Abstract
Background
Patients with non-alcoholic fatty liver disease (NAFLD) are more likely to develop left ventricular diastolic dysfunction (LVDD). Although lifestyle adjustments contribute to the improvement of NAFLD, thereby delaying or even preventing LVDD progression, it is difficult to maintain a healthy lifestyle, resulting in a higher incidence of LVDD in NAFLD patients.
Objective
This study aims to develop a nomogram for assessing the risk of LVDD progression in NAFLD patients to increase their adherence to therapeutic interventions and adjust their treatment regimens timely.
Methods
A total of 148 medical records of NAFLD patients were retrospectively analyzed. Sixty-three were assigned to the LVDD+ group and 85 were assigned to the LVDD- group. The independent correlates of LVDD, which were screened via least absolute shrinkage and selection operator logistic regression model first, followed by multivariate Logistic regression model, constituted the nomogram to determine the likelihood of LVDD in NAFLD patients.
Results
Number of comorbidities, glycosylated hemoglobin, and epicardial adipose tissue (EAT) volume index were independent correlates of LVDD (all P < 0.05). They served as components in the newly developed nomogram. It obtained significant clinical benefit in detecting NAFLD patients at the risk of LVDD progression, with satisfied discrimination and calibration.
Conclusion
We developed a nomogram for identifying NAFLD patients with a normal diastolic function who are at risk of LVDD progression, thus contributing to effective prevention of LVDD progression.
Introduction
Left ventricular diastolic dysfunction (LVDD) is currently considered an independent predictor of cardiovascular events in various populations. The assessment of left ventricular diastolic function has attracted considerable attention in recent years since it is one of the key determinants of cardiac performance.Citation1 People with LVDD may develop irreversible heart failure without experiencing telltale signs and symptoms.Citation2 Given that LVDD is a dynamic process, its worsening emerged as a marker of poorer prognosis, while its improvement is associated with better outcomes.Citation3 Clinicians must recognize the potentially reversible causes of LVDD in order to improve LVDD or reduce the potential risk of LVDD in individuals with a normal diastolic function through targeted interventions.
Among the reversible causes of LVDD (eg, acute myocardial ischemia, myocarditis, etc.), obesity-induced LVDD is becoming an essential component of worldwide research due to its enormous population.Citation4 Multiple studies have identified an increased prevalence of impaired diastolic function in obese patients compared with normal-weight subjects, independent of hypertension and type 2 diabetes mellitus (T2DM).Citation5–7 This may be because obese people show a greater propensity for ectopic fat deposition.Citation8 With a better understanding of the potential impact of epicardial adipose tissue (EAT) on cardiovascular risk, it has been discovered that a pro-inflammatory and pro-fibrotic secretome characterized by a dysfunctional EAT may damage cardiac structure and function. This resulted in a significant association between increased EAT and LVDD in obese subjects.Citation9 Because of the rising prevalence of obesity globally, the harmful effects of non-alcoholic fatty liver disease (NAFLD), which has a global prevalence of 25%, are becoming a serious public health challenge.Citation10 To date, mounting evidence linking NAFLD with functional and structural myocardial alterations supports the hypothesis that NAFLD is associated with the pathogenesis of LVDD, independently of established cardiovascular risk factors.Citation11–15 Thus, assessing the risk of LVDD in individuals with NAFLD is important, since changes in unhealthy lifestyles can improve NAFLD, thereby delaying or even preventing the progression to LVDD.Citation16
Although several studies have proved significant improvements in LV filling or relaxation with weight loss, it is difficult to quantify the likelihood of LVDD progression in NAFLD patients with a normal diastolic function during diet and lifestyle interventions, resulting in a higher incidence of LVDD in NAFLD patients.Citation17,Citation18 With this background, this study aims to develop a nomogram for quantitatively assessing the risk of LVDD progression in patients with NAFLD. It helps NAFLD patients increase their willpower and adherence to long-term therapeutic interventions, while also allowing clinicians to change treatment in a timely manner to prevent further progression to LVDD.
Materials and Methods
This retrospective study complied with the principles stated in the declaration of Helsinki, and was approved by the ethics committee of Hwa Mei Hospital, University of Chinese Academy of Sciences (YJ-NBEY-KY-2021-081-01).
Study Population
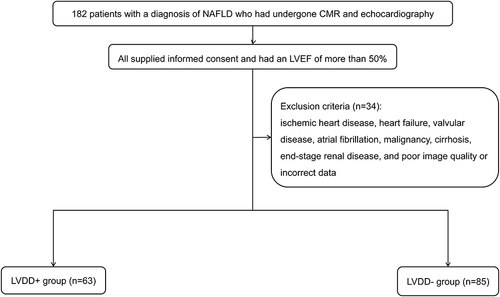
We reviewed the medical records of 182 patients with a diagnosis of NAFLD who had undergone cardiac magnetic resonance (CMR) and echocardiography at Hwa Mei Hospital, University of Chinese Academy of Sciences between January 2019 and March 2022. NAFLD is diagnosed when (a) hepatic steatosis is present, (b) no viral hepatitis, autoimmune hepatitis, or other known causes of liver disease are present, and (c) there are no secondary reasons of hepatic fat accumulation, such as excessive alcohol consumption.Citation19,Citation20 All patients received weight-loss suggestions and took antidiabetic and antihypertensive medications as needed. Patients were eligible for inclusion if they supplied informed consent. Each of them had a left ventricular ejection fraction (LVEF) of more than 50%. Subjects with a history of ischemic heart disease, heart failure, valvular disease, atrial fibrillation, malignancy, cirrhosis, end-stage renal disease, and patients with poor image quality or incorrect data were excluded (n = 34). Ultimately, 148 patients were included in this study. Among them, 63 patients with LVDD were assigned to the LVDD+ group, while those with normal diastolic function were assigned to the LVDD- group (n = 85). depicts a flow diagram exhibiting patient selection and grouping.
Collection of Anthropometric and Biochemical Data
Demographics and medical history were collected via a self-reported questionnaire. Their anthropometric data including body mass index (BMI), waist circumference, body surface area (0.0061 * height + 0.0128 * weight − 0.1529), and blood pressure were recorded. Obesity was defined according to the WHO criteria from the Asia-Pacific region (BMI ≥ 25 kg/m2).Citation21 Blood samples were measured for fasting plasma glucose (FBG), glycosylated hemoglobin (HbA1c), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglyceride (TG), aspartate aminotransferase (AST), and alanine aminotransferase (ALT).
CMR Protocol
A 3-Tesla Magnetom Prisma MR scanner (Siemens Healthcare, Erlangen, Germany) with an 18-channel phased-array body coil was used to perform CMR scanning. Using a standard ECG-triggering equipment, approximately 15 continuous cine images in the short-axis view and LV two- and four-chamber cine images in the long-axis view were obtained. The cine loop images were analyzed by two observers with more than 10 years who were blinded to patients’ status.
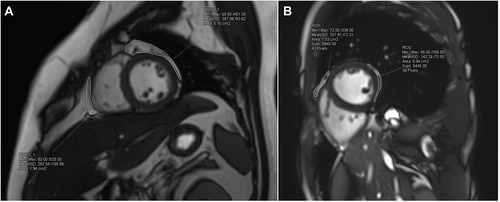
EAT volume was determined by manually delineating EAT, the adipose tissue situated between the outer wall of the myocardium and the visceral layer of the pericardium, extending the upper slice limit, marked by the bifurcation of the pulmonary trunk, toward the most apical slice, on short-axis cine slices at end-diastole. EAT volume index (EATVi, cm3/m2) was calculated by summing the EAT volume of each slice (8 mm thickness), and then indexed to body surface area ().Citation22,Citation23
Figure 2 EAT volume calculation in CMR. The EAT region is delineated on short-axis cine slices at end-diastole, from the upper slice limit, marked by the bifurcation of the pulmonary trunk, to the most apical slice. EAT volume is calculated by summing the EAT volume of each slice (8 mm thickness). Representative outputs of EAT delineation in NAFLD patients with and without LVDD are shown in (A and B), respectively.
Echocardiography
All participants underwent a standard transthoracic echocardiography using Vivid E80 Ultrasonography (GE Medical Systems, Milwaukee, WI) at rest by a specialized echocardiologist with more than 10 years of experience. The cardiac parameters included left ventricular end diastolic dimension (LVDd), left ventricular end systolic dimension (LVDs), posterior wall thickness (PWT), left atrial volume index (LAVI), LVEF, pulsed-wave Doppler examination of the mitral inflow, and pulsed-wave tissue Doppler imaging at the medial mitral annulus according to American Society of Echocardiography guidelines.Citation24 LAVI was assessed through the biplane area-length method. LVEF was determined by modified biplane Simpson’s method. E/A ratio represented the ratio of peak left ventricle filling velocity in early diastole (E wave) to that in late diastole (A wave), based on mitral inflow Doppler signals. E wave deceleration time (DT) was also measured. For tissue Doppler imaging, E/e’ ratio represented the ratio of E wave to early diastolic mitral annular velocity (e’), which was the average value of the two measurements at septal and lateral sides of mitral annulus. Continuous-wave Doppler was performed to determine the tricuspid regurgitation peak velocity (TRPV) and isovolumetric relaxation time (IVRT).
In this study, LVDD was identified if more than two criteria were met: septal e’ <7cm/s or lateral e’ <10cm/s, average E/e’ >14, TRPV > 2.8m/s, and LAVI > 34mL/m2.Citation25
Nomogram Development
The least absolute shrinkage and selection operator (LASSO) regression model, which was suitable for simplifying high-dimensional data, was used to identify the variables significantly associated with the presence of LVDD in NAFLD patients among demographic, anthropometric and biochemical data by means of a penalty function. The coefficient of each variable was compressed along with the changes of penalty regularization parameter (λ). Ten-fold cross validation processing to select the optimal λ with the minimum error was carried out to identify the selected variables.Citation26 The multivariate Logistic regression analysis only included the variables filtered by the LASSO model in order to investigate the independent correlates of LVDD. Finally, these independent variables were utilized to develop a nomogram to determine the likelihood of LVDD in NAFLD patients.
Statistical Analysis
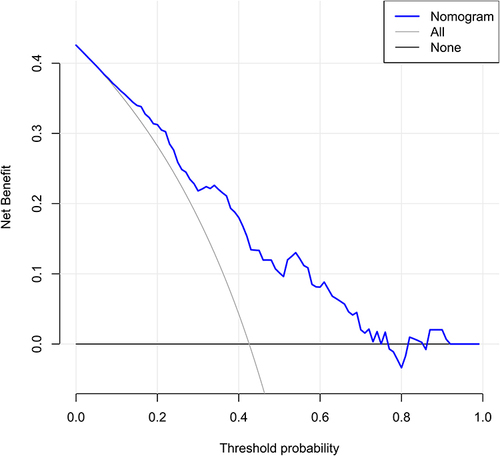
Continuous variables were expressed as mean ± standard deviation (normal distribution) or median (interquartile range) (skewed distribution), and categorical variables were expressed as frequency (percentage). Comparison between groups were assessed using the Student t-test, Mann–Whitney U-test, and chi-squared test as appropriate. The primary goal of this study was to investigate variables independently associated with LVDD in NAFLD patients via LASSO and multivariate logistic regression models and to constitute a nomogram model. For the validation of the nomogram, the discrimination performance was assessed by the area under the receiver operating characteristic curve (AUROC). It was calibrated by a calibration curve accompanied by a Hosmer-Lemeshow (HL) test and a Brier score. A decision curve analysis (DCA) was applied to determine the clinical application of our model. Bootstraps (1000 times) analyses were implemented on the AUROC, calibration curve, and DCA to adjust overfitting deviation. All statistical tests were performed using SPSS software (Version 22.0), MedCalc (Version 22.0.22), and R package (Version 4.1.3).
Results
Clinical and Imaging Characteristics in the LVDD- and LVDD+ Groups
In this study, LVDD was found in 63 of the 148 patients with NAFLD, with an incidence of 42.6%. The comparisons of anthropometric, biochemical, and imaging features between the LVDD- and LVDD+ groups are summarized in . Compared with the LVDD- group, age, HbA1c, EATVi, proportion of obesity, hypertension, and T2DM in the LVDD+ group were statistically higher, while the proportion of regular exercise was statistically lower (all P < 0.05). Among the echocardiographic parameters, LAVI, TRPV, septal e’, lateral e’, and E/e’ were statistically different between the two groups (all P < 0.05).
Table 1 Differences in Anthropometric, Biochemical, and Imaging Characteristics Between the LVDD- and LVDD+ Groups
Selection of Variables Associated with LVDD by LASSO Model
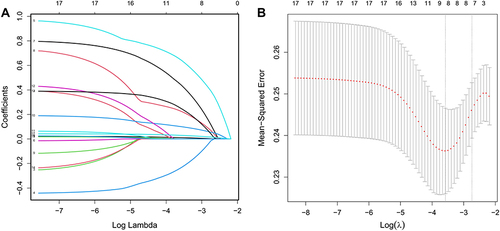
Seventeen clinical and imaging characteristics were selected and analyzed by the LASSO model, which was utilized to select potential variables associated with LVDD in collinear data (). By constructing a penalty function, 17 variables were reduced to 8 according to the optimal λ with the minimum cross-validation error, including age, regular exercise, hypertension, T2DM, obesity, HbA1c, LDL-C, and EATVi.
Figure 3 Screening of variables associated with LVDD by LASSO regression model. LASSO coefficient profiles of all variables are plotted in (A). The trajectory of each independent variable coefficient is shown by each differently colored curve. Identification of the penalty regularization parameter (λ) in the LASSO model is achieved by 10-fold cross-validation and the minimum criteria (B). The first dashed line represents the minimum error, while the second represents the cross-validated error within 1 standard error of the minimum value. Eight variables (age, regular exercise, hypertension, T2DM, obesity, HbA1c, LDL-C, and EATVi) are selected by deriving the optimal λ value with the minimum error.
Independent Factors Associated with LVDD
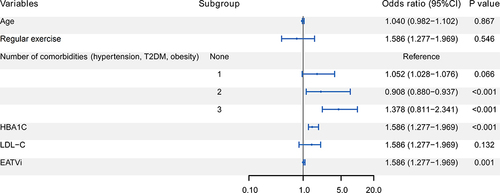
Eight variables were incorporated into the multivariate Logistic regression analysis after being filtered by the LASSO model to investigate the independent correlates of LVDD in NAFLD patients. shows a forest plot, which is utilized to depict the results of multivariate logistic regression analysis. The result revealed that number of comorbidities, HbA1c, and EATVi were independently associated with LVDD (all P < 0.05). Age and regular exercise were not independently associated with LVDD (both P > 0.05).
Figure 4 Forest plot of multivariate Logistic regression analysis for independent factors associated with LVDD in NAFLD patients. Number of comorbidities, HbA1c, and EATVi are independently associated with LVDD (all P < 0.05).
Nomogram Development
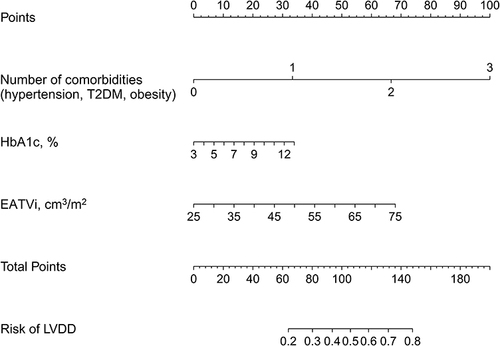
Using the three selected variables, a nomogram was developed for predicting the risk of LVDD in NAFLD patients. As indicated in , the estimated risk of LVDD was calculated by summing the points of each independent factor, with a weight equal to the OR value. The sum included the total point and matched the risk on the bottom axis.
Figure 5 Nomogram for estimating the risk of LVDD in NAFLD patients. Number of comorbidities, HbA1c, and EATVi are included in the nomogram. The point assignment for each factor is shown in the first row. The variables in the nomogram are listed in rows 2–4. The risk of LVDD is presented in the bottom row. For example, in a 50-year-old NAFLD patient with T2DM and hypertension, his HbA1c and EATVi is 7% and 60 cm3/m2, respectively. His total score is about 120, indicating that his risk of LVDD progression is about 60%. It suggests that more aggressive glycemic control and weight reduction should be implemented to keep his risk below 50%.
Performance Evaluation of the Nomogram
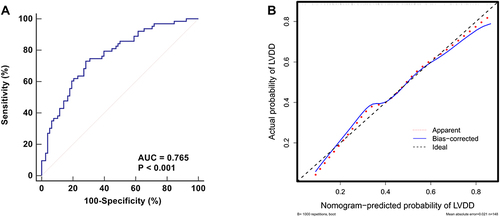
The developed nomogram was validated to assess the discrimination, calibration, and clinical applicability. The stability of the model was tested after 1000 bootstrapping to adjust overfitting deviation. As indicated in , the AUROC of the model was 0.765 (95% CI: 0.686–0.832), demonstrating a moderately good performance in discrimination. The calibration curve revealed that the model showed good agreement between the predicted and actual probabilities of LVDD. Good calibration was demonstrated according to the HL test (χ2 = 9.748, P = 0.283) and Brier score (0.112). The DCA of the nomogram revealed that predicting the risk of LVDD in NAFLD patients using this nomogram generated a clinical net benefit if the risk threshold of LVDD was less than 80% ().
Figure 6 Evaluation of the discrimination and calibration for the established nomogram. ROC curve is plotted for evaluating the discrimination. The AUC is 0.765, indicating moderately good discrimination (A). The calibration curve, which is plotted for evaluating the calibration, indicates that the predicted probability of LVDD matches the actual probability well (B).
Discussion
For most asymptomatic NAFLD patients, weight loss with long-term lifestyle adjustments is the key to reducing the progression to LVDD. However, it is sometimes difficult for people to maintain healthy lifestyle practices for a long time, which eventually leads to LVDD, because the progress of both NAFLD and LVDD is imperceptible. In this study, we developed a nomogram to estimate the risk of LVDD in NAFLD patients via LASSO and multivariate Logistic regression models. Our study revealed that number of comorbidities, HbA1c, and EATVi were independently associated with LVDD. To our knowledge, this is the first study to assess the risk of LVDD progression in individuals with NAFLD by a nomogram. The widespread use of this nomogram in NAFLD patients may boost their willpower and compliance with long-term life interventions, while also allowing clinicians to adjust treatment regimens in a timely manner to avoid LVDD progression.
Since Granér et alCitation27 first investigated the effect of EAT on the development of LV diastolic function in nondiabetic patients with NAFLD, the role of EAT in NAFLD is well studied and has been proven to increase the risk of cardiovascular disease in these patients. EAT is a component of visceral adipose tissue, which has both systemic and local effects in the vicinity of the heart. Increased EAT is consistently associated with impaired diastolic function, despite the fact that the underlying mechanisms are not fully understood.Citation9 EAT contains high levels of various cytokines, which may cause inflammation and subsequent collagen turnover.Citation28,Citation29 On the other hand, myocardial dysfunction may be induced by decreased adiponectin secretion or nitric oxide synthase activity in EAT.Citation30 Both may act directly on cardiomyocytes or indirectly through impaired microvascular relaxation in the myocardium, leading to LVDD.Citation31,Citation32 Reassuringly, according to the findings of Rider et al,Citation17 weight loss can at least partially improve obesity-induced LVDD. Therefore, it is meaningful to assess the risk or severity of LVDD by detecting the EAT amount in NAFLD patients.
Although the EAT measurement by echocardiography boasts unique advantages such as cheap, easily obtained, and fast application, it can only indirectly reflect the EAT volume. The accuracy is lower than that of EAT volume measured by CT or MRI.Citation33 It has been recognized that EAT volume is an independent correlate of LVDD.Citation34–36 In addition to EAT volume, our study revealed that number of comorbidities (T2DM, hypertension, obesity) and Hb1Ac were also independent correlates of LVDD after screened by LASSO and multivariate Logistic models. These findings are expected because T2DM and hypertension are usual suspects of LVDD.Citation37–39 Notably, BMI was not independently associated with LVDD in this study, suggesting that a moderate decrease in BMI from weight reduction did not have a significant effect on LVDD unless BMI was reduced below 25 kg/m2.
The established nomogram in this study showed satisfied discrimination and calibration, and obtained significant clinical benefit in detecting NAFLD patients at the risk of LVDD progression. It is helpful to dynamically evaluate the risk of LVDD progression during long-term lifestyle intervention if further validated. When the predicted risk of LVDD progression in an NAFLD patient with a normal diastolic function is greater than 50%, more effective weight reduction interventions, such as increased intensity of physical exercise on the premise of a low-calorie diet, and more aggressive glycemic control should be recommended. Furthermore, a re-evaluation with the nomogram should be performed after one year to ensure his risk remains below 50%.
We acknowledge that this study has several limitations. The retrospective and cross-sectional design of this study limited our access to longitudinal data and outcomes in NAFLD patients. As a result, our model was unable to predict when NAFLD patients with a normal diastolic function would progress to LVDD. Furthermore, no external validation was applied to our model due to the limited sample size. Further multi-center prospective investigations are required in the future to improve the ability of our model in predicting the time of LVDD progression and to remedy the absence of a validation study.
Conclusion
We developed a nomogram, which incorporated number of comorbidities, HbA1c, and EATVi, for estimating the likelihood of LVDD progression in NAFLD patients. Our model may identify NAFLD patients with a normal diastolic function who are at a high risk of LVDD progression, thus contributing to effective prevention of LVDD progression by improving their adherence to life interventions and timely adjusting treatment regimens.
Data Sharing Statement
The data during the current study are available from the corresponding author on reasonable request.
Ethical Approval
Ethical approval for the study was obtained from the ethics committee of Hwa Mei Hospital, University of Chinese Academy of Sciences (YJ-NBEY-KY-2021-081-01).
Informed Consent
Informed consents were obtained from all participants.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Study design: Jinying Xia, Jianhui Li, and Qifeng Hua.
Data collection and analysis: Jianhui Li, Guang Jin, and Danzhen Yao.
Supervision: Jinying Xia and Qifeng Hua.
Statistics: Jinying Xia, Jianhui Li, Guang Jin, and Danzhen Yao.
Manuscript writing: Jinying Xia, Jianhui Li, Guang Jin, and Danzhen Yao.
Manuscript revision: Jinying Xia and Qifeng Hua.
Approval of the manuscript: all authors.
Disclosure
The authors declare that they have no conflicts of interest in this work.
Additional information
Funding
References
- Ibrahim EH, Dennison J, Frank L, Stojanovska J. Diastolic cardiac function by MRI-imaging capabilities and clinical applications. Tomography. 2021;7(4):893–914. doi:10.3390/tomography7040075
- Morbach C, Wanner C, Störk S. [Update on diastolic heart failure]. Internist. 2022. doi:10.1007/s00108-022-01286-z
- Grigorescu ED, Lacatusu CM, Floria M, Mihai BM, Cretu I, Sorodoc L. Left ventricular diastolic dysfunction in type 2 diabetes-progress and perspectives. Diagnostics. 2019;9(3):121. doi:10.3390/diagnostics9030121
- Beladan CC, Botezatu S, Popescu BA. Reversible left ventricular diastolic dysfunction-overview and clinical implications. Echocardiography. 2020;37(11):1957–1966. doi:10.1111/echo.14838
- Herszkowicz N, Barbato A, Salvi W, et al. Contribution of Doppler echocardiography to the evaluation of systolic and diastolic function of obese women versus a control group. Arq Bras Cardiol. 2001;76(3):189–196. doi:10.1590/s0066-782x2001000300002
- Wong CY, O’Moore-Sullivan T, Leano R, Byrne N, Beller E, Marwick TH. Alterations of left ventricular myocardial characteristics associated with obesity. Circulation. 2004;110(19):3081–3087. doi:10.1161/01.Cir.0000147184.13872.0f
- Russo C, Jin Z, Homma S, et al. Effect of obesity and overweight on left ventricular diastolic function: a community-based study in an elderly cohort. J Am Coll Cardiol. 2011;57(12):1368–1374. doi:10.1016/j.jacc.2010.10.042
- Poirier P, Giles TD, Bray GA, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113(6):898–918. doi:10.1161/circulationaha.106.171016
- Park HE, Choi SY, Kim M. Association of epicardial fat with left ventricular diastolic function in subjects with metabolic syndrome: assessment using 2-dimensional echocardiography. BMC Cardiovasc Disord. 2014;14:3. doi:10.1186/1471-2261-14-3
- Browning JD, Szczepaniak LS, Dobbins R, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40(6):1387–1395. doi:10.1002/hep.20466
- Pouwels S, Sakran N, Graham Y, et al. Non-alcoholic fatty liver disease (NAFLD): a review of pathophysiology, clinical management and effects of weight loss. BMC Endocr Disord. 2022;22(1):63. doi:10.1186/s12902-022-00980-1
- Lonardo A, Sookoian S, Pirola CJ, Targher G. Non-alcoholic fatty liver disease and risk of cardiovascular disease. Metabolism. 2016;65(8):1136–1150. doi:10.1016/j.metabol.2015.09.017
- Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol. 2015;62(1, Supplement):S47–S64. doi:10.1016/j.jhep.2014.12.012
- VanWagner LB, Wilcox JE, Colangelo LA, et al. Association of nonalcoholic fatty liver disease with subclinical myocardial remodeling and dysfunction: a population-based study. Hepatology. 2015;62(3):773–783. doi:10.1002/hep.27869
- Petta S, Argano C, Colomba D, et al. Epicardial fat, cardiac geometry and cardiac function in patients with non-alcoholic fatty liver disease: association with the severity of liver disease. J Hepatol. 2015;62(4):928–933. doi:10.1016/j.jhep.2014.11.030
- Nseir W, Hellou E, Assy N. Role of diet and lifestyle changes in nonalcoholic fatty liver disease. World J Gastroenterol. 2014;20(28):9338–9344. doi:10.3748/wjg.v20.i28.9338
- Rider OJ, Francis JM, Ali MK, et al. Beneficial cardiovascular effects of bariatric surgical and dietary weight loss in obesity. J Am Coll Cardiol. 2009;54(8):718–726. doi:10.1016/j.jacc.2009.02.086
- Luaces M, Cachofeiro V, García-Muñoz-Najar A, et al. Anatomical and functional alterations of the heart in morbid obesity. Changes after bariatric surgery. Rev Esp Cardiol. 2012;65(1):14–21. doi:10.1016/j.recesp.2011.06.018
- European Association for the Study of The Liver, European Association for the Study of Diabetes. EASL-EASD-EASO Clinical practice guidelines for the management of non-alcoholic fatty liver disease. Diabetologia. 2016;59(6):1121–1140. doi:10.1007/s00125-016-3902-y
- Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology. 2012;55(6):2005–2023. doi:10.1002/hep.25762
- World Health Organization. The Asia-Pacific perspective: redefining obesity and its treatment; 2000.
- Flüchter S, Haghi D, Dinter D, et al. Volumetric assessment of epicardial adipose tissue with cardiovascular magnetic resonance imaging. Obesity. 2007;15(4):870–878. doi:10.1038/oby.2007.591
- Dey D, Wong ND, Tamarappoo B, et al. Computer-aided non-contrast CT-based quantification of pericardial and thoracic fat and their associations with coronary calcium and Metabolic Syndrome. Atherosclerosis. 2010;209(1):136–141. doi:10.1016/j.atherosclerosis.2009.08.032
- Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18(12):1440–1463. doi:10.1016/j.echo.2005.10.005
- Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2016;17(12):1321–1360. doi:10.1093/ehjci/jew082
- Tibshirani R. Regression shrinkage and selection via the lasso. J R Stat Soc Series B. 1996;58(1):267–288. doi:10.1111/j.2517-6161.1996.tb02080.x
- Granér M, Nyman K, Siren R, et al. Ectopic fat depots and left ventricular function in nondiabetic men with nonalcoholic fatty liver disease. Circ Cardiovasc Imaging. 2015;8(1). doi:10.1161/circimaging.114.001979
- Mazurek T, Zhang L, Zalewski A, et al. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation. 2003;108(20):2460–2466. doi:10.1161/01.Cir.0000099542.57313.C5
- Mak GJ, Ledwidge MT, Watson CJ, et al. Natural history of markers of collagen turnover in patients with early diastolic dysfunction and impact of eplerenone. J Am Coll Cardiol. 2009;54(18):1674–1682. doi:10.1016/j.jacc.2009.08.021
- Greenstein AS, Khavandi K, Withers SB, et al. Local inflammation and hypoxia abolish the protective anticontractile properties of perivascular fat in obese patients. Circulation. 2009;119(12):1661–1670. doi:10.1161/circulationaha.108.821181
- Silberman GA, Fan TH, Liu H, et al. Uncoupled cardiac nitric oxide synthase mediates diastolic dysfunction. Circulation. 2010;121(4):519–528. doi:10.1161/circulationaha.109.883777
- Löhn M, Dubrovska G, Lauterbach B, Luft FC, Gollasch M, Sharma AM. Periadventitial fat releases a vascular relaxing factor. FASEB J. 2002;16(9):1057–1063. doi:10.1096/fj.02-0024com
- Wong CX, Ganesan AN, Selvanayagam JB. Epicardial fat and atrial fibrillation: current evidence, potential mechanisms, clinical implications, and future directions. Eur Heart J. 2017;38(17):1294–1302. doi:10.1093/eurheartj/ehw045
- Ansaldo AM, Montecucco F, Sahebkar A, Dallegri F, Carbone F. Epicardial adipose tissue and cardiovascular diseases. Int J Cardiol. 2019;278:254–260. doi:10.1016/j.ijcard.2018.09.089
- Cavalcante JL, Tamarappoo BK, Hachamovitch R, et al. Association of epicardial fat, hypertension, subclinical coronary artery disease, and metabolic syndrome with left ventricular diastolic dysfunction. Am J Cardiol. 2012;110(12):1793–1798. doi:10.1016/j.amjcard.2012.07.045
- Meng X, Wang W, Zhang K, et al. Epicardial adipose tissue volume is associated with non-alcoholic fatty liver disease and cardiovascular risk factors in the general population. Ther Clin Risk Manag. 2018;14:1499–1506. doi:10.2147/tcrm.S168345
- Kenny HC, Abel ED. Heart failure in type 2 diabetes mellitus: impact of glucose-lowering agents, heart failure therapies, and novel therapeutic strategies. Circ Res. 2019;124(1):121–141. doi:10.1161/CIRCRESAHA.118.311371
- Newman JD, Schwartzbard AZ, Weintraub HS, Goldberg IJ, Berger JS. Primary prevention of cardiovascular disease in diabetes mellitus. J Am Coll Cardiol. 2017;70(7):883–893. doi:10.1016/j.jacc.2017.07.001
- Nadruz W, Shah AM, Solomon SD. Diastolic dysfunction and hypertension. Med Clin. 2017;101(1):7–17. doi:10.1016/j.mcna.2016.08.013