated or not receiving the most appropriate medication. Further, it has been shown that many patients experience symptoms despite treatment. In light of the evidence provided by this analysis, evidence-based prescription of COPD therapies should be encouraged among UK primary-care physicians in order to limit the risks and costs associated with undertreatment and overtreatment and to improve patient outcomes.
Acknowledgments
The analyses reported in this manuscript were funded by Novartis Pharma AG (Basel, Switzerland) and were conducted by Research in Real-Life Ltd (Cambridge, UK), an independent company. The authors were assisted in the preparation of the manuscript by Roberta Sottocornola, a professional medical writer contracted to CircleScience (Tytherington, UK), part of KnowledgePoint360, an Ashfield Healthcare Communications (Ashby de la Zouch, UK) company. Writing support was funded by Novartis Pharma AG.
Supplementary materials
Figure S1 Model of symptom/risk evaluation of COPD.
Notes: When assessing risk, choose the highest risk according to GOLD stage or exacerbation history (one or more hospitalizations for COPD exacerbations should be considered high risk). GOLD 1, 2, 3, and 4 correspond to mild (FEV1 ≥80% predicted), moderate (50% ≤ FEV1 <80% predicted), severe (30% ≤ FEV1 <50% predicted), and very severe (FEV1 <30% predicted) airflow limitation, respectively. Reproduced from the Global Strategy for Diagnosis, Management and Prevention of COPD 2014. Copyright © Global Initiative for Chronic Obstructive Lung Disease (GOLD), all rights reserved. Available from http://www.goldcopd.org.Citation1
Abbreviations: CAT, COPD Assessment Test; COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in 1 second; GOLD, Global Initiative for Chronic Obstructive Lung Disease; mMRC, modified Medical Research Council.
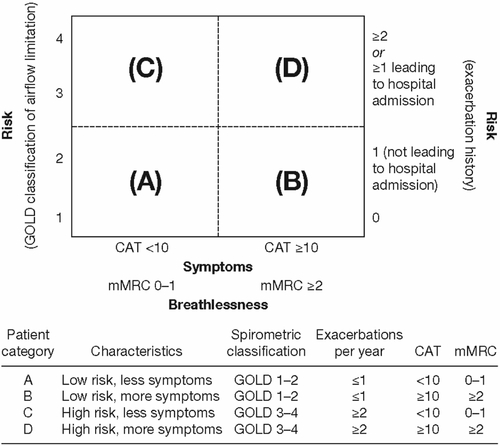
Figure S2 Modified Medical Research Council questionnaire for assessing the severity of breathlessness.
Reproduced from the Global Strategy for Diagnosis, Management and Prevention of COPD 2014. Copyright © Global Initiative for Chronic Obstructive Lung Disease (GOLD), all rights reserved. Available from http://www.goldcopd.org.Citation1
Abbreviation: mMRC, modified Medical Research Council.
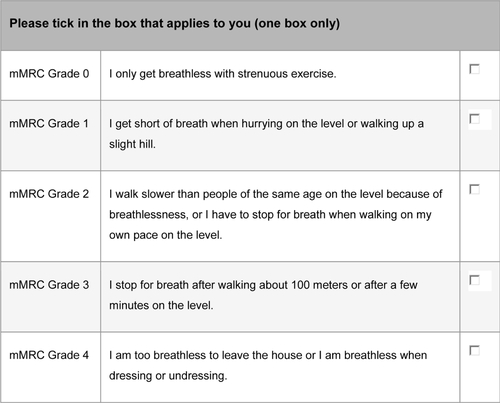
Figure S3 COPD Assessment Test.
Notes: The COPD Assessment Test score is calculated as the sum of the responses present. If more than two responses are missing, a score cannot be calculated; when one or two items are missing their scores can be set to the average of the nonmissing item scores. Reproduced with permission. COPD Assessment Test and CAT logo is a trade mark of the GlaxoSmithKline group of companies. © 2009 GlaxoSmithKline group of companies. All rights reserved.Citation2
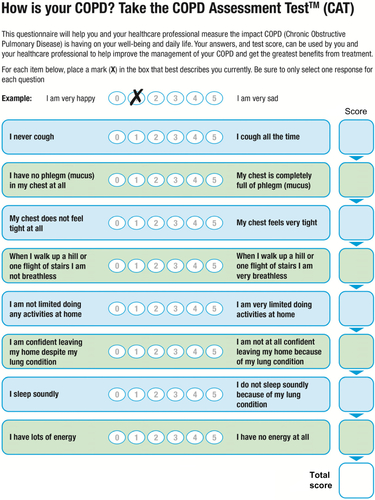
Table S1 Characteristics of patients with COPD who were responders or nonresponders to the study questionnaires
References
- Global Initiative for Chronic Obstructive Lung Disease (GOLD 2014)Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease: Updated 2014Global Initiative for Chronic Obstructive Lung Disease2014 Available from: http://www.goldcopd.org/uploads/users/files/GOLD_Report_2014.pdfAccessed June 18, 2014
- JonesPWHardingGBerryPWiklundIChenWHKline LeidyNDevelopment and first validation of the COPD Assessment TestEur Respir J200934364865419720809
Disclosure
DP has served on advisory boards for Aerocrine, Almirall, Amgen, AstraZeneca, Boehringer Ingelheim, Chiesi, Meda, Mundipharma, Napp, Novartis, and Teva. He has consultant arrangements with Almirall, Amgen, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Meda, Mundipharma, Napp, Novartis, Pfizer, and Teva. He or his research team has received grants (or grants pending) and support for research in respiratory disease from the following organizations in the last 5 years: UK National Health Service, British Lung Foundation, Aerocrine, AstraZeneca, Boehringer Ingelheim, Chiesi, Eli Lilly, GlaxoSmithKline, Meda, Merck, Mundipharma, Novartis, Orion, Pfizer, Respiratory Effectiveness Group, Takeda, Teva, and Zentiva. He has received unrestricted funding for investigator-initiated studies from Aerocrine, AKL Ltd, Almirall, Boehringer Ingelheim, Chiesi, Meda, Mundipharma, Napp, Novartis, Orion, Takeda, Teva, and Zentiva. He has received funding for patient enrollment or completion of research from Almirall, Chiesi, Teva, and Zentiva. He has received payments for lectures/speaking from Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, GlaxoSmithKline, Kyorin, Meda, Merck, Mundipharma, Novartis, Pfizer, Skyepharma, Takeda, and Teva; travel/accommodations/meeting expenses from Aerocrine, Boehringer Ingelheim, Mundipharma, Napp, Novartis, and Teva; manuscript preparation from Mundipharma and Teva; and development of educational materials from GlaxoSmithKline and Novartis. He has patents and shares with AKL Ltd and owns 80% of Research in Real-Life Ltd and its subsidiary social enterprise Optimum Patient Care.
GB has received lecture fees from AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Novartis, and Pfizer. He is a member of advisory boards for AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, and Novartis.
KG-J has spoken on behalf of, or acted as a consultant for, Almirall, Chiesi, AstraZeneca, GlaxoSmithKline, Boehringer Ingelheim, Merck Sharp & Dohme, Napp/Mundipharma, and Novartis.
RJ has been paid to take part in educational activities related to COPD for Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Novartis, Nutricia, and Pfizer in the last 3 years. He is consultant to COPDexchange educational programs supported by Boehringer Ingelheim, to the iCOPD project supported by Almirall, and to Health Intelligence.
MM has received speaker fees from AstraZeneca, Bayer Schering, Boehringer Ingelheim, Merck Sharp and Dohme, Novartis, Pfizer, Takeda-Nycomed, and Talecris-Grifols and consulting fees from Almirall, AstraZeneca, Bayer Schering, Boehringer Ingelheim, GlaxoSmithKline, Merck Sharp and Dohme, Novartis, Pfizer, Talecris-Grifols, and Takeda-Nycomed.
AR has received reimbursement for attending symposia, fees for speaking, fees for organizing education, funds for research, and fees for consulting from AstraZeneca, Boehringer Ingelheim/Pfizer, Chiesi, GlaxoSmithKline, Novartis, and Nycomed/Tanaka.
DW, CH, VLA, RS, and KB are employees of Research in Real-Life Ltd, which has conducted paid research in respiratory disease on behalf of the following organizations in the past 5 years: Aerocrine, AKL Ltd, Almirall, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Meda, Mundipharma, Napp, Novartis, Orion, Takeda, Teva, Zentiva.
References
- Global Initiative for Chronic Obstructive Lung Disease (GOLD 2014)Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease: Updated 2014Global Initiative for Chronic Obstructive Lung Disease2014 Available from: http://www.goldcopd.org/uploads/users/files/GOLD_Report_2014.pdfAccessed June 18, 2014
- National Institute for Health and Care ExcellenceNICE Guidelines [CG101]: Chronic Obstructive Pulmonary Disease: Management of Chronic Obstructive Pulmonary Disease in Adults in Primary and Secondary Care (Partial Update)LondonNational Institute for Health and Care Excellence2010 Available from: http://www.nice.org.uk/guidance/CG101Accessed June 18, 2014
- CazzolaMMateraMGLong-acting bronchodilators are the first-choice option for the treatment of stable COPDChest2004125191114718412
- VogelmeierCKardosPHarariSGansSJStengleinSThirlwellJFormoterol mono- and combination therapy with tiotropium in patients with COPD: a 6-month studyRespir Med2008102111511152018804362
- Van NoordJAAumannJLJanssensECombining tiotropium and salmeterol in COPD: effects on airflow obstruction and symptomsRespir Med20101047995100420303247
- MahlerDAD’UrzoABatemanEDConcurrent use of indacaterol plus tiotropium in patients with COPD provides superior bronchodilation compared with tiotropium alone: a randomised, double-blind comparisonThorax201267978178822544891
- BatemanEDFergusonGTBarnesNDual bronchodilation with QVA149 versus single bronchodilator therapy: the SHINE studyEur Respir J20134261484149423722616
- AntónEHow and when to use inhaled corticosteroids in chronic obstructive pulmonary disease?Expert Rev Respir Med20137Suppl 2253223551021
- MiravitllesMSoler-CataluñaJJCalleMA new approach to grading and treating COPD based on clinical phenotypes: summary of the Spanish COPD guidelines (GesEPOC)Prim Care Respir J201322111712123443227
- PostmaDSCalverleyPInhaled corticosteroids in COPD: a case in favourEur Respir J2009341101219567598
- SuissaSBarnesPJInhaled corticosteroids in COPD: the case againstEur Respir J2009341131619567599
- PriceDYawnBBrusselleGRossiARisk-to-benefit ratio of inhaled corticosteroids in patients with COPDPrim Care Respir J20132219210023135217
- NanniniLJLassersonTJPoolePCombined corticosteroid and long-acting beta(2)-agonist in one inhaler versus long-acting beta(2)-agonists for chronic obstructive pulmonary diseaseCochrane Database Syst Rev20129CD00682922972099
- CrimCCalverleyPMAndersonJAPneumonia risk in COPD patients receiving inhaled corticosteroids alone or in combination: TORCH study resultsEur Respir J200934364164719443528
- SuissaSAuthor’s response to letter on number needed to treat in COPD: exacerbations versus pneumoniasThorax201368988288323935172
- KimJHParkJSKimKHJeongHCKimEKLeeJHInhaled corticosteroid is associated with an increased risk of TB in patients with COPDChest201314341018102423079688
- CorradoARossiAHow far is real life from COPD therapy guidelines? An Italian observational studyRespir Med2012106798999722483189
- FitchKIwasakiKPyensonBPlauschinatCZhangJVariation in adherence with Global Initiative for Chronic Obstructive Lung Disease (GOLD) drug therapy guidelines: a retrospective actuarial claims data analysisCurr Med Res Opin20112771425142921599554
- JebrakGCOPD routine management in France: are guidelines used in clinical practice?Rev Mal Respir20102711118 French [with English abstract]20146947
- JochmannANeubauerFMiedingerDGeneral practitioners’ adherence to the COPD GOLD guidelines: baseline data of the Swiss COPD Cohort StudySwiss Med Wkly Epub4212010
- JonesRCDickson-SpillmannMMatherMJMarksDShackellBSAccuracy of diagnostic registers and management of chronic obstructive pulmonary disease: the Devon primary care auditRespir Res200896218710575
- LucasAESmeenkFWSmeeleIJvan SchayckCPOvertreatment with inhaled corticosteroids and diagnostic problems in primary care patients, an exploratory studyFam Pract2008252869118304973
- Global Initiative for Chronic Obstructive Lung Disease (GOLD 2007)Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease: Updated December 2007Global Initiative for Chronic Obstructive Lung Disease2007 Available from: http://www.goldcopd.org/uploads/users/files/GOLDReport07_0108.pdfAccessed June 18, 2014
- British Medical Association2014/15 General Medical Services (GMS) Contract Quality and Outcomes Framework (QOF)LondonBritish Medical Association2014 Available from: http://bma.org.uk/practical-support-at-work/contracts/independent-contractors/qof-guidanceAccessed June 18, 2014
- JonesPWHardingGBerryPWiklundIChenWHKline LeidyNDevelopment and first validation of the COPD Assessment TestEur Respir J200934364865419720809
- Global Initiative for Chronic Obstructive Lung Disease (GOLD 2013)Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease: Updated 2013Global Initiative for Chronic Obstructive Lung Disease2013 Available from: http://www.goldcopd.org/uploads/users/files/GOLD_Report_2013_Feb20.pdfAccessed June 18, 2014
- HillSCMillerGESingMAdults with diagnosed and untreated diabetes: who are they? How can we reach them?J Health Care Poor Underserved20112241221123822080705
- AvasaralaJRO’DonovanCARoachSECamachoFFeldmanSRAnalysis of NAMCS data for multiple sclerosis, 1998–2004BMC Med20075617411425
- GavrasHPIssues in hypertension: drug tolerability and special populationsAm J Hypertens2001147 Pt 2231S236S11459211
- Harris InteractiveMany Who Suffer From Multiple Sclerosis (MS) Are Not Getting Treatment They Could Benefit From2001 Available from: http://www.mult-sclerosis.org/news/May2001/HarrisPollPwMSundertreated.htmlAccessed June 18, 2014
- WongNDLopezVAL’ItalienGChenRKlineSEFranklinSSInadequate control of hypertension in US adults with cardiovascular disease comorbidities in 2003–2004Arch Intern Med2007167222431243618071164
- FranssenFMSpruitMAWoutersEFDeterminants of polypharmacy and compliance with GOLD guidelines in patients with chronic obstructive pulmonary diseaseInt J Chron Obstruct Pulmon Dis2011649350122069360
- SmallMBroomfieldSHigginsVQuantification and treatment patterns of real-world patients classified by the GOLD 2011 strategyPoster presented at: 22nd Annual Congress of the European Respiratory SocietySeptember 1–5, 2012Vienna, Austria
- DecramerMBartschPPauwelsRYernaultJCManagement of COPD according to guidelines. A national survey among Belgian physiciansMonaldi Arch Chest Dis2003591628014533285
- GlaabTBanikNRutschmannOTWenckerMNational survey of guideline-compliant COPD management among pneumologists and primary care physiciansCOPD20063314114817240616
- MiravitllesMBrosaMVelascoMAn economic analysis of pharmacological treatment of COPD in SpainRespir Med2009103571472119168340
- MiravitllesMAndreuIRomeroYSitjarSAltésAAntonEDifficulties in differential diagnosis of COPD and asthma in primary careBr J Gen Pract201262595e68e7522520766
- PerezXWisniveskyJPLurslurchachaiLKleinmanLCKronishIMBarriers to adherence to COPD guidelines among primary care providersRespir Med2012106337438122000501
- SalinasGDWilliamsonJCKalhanRBarriers to adherence to chronic obstructive pulmonary disease guidelines by primary care physiciansInt J Chron Obstruct Pulmon Dis2011617117921468169
- PearsonMAyresJGSarnoMMasseyDPriceDDiagnosis of airway obstruction in primary care in the UK: the CADRE (COPD and Asthma Diagnostic/management REassessment) programme 1997–2001Int J Chron Obstruct Pulmon Dis20061443544318044099
- WhitePThorntonHPinnockHGeorgopoulouSBoothHPOvertreatment of COPD with inhaled corticosteroids – implications for safety and costs: cross-sectional observational studyPLoS One2013810e7522124194824
- BrusascoVHodderRMiravitllesMKorduckiLTowseLKestenSHealth outcomes following treatment for six months with once daily tiotropium compared with twice daily salmeterol in patients with COPDThorax200358539940412728159
- CasaburiRMahlerDAJonesPWA long-term evaluation of once-daily inhaled tiotropium in chronic obstructive pulmonary diseaseEur Respir J200219221722411866001
- DonohueJFvan NoordJABatemanEDA 6-month, placebo-controlled study comparing lung function and health status changes in COPD patients treated with tiotropium or salmeterolChest20021221475512114338
- DonohueJFKalbergCEmmettAMerchantKKnobilKA short-term comparison of fluticasone propionate/salmeterol with ipratropium bromide/albuterol for the treatment of COPDTreat Respir Med20043317318115219176
- WilsonIDepression in the patient with COPDInt J Chron Obstruct Pulmon Dis200611616418046903
- AgustiAHurdSJonesPFAQs about the GOLD 2011 assessment proposal of COPD: a comparative analysis of four different cohortsEur Respir J20134251391140123645406
- BednarekMMaciejewskiJWozniakMKucaPZielinskiJPrevalence, severity and underdiagnosis of COPD in the primary care settingThorax200863540240718234906
- MapelDWDalalAABlanchetteCMPetersenHFergusonGTSeverity of COPD at initial spirometry-confirmed diagnosis: data from medical charts and administrative claimsInt J Chron Obstruct Pulmon Dis2011657358122135490
- SorianoJBZielinskiJPriceDScreening for and early detection of chronic obstructive pulmonary diseaseLancet2009374969172173219716965
- HaughneyJGruffydd-JonesKRobertsJLeeAJHardwellAMcGarveyLThe distribution of COPD in UK general practice using the new GOLD classificationEur Respir J2014434993100224176990
- JonesRCPriceDRyanDOpportunities to diagnose chronic obstructive pulmonary disease in routine care in the UK: a retrospective study of a clinical cohortLancet Respir Med20142426727624717623