Abstract
Background
With scientific and technological advances, the practice of orthopedic surgery has transformed the lives of millions worldwide. Such successes however have a downside; not only is the provision of comprehensive orthopedic care becoming a fiscal challenge to policy-makers and funders, concerns are also being raised about the extent of the associated iatrogenic harm. The National Reporting and Learning System (NRLS) in England and Wales is an underused resource which collects intelligence from reports about health care error.
Methods
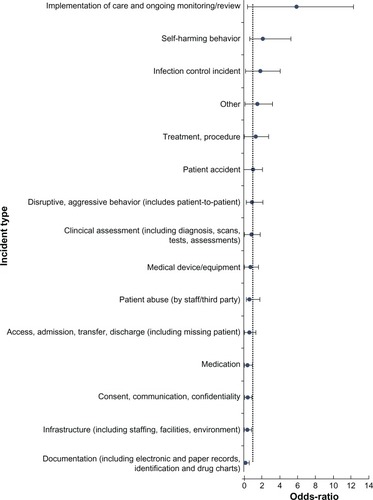
Using methods akin to case-control methodology, we have identified a method of prioritizing the areas of a national database of errors that have the greatest propensity for harm. Our findings are presented using odds ratios (ORs) and 95% confidence intervals (CIs).
Results
The largest proportion of surgical patient safety incidents reported to the NRLS was from the trauma and orthopedics specialty, 48,095/163,595 (29.4%). Of those, 14,482/48,095 (30.1%) resulted in iatrogenic harm to the patient and 71/48,095 (0.15%) resulted in death. The leading types of errors associated with harm involved the implementation of care and on-going monitoring (OR 5.94, 95% CI 5.53, 6.38); self-harming behavior of patients in hospitals (OR 2.14, 95% CI 1.45, 3.18); and infection control (OR 1.91, 95% CI 1.69, 2.17). We analyze these data to quantify the extent and type of iatrogenic harm in the specialty, and make suggestions on the way forward.
Conclusion and level of evidence
Despite the limitations of such analyses, it is clear that there are many proven interventions which can improve patient safety and need to be implemented. Avoidable errors must be prevented, lest we be accused of contravening our fundamental duty of primum non nocere. This is a level III evidence-based study.
Introduction
The high frequency of medical errors and the associated disease burden resulting from iatrogenic harm remains an important challenge for health care systems globally.Citation1 Almost a decade ago, the Institute of Medicine published a sentinel report, To Err is Human, which identified medical errors as a major challenge for public health. The report demonstrated the lethality of medical error and placed it on par with breast cancer or road traffic accidents; this analogy helped initiate efforts worldwide for addressing the threat to public health and safety.Citation2
Surgical specialties have been a focus of opportunity as patient safety has developed its global enterprise. More than 234 million people require surgical treatment every year globally, and more than half of these treatments occur in developed countries.Citation3 By the sheer numbers of procedures, both for emergency and elective problems, trauma and orthopedics as a specialty could be deemed more “risky,” as partly evidenced by the fact that 20% of wrong-site surgery incidents occurred in the specialty in 2006–2007.Citation4
In addition to additional mortality and morbidity, there are direct financial implications of unsafe care, and clinical negligence claims against the UK’s National Health Service (NHS) demonstrate this. During the 2010/2011 financial year, negligence cost the NHS £860 million – a 9% increase from the previous year. Trauma and orthopedics was the specialty with the highest number of clinical claims made.Citation5
In the Institute for Medicine’s follow up report, Crossing the Quality Chasm,Citation6 the poor use of incident reporting systems was highlighted, since they are necessary to help inform actions to improve patient safety. Patient safety reporting systems (PSRSs) can aid understanding of the extent and nature of the problems that occur from errors. Such learning insights can lead to the development of interventions aimed at mitigating against errors; for example, the generation of alerts on the complications of a new drug; dissemination of lessons learned by health care organizations experiencing serious patient safety incidents (PSIs); and revelation of unrecognized trends in errors.Citation7 National databases of errors have been created in many parts of the world, including the USA.Citation8,Citation9,Citation10 These have offered important insights that have helped to shape national policy – for example, for demonstrating the risks of bone cement implantation syndrome associated with use of cement in hip fracture surgery, and the potential for IT-based interventions to reduce many cases of drug allergy related morbidity.Citation11,Citation12
The aim of this study was to understand the burden of harm in trauma and orthopedics using a cross-sectional methodology. As such, we wanted to ascertain what types of errors are associated with the greatest burden of harm in orthopedic patients.
Methods
The National Reporting and Learning System (NRLS) is a voluntary, national reporting system set up in 2003 for the NHS in England and Wales. It is the largest and most comprehensive reporting system in the world, with over 7 million PSIs recorded to date, with increases in the number of reports received each year since 2003.Citation13 All staff working within the NHS can report incidents through their parent institution to ensure that local action can be taken when necessary. A representative from each parent institution is responsible for uploading records to the national database. In addition, health care staff, patients, and members of the public can report incidents independently through the NRLS website.Citation14
Each NRLS report refers to an unintended or unexpected incident that could have or did lead to harm for one or more patients receiving NHS-funded care. It also includes reports of incidents which reached the patient but did not lead to harm, and those which did not lead to harm because an incident was prevented from reaching the patient. Incidents are further stratified into different levels of harm.Citation13 In order to integrate the wide variety of local safety management systems and software, the NRLS has 75 data fields, including incident categories at two levels, specialty and location of the incident, and free-text descriptions of the events.Citation15 Each incident that is reported as leading to death or serious harm is reviewed individually by trained clinical staff and a range of outputs are produced to provide solutions to patient safety problems. These include one-page reports called Rapid Response Reports, quarterly data summaries, and topic-specific information on topics such as preventing inpatient falls in hospitals. There is constant consultation with subject-matter experts including professional organizations such as the Royal Colleges. NHS organizations also have deadlines imposed on them by which time they should have implemented any findings from those reports.Citation13
Data from the NRLS database were analyzed for all incidents reported in the specialty of trauma and orthopedics from January 2009 to December 2009. The domains searched were “Acute/General Hospital” and “Trauma and Orthopedics” and limited to England.
There are 16 types of incident categories with further sub-divisions. Free text descriptions of all the PSIs were also abstracted. Harm was defined by user self-report as: no harm, low harm (minimal harm – patient[s] required extra observation or minor treatment), moderate harm (short term harm – patient[s] required further treatment or procedure), severe harm (permanent or long term harm), or death.
Our statistical approach involved the use of case-control methodology. The first case-control study revealed a link between tobacco smoking and lung cancer.Citation16 We sought to extend this approach further, with the caveat that a deeper understanding of confounding factors would not be possible owing to the structure of the database. Our definition of a “case” was one where an error resulted in harm. The “controls” were defined as errors where no harm occurred or “near-misses.” Errors were clustered into 15 discrete categories called “incident types.”Citation15 We sought to evaluate the degree of association between different types of errors and the resultant harm to the patient.
Measures of relative effect express the outcome in one group relative to that in the other. Two common methods are used, the relative risk (RR) and the odds ratio (OR). The OR is the probability that a particular event will occur to the probability that it will not occur, and can be any number between zero and infinity. In gambling, the odds describe the ratio of the size of the potential winnings to the gambling stake; in health care, it is the ratio of the number of people with the event to the number without. Risk is the concept more familiar to patients and health professionals. Risk describes the probability with which a health outcome (usually an adverse event) will occur. Measures of relative effect express the outcome in one group relative to that in the other. Hence, the RR is the ratio of the risk of an event in the two groups whereas the OR is the ratio of the odds of an event.
For treatments that increase the chances of events, the OR will be larger than the risk ratio, so the tendency will be to misinterpret the findings in the form of an overestimation of treatment effect, especially when events are common (with, say, risks of events more than 20). For treatments that reduce the chances of events, the OR will be smaller than the risk ratio, so that again misinterpretation overestimates the effect of treatment. Furthermore, the RR is an easier concept to understand.Citation17 A 2 × 2 design was constructed for each of the categories ().
Table 1 2 × 2 table to calculate degree of association
Results
There were 48,095 PSIs from trauma and orthopedics incidents reported to the NRLS in 2009. Of those, 14,482/48,095 (30.1%) resulted in iatrogenic harm to the patient, and 71/48,095 (0.15%) resulted in death. There were 155 NHS trusts that reported data to the database. Aggregate frequencies of harm and examples of the free-text are shown in . Large proportions of harm were seen in the following categories of harm: patient accident (n = 5639, 11.72%), implementation of care and on-going monitoring/review (n = 2600, 5.41%), treatment (n = 2091, 4.35%), medication (n = 744, 1.55%), and access, admission, transfer, discharge (including missing patient) (n = 606, 1.26%). lists the proportion of harm exhibited by each category of error.
Table 2 Frequency of harm by category
Table 3 Proportion of harmful incidents in each category
A breakdown of incidents according to the pre-defined categories is given in . The five statistically significant areas of harm include implementation of care and ongoing monitoring/review; self-harming behavior; infection control incidents; other; and treatment/procedure.
Discussion
The areas of concern that we have highlighted in our study are well recognized within the specialty. The largest category of concern is “implementation of care and on-going monitoring/review” [OR = 2.55, 95% CI 2.49, 2.62], and this is a recognized problem for the fragility of hip fractures. Uptake of best practice guidelines released by the UK Department of Health has been variable.Citation18 Key components for delivery of its best practice agenda include a reduction in the delay to surgery and involvement of an orthogeriatrician in the care of patients. Different models of orthogeriatric care have been proposed with the aim of ensuring an integrated multi-disciplinary team approach with evidence-based pathways.Citation19 Overall, several tools are now available to mitigate harm associated with poor care of orthopedic patients; pre- and post-operative adjuncts such as better use of orthogeriatric services,Citation19 early warning scores and trigger tools to prevent major catastrophes during the pre-, intra-, and post-operative phases of care,Citation20 enhanced recovery protocolsCitation21 for the entire patient journey to ensure that best practice guidelines are adhered to, and intra-operative tools such as the World Health Organization surgical checklist.Citation22
A second finding of interest was the greater propensity of self-harming behavior incidents on orthopedic wards. Several recommendations have been made which place the onus on clinical services to place priority for suicide prevention and monitoring,Citation23 including a suicide prevention for hospital patients toolkit.Citation24 Infection control incidents were also a domain of concern in our analyses [OR = 1.50 (95% CI 1.41, 1.61)], and health care associated infections are recognized to be the most frequent adverse event that threaten patients’ safety, with a large burden of avoidable harm.Citation25 Prevention of these infections occurs in the pre-, peri-, and post-operative phases.Citation26
This is the first attempt to our knowledge of quantifying the burden of iatrogenic harm in the specialty of orthopedics and trauma using a PSRS. However, this is only a start and much more needs to be done, given concerns about the utility of databases to promote safety. An increased rate of reporting, whereas in itself could imply that the culture of patient safety is improving, on its own is of limited value. The National Patient Safety Agency had 158 incidents reported in 2003 and to date has over 7 million incidents reported to it.Citation27,Citation28 Paradoxically, despite the large number of incident reports received by the NRLS, reporting systems have been shown to detect only about 6% of adverse events found by a systematic review of records.Citation29 Indeed, it has been argued that national reporting systems are of great importance at identifying rare events, but of limited use in analyzing trends or acting as measurements of patient safetyCitation30 It is commendable that several solutions have been provided in the form of alerts and rapid responses.Citation11 However, most of these solutions seem reactive.Citation31 At present, the lesson from national PSRS is limited; some of the information is lost in translation.Citation32 Local systems of risk management opt for root cause analyses to develop local solutions to mitigate against harm to the patient. National systems rely on patient safety experts methodically trawling through PSIs by severity and frequency, thereby leading to the production of quarterly reports, alerts, and rapid response solutions.Citation14 Such analyses are time-consuming as the size of the PSRS increases and may be of limited value. There is a need for applied epidemiological tools to be created to allow clusters of harmful incidents to be identified, both by hospital and specialty. This may offer a true reporting and learning system which actively engages stakeholders in delivering error-free care for patients. Most commentators agree that the long term and sustainable solution lies in professional engagement and local efforts.
The gross under-reporting to PSRSs has been cited as their “Achilles heel” and, as such, their use is often limited to warning, communication, and detection of rare PSIs.Citation30 Whilst this may be a valid criticism, it is clear that reporting is increasing as clinicians become more aware of the presence of PSRSs, and furthermore develop confidence that there will not be any personal repercussions to making reports. Also, one might argue that a vast majority of incidents result in no harm whatsoever, and it could create a false impression of over-reporting and the subsequent arguments of bureaucracy and misrepresentation of the situation. However, convincing clinicians of the usefulness of the data they contribute should in due course further increase the frequency and quality of reporting. It will also help specialties such as orthopedics to develop surveillance tools and easier methods of understanding highly error-prone situations to which ameliorative solutions must be provided. There are some limitations to our methods as they stretch the application of case-control methodology. Owing to missing data, we are unable to definitely assess the effect of causative factors for errors, including those such as age and experience of the doctor.
The number of orthopedic patients suffering preventable adverse events is high. This has been shown in non-UK settings as well; almost half of all members of the American Academy of Orthopaedic Surgeons, who agreed to a survey, reported that they had observed a medical error.Citation33 Looking at the number of orthopedic surgery consultations in the NHS during 2008/2009, the crude proportion of these errors would appear to be small (48,095/1,144,520, 4.2%), but it is the absolute number that is key.Citation34
Iatrogenic harm in trauma and orthopedic surgery is an important issue and we need a multi-pronged strategy to address it. In addition, to better study the problem by building research capacity in the area, we need to act on known and proven interventions for delivering safer care: better clinical leadership, promoting the use of patient safety indicators as part of quality accounts for orthopedic surgeons within hospitals, and to showcase examples of best practice that use quality improvement and patient safety metrics.
Disclosure
The authors report no conflicts of interest in this work.
References
- HurwitzBSheikhAHealth Care Errors and Patient SafetyOxfordWiley Blackwell2009
- KohnLTCorriganJMDonaldsonMSTo Err Is Human: Building a Safer Health SystemWashingtonNational Academy Press1999
- WeiserTGRegenbogenSEThompsonKDAn estimation of the global volume of surgery: a modelling strategy based on available dataLancet2008372963313914418582931
- RobinsonPMMuirLTWrong-site surgery in orthopaedicsJ Bone Joint Surg Br200991101274128019794159
- National Health Service Litigation Authority (NHSLA)Reports and Accounts 2010–2011London2011
- Institute of MedicineCrossing the Quality Chasm: A New Health System for the Twenty-first CenturyWashingtonNational Academy Press2001
- LeapeLLReporting of adverse eventsN Engl J Med2002347201633163812432059
- SheikhAHurwitzBA national database of medical errorJ R Soc Med1999921155455510703490
- PanesarSSClearyKSheikhARefections on the National Patient Safety Agency’s database of medical errorsJ R Soc Med2009102725625819605852
- HicknerJZafarAKuoGMField test results of a new ambulatory care medication error and adverse drug event reporting system – MEADERSAnn Fam Med20108651752521060122
- PanesarSSClearyKBhandariMSheikhATo cement or not in hip fracture surgery?Lancet200937496951047104919782857
- CresswellKMSheikhAInformation technology-based approaches to reducing repeat drug exposure in patients with known drug allergiesJ Allergy Clin Immunol200812151112111718313132
- LamontTScarpelloJNational Patient Safety Agency: combining stories with statistics to minimise harmBMJ2009339b448919926688
- National Reporting and Learning Service [homepage on the Internet]LondonNHS Available from: http://www.nrls.npsa.nhs.uk/Accessed September 27, 2012
- CatchpoleKBellMDJohnsonSSafety in anaesthesia: a study of 12,606 reported incidents from the UK National Reporting and Learning SystemAnaesthesia200863434034618336482
- DollRHillABSmoking and carcinoma of the lung; preliminary reportBr Med J19502468273974814772469
- LeeJOdds ratio or relative risk for cross-sectional data?Int J Epidemiol1994232012028194918
- Confirmation of Payment by results Guidance for 2010–2011 [webpage on the Internet]LondonDepartment of Health2010 Available from: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_112284Accessed September 27, 2012
- The Management of Hip Fracture in Adults [webpage on the Internet]LondonNational Clinical Guideline Centre Available from: http://guidance.nice.org.uk/CG124Accessed September 27, 2012
- Gardner-ThorpeJLoveNWrightsonJWalshSKeelingNThe value of Modified Early Warning Score (MEWS) in surgical in-patients: a prospective observational studyAnn R Coll Surg Engl200688657157517059720
- MalviyaAMartinKHarperIEnhanced recovery program for hip and knee replacement reduces death rateActa Orthop201182557758121895500
- HaynesABWeiserTGBerryWRSafe Surgery Saves Lives Study GroupA surgical safety checklist to reduce morbidity and mortality in a global populationN Engl J Med2009360549149919144931
- Safety First: Five-year report of the National Confidential Inquiry into Suicide and Homicide by People with Mental Illness [webpage on the Internet]LondonDepartment of Health2001 Available from: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4006679Accessed September 27, 2012
- Preventing suicide – a toolkit for mental health services [webpage on the Internet]LondonNational Patient Safety Agency2009 Available from: http://www.nrls.npsa.nhs.uk/resources/?entryid45=65297Accessed September 27, 2012
- Surgical site infection: prevention and treatment of surgical site infection [webpage on the Internet]LondonNational Institute for Health and Clinical Excellence2008 Available from: http://www.nice.org.uk/Guidance/CG74Accessed September 27, 2012
- HumphreysHPreventing surgical site infection. Where now?J Hosp Infect200973431632219700219
- NRLS Quarterly Data Workbook up to June 2010 [webpage on the Internet]LondonNational Patient Safety Agency2010 Available from: http://www.nrls.npsa.nhs.uk/resources/collections/quarterly-data-summaries/?entryid45=83732Accessed September 27, 2012
- PhamJCGianciSBattlesJEstablishing a global learning community for incident-reporting systemsQual Saf Health Care201019544645120977995
- SariABSheldonTACracknellATurnbullASensitivity of routine systems for reporting patient safety incidents in an NHS hospital: retrospective patient case note reviewBMJ200733475847917175566
- VincentCAylinPFranklinBDIs health care getting safer?BMJ2008337a242619008272
- Memorandum by Andrew Lansley [webpage on the Internet]LondonHouse of Commons2009 Available from: http://www.publications.parliament.uk/pa/cm200809/cmselect/cmhealth/151/151we52.htmAccessed September 27, 2012
- LankshearALowsonKHardenJLowsonPSaxbyRCMaking patients safer: nurses’ responses to patient safety alertsJ Adv Nurs200863656757518808578
- WongDAHerndonJHCanaleSTMedical errors in orthopaedics: results of an AAOS member surveyJ Bone Joint Surg Am200991354755719255214
- Hospital Episode Statistics online [webpage on the Internet]. Main specialty 2008–2009Hospital Episode Statistics2012 Available from: http://www.hesonline.nhs.uk/Ease/servlet/ContentServer?siteID=1937&categoryID=207Accessed January 10, 2013