Abstract
Background
This meta-analysis was performed to determine the effectiveness of steroids as an adjunct following rhegmatogenous retinal detachment (RRD) surgery.
Methods
RRD patients with or without proliferative vitreoretinopathy (PVR) were included. The treatment group included patients in whom steroids were used as an adjunct and a control group in which placebo was used. Only randomized controlled trials were included. We searched the main electronic databases and included studies published until July 2014. PVR odds ratio, visual acuity, retinal reattachment rate, and complications were evaluated in three trials.
Results
Three randomized controlled trials were included in the meta-analysis. There was no significant difference in the incidence of postoperative PVR between groups (heterogeneity I2=48%, P=0.14). However, the incidence of postoperative PVR was lower in the treatment group (I2=0%, P<0.0001) than in the control group when a PVR grade C study was excluded. There was no statistically significant difference in postoperative visual acuity between the treatment and control groups (odds ratio −0.18; 95% confidence interval −0.38, 0.02; P=0.08). The two groups had similar results for primary/final retinal reattachment and reoperation rate. There was no significant difference in postoperative intraocular pressure.
Conclusion
This systematic review demonstrates that steroids may significantly reduce the incidence of postoperative PVR grade B or lower following RRD surgery.
Introduction
Rhegmatogenous retinal detachment (RRD) is the most common form of retinal detachment (RD). Proliferative vitreoretinopathy (PVR) is primarily a result of failure to correct RRD after initial retinal reattachment surgery, occurs in 5%–10% of patients, and may lead to recurrent RD.Citation1 Further surgery is the only proven therapy for recurrent RD with PVR. However, the postoperative anatomic success rate is in the range of 60%–80%, and rates are lower for more severe PVR stages.Citation2
Several drugs have shown potential benefit as adjunctive therapy for reducing the postoperative risk of PVR. Use of 5-fluorouracil and low molecular weight heparin can reduce the incidence of postoperative PVR and the associated reoperation rate.Citation3,Citation4 Several recent studies have indicated that postoperative treatment with oral 13-cis-retinoic acid decreases the risk of PVR and improves the operative rate of RD and visual acuity (VA).Citation5,Citation6 Curcumin effectively causes human fetal retinal pigment epithelium cell accumulation at the G2/M phase in vitroCitation7 and also inhibits proliferation by causing cell death.Citation8,Citation9 Daunomycin inhibits formation of PVR in pigmented rabbitsCitation10 and proliferation of human retinal cells.Citation11,Citation12 In some hospitals, steroids, including prednisone, dexamethasone, and triamcinolone acetonide (TA), are regularly used during RRD surgery to reduce the risk of PVR.Citation13–Citation16
Steroids have been used to reduce intraocular inflammation since 1950.Citation17 These agents were thought to suppress postoperative PVR by inhibition of cell proliferation and the intraocular inflammatory reaction.Citation18–Citation20 Further, steroids not only inhibit the production of histamine and decrease its synthesis, but can also cause release of prostaglandins and production of histamine.Citation21 Intraoperative TA can improve the visibility of the posterior hyaloids and epiretinal membrane during pars plana vitrectomy, making surgery more safe and effective.Citation22–Citation24 Continuing TA after surgery can also continue to suppress the intraocular inflammation reaction.Citation24
However, there is a lack of consensus regarding the best route of administration of steroids, the optimal dosage, and the most useful drug. The various steroid agents have different degrees of efficacy. This systematic review and meta-analysis may facilitate the comparison of such interventions.
Materials and methods
Search strategy
We searched the PubMed, EMBASE, and Cochrane Central Register electronic databases using the keywords “proliferative vitreoretinopathy”, “steroids”, “dexamethasone”, “triamcinolone acetonide”, “corticosteroids”, and “prednisolone”. The search was limited to human studies published in English up to July 2014.
Inclusion criteria
We selected papers using the following inclusion criteria: randomized controlled trial (RCT) design; inclusion limited to RRD patients with or without PVR; use of steroids as an adjunct; a placebo control group; and measurement of at least one of the outcomes of interest.
Exclusion criteria
Exclusion criteria included the following: non-RCT design; no detailed and comprehensive data; use of different evaluation outcomes; and the recent publications containing the most updated data from the same trail were included.
Data extraction and quality assessment
TG and PCL reviewed the titles and abstracts following the selection criteria independently. Full publications of appropriate studies were obtained for detailed evaluation, and the data were rechecked after extraction. Any disagreement regarding eligibility was discussed by the two reviewers. The information extracted from each study included method of allocation, blinding, first author, year, country, randomized counts, age, sex, inclusion and exclusion criteria, drugs, route of administration, duration of treatment, type of surgery, and duration of follow-up. The PVR incidence rate was compared in the meta-analysis. Secondary outcomes, including final VA, primary reattachment, and reoperation rate for retinal redetachment were extracted. Systemic and ocular complications were also noted.
Studies eligible for inclusion were assessed for methodological quality using the guidelines in the Cochrane Handbook for Systematic Reviews of Interventions (version 5.1.0, Oxford, UK).Citation25
Statistical analysis
For both continuous and dichotomous data, the meta-analysis was conducted using the statistical software provided by the Cochrane Collaboration Review Manager 5.3.3 (Cochrane Collaboration, Nordic Cochrane Centre, Copenhagen, Denmark). The statistical summaries are presented as odds ratios (ORs) with 95% confidence intervals (CIs). The estimated effect of the data was calculated using the weighted mean difference (WMD) and 95% CI. The Q test or I2 test was used to evaluate heterogeneity. ORs and WMDs were considered to be statistically significant at the P<0.05 level. Both fixed-effects and random-effects models were used to obtain summary ORs or WMDs. In the absence of heterogeneity between groups, the fixed-effects model and the random-effects model provided concordant results. When heterogeneity was significant, the random-effects model was employed. Potential publication bias was estimated using the Egger test and by visually evaluating a funnel plot.Citation26,Citation27
Results
Literature search
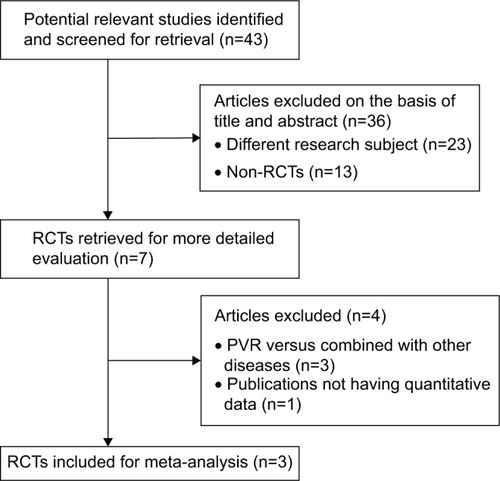
A total of 43 articles were initially identified; 42 records were identified in the database search and one was found in a reference. Seven papers with full text that matched the inclusion criteria were assessed. Three studies investigated additional diseases, and one paper did not include quantitative data. Finally, three studies published before August 2014 were suitable for meta-analysis.Citation28–Citation30 contains a flow diagram of the search results.
Study description
All of the studies included were RCTs conducted in Europe. The sample sizes ranged from 52 to 220. In total, 347 participants were included, comprising 237 (68.3%) males and 110 (31.7%) females. The steroid group contained 173 patients and the control group contained 174 patients. Various degrees of preoperative PVR were included (except PVR grade D). Pars plana vitrectomy or scleral buckling was performed in all patients. Two of the three trials used oral prednisone postoperatively, and the other involved injection of TA into the vitreous cavity during pars plana vitrectomy. The mean age of the participants was 52.3 years. All three studies included at least 6 months of follow-up. The outcomes were assessed in a blinded fashion. shows the patient characteristics and baseline data for the three trials.
Table 1 Patient characteristics in the included trials
Quality assessment
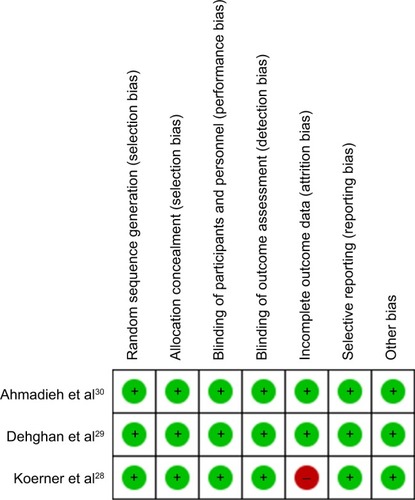
In the three RCTs, the patients were divided using a random block permutation method, such as sealed envelopes, random numbers, or a computer-generated randomization list. The quality of the eligible studies is shown in .
Primary outcome
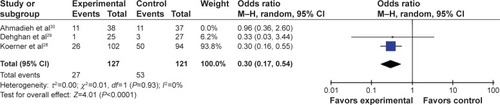
The OR for PVR was evaluated in the three trials, and no difference was found between the steroid and control groups (OR 0.46, 95% CI 0.20–1.10, P=0.08; ). Because the data showed significant heterogeneity (I2=48%, P=0.14), the random-effects model was used for meta-analysis. When the study with PVR grade CCitation30 was excluded, the incidence of PVR was significantly decreased in the steroid group when compared with the control group (OR 0.30, 95% CI 0.17–0.54, P<0.0001; ).
Figure 3 Forest plot of the postoperative PVR incidence rate.
Abbreviations: CI, confidence interval; M–H, Mantel–Haenszel test; PVR, proliferative vitreoretinopathy.
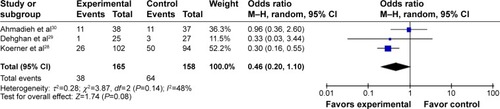
Figure 4 Forest plot of the postoperative PVR incidence rate (excluding grade C, Ahmadieh et al study). There was a statistically significant difference between the steroid group and the control group, when the study of PVR grade C was excluded.
Secondary outcomes
Visual acuity
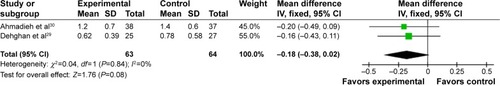
One studyCitation28 was excluded from 6-month follow-up analysis because the relevant data could not be extracted from the original paper. Analysis of VA at 6 months was based on two papers (127 eyes) in which all patients were followed. There was no significant improvement in the steroid group compared with the control group (WMD −0.18, 95% CI −0.38, 0.02, P=0.08). Because the data were not heterogeneous (I2=0%, P=0.84), the fixed-effects model was used for meta-analysis ().
Retinal reattachment rate
One studyCitation29 was excluded from analysis of primary/final reattachment and reoperation rate for retinal redetachment because the relevant data could not be extracted from the original publication. In total, 127 eyes (85.8%) achieved retinal reattachment after primary surgery in the steroid group compared with 123 eyes (83.7%) in the control group. The primary reattachment rate showed no significant difference between the steroid and control groups (heterogeneity I2=0%, P=0.66; OR 1.18, 95% CI 0.63–2.23, P=0.61). The final reattachment rate was 94.29% (132 of 140 eyes) in the steroid group and 90.08% (118 of 131 eyes) in the control group (). The difference was not significant between the two groups (heterogeneity I2=0%, P=0.43; OR 1.81, 95% CI 0.73–4.52, P=0.20). The reoperation rate was 13.51% (20 in 148 eyes) for retinal reattachment in the steroid group; the corresponding data for the control group was 20.41% (30 in 147 eyes). The data were not heterogeneous (I2=0%, P=0.95; ).
Table 2 Outcome indicators in the included trials
Complications
Complication rates, including choroidal detachment, postoperative macular edema via fluorescein angiography, macular pucker formation, and intraocular pressure were not different between the two groups. There were no unexpected side effects due to administration of systemic corticosteroids.
Heterogeneity, sensitivity analysis, and publication bias
Some of the outcomes were heterogeneous. The heterogeneity for PVR incidence rate was significant. After excluding the PVR grade C study, the analysis yielded good results. A sensitivity analysis was conducted to evaluate the stability of the results by sequential removal of individual studies, and the results indicated stability. We therefore performed a heterogeneity interstudy, and the results indicated confidence in our conclusions. The random-effects model was chosen due to the high heterogeneity. The sensitivity analyses indicated that our conclusions were generally strong. Funnel plots were not used because there were fewer than ten trials available for each comparison.
Discussion
This meta-analysis examined the effectiveness and safety of steroids as an adjunct to RRD surgery. The quality of the evidence in this review was moderate. Overall, the three publications included in the meta-analysis were of good quality.
PVR is a common cause of recurrent RD, which often requires additional, multiple surgical interventions. The postoperative VA is worse, and surgical interventions have significantly increased costs.Citation31 Therefore, it is necessary to prevent postoperative PVR.
Drug and tamponade agents are administered to patients with RRD. The clinical evidence indicates that low-dose intravitreal TA injections as an adjunct to vitrectomy and silicone oil tamponade for PVR are effective and safe.Citation13 Jonas et alCitation15 found that intravitreal injections of crystalline cortisone could reduce postoperative intraocular inflammation without toxicity to the intraocular structures. The above-mentioned studies suggest that steroids might be a potentially effective adjunct to PVR. However, our meta-analysis failed to identify significant differences. Due to the clinical heterogeneity, our inclusion criteria lead to a very different preoperative risk across the included studies compared to previous systemic reviews.
In fact, the treatment group showed a lower albeit not statistically significant PVR rate when compared with the control group. However, when excluding the PVR grade C study, the steroid group was more effective than the control group for PVR rate. Multiple studies have indicated that the development of epiretinal membrane results in an inflammatory cascade.Citation32,Citation33 Increased levels of interleukin-8 and vascular endothelial growth factor indicate an inflammatory process associated with a breakdown of the blood–retina barrier.Citation34 Postoperative autoimmune reactions against retinal antigens can be much stronger.Citation35 Steroids might facilitate the prevention or reduction of PVR. Overall, larger and stricter clinical trials are required.
The rate of increased intraocular pressure was lower in patients administered 4 mg TA than in those administered TA 25 mg.Citation36,Citation37 Blumenkranz et alCitation38 found that steroids have an inhibitory effect on PVR at high doses and a stimulatory effect at low doses. Our meta-analysis failed to find a difference in the incidence rate of PVR grade C between the two groups. This result might be due to the following reasons. First, considering the increased intraocular pressure and systemic side effects associated with steroid use, the low doses were used more often, and might be insufficient to treat severe PVR. Second, the inclusion criteria were different between the three studies. There may be other more effective approaches, and this meta-analysis included only RCTs. In one prospective study,Citation14 TA 4 mg was injected into the vitreous cavity filled with silicone oil after pars plana vitrectomy in patients with complicated RRD and PVR grade C2–C9. Twenty-one (87.5%) patients had attached retinas at the final follow-up visit, which is similar to the results in this meta-analysis.
Postoperative VA at 6 months was compared in this meta-analysis. No significant difference in VA was found at postoperative month 6 between the steroid and control groups. As in other studies, mean postoperative VA improved significantly in both groups. However, postoperative VA and changes in VA were not significantly different with or without TA. Overall, steroid use did not increase postoperative VA, potentially because anatomical success did not equate to functional success.
As reported by Williams et alCitation39 the primary retinal reattachment and reoperation rates were not significantly different between the groups. The primary retinal reattachment rate was higher and the reoperation rate was lower in the steroid group; however, the rates were not significantly different. Acar et alCitation16 found that their TA group (87.50%) had a higher albeit not statistically significant primary redetachment rate than their control group (78.12%). The final retinal reattachment rate was not different between the groups.
Use of steroids did not have any unexpected side effects. Postoperative intraocular pressure measurements did not differ significantly between the two groups and were similar to those in other studies.Citation16,Citation39 This might be a result of low-dose, short-term use of steroids. Unfortunately, we could not compare the postoperative cataract rate because cataract surgery is usually performed as a routine procedure along with most retinal reattachment surgeries.
Although only RCTs were included in this meta-analysis, some limitations should not be overlooked. First, only three studies were eligible for meta-analysis, which limits our ability to generalize the results, especially regarding differences between drugs. Some conclusions were difficult to reach due to the small sample sizes. Second, many factors, such as surgeon skills, PVR levels, surgical methods, approach, or steroid doses used, could have affected our results. Long-term follow-up is necessary because steroid use may have systemic side effects.
Conclusion
This meta-analysis demonstrates that use of steroids as an adjunct to RRD surgery can significantly decrease the postoperative PVR incidence rate, especially for grade B PVR.
Acknowledgments
This work was supported by the National Nature Science Foundation Project (81470648) and the New Excellence Project of Shanghai Health Bureau (XYQ2011067). No additional external funding was received.
Disclosure
The authors do not have any commercial or financial disclosures to report in this work.
References
- CharterisDGSethiCSLewisGPFisherSKProliferative vitreoretinopathy – developments in adjunctive treatment and retinal pathologyEye (Lond)200216436937412101443
- HeimannHBartz-SchmidtKUBornfeldNScleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment: a prospective randomized multicenter clinical studyOphthalmology2007114122142215418054633
- WickhamLBunceCWongDMcGurnDCharterisDGRandomized controlled trial of combined 5-fluorouracil and low-molecular-weight heparin in the management of unselected rhegmatogenous retinal detachments undergoing primary vitrectomyOphthalmology2007114469870417398320
- CharterisDGAylwardGWWongDA randomized controlled trial of combined 5-fluorouracil and low-molecular-weight heparin in management of established proliferative vitreoretinopathyOphthalmology2004111122240224515582080
- FekratSde JuanEJCampochiaroPAThe effect of oral 13-cis-retinoic acid on retinal redetachment after surgical repair in eyes with proliferative vitreoretinopathyOphthalmology199510234124187891978
- ChangYCHuDNWuWCEffect of oral 13-cis-retinoic acid treatment on postoperative clinical outcome of eyes with proliferative vitreoretinopathyAm J Ophthalmol2008146344044618599016
- GongLJiangDZhuXGuoLCurcumin inhibits the proliferation of cultured human fetal retinal pigment epithelium cellsYan Ke Xue Bao2004204246248 Chinese15656371
- AnJBMaJXLiuDYThe effect of curcumin on DNA content, mitochondrial transmembrane potential and calcium of rabbit cultured retinal pigment epithelial cellsZhonghua Yan Ke Za Zhi2009453210215 Chinese19575913
- AlexAFSpitznasMTittelAPKurtsCEterNInhibitory effect of epigallocatechin gallate (EGCG), resveratrol, and curcumin on proliferation of human retinal pigment epithelial cells in vitroCurr Eye Res201035111021103320958191
- ShinoharaKTanakaMSakumaTKobayashiYEfficacy of daunorubicin encapsulated in liposome for the treatment of proliferative vitreoretinopathyOphthalmic Surg Lasers Imaging200334429930512875458
- CaiJWeiRMaXZhuHLiYCytotoxic effects of antiproliferative agents on human retinal glial cells in vitroInt Ophthalmol200124422523112678400
- WuWCKaoYHTsengHYThe cell cycle distribution of cultured human retinal pigmented epithelial cells under exposure of anti-proliferative drugsJ Ocul Pharmacol Ther2003191839012648307
- ChenWChenHHouPMidterm results of low-dose intravitreal triamcinolone as adjunctive treatment for proliferative vitreoretinopathyRetina20113161137114221317835
- CheemaRAPeymanGAFangTTriamcinolone acetonide as an adjuvant in the surgical treatment of retinal detachment with proliferative vitreoretinopathyOphthalmic Surg Lasers Imaging200738536537017955840
- JonasJBHaylerJKPanda-JonasSIntravitreal injection of crystalline cortisone as adjunctive treatment of proliferative vitreoretinopathyBr J Ophthalmol20008491064106710966969
- AcarNKapranZAltanTUnverYBPasaogluEPars plana vitrectomy with and without triamcinolone acetonide assistance in pseudophakic retinal detachment complicated with proliferative vitreoretinopathyJpn J Ophthalmol201054433133720700802
- HowardJEHarveyAMCareyRAWinkenwerderWLEffects of pituitary adrenocorticotropic hormone (ACTH) on the hypersensitive stateJ Am Med Assoc1950144161347134914778745
- ShenLYouYSunSIntraocular and systemic pharmacokinetics of triamcinolone acetonide after a single 40-mg posterior subtenon applicationOphthalmology2010117122365237120678801
- MankowskaARejdakROleszczukADecrease of the postoperative inflammatory reaction during pars plana vitrectomy (PPV) after administration of triamcinolone acetonideKlin Oczna20081104–6151154 Polish18655452
- WellerMWiedemannPHeimannKProliferative vitreoretinopathy – is it anything more than wound healing at the wrong place?Int Ophthalmol19901421051172187005
- PeymanGASchulmanJAIntravitreal Surgery: Principles and PracticeNorwalk, CT, USAAppleton & Lange1994
- FurinoCMicelliFTBosciaFTriamcinolone-assisted pars plana vitrectomy for proliferative vitreoretinopathyRetina200323677177614707825
- SakamotoTIshibashiTVisualizing vitreous in vitrectomy by triamcinoloneGraefes Arch Clin Exp Ophthalmol200924791153116319543906
- SonodaKHEnaidaHUenoAPars plana vitrectomy assisted by triamcinolone acetonide for refractory uveitis: a case series studyBr J Ophthalmol20038781010101412881346
- MoherDCookDJJadadARAssessing the quality of reports of randomised trials: Implications for the conduct of meta-analysesHealth Technol Assess1999312198
- BeggCBMazumdarMOperating characteristics of a rank correlation test for publication biasBiometrics1994504108811017786990
- EggerMDaveySGSchneiderMMinderCBias in meta-analysis detected by a simple, graphical testBMJ199731571096296349310563
- KoernerFKoerner-StiefboldUGarwegJGSystemic corticosteroids reduce the risk of cellophane membranes after retinal detachment surgery: a prospective randomized placebo-controlled double-blind clinical trialGraefes Arch Clin Exp Ophthalmol2012250798198722270216
- DehghanMHAhmadiehHSoheilianMEffect of oral prednisolone on visual outcomes and complications after scleral bucklingEur J Ophthalmol201020241942319924670
- AhmadiehHFeghhiMTabatabaeiHTriamcinolone acetonide in silicone-filled eyes as adjunctive treatment for proliferative vitreoretinopathy: a randomized clinical trialOphthalmology2008115111938194318584876
- PatelNNBunceCAsariaRHCharterisDGResources involved in managing retinal detachment complicated by proliferative vitreoretinopathyRetina200424688388715579985
- GilbertCHiscottPUngerWGriersonIMcLeodDInflammation and the formation of epiretinal membranesEye (Lond)19882SupplS140S1563076143
- JoshiMAgrawalSChristoforidisJBInflammatory mechanisms of idiopathic epiretinal membrane formationMediators Inflamm20132013192582
- RasierRGormusUArtunayOVitreous levels of VEGF, IL-8, and TNF-alpha in retinal detachmentCurr Eye Res201035650550920465445
- RickerLJKijlstraAKesselsAGInterleukin and growth factor levels in subretinal fluid in rhegmatogenous retinal detachment: a case-control studyPLoS One201164e1914121556354
- GilliesMCSimpsonJMLuoWA randomized clinical trial of a single dose of intravitreal triamcinolone acetonide for neovascular age-related macular degeneration: one-year resultsArch Ophthalmol2003121566767312742844
- JonasJBAkkoyunIBuddeWMKreissigIDegenringRFIntravitreal reinjection of triamcinolone for exudative age-related macular degenerationArch Ophthalmol2004122221822214769599
- BlumenkranzMSClaflinAHajekASSelection of therapeutic agents for intraocular proliferative disease. Cell culture evaluationArch Ophthalmol198410245986046704019
- WilliamsRGChangSComarattaMRSimoniGDoes the presence of heparin and dexamethasone in the vitrectomy infusate reduce reproliferation in proliferative vitreoretinopathy?Graefes Arch Clin Exp Ophthalmol199623484965038858355