Abstract
Introduction
In Colombia, HIV and gestational syphilis are notifiable events; however, they are poorly investigated infections in men who have sex with men (MSM).
Objective
To determine the prevalence of HIV, Treponema pallidum, and their co-infection in MSM treated at a Health Services Provider Institution (HSPI) specialized in infectious diseases from Medellín.
Methods
Cross-sectional study with 3454 MSM. Prevalence was determined with its 95% confidence interval; associated factors were identified using Fisher’s Exact test, Pearson’s Chi-square, and trend Chi-square. Multivariate adjustment was performed using logistic regression. Analyses were performed using SPSS 29.0.
Results
The prevalence of HIV was 5.7%, T. pallidum 0.7%, and co-infection 0.6%. The prevalence of HIV was higher in MSM aged between 24–40 years (7.5%), with technical or university studies (10.0%), without health insurance affiliation (12.4%), and those who have had a sexual partner with HIV (36.2%). T. pallidum was higher in MSM without health insurance affiliation (3.4%), who had sexual relations with people diagnosed with an STI (5.9%), and a sexual partner with HIV (12.1%). Co-infection was higher in MSM without health insurance affiliation (2.7%), and those who had a partner with HIV (11.2%).
Conclusion
Compared with the general Colombian population, MSM have a higher risk of HIV, but are similar to T. pallidum. The identification of the main associated factors in each infection demonstrates the need to prioritize subgroups of MSM that show greater vulnerability to these events. This research demonstrates the urgency of implementing health education strategies in MSM who have a sexual partner with HIV or other STIs. Large gaps were also evident in the magnitude of the three events according to the health insurance affiliation regime, which demonstrates problems of social and health injustice, especially with MSM without health insurance affiliation.
Introduction
Every day, more than one million people contract a sexually transmitted infection (STI), with most cases being asymptomatic.Citation1 Over 30 sexually transmissible microorganisms have been identified, with the most prevalent in bacterial etiology being those causing syphilis, gonorrhea, and chlamydia; trichomoniasis in parasitic etiology; and Hepatitis B, Herpes simplex, Human Papillomavirus, and Human Immunodeficiency Virus (HIV) in viral etiology.Citation1 In Colombia, STIs constitute a significant cause of morbidity and mortality, with negative effects on individual health and high healthcare costs.Citation2 Among these infections, syphilis and HIV stand out due to their high prevalence, especially in the young and adult population, their risks for maternal and neonatal health, and shared risk factors and transmission mechanisms. It is worth noting that STIs causing ulcers, such as syphilis, facilitate the entry of HIV, and individuals infected with HIV have a higher risk of acquiring syphilis due to immunosuppression, creating a synergistic effect between these two STIs.Citation3,Citation4
In 2022, the global number of people living with HIV was 39 million, with 1.3 million new infections reported in the same year.Citation5 Homosexual men and men who have sex with men (MSM) recorded a prevalence of 7.7% (10 times higher than that reported in adults from the general population in whom the prevalence was 0.7%).Citation5 Regarding syphilis, the World Health Organization (WHO) reported 5.6 million new cases in 2016.Citation6 A systematic review on T. pallidum covering the period from 2000 to 2020 revealed a prevalence of 7.5%, which increased to 10.6% in data from Latin America and the Caribbean.Citation7 In Colombia, approximately 20,000 new cases of HIV are reported annually, with an incidence of 39.2 per 100,000 inhabitants, approximately 40% of which are in MSM.Citation8,Citation9 The incidence of syphilis is approximately 300 per 100,000 people, with prevention, diagnosis, and treatment efforts primarily focused on pregnant women and their children, leading to a lack of solid data on syphilis in the general population or at-risk groups.Citation10
In terms of research, several studies have highlighted a high prevalence of co-infection with HIV and Treponema pallidum. In Asia, a systematic review in 2023 showed a prevalence of 3.0%.Citation11 In 2021, the Hospital in Guayaquil, Ecuador reported a syphilis prevalence of 5.2% in individuals with HIV.Citation12 In Venezuela in 2022, 15.6% of subjects with a recent diagnosis of HIV were co-infected with Treponema pallidum. In Colombia, there are also reports of this co-infection, with 2.1% coinfection found in 1698 individuals from the general population with HIV in Montería,Citation13 and a study in Medellín involving the general population, MSM, and vulnerable young people from a social organization reported a co-infection rate of 1.5%.Citation14
Men who have sex with men (MSM) represent a significantly affected population concerning HIV and T. pallidum, with vulnerability stemming from a combination of biological, behavioral, and socio-structural factors. Biologically, unprotected anal sex is associated with a higher risk of STI transmission due to the exposure of the rectal mucosa, lack of lubrication, and increased vascularity of the area, factors that favor the presence of lesions and heightened susceptibility to infections.Citation15 Behavioral factors include the prevalence of multiple sexual partners, inconsistent condom use, and recreational drug use, all of which can increase the likelihood of infection.Citation16 Moreover, structural factors such as stigma, discrimination, and the criminalization of sex behavior in certain societies may limit MSM’s access to sexual health services, including education on STIs, testing, and treatment.Citation17 In other contexts, migration and displacement have been indicated to hinder access to healthcare, making MSM vulnerable to sexual exploitation and exposure to infectious diseases due to poor living conditions.Citation18
In addition to the risk of these infections in MSM, various authors have reported extensive heterogeneity in the associated factors. These may include having a higher number of sexual partners,Citation19,Citation20 not using condoms,Citation19 engaging in receptive anal sex,Citation21 identifying as homosexual or bisexual,Citation19,Citation22 a history of STIs,Citation23 alcohol consumption,Citation21–23 lack of a stable partner,Citation20,Citation21 and educational level.Citation20,Citation24
Despite this background, research on this co-infection in MSM is scarce in Colombia, as evidenced by the limited number of studies found in PubMed, ScienceDirect, SciELO, OVID, and other multidisciplinary databases using the terms (HIV AND (Syphilis OR T. pallidum) AND (MSM OR men who have sex with men) AND Colombia. This scarcity hinders understanding the magnitude of the problem and associated factors, impedes the design of effective prevention and control strategies tailored to the needs of MSM, and prevents knowledge of the impact of health interventions, among other crucial aspects for mitigating health risks in this group. Therefore, the present study aimed to determine the prevalence of HIV and Treponema pallidum, as well as their coinfection, in MSM attending at a specialized health service provider for infectious diseases in Medellin.
Methods
Study Design and Subjects
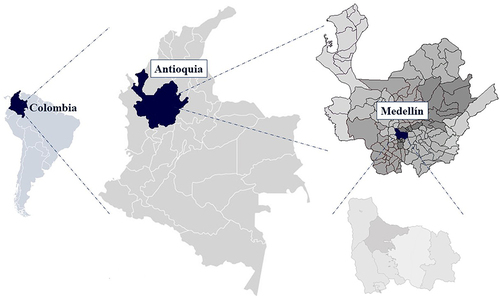
A cross-sectional study was conducted with 3454 MSM attended at the Fundación Antioqueña de Infectología (FAI) selected with non-probabilistic sampling. FAI is an institution that attracts patients both intramurally and extramurally in public spaces frequented by MSM (saunas, steam rooms, meeting rooms of foundations, typically located in the city center), located in Medellin-Colombia (). Men aged 14 to 75 who reported having sex with other men, regardless of their sexual orientation or identity (including heterosexuals, bisexuals, pansexuals), voluntarily agreed to be screened for HIV and T. pallidum at the FAI and signed informed consent.
Diagnostic Test
The SD BIOLINE HIV/Syphilis Duo® was used in peripheral blood samples. This test is a solid-phase chromatographic immunoassay detecting IgG, IgM, and IgA antibodies specific to T. pallidum using strips coated with recombinant capture antigens of 17 kDa, with a sensitivity and specificity of 99.7%. For HIV, it includes recombinant antigens gp41 and p24 specific to HIV-1, including subtypes O and gp36 for HIV-2, with a sensitivity and specificity of 99%. A second test in peripheral blood, Alere Determine TM HIV-1/2 Ag/Ab combo, was applied internally to positive cases, an immunochromatography for the qualitative detection of p24 antigen and HIV 1/2 antibodies, with a sensitivity of 100% and specificity of 99.7%.
Data Collection
Secondary information source was collected from the FAI records, in an anonymized Excel file. The FAI field team, comprising a physician, project leader, community work coordinator, and nursing assistants, conducted various workshops, playful encounters, and theatrical performances to promote STI screening. MSM expressing interest in participating were interviewed by the team’s doctor, who conducted pre-test counseling. If the individual agreed to participate, the study was explained to them and they provided informed consent. Subsequently, a nursing assistant administered a survey capturing socioeconomic data and sexual risk factors, while also collecting peripheral blood samples processed at a high-complexity clinical laboratory in the city. Upon obtaining diagnostic test results, the FAI doctor delivered the results, provided post-test counseling, and, for positive cases, activated the patient’s care pathway in the treating healthcare institution or provided direct care at the FAI by their infectious disease team.
Information Bias Control
Information bias was controlled through data collection by medical personnel, an extramural fieldwork manual with apparent validity, motivational campaigns for participants, pre and post-test counseling, and application of diagnostic tests with a risk of false positives (complement of specificity) or negatives (complement of sensitivity) less than 1%.
Statistical Analysis
Variables were described with absolute frequencies (#) and percentages (%). The comparison of HIV, T. pallidum, and coinfection with nominal variables was performed using Pearson’s Chi-square or Fisher’s Exact test (when at least one absolute frequency was ≤5) and Trend Chi-square for ordinal variables. Logistic regression models were used to identify confounding variables and those associated with the prevalence of each infection and coinfection, with goodness of fit determined by Wald and Hosmer-Lemeshow statistics. The presence of interaction was ruled out through multivariate logistic models, introducing independent variables (eg, variables A, B, C, and D) with interaction factors for each variable (eg, AB, AC, A*D), formulated as follows:
Statistical analyses were conducted using IBM SPSS 29.0, with p-values < 0.05 considered significant.
Results
In the study group, most of MSM were young <25 years (46.8%), had basic education (46.6%), were single (66.0%), and affiliated with the contributory health insurance system (67.6%). The most common sexual risk factors were changing sexual partners in the last six months (50.9%) and the use of hallucinogens during sexual encounters (47.2%) ().
Table 1 Socioeconomic Description and Sexual Risk Factors of the Study Group
The general prevalence of HIV was 5.7%, T. pallidum was 0.7%, and coinfection was 0.6%. The prevalence of HIV showed statistically significant differences based on education, marital status, health insurance affiliation, and specific sexual risks. Specifically, the prevalence was statistically higher in those who had not received psychoactive substances or money in exchange for sexual relations, those who had sexual relations with individuals diagnosed with STIs, and those who had a sexual partner with HIV. For T. pallidum, statistical differences were observed based on marital status, health insurance affiliation, changing sexual partners in the last six months, having sexual relations with individuals with STIs, or having had a sexual partner with HIV. Coinfection presented statistical differences with health insurance affiliation, having sexual relations with individuals with STIs, or having had a sexual partner with HIV ().
Table 2 General Prevalence of HIV, T. Pallidum, Coinfection, and Specific Prevalences According to Socioeconomic Conditions and Sexual Risk Factors
In the multivariate adjustment for HIV prevalence, marital status and sexual relations, particularly with individuals diagnosed with STIs, were identified as confounding variables (did not show statistically significant in the regression model). According to this regression model, a higher prevalence of HIV was observed in the following groups: among MSM aged 24–40 years, the prevalence was twice that found in the group aged 41–75 years old; in MSM with basic education, it was 5.2 times the prevalence in MSM without formal education, and among those with technical or university studies, it was 11.4 times that of those without formal education; in MSM without health insurance affiliation, the prevalence was 3.1 times that recorded in those affiliated with the contributory health insurance system; in those who have not had sexual relations in exchange for psychoactive substances or money, the prevalence was 2.1 times compared to those who reported this practice, and in MSM who have had a partner with HIV, the prevalence was 18.7 times compared to those who have not had such a partner ().
Table 3 Explanatory Factors for the General Prevalence of HIV, T. Pallidum, and Co-Infection
The prevalence of T. pallidum in MSM without health insurance affiliation was 4.8 times that in MSM affiliated with the contributory health insurance system; 15 times higher in those who have had sexual relations with individuals diagnosed with an STI, and 5 times higher in MSM who have had a partner with HIV. Co-infection was 5 times higher in MSM without health insurance affiliation (compared to those affiliated with the contributory health insurance system) and 47 times higher in MSM who have had a partner with HIV ().
Discussion
Prevalence of HIV and Associated Factors
Our study showed a 5.7% HIV prevalence slightly lower than the global reports in homosexuals and MSM of 7.7%.Citation5 Locally, a study reported HIV prevalence in MSM from different cities, specifically in the case of Medellín, it was 21.0% in 2016 and 11.4% in 2019. This decrease could be attributed to educational and preventive efforts for HIV in this population, improved access to healthcare services, increased awareness of the importance of preventing and timely diagnosing and treating HIV to reduce transmission.Citation25
Regarding age, the specific prevalence of HIV was higher in MSM aged 24–40 years, a finding similar to the UNICEF 2018 report, indicating that global infections are higher in individuals aged between 25 and 49 years. It also aligns with the Colombian National Institute of Health (Acronym in Spanish INS) report in 2020 on HIV in the general Colombian population, where the highest number of infections was between 25–34 years, followed by ages 15–24 and 35–44 years, mainly in the homosexual population.Citation26
In the study population, the prevalence of HIV was 11.4 times higher in MSM with technical or university studies and 5.2 times higher in MSM with basic education compared to MSM without formal education. In a study conducted in seven cities in Colombia, the prevalence of HIV among MSM with technical or technological studies was highest in Cartagena, Cali, and Cúcuta, at 21.4%, 33.4%, and 18.2%, respectively. Some reports also indicate that a higher proportion of MSM comes from individuals with a high level of education, where most cases are concentrated.Citation27,Citation28 The university environment is constantly undergoing cultural transformations regarding the acceptance of sexual diversity, openness to new sexual dynamics, and the congregation of young people who are beginning to become independent, seek new sexual experiences, and have a low perception of the risk of infection. This can increase risky sexual behaviors such as having multiple sexual partners, engaging in unprotected sexual relations, consuming drugs and alcohol before sex, and using dating apps, among other situations that warrant further study in Medellín.Citation29–33
The prevalence of HIV was higher in MSM without health insurance affiliation, aligning with a previous study in Colombia that found an infection prevalence of 25% in unaffiliated individuals, 17% for individuals under the subsidized regime, and 9.8% in the contributory regime. Understanding that unaffiliated and subsidized regime individuals correspond to groups without formal employment that involve health insurance contributions, the previously described confluence indicates a higher probability of infection in groups with socioeconomic disadvantages. This should alert health authorities to implement actions that address this inequality in HIV figures based on the type of health insurance affiliation.Citation28
The prevalence of HIV was also higher in MSM who had not had sexual relations in exchange for psychoactive substances or money. This contradicts the available evidence on this risk factor, as transactional sex is associated with socioeconomic vulnerability, recreational drug use, and a higher probability of reporting other HIV risk behaviors such as unprotected anal sex.Citation34,Citation35 In this study population, the lower prevalence of HIV in those who reported sexual relations in exchange for psychoactive substances or money may be explained by health education efforts on these risk factors or the targeting of some health campaigns by health departments in areas of the city that concentrate transactional sex, prostitution, and drug use. However, further studies are needed to delve into the explanatory factors for this finding.
The prevalence of HIV was higher among MSM who had a HIV-positive partner, which aligns with previous data from Colombia reporting a high proportion of MSM who know that their partner has HIV, especially in those who have had a stable partner in the last year.Citation28 In this context, it is important to highlight several aspects: (i) having sexual relations with a person whose viral load is completely suppressed through antiretroviral therapy (ART) is safe; (ii) correct condom use is also considered an effective measure to prevent transmission; (iii) pre-exposure prophylaxis for HIV-negative individuals at high risk of contracting the virus, under proper medical supervision, has proven to be effective, indicating that sex can be considered safe even with HIV-positive individuals.Citation36,Citation37 In this regard, efforts should be made to improve educational strategies on the prevention of transmission risks among HIV-positive individuals or their partners through various means, such as sharp or pointed objects, unprotected sexual relations, and low adherence to ART.Citation37 Finally, it is relevant to consider that adherence to ART can be affected by multiple social issues, mainly stigma, discrimination, mistreatment, rejection, drug use during sex, combined medication use, and structural barriers.Citation28,Citation38
Prevalence of T. Pallidum, Co-Infection with HIV, and Associated Factors
The prevalence of T. pallidum was 0.7%. In Latin America and the Caribbean, a prevalence of 10.6% has been reported.Citation7 This finding contrast notably with the current study, challenging the projected trend of increasing syphilis infections in the general population of the Americas.Citation39 The low recorded prevalence could be attributed to a combination of factors, including specific public health interventions such as “Medellín me cuida”, which in 2022 conducted around 10,000 rapid HIV tests and 5000 syphilis tests; 520 educational activities in sexual and reproductive health listening centers, and 204 “city takeovers”.Citation40 It is also necessary to explore the improvement of preventive practices, such as increased awareness of condom use during sexual relations, decreased number of sexual partners, more frequent testing to mitigate transmission, especially in asymptomatic individuals, increased diagnostic efforts, and the supply of treatments as a result of increased affiliation with the General Social Security System in Health, among others.Citation6,Citation41–44
The prevalence of T. pallidum was higher in MSM without health insurance affiliation. Although Colombia lacks data on the prevalence of syphilis in MSM in different health regimes, it is clear that the absence of affiliation is one of the main barriers to access basic health promotion and prevention programs, screening, diagnosis, and treatment.Citation45
The prevalence of T. pallidum was 15 times higher in those who had sexual relations with individuals diagnosed with an STI. Although specific information on this prevalence is limited to contrast our data, this phenomenon can be attributed to the confluence of multiple factors: greater exposure to T. pallidum or other agents that facilitate this infection, exposure to general risk factors for STIs such as unprotected sex or contact with multiple sexual partners, higher risk of coinfection and reinfection, especially in STIs that cause skin lesions, low risk perception, or little awareness of the importance of preventing such infections,Citation31,Citation46–50 among other factors that highlight the difficulty of reducing STI morbidity in this subgroup of MSM.
The prevalence of T. pallidum was 5 times higher in MSM who had a partner with HIV, a finding that agrees with previous research that has established a significant association between HIV infection and an increased risk of acquiring syphilis, attributable to shared risk factors and the microbiological convergence of these two infections.Citation3,Citation4,Citation15,Citation16,Citation51 In this context, the prevalence of co-infection was 0.6%. Although the magnitude of this co-infection in MSM is not well known in Colombia, other authors have reported a higher magnitude. For instance, in Paraguay, the prevalence of HIV-syphilis co-infection in 315 MSM was 6%,Citation47,Citation52 in Ecuador, a study with 1002 HIV-positive individuals found a co-infection rate of 4.8%,Citation18 and in Brazil, it was 10%.Citation23 All of this is attributable to the biological, behavioral, and social risks shared by these two STIs.Citation3,Citation15–17,Citation48 As discussed previously for each infection, coinfection was higher in those without health insurance and those who had a partner with HIV, demonstrating structural healthcare system gaps, as well as low awareness of the importance of breaking the STI transmission chain.
Limitations and Strengths
The primary limitations lie in the fact that the statistical associations are not of a causal nature, and there was not a comprehensive record of the main sexual risk factors. Among the strengths, it is worth highlighting that this is one of the few Colombian studies with a substantial sample size of men who have sex with men (MSM). The assessment of coinfection as an independent outcome and the identification of social inequities in a group inherently stigmatized are notable strengths.
Conclusion
In comparison to the general Colombian population, MSM face a higher risk of HIV but a similar risk for T. pallidum. The identification of key factors associated with each infection underscores the need to prioritize specific subgroups of MSM that exhibit greater vulnerability to these events. This research highlights the urgency of implementing health education strategies for MSM who have had a sexual partner with HIV, given its strong association with HIV, T. pallidum, and coinfection. Furthermore, significant disparities were observed in the prevalence of the three events based on health insurance affiliation, indicating issues of social and healthcare injustice, particularly for MSM without health insurance.
Data Sharing Statement
Data has not been deposited in a public repository. Anonymized data is available on reasonable request to the authors.
Ethics Approval and Consent to Participate
The study complies with the Declaration of Helsinki. The study received approval from the scientific committee of the FAI and adhered to the guidelines of Colombia’s Ministry of Health Resolution 8430, categorizing it as a risk-free study. Additionally, Resolution 1995 of 1999, governing the handling of medical records and access to this information by the healthcare team, was followed. Compliance with National Decree 1377 of 2013, partially regulating Law 1581 of 2012 for the protection of personal data, was ensured. Recommendations from the World Health Organization regarding informed consent, confidentiality, counseling, result quality, and referral to health services for treatment were implemented. The database information was coded to guarantee the confidentiality of information and not jeopardize the identity or privacy of individuals (non-linked or anonymized information). All participants signed informed consent forms before participation. In cases where possible, parental consent was obtained; however, according to sentence C-246/17 and T-675-17 about the Self-determination of minors; the Constitutional Court of the Republic of Colombia in 2017 determined that parental consent is not necessary in these cases given that the age of 14 has been established that minors may have the maturity to begin to assume obligations and responsibilities in society, such as marriage, consent of sexual relations, and the right to privacy in the family environment.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in relation to this work and declared no potential conflicts of interest with respect to the research and publication of this article.
References
- Organización Mundial de la Salud [World Health Organization]. Infecciones de transmisión sexual [Sexually transmitted infections (STIs)]; 2023. Available from: https://www.who.int/es/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis). Accessed April 10, 2024.
- Ministerio de Salud y Protección Social. Infecciones de transmisión sexual [Sexually transmitted infections (STIs)]; 2023. Available from: https://www.minsalud.gov.co/salud/publica/ssr/Paginas/infecciones-transmision-sexual-vih-sida.aspx. Accessed April 10, 2024.
- Ministerio de Salud y Protección Social. Otras infecciones de transmisión sexual (ITS) [Other sexually transmitted infections (STIs)]; 2023. Available from: https://www.minsalud.gov.co/salud/publica/ssr/Paginas/Otras-infecciones-de-transmision-sexual-ITS.aspx. Accessed April 10, 2024.
- Rodríguez I, Rodríguez ME, Fernández C, Blanco O, Llop A. Diagnóstico serológico de sífilis en pacientes cubanos con VIH/SIDA [Serological diagnosis of syphilis in Cuban HIV/AIDS patients]. Rev Cubana Med Trop. 2021;73(1):e489.
- ONUSIDA. Hoja informativa - Últimas estadísticas sobre el estado de la epidemia de sida [UNAIDS. Global HIV & AIDS statistics — Fact sheet]; 2022. Available from: https://www.unaids.org/es/resources/fact-sheet. Accessed April 10, 2024.
- Organización Panamericana de la Salud [Pan American Health Organization]. Sífilis [Syphilis]; 2018. Available from: https://www3.paho.org/hq/index.php?option=com_content&view=article&id=14869:sti-syphilis&Itemid=0&lang=es#gsc.tab=0. Accessed April 10, 2024.
- Tsuboi M, Evans J, Davies EP, et al. Prevalence of syphilis among men who have sex with men: a global systematic review and meta-analysis from 2000–20. Lancet Glob Health. 2021;9(8):e1110–8. doi:10.1016/S2214-109X(21)00221-7
- Instituto Nacional de Salud. Informe de evento y tableros de control. Informe de evento y tableros de control. Año 2022/ VIH-SIDA/ VIH PE Xlll 2022. VIH/SIDA Periodo epidemiológico XIII [Event reporting and dashboards. Epidemiological period XII]. Colombia; 2022. Available from: https://www.ins.gov.co/buscador-eventos/Informesdeevento/VIH%20PE%20XIII%202022.pdf. Accessed April 10, 2024.
- Cuenta de Alto Costo C. VIH Sida en Colombia, retos y apuestas en salud [HIV AIDS in Colombia, challenges and bets on health]; 2020. Available from: https://cuentadealtocosto.org/vih/vih-sida-en-colombia-retos-y-apuestas-en-salud/. Accessed April 10, 2024.
- García-Luna JA, Romero-Rosas N, Silva-Peña SA, et al. Diagnostic performance of two rapid tests for syphilis screening in people living with HIV in Cali, Colombia. PLoS One. 2023;18(3):e0282492. doi:10.1371/journal.pone.0282492
- Mahmud S, Mohsin M, Muyeed A, Islam MM, Hossain S, Islam A. Prevalence of HIV and syphilis and their co-infection among men having sex with men in Asia: a systematic review and meta-analysis. Heliyon. 2023;9(3):e13947. doi:10.1016/j.heliyon.2023.e13947
- Ferrín Sabando VJ, Murillo Carriel JJ. Prevalencia de Sífilis en pacientes con VIH/SIDA en el Hospital DR José Daniel Rodríguez Maridueña de Guayaquil en 2021. [Prevalence of Syphilis in patients with HIV/AIDS in the Guayaquil Hospital DR José Daniel Rodríguez Maridueña in 2021] Tesis; 2023. Available from: http://repositorio.ug.edu.ec/handle/redug/69359. Accessed April 10, 2024.
- Tapia Y. Prevalencia de sífilis en adultos VIH positivos en una IPS, Montería [Prevalence of syphilis in HIV positive adults in an IPS, Montería]. Tesis; 2021. Available from: https://repositorio.unicordoba.edu.co/entities/publication/8348466b-12cb-4111-a37b-8873cd2f1777. Accessed April 10, 2024.
- Cardona Arias J, Higuita-Gutiérrez LF, Cataño-Correa JC. Prevalencia de infección por Treponema pallidum en individuos atendidos en un centro especializado de Medellín, Colombia [Prevalence of Treponema pallidum infection in individuals treated in a specialized center in Medellín, Colombia]. Rev Fac Nac Salud Pública. 2022;40(1):e343212. doi:10.17533/udea.rfnsp.e343212
- Cruz-Palacios C, Ramos-Alamillo U, González-Rodríguez A. Guía de prevención, diagnóstico y tratamiento de las ITS: dirigida a personal de servicios de salud [Guide to prevention, diagnosis and treatment of STIs: aimed at health services personnel]. Gob.mx; 2011. Available from: https://www.gob.mx/cms/uploads/attachment/file/27258/guia_its.pdf. Accessed April 10, 2024.
- Beyrer C, Baral SD, van Griensven F, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380(9839):367–377. doi:10.1016/s0140-6736(12)60821-6
- Pachankis JE, Hatzenbuehler ML, Hickson F, et al. Hidden from health. Structural stigma, sexual orientation concealment, and HIV across 38 countries in the European MSM Internet Survey. AIDS. 2015;10:1239–1246. doi:10.1097/QAD.0000000000000724
- Organización Mundial de la Salud. Los migrantes y los refugiados presentan un mayor riesgo de tener mala salud que las poblaciones de acogida [Migrants and refugees are at higher risk of poor health than host populations]; 2019. Available from: https://www.who.int/es/news/item/21-01-2019-21-01-2019-21-01-2019-migrants-and-refugees-at-higher-risk-of-developing-ill-health. Accessed April 10, 2024.
- Huamán-García M, Pereira-Victorio C, Valladares-Garrido D, Valladares-Garrido M. Factores asociados a la coinfección VIH-sífilis [Factors associated with HIV-syphilis coinfection]. Revista Cubana de Medicina Militar. 2022;51:3.
- Das A, Li J, Zhong F, et al. Factores asociados con la coinfección por VIH y sífilis entre hombres que tienen sexo con hombres en siete ciudades chinas [Factors associated with HIV and syphilis co-infection among men who have sex with men in seven Chinese cities]. Int J ETS SIDA. 2015;26(3):145–155. doi:10.1177/0956462414531560
- Varshney K, Ikanovic A, Ghosh P, et al. A Global Scoping Review of the Factors Associated with HIV and Syphilis Co-Infection: Findings from 40 Countries. Venereología. 2022;1(1):98–113. doi:10.3390/venereology1010007
- Das A, Li J, Zhong F, et al. Factors associated with HIV and syphilis coinfection among men who have sex with men in seven Chinese cities. Int J STD AIDS. 2015;26(3):145–155. doi:10.1177/0956462414531560
- Simões LA, Mendes JC, Silveira MR, Costa AMGD, Lula MD, Ceccato MDGB. Factors associated with HIV/syphilis coinfection initiation of antiretroviral therapy. Rev Saúde Pública. 2022;56:59. doi:10.11606/s1518-8787.2022056003904
- Gilbert L, Dear N, Esber A, et al.; AFRICOS Study Group. Prevalence and risk factors associated with HIV and syphilis co-infection in the African Cohort Study: a cross-sectional study. BMC Infect Dis. 2021;21(1):1123. doi:10.1186/s12879-021-06668-6
- Enterritorio. Por primera vez Colombia cuenta con datos actualizados sobre población vulnerable al VIH [For the first time, Colombia has updated data on the population vulnerable to HIV]. Gov.co; 2020. Available from: https://www.enterritorio.gov.co/web/node/1006. Accessed April 10, 2024.
- Instituto Nacional de Salud. Informe de evento. VIH, SIDA Y MUERTE POR SIDA COLOMBIA 2020 [Event report. HIV, AIDS AND DEATH FROM AIDS COLOMBIA]. Gov.co; 2020. Available from: https://www.ins.gov.co/buscador-eventos/Informesdeevento/VIH-SIDA_2020.pdf. Accessed April 10, 2024.
- MINSALUD & UNFPA. Estudio sobre comportamiento sexual y prevalencia de VIH en hombres que tienen relaciones sexuales con hombres en siete ciudades de Colombia [Sexual behavior and HIV prevalence in men who have sex with men in seven cities in Colombia]. Gov.co; 2010. Available from: https://www.minsalud.gov.co/salud/Documents/observatorio_vih/documentos/monitoreo_evaluacion/2_evaluacion_respuesta/b_estudios_complementarios/Resultados_Estudio_HSH_final125.pdf. Accessed April 10, 2024.
- Departamento Nacional de Planeación. Comportamiento sexual y prevalencia de VIH en hombres que tienen relaciones sexuales con hombres en tres ciudades de Cali [Sexual behavior and HIV prevalence in men who have sex with men in three cities in Colombia: Bogotá, Medellín and Santiago de Cali] Colombia: Bogotá, Medellín y Santiago de Cali; 2019; Available from: https://editorial.ces.edu.co/wp-content/uploads/2020/07/Comportamiento-sexual-y-prevalencia-VIH_baja.pdf. Accessed April 10, 2024.
- Aguirre Rivera JC, Restrepo Soto JA. Conducta sexual en jóvenes universitarios: estudio de revisión [Sexual behavior in Ibero-American youth: review study]. Psicogente. 2022;25(48):1–28. doi:10.17081/psico.25.48.5500
- Paz Bermudez M, Ramiro MT, Teva I, Ramiro Sanchez T, Buela Casal G. Conducta sexual y realización de la prueba del virus de la inmunodeficiencia humana en jóvenes que estudian en la universidad en Cuzco (Perú) [Sexual behaviour and human immunodeficiency virus testing in university students from Cuzco (Peru)]; 2017. Available from: https://www.clinicalkey.es/service/content/pdf/watermarked/1-s2.0-S0213911117301802.pdf?locale=es_ES&searchIndex=. Accessed April 10, 2024.
- González Garrido JA, Carmona F, Seroprevalencia de VIH en población estudiantil de la Universidad Juárez Autónoma de Tabasco, campus Chontalpa [HIV seroprevalence in the student population of the Juárez Autonomous University of Tabasco, Chontalpa campus, Mexico]. UVserva. 2020;9:105–112. doi:10.25009/uvs.v0i9.2685
- UNESCO, IIEP-UNESCO, SITEAL. Perfil del país [Country profile], COLOMBIA; 2019. Available from: https://siteal.iiep.unesco.org/sites/default/files/sit_informe_pdfs/siteal_ed_colombia_20190619.pdf#:~:text=Se%20divide%20en%20dos%20ciclos%3A%20la%20educaci%C3%B3n%20b%C3%A1sica,ni%C3%B1os%20y%20ni%C3%B1as%20de%2011%20a%2014%20a%C3%B1os. Accessed April 10, 2024.
- Gea Pattier A Relación entre el uso de aplicaciones y páginas web de citas, con las conductas sexuales en adolescentes [Relationship between the use of dating applications and websites and sexual behavior in adolescents]; 2022. Available from: https://hdl.handle.net/11000/27583. Accessed April 10, 2024.
- Michelow W, Hogg R, Moore D, et al. P1-S2.60 Prevalence and correlates of giving or receiving sex for money, drugs or goods among men who have sex with men in Vancouver, British Columbia. Sex Transm Infect. 2011;87(Suppl 1):A148. doi:10.1136/SEXTRANS-2011-050108.117
- Alecrim DJD, Ceccato MDGB, Dourado I, Kerr L, Brito AM, Guimarães MDC. Factors associated with exchanging sex for money in men who have sex with men in Brazil. Cien Saude Colet. 2020;25(3):1025–1039. Portuguese, English. doi:10.1590/1413-81232020253.18052018
- CDC. If I have HIV, what is the best way to protect others? Cdc.gov; 2022. Available from: https://www.cdc.gov/hiv/spanish/basics/hiv-prevention/hiv-positive.html. Accessed April 10, 2024.
- ONUSIDA. Preguntas frecuentes con relación al VIH y el sida [Frequently asked questions about HIV and IDS]. Unaids.org. Available from: https://www.unaids.org/es/frequently-asked-questions-about-hiv-and-aids. Accessed April 10, 2024.
- ONUSIDA. Comunicado de prensa: ONUSIDA celebra el anuncio del gobierno Colombiano que permitirá a las personas acceder al tratamiento del VIH más adecuado para ellas [UNAIDS welcomes announcement by Colombian government that will enable people access to the most appropriate HIV treatment for them]. Unaids.org. Available from: https://www.unaids.org/es/resources/presscentre/pressreleaseandstatementarchive/2023/june/20230612_colombia-hiv-treatment. Accessed April 10, 2024.
- Organización Panamericana de Salud. Ante la tendencia de aumento de sífilis y sífilis congénita en algunos países de las Américas, la OPS pide reforzar acciones de salud pública [With rising trends of syphilis and congenital syphilis in some countries in the Americas, PAHO calls for reinforcement of public health measures]. Paho.org; 2022. Available from: https://www.paho.org/es/noticias/5-7-2022-ante-tendencia-aumento-sifilis-sifilis-congenita-algunos-paises-americas-ops-pide. Accessed April 10, 2024.
- Alcaldía de medellín, secretaría de salud. Con la campaña “Enfrentando Desigualdades”, Medellín conmemora el Día Mundial de la Lucha contra el Sida [With the campaign “Facing Inequalities”, Medellín commemorates World AIDS Day]. Alcaldía de Medellín; 2022. Available from: https://www.medellin.gov.co/es/sala-de-prensa/noticias/con-la-campana-enfrentando-desigualdades-medellin-conmemora-el-dia-mundial-de-la-lucha-contra-el-sida/. Accessed April 10, 2024.
- CDC. Syphilis & MSM (Men Who Have Sex With Men) – CDC Fact Sheet. Cdc.gov; 2022. Available from: https://www.cdc.gov/std/spanish/sifilis/stdfact-msm-syphilis-s.htm. Accessed April 10, 2024.
- OMS. Sífilis [Syphilis]; 2023. Available from: https://www.who.int/es/news-room/fact-sheets/detail/syphilis. Accessed April 10, 2024.
- Ministerio de Salud y Protección Social, Protección social, Régimen Subsidiado, Comportamiento del aseguramiento. Comportamiento del aseguramiento [Assurance behavior]. Gov.co. Available from: https://www.minsalud.gov.co/proteccionsocial/Regimensubsidiado/Paginas/coberturas-del-regimen-subsidiado.aspx. Accessed April 10, 2024.
- DANE. Encuesta nacional de calidad de vida [National quality of life survey]; 2022. Available from: https://www.dane.gov.co/files/investigaciones/condiciones_vida/calidad_vida/2022/comunicado_ECV_2022.pdf. Accessed April 10, 2024.
- Hospital Provincial Docente Manuel Ascunce Doménech. La Salud Pública en América Latina y El Caribe [Public Health in Latin America and the Caribbean]; 2002. Available from: https://www.researchgate.net/publication/260776163_La_Salud_Publica_en_America_Latina_y_El_Caribe. Accessed April 10, 2024.
- Chacón-Quesada T, Corrales-González D, Garbanzo-Núñez D, et al. ITS Y SIDA en adolescentes: descripción, prevención y marco legal [STIs and AIDS in adolescents: description, prevention and legal framework]. Med Leg Costa Rica. 2009;26(2):79–98.
- Sánchez-Alemán MA, Rogel-González AE, García-Cisneros S, et al. Alta seroprevalencia de sífilis y herpes genital en migrantes en tránsito en Chiapas, México [High seroprevalence of syphilis and genital herpes in migrants in transit in Chiapas, Mexico]. Rev Panam Salud Pública. 2023;47:e71. doi:10.26633/RPSP.2023.71
- Parra Sanchez M. úlceras genitales por virus herpes simplex [Genital ulcers caused by herpes simplex virus]. Enfermed Infecc y Microbiol Clin. 2019;37(4):260–264. doi:10.1016/j.eimc.2018.10.020
- Contreras E, Zuluaga SX, Ocampo V. Sífilis: la gran simuladora [Syphilis: The Great Mimicker]. Org.co. Available from: http://www.scielo.org.co/pdf/inf/v12n2/v12n2a06.pdf. Accessed April 10, 2024.
- López Domínguez DM, Peñafiel Jaramillo K, Wong Vázquez L, Hernández Bandera N. Conducta sexual y percepción del riesgo de ITS en estudiantes universitarios con enfoque de género [Sexual behavior and STI risk perception in university students with a gender perspective]. Bol Malariol Salud Ambient. 2021;61(4):664–672. doi:10.52808/bmsa.7e5.614.014
- Kawi NH, Sihotang EP, Nisa T, et al. Incidence and risk factors for syphilis infection among men who have sex with men: a cohort study from an urban sexual health clinic in Jakarta, Indonesia. Int J STD AIDS. 2022;33(12):1065–1072. doi:10.1177/09564624221125079
- Ministerio de Salud Pública y Bienestar Social. Estudio de prevalencia de VIH Sífilis, conocimientos y prácticas de riesgo de hombres que tienen sexo con hombres (HSH) en 6 Regiones Sanitarias del Paraguay; 2014. Available from: https://www.mspbs.gov.py/dependencias/pronasida/adjunto/79bff1-InformeHSH2014.pdf. Accessed April 10, 2024.