Abstract
Introduction
Polycystic ovary syndrome (PCOS) is associated with biochemical and hormonal disturbance and adverse cosmetic, reproductive, metabolic, and psychological consequences, resulting in reduced health-related quality of life (HRQoL). Various generic and specific questionnaires have been used for assessing different dimensions of HRQoL in PCOS women. The purpose of this systematic review was to identify those general and specific instruments and to determine the factors that affect HRQoL in PCOS women.
Materials and methods
The research strategy involved general and specific terms in relation to PCOS women and their QoL. A review was performed on studies that were published between 1945 to 2017 and that were indexed in MEDLINE, ISI Web of Science, and Scopus. A narrative synthesis of the data was provided.
Results
In total, 52 studies (9 qualitative and 43 quantitative) were included in the review. The analysis indicated that 3 specific and 5 general instruments were used to measure the QoL in PCOS women. Of these, the 36-Item Short Form Health Survey (SF-36) and the Polycystic Ovary Syndrome Health-Related Quality of Life Questionnaire (PCOSQ) were used most frequently. All studies assessed different aspects of QoL in PCOS women and found that PCOS had negative effects on QoL in this population.
Conclusion
The PCOSQ and the SF-36 were used most frequently for the assessment of QoL in PCOS women. Perhaps using either a specific questionnaire solely or a specific questionnaire in conjunction with a generic measure would be more appropriate when measuring QoL in PCOS women. However, both questionnaires showed that they are able to capture different aspects of QoL in PCOS women and to identify areas that can help to improve QoL in these women.
Introduction
Polycystic ovary syndrome (PCOS) is the most common hormonal disturbance that, depending on the population studied and diagnostic criteria, affects up to 15%–20% of women at reproductive age.Citation1,Citation2 The pathophysiology of this heterogeneous disease has not been clearly determined, but it is believed that it results from complex interactions between genetic, metabolic, and environmental factors.Citation3 It is characterized by hyperandrogenism, ovulatory dysfunction, and polycystic ovarian morphology.Citation4 PCOS is associated with adverse clinical complications including reproductive (menstrual irregularity and infertility),Citation2,Citation3 metabolic (insulin resistance, diabetes, and cardiovascular risk),Citation5 and psychological disabilities (anxiety and depression).Citation6 All have been mentioned as factors responsible for the reduction of life quality.Citation7
Health-related quality of life (HRQoL) is a multidimensional concept used to describe physical, emotional, and social aspects of particular diseases or their treatment.Citation8 Chronic disorders such as PCOS may have major effects on the QoL that need to be precisely assessed.Citation9
HRQoL can be assessed using both general and specific tools. General tools have generally no questions for specific conditions and diseases.Citation10 Therefore, specific tools are generally preferable for each condition assessed, and PCOS is no exception. However, both tool types have been used for measuring QoL in the literature. The aims of this study were to identify 1) studies that have used standard instruments to measure HRQoL in women with PCOS; 2) general and specific instruments that have been used for assessing HRQoL in PCOS women; and 3) the effects of PCOS on different aspects of women’s QoL.
Methods
Search engines
The electronic databases searched included MEDLINE (January 1950–March 2017), ISI Web of Knowledge (January 1945–26 July 2017), Scopus (May 2000–January 2017), and Google Scholar (March 1996–January 2017). More data were collected from the reference lists and databases related to scientific conference, and we contacted the authors of the publications to know they had any other studies which had remained unpublished.
Search strategy
In the current systematic review article, we managed to find general and specific instruments that assessed QoL, and we further delineated the factors relevant to QoL in women suffering from PCOS using key words: (questionnaire OR scale OR inventory) AND (“Quality of life” OR “Health-related quality of life” OR “Patient-Reported Outcome”) AND (“Polycystic ovary syndrome” OR “PCOS”).
Inclusion criteria
The following criteria were used to decide which relevant resources to be included:
Document type: article;
Article type: original, review, and theoretical;
Language: English;
Study design: qualitative, quantitative, and mixed methods;
Species: humans;
Subject: health and medicine;
Documents’ subjects: QoL and its related factors in PCOS women; and
Questionnaire used for HRQoL: measured more than one dimension.
Data synthesis
Two authors were asked to go through the title and abstract of the studies obtained and to read the full texts finally to decide which studies had met the criteria to be included in the current systematic review. The variables of interest were the first author’s name, year, country, study design, and study results. The two authors negotiated any disagreements to reach consensus.
In order to assess HRQoL measures, the Consensus-based Standards for the Selection of Health Status Measurement Instruments checklist was employed. Specifically, we assessed measures for the following criteria: internal consistency, reliability, content validity, construct validity, and factor analysis.Citation11
Results
Statistics
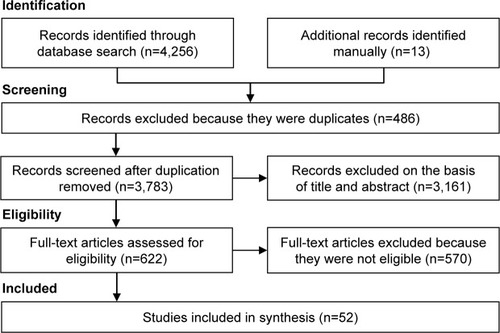
In all, 4,269 citations were identified. After removing duplicates (n=486), the remaining 3,783 citations were assessed, and an additional 3,161 irrelevant records were excluded. Of the remaining 622 papers, 570 articles were also removed because they were not eligible, and finally 52 full-text articles were included in the analysis (). Of these, 9 studies were qualitative and had focused upon the impact of PCOS on patients’ HRQoL.Citation12–Citation20 The remaining 43 studies were quantitative which are summarized in . The frequency of studies on QoL in PCOS women from various countries (n=52) was as follows: USA (n=13), UK (n=9), Iran (n=7), Australia (n=3), Germany (n=5), Sweden (n=2), Italy (n=2), Canada (n=2), the Netherlands (n=2), and Brazil (n=2). In addition, there was one article from each of the following countries: Belgium, Turkey, Austria, Taiwan, and Greece. displays and summarizes different components of QoL in PCOS women.
Table 1 Quantitative studies that measured HRQoL of women with PCOS (n=43)
Table 2 Different components of quality of life in PCOS women
Instruments used
Various general and specific questionnaires were used to assess QoL in PCOS women. Overall, three specific and 5 general measures were used to assess the QoL in PCOS women. Of these, one general instrument (36-Item Short Form Health Survey [SF-36]) and one specific instrument (Polycystic Ovary Syndrome Health-Related Quality of Life Questionnaire [PCOSQ]) were used most frequently (). The generic questionnaires were the following: the SF-36 (n=17), Symptom Checklist-90-Revised (SCL-90-R; n=5), World Health Organization Quality-of-Life-BREF (WHOQOL-BREF; n=4), Child Health Questionnaire-Child Form (CHQ-CF87; n=3), and General Health Questionnaire-28 (n=1). The PCOS disease-specific instruments were the PCOSQ (n=20), the Modified PCOSQ (MPCOSQ; n=3), and the Polycystic Ovary Syndrome Questionnaire (PCOSQ-50; n=1). In the following sections, a short description for each of these is presented.
Table 3 Most general and specific instruments for assessing HRQoL in women with PCOS
PCOSQ/MPCOSQ
The PCOSQ is an instrument that was specifically designed and validated to evaluate HRQoL in PCOS.Citation21–Citation23 In the first stage of the instrument development, 182 items were incorporated which belonged to 8 areas chosen as a result of running semi-structured interviews with 10 patients suffering from PCOS and an extensive literature review.Citation21 In item reduction phase, 100 women with PCOS completed the instrument, and they identified the items of highest impact on their daily lives. By considering the factors influencing women and identifying the items that clinicians take as important, a factor analysis was performed, and the final questionnaire containing 26 items was provided. The PCOSQ contains the following domains: emotions (8 items), hirsutism (5 items), weight (5 items), infertility (4 items), and menstrual disorders (4 items). Each item can be answered by choosing from a Likert scale with 7 options from 1 (always) to 7 (never). Higher scores are indicative of better function. Studies that incorporated the PCOSQ revealed that women with PCOS had functioning impairments pertinent to some measured domains.Citation24–Citation29 However, the relative degree of impairment caused by each domain varied in societies depending on the religious, racial, cultural, and social factors.Citation24 Excess body weight has been widely reported as an important concern to women with PCOS, especially in adolescents.Citation27,Citation30–Citation32 In two more studies that were carried out in Australia and Germany, body weight domain was found to have the strongest association with lower QoL.Citation33,Citation34 The psychometric properties of PCOSQ are well documented in several studies indicating that it is a reliable and valid measure for assessing QoL in PCOS women.Citation22,Citation23,Citation25,Citation35 However, the PCOSQ was modified by Barnard et al, and 4 questions were added to it in order to evaluate issues associated with acne.Citation33 Thus, the MPCOSQ includes 30 questions from 6 HRQoL domains: emotional disturbance (8 items), weight concerns (5 items), infertility (4 items), acne (4 items), menstrual symptoms and predictability (4 items), and hirsutism (5 items). Each item was rated on a 7-point Likert scale where higher scores represent better function. The psychometric properties of the MPCOSQ were promising.Citation33 Using this instrument, Bazarganipour et al in a cross-sectional study of 300 women with PCOS found that infertility and menstrual domains were the most affected areas of HRQoL.Citation36
PCOSQ-50
The PCOSQ-50 was specifically developed by Nasiri-Amiri et al for measuring QoL in PCOS women.Citation37 They used a mixed-method, sequential, exploratory design to define the components of health-related QoL questionnaire and assessed the psychometric properties of instrument. A rudimentary questionnaire composed of 147 items was designed drawing on the findings of a qualitative study that was carried out with 23 Iranian women who suffered from PCOS. Exploratory factor analysis helped to reduce the number of items from 147 to 50. The ultimate draft of the questionnaire incorporated 50 items representing 6 areas, namely emotion, obesity and menstrual disorders, fertility, sexual function, hirsutism, and coping. Each item could be answered by selecting from options on a 5-point Likert scale with higher scores meaning better condition. The analysis of the psychometric properties of the questionnaire revealed promising results.
SF-36
The SF-36 is one of the most acknowledged and most frequently used instruments to measure QoL. The SF-36 is used in all types of patients and has been validated in many countries. This instrument has been proved to be reliable and widely validated and has been employed in the assessment of HRQoL in various medical conditions. It consists of 36 items tapping into 8 subscales, namely physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional, and mental health.Citation38 The scores on each domain range from 0 to 100 where the higher scores indicate better conditions. Several studies used the SF-36 in order to assess HRQoL in PCOS patients.Citation30,Citation39–Citation42 Findings have been rather consistent in revealing lower HRQoL in women suffering from PCOS. However, evidence suggests that poor QoL in these women might be due to obesity. In some studies, it has been shown that body mass index (BMI) was a predictor of physical functioning as measured by the SF-36.Citation43,Citation44 Furthermore, by using a multivariable regression model, Panico et al in a recent study indicated that BMI is a predictor of physical functioning score.Citation44 Jones et al found that the role emotional was the poorest area of health, with mean scores of 50.4 on the SF-36 questionnaire, which had the greatest negative impact on HRQoL in women with PCOS.Citation23 In a study by Coffey et al, the psychological dimension was more affected than the physical dimension as measured by the SF-36.Citation25 Bazarganipour et al found that PCOS affected all domains in the SF-36, and psychological domains were most affected by PCOS.Citation45
SCL-90-R
The SCL-90 has also been widely used and extensively validated. It includes 90 items grouped into 10 main domains, namely somatization, obsessive–compulsive, interpersonal sensitivity, depression, anxiety, aggression, phobia, paranoid ideation, psychoticism, and sleep disorders.Citation46 Three global areas are measured, including the Global Severity Index, Positive Symptom Distress Index, and Positive Symptom Total. For each item related to a single domain, a score ranging from 0 (not at all) to 4 (very much) can be selected. Higher scores represent less favorable conditions.Citation44 Some studies targeting adult women suffering from PCOS have employed the SCL-90 to measure life quality.Citation30,Citation40,Citation44,Citation47,Citation48 By using this tool, Elsenbruch et al showed that emotional distress and obesity in PCOS women are associated with significant decrease in HRQoL.Citation40
WHOQOL-BREF
WHOQOL-BREF instrument is comprised of 26 items, which measure broad domains consisting of physical health, psychological health, social relationships, and environment. The WHOQOL-BREF is a shorter version of the original instrument and can be used for assessing the QoL in different cultures and populations. In a study on 146 women having PCOS and 170 controls who were assessed by the WHOQOL-BREF questionnaire, it was discovered that the hirsutism scores were a major predictor of psychological distress and showed correlation with the emotion domain.Citation49 In Benetti-Pinto et al’s study, the BMI was inversely correlated to the QoL in women suffering from PCOS, mainly with the physical, psychological, and environmental aspects of QoL.Citation50
CHQ-CF87
The CHQ-CF87 is a self-report questionnaire that was developed and validated at the Health Institute of the New England Medical Center in Boston.Citation51 It has been used to measure HRQoL in general populations of youth. It consists of 12 summated scales and is designed to measure both the physical and psychosocial HRQoL of adolescents. The items on the CHQ-CF87 are scored from 0 to 100 except for the change in health in the last year, and the items on family cohesion subscales are scored from 1 to 5 as single-item measures. A higher score on each subscale indicates better QoL in a specific area or health improvement in the last year.
Trent et al in their study used the CHQ-CF87 and revealed that HRQoL scores of adolescents suffering from PCOS were significantly lower in 4 areas of physical functioning, general health perceptions, behavior, and family activities as measured by the questionnaire.Citation52 These authors also carried out another study in this area and evaluated the influence of BMI on QoL disturbances in adolescent patients. PCOS adolescents had higher BMI than those of the controls and a significantly lower HRQoL. Similarly, PCOS girls scored lower on the general health perceptions, physical functioning, family activities, and the general behavior subscales of CHQ-CF87.Citation53
Discussion
The studies identified in this review have shown that PCOS is a major cause of psychological morbidity and has a negative impact on women’s HRQoL. This feature has also been demonstrated in some qualitative studies.Citation13,Citation14,Citation16,Citation19 In all the studies reviewed, different aspects of the QoL in PCOS women were evaluated including physical, psychological, social, sexual as well as medical ones.
The impact of PCOS on the HRQoL may be more specifically seen in the perception of values and culture;Citation24 therefore, the major contributing factors of reductions of life quality in PCOS were discovered to be different in a variety of population. However, physical aspects of QoL may be best predicted by obesity and hirsutism.Citation29,Citation49 Excess body weight has been widely reported as an important concern to women with PCOS, especially in adolescents.Citation27,Citation30–Citation32 Obesity is believed to be a primary source for poor HRQoL and contributes substantially to negative psychological symptoms in women with PCOS.Citation54 The findings of an Italian study that was recently performed yielded a significant aggravation of HRQoL in PCOS patients with obesity compared with controls.Citation44
Hirsutism can be found in nearly 70% of women suffering from PCOS,Citation2 and patients take it as one of the most annoying aspects of PCOS.Citation29,Citation55 Women suffering from PCOS who experience hirsutism have often complained that they feel “unfeminine.”Citation12,Citation30,Citation56,Citation57
The comparison of psychological well-beings between women suffering from PCOS and control groups showed an increased risk for emotional distress in those with PCOS.Citation6 Recent meta-analysis in PCOS women has yielded a raise in the prevalence of both depressive and anxiety symptoms in women suffering from PCOS in comparison with controls.Citation58 Loss of femininity, body image concerns, and coping with these conditions may all contribute to poorer mental health outcomes.Citation59
Moreover, changes in body dimensions and physical beauty as well as imbalance of sexual hormones could lead to reduction in QoL and sexual performance. Psychological distress from long-term health risks, infertility, and changes in appearance (obesity, acne, and hirsutism) can influence sexual function among PCOS women.Citation50,Citation60 These women often complain that they feel less attractive and being less sexually satisfied in comparison with non-PCOS women.Citation30
PCOS can also affect patients’ QoL socially. Based on the results of qualitative studies, other factors that affected QoL were the reduction of interpersonal and social relationships.Citation61,Citation62 Accordingly, Ekbäck et al in their qualitative study showed that hirsutism causes severe psychological burden and negatively affected patients’ HRQoL and social interactions.Citation14 A few studies explored the impact of treatment on HRQoL. In 2009, Rofey et al showed that an enhanced cognitive behavioral therapy was practical and encouraging for adolescents suffering from PCOS.Citation41
One of the major findings of the current research was the high frequency of application of specific and general instruments such as PCOSQ and SF-36. In our review, 24 studies had used specific tools for this purpose, and general questionnaires had been applied in other studies. PCOS affects women both psychologically and physically according to the SF-36. A recent meta-analysis showed that women with PCOS score lower in each dimension of the SF-36, mostly in the “Role Emotional” subscale.Citation7 General tools are designed to measure HRQoL in a wide range of diseases and therefore may not be sensitive enough to be used in specific conditions.Citation63 However, specific tools such as PCOSQ include some certain questions for these conditions. Obesity, hirsutism, irregular menses, and infertility are different aspects of PCOS exerting negative impacts on HRQoL that would not easily be detected by employing only a generic questionnaire. By using PCOSQ, it was demonstrated that clinical symptoms of PCOS, especially excess body weightCitation22,Citation23,Citation25–Citation27 and hirsutism,Citation29 could compromise women’s QoL. Ideally, employing both general and specific disease instruments in measuring HRQoL is recommended in order to make comparisons possible at a generic level and especially in the case of the disease under focus.Citation64
Conclusion
PCOS symptoms can result in remarkable worsening of life quality and may be highly stressful, adversely affecting psychological, social well-being and sexuality. This study revealed that the specific questionnaire PCOSQ and the SF-36 were mainly used for measuring life quality in women having PCOS. Perhaps using either a specific questionnaire solely or a specific questionnaire in conjunction with a generic measure would be more appropriate when measuring QoL in PCOS women. However, both questionnaires showed that they are able to capture different aspects of QoL in PCOS women and to identify areas that can help to improve QoL in these women.
Acknowledgments
We would like to thank the Tehran University’s vice-chancellor of education and vice-chancellor of research and technology for their financial support to carry out the study. This article is a part of the PhD thesis of Bita Feridoni supported by Tehran University of Medical Sciences (the ethics code: IR.TUMS.FNM.REC.1395.781).
Disclosure
The authors report no conflicts of interest in this work.
References
- SirmansSMPateKAEpidemiology, diagnosis, and management of polycystic ovary syndromeClin Epidemiol2013611324379699
- FauserBCTarlatzisBCRebarRWConsensus on women’s health aspects of polycystic ovary syndrome (PCOS): the Amsterdam ESHRE/ASRM-Sponsored 3rd PCOS Consensus Workshop GroupFertil Steril201297283822153789
- TeedeHDeeksAMoranLPolycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespanBMC Med201084120591140
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop GroupRevised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS)Hum Reprod200419414714688154
- MoranLJNormanRJTeedeHJMetabolic risk in PCOS: phenotype and adiposity impactTrends Endocrinol Metab20152613614325591984
- Veltman-VerhulstSMBoivinJEijkemansMJFauserBJEmotional distress is a common risk in women with polycystic ovary syndrome: a systematic review and meta-analysis of 28 studiesHum Reprod Update20121863865122824735
- LiYLiYYu NgEHPolycystic ovary syndrome is associated with negatively variable impacts on domains of health-related quality of life: evidence from a meta-analysisFertil Steril20119645245821703610
- ColwellHHMathiasSDPastaDJHenningJMSteegeJFA health-related quality-of-life instrument for symptomatic patients with endometriosis: a validation studyAm J Obstet Gynecol199817947559704764
- StracquadanioMCiottaLMetabolic Aspects of PCOS: Treatment with Insulin SensitizersSwitzerlandSpringer International Publishing2015
- LuckettTKingMButowPFriedlanderMParisTAssessing health-related quality of life in gynecologic oncology: a systematic review of questionnaires and their ability to detect clinically important differences and changeInt J Gynecol Cancer20102066468420442592
- TerweeCBBotSDde BoerMRQuality criteria were proposed for measurement properties of health status questionnairesJ Clin Epidemiol200760344217161752
- KitzingerCWillmottJ‘The thief of womanhood’: women’s experience of polycystic ovarian syndromeSoc Sci Med20025434936111824912
- SnyderBSThe lived experience of women diagnosed with polycystic ovary syndromeJ Obstet Gynecol Neonatal Nurs200635385392
- EkbäckMWijmaKBenzeinE“It is always on my mind”: women’s experiences of their bodies when living with hirsutismHealth Care Women Int20093035837219350434
- PercyCAGibbsTPotterLBoardmanSNurse-led peer support group: experiences of women with polycystic ovary syndromeJ Adv Nurs2009652046205519686401
- WeissTRBulmerSMYoung women’s experiences living with polycystic ovary syndromeJ Obstet Gynecol Neonatal Nurs201140709718
- JonesGLHallJMLashenHLBalenAHLedgerWLHealth-related quality of life among adolescents with polycystic ovary syndromeJ Obstet Gynecol Neonatal Nurs201140577588
- Nasiri AmiriFRamezani TehraniFSimbarMMohammadpour ThamtanRAShivaNFemale gender scheme is disturbed by polycystic ovary syndrome: a qualitative study from IranIran Red Crescent Med J201416e1242324719724
- TaghaviSABazarganipourFHugh-JonesSHosseiniNHealth-related quality of life in Iranian women with polycystic ovary syndrome: a qualitative studyBMC Womens Health20151511126620588
- WilliamsSSheffieldDKnibbRC‘Everything’s from the inside out with PCOS’: exploring women’s experiences of living with polycystic ovary syndrome and co-morbidities through Skype™ interviewsHealth Psychol Open20152 2055102915603051
- CroninLGuyattGGriffithLDevelopment of a health-related quality-of-life questionnaire (PCOSQ) for women with polycystic ovary syndrome (PCOS)J Clin Endocrinol Metab199883197619879626128
- GuyattGWeaverBCroninLDooleyJAAzzizRHealth-related quality of life in women with polycystic ovary syndrome, a self-administered questionnaire, was validatedJ Clin Epidemiol2004571279128715617954
- JonesGBenesKClarkTLThe Polycystic Ovary Syndrome Health-Related Quality of Life Questionnaire (PCOSQ): a validationHum Reprod20041937137714747184
- SchmidJKirchengastSVytiska-BinstorferEHuberJInfertility caused by PCOS – health-related quality of life among Austrian and Moslem immigrant women in AustriaHum Reprod2004192251225715333601
- CoffeySBanoGMasonHDHealth-related quality of life in women with polycystic ovary syndrome: a comparison with the general population using the Polycystic Ovary Syndrome Questionnaire (PCOSQ) and the Short Form-36 (SF-36)Gynecol Endocrinol200622808616603432
- ChingHLBurkeVStuckeyBGQuality of life and psychological morbidity in women with polycystic ovary syndrome: body mass index, age and the provision of patient information are significant modifiersClin Endocrinol (Oxf)20076637337917302871
- McCookJGReameNEThatcherSSHealth-related quality of life issues in women with polycystic ovary syndromeJ Obstet Gynecol Neonatal Nurs2005341220
- McCookJGBaileyBAWilliamsSLAnandSReameNEDifferential contributions of polycystic ovary syndrome (PCOS) manifestations to psychological symptomsJ Behav Health Serv Res20154238339424390359
- KhomamiMBTehraniFRHashemiSFarahmandMAziziFOf PCOS symptoms, hirsutism has the most significant impact on the quality of life of Iranian womenPLoS One201510e012360825874409
- ElsenbruchSHahnSKowalskyDQuality of life, psychosocial well-being, and sexual satisfaction in women with polycystic ovary syndromeJ Clin Endocrinol Metab2003885801580714671172
- KerchnerALesterWStuartSPDokrasARisk of depression and other mental health disorders in women with polycystic ovary syndrome: a longitudinal studyFertil Steril20099120721218249398
- KaczmarekCHallerDMYaronMHealth related quality of life in adolescents and young adults with polycystic ovary syndrome: a systematic reviewJ Pediatr Adolesc Gynecol20162955155727262833
- BarnardLFerridayDGuentherNStraussBBalenAHDyeLQuality of life and psychological well being in polycystic ovary syndromeHum Reprod2007222279228617537782
- ThomsonRLBuckleyJDLimSSLifestyle management improves quality of life and depression in overweight and obese women with polycystic ovary syndromeFertil Steril2010941812181620004371
- Malik-AslamAReaneyMDSpeightJThe suitability of polycystic ovary syndrome-specific questionnaires for measuring the impact of PCOS on quality of life in clinical trialsValue Health20101344044620230548
- BazarganipourFZiaeiSMontazeriAForoozanfardFKazemnejadAFaghihzadehSPredictive factors of health-related quality of life in patients with polycystic ovary syndrome: a structural equation modeling approachFertil Steril20131001389139623891270
- Nasiri-AmiriFRamezani TehraniFSimbarMMontazeriAMohammadpourRAHealth-related quality of life questionnaire for polycystic ovary syndrome (PCOSQ-50): development and psychometric propertiesQual Life Res2016251791180126814480
- ShielyJCBaylissMSKellerSDSF-36 Health Survey Annotated BibliographyBostonHealth Institute, New England Medical Center1996
- HahnSBensonSElsenbruchSMetformin treatment of polycystic ovary syndrome improves health-related quality-of-life, emotional distress and sexualityHum Reprod2006211925193416549423
- ElsenbruchSBensonSHahnSDeterminants of emotional distress in women with polycystic ovary syndromeHum Reprod2006211092109916459352
- RofeyDLSzigethyEMNollRBDahlRELobstEArslanianSACognitive–Behavioral therapy for physical and emotional disturbances in adolescents with polycystic ovary syndrome: a pilot studyJ Pediatr Psychol20093415616318556675
- ShishehgarFRamezani TehraniFMirmiranPHajianSBaghestaniARComparison of the association of excess weight on health related quality of life of women with polycystic ovary syndrome: an age- and BMI-matched case control studyPLoS One201611e016291127736861
- HahnSTanSElsenbruchSClinical and biochemical characterization of women with polycystic ovary syndrome in North Rhine-WestphaliaHorm Metab Res20053743844416034717
- PanicoAMessinaGLupoliGAQuality of life in overweight (obese) and normal-weight women with polycystic ovary syndromePatient Prefer Adherence20171142342928280314
- BazarganipourFZiaeiSMontazeriAForoozanfardFFaghihzadehSIranian version of modified polycystic ovary syndrome health-related quality of life questionnaire: discriminant and convergent validityIran J Reprod Med20131175376024639816
- DerogatisLRSCL-90-R: Administration, Scoring and Procedures Manual for the R (evised) Version and Other Instruments of the Psychopathology Rating Scale SeriesTowson, MDClinical Psychometric Research1992
- HahnSJanssenOETanSClinical and psychological correlates of quality-of-life in polycystic ovary syndromeEur J Endocrinol200515385386016322391
- TanSHahnSBensonSPsychological implications of infertility in women with polycystic ovary syndromeHum Reprod2008232064207118583330
- KumarapeliVSeneviratne RdeAWijeyaratneCNYapaRMDodampahalaSHA simple screening approach for assessing community prevalence and phenotype of polycystic ovary syndrome in a semi-urban population in Sri LankaAm J Epidemiol200816832132818550559
- Benetti-PintoCLFerreiraSRAntunesAJrYelaDAThe influence of body weight on sexual function and quality of life in women with polycystic ovary syndromeArch Gynecol Obstet201529145145525138126
- LandgrafJAbetzLWareJThe CHQ User’s ManualBostonThe Health Institute, New England Medical Center1996571
- TrentMERichMAustinSBGordonCMQuality of life in adolescent girls with polycystic ovary syndromeArch Pediatr Adolesc Med200215655656012038887
- TrentMAustinSBRichMGordonCMOverweight status of adolescent girls with polycystic ovary syndrome: body mass index as mediator of quality of lifeAmbul Pediatr2005510711115780012
- ChingHLBurkeVStuckeyBGQuality of life and psychological morbidity in women with polycystic ovary syndrome: body mass index, age and the provision of patient information are significant modifiersClin Endocrinol (Oxf)20076637337917302871
- KeeganALiaoLMBoyleM‘Hirsutism’: a psychological analysisJ Health Psychol2003832734514670212
- DrosdzolASkrzypulecVMazurBPawlińska-ChmaraRQuality of life and marital sexual satisfaction in women with polycystic ovary syndromeFolia Histochem Cytobiol200745S93S9718292843
- ThomasSAFanAWPastoreLMA review of the impact of body image on quality of life in women with polycystic ovary syndromeInt J Psychol Res2014917
- CooneyLGLeeISammelMDDokrasAHigh prevalence of moderate and severe depressive and anxiety symptoms in polycystic ovary syndrome: a systematic review and meta-analysisHum Reprod2017321075109128333286
- DeeksAAGibson-HelmMEPaulETeedeHJIs having polycystic ovary syndrome a predictor of poor psychological function including anxiety and depression?Hum Reprod2011261399140721436137
- DrosdzolASkrzypulecVMazurBPawlinska-ChmaraRQuality of life and marital sexual satisfaction in women with polycystic ovary syndromeFolia Histochem Cytobiol200745S93S9718292843
- Nasiri AmiriFRamezani TehraniFSimbarMMontazeriAMohammadpour ThamtanRAThe experience of women affected by polycystic ovary syndrome: a qualitative study from IranInt J Endocrinol Metab201412e1361224829583
- Podfigurna-StopaALuisiSReginiCMood disorders and quality of life in polycystic ovary syndromeGynecol Endocrinol20153143143426204044
- JenkinsonCAssessment and Evaluation of Health and Medical Care: A Methods TextUKOpen University Press1997
- JonesGLKennedySHJenkinsonCHealth-related quality of life measurement in women with common benign gynecologic conditions: a systematic reviewAm J Obstet Gynecol200218750151112193950
- WongECroninLGriffithLIrvineEJGuyattGHProblems of HRQL assessment: how much is too much?J Clin Epidemiol2001541081108511675158
- TrentMERichMAustinSBGordonCMFertility concerns and sexual behavior in adolescent girls with polycystic ovary syndrome: implications for quality of lifeJ Pediatr Adolesc Gynecol200316333712604144
- HashimotoDMSchmidJMartinsFMThe impact of the weight status on subjective symptomatology of the polycystic ovary syndrome: a cross-cultural comparison between Brazilian and Austrian womenAnthropol Anz20036129731014524003
- Van WelyMBayramNBossuytPMvan der VeenFLaparoscopic electrocautery of the ovaries versus recombinant FSH in clomiphene citrate-resistant polycystic ovary syndrome. Impact on women’s health-related quality of lifeHum Reprod2004192244225015242999
- ClaytonWJLiptonMElfordJRustinMSherrLA randomized controlled trial of laser treatment among hirsute women with polycystic ovary syndromeBr J Dermatol200515298699215888157
- LiptonMGSherrLElfordJRustinMHClaytonWJWomen living with facial hair: the psychological and behavioral burdenJ Psychosom Res20066116116816880018
- Harris-GlockerMDavidsonKKochmanLGuzickDHoegerKImprovement in quality-of-life questionnaire measures in obese adolescent females with polycystic ovary syndrome treated with lifestyle changes and oral contraceptives, with or without metforminFertil Steril2010931016101919781696
- LadsonGDodsonWCSweetSDEffects of metformin in adolescents with polycystic ovary syndrome undertaking lifestyle therapy: a pilot randomized double-blind studyFertil Steril20119525952598e1e621704212
- MoranLGibson-HelmMTeedeHDeeksAPolycystic ovary syndrome: a biopsychosocial understanding in young women to improve knowledge and treatment optionsJ Psychosom Obstet Gynecol2010312431
- LadsonGDodsonWCSweetSDThe effects of metformin with lifestyle therapy in polycystic ovary syndrome: a randomized double-blind studyFertil Steril20119510591066e1e721193187
- BazarganipourFZiaeiSMontazeriAForoozanfardFKazemnejadAFaghihzadehSPsychological investigation in patients with polycystic ovary syndromeHealth Qual Life Outcomes20131114123947827
- BazarganipourFZiaeiSMontazeriAForoozanfardFFaghihzadehSHealth-related quality of life and its relationship with clinical symptoms among Iranian patients with polycystic ovarian syndromeIran J Reprod Med20131137137824639768
- Stener-VictorinEHolmGJansonPOGustafsonDWaernMAcupuncture and physical exercise for affective symptoms and health-related quality of life in polycystic ovary syndrome: secondary analysis from a randomized controlled trialBMC Complement Altern Med20131313123763822
- BazarganipourFZiaeiSMontazeriAForoozanfardFKazemnejadAFaghihzadehSHealth-related quality of life in patients with polycystic ovary syndrome (PCOS): a model-based study of predictive factorsJ Sex Med2014111023103224308752
- De FrèneVVerhofstadtLLoeysTStuyverIBuysseADe SutterPSexual and relational satisfaction in couples where the woman has polycystic ovary syndrome: a dyadic analysisHum Reprod20153062563125534460
- GuidiJGambineriAZanottiLFanelliFFavaGAPasqualiRPsychological aspects of hyperandrogenic states in late adolescent and young womenClin Endocrinol201583872878
- StefanakiCBacopoulouFLivadasSImpact of a mindfulness stress management program on stress, anxiety, depression and quality of life in women with polycystic ovary syndrome: a randomized controlled trialStress201518576625287137
- Huang-TzOuHTChenPCWuMHLinCYMetformin improved health-related quality of life in ethnic Chinese women with polycystic ovary syndromeHealth Qual Life Outcomes20161411927553217
- DokrasASarwerDBAllisonKCWeight loss and lowering androgens predict improvements in health related quality of life in women with PCOSJ Clin Endocrinol Metab201610182966297427253669
- Ozcan DagZAlpuaMIsikYButurakSVTulmacOBTurkelYThe evaluation of temperament and quality of life in patients with polycystic ovary syndromeGynecol Endocrinol20173325025327908217
- JedelEWaernMGustafsonDAnxiety and depression symptoms in women with polycystic ovary syndrome compared with controls matched for body mass indexHum Reprod20102545045619933236
- MånssonMNorströmKHolteJLandin-WilhelmsenKDahlgrenELandénMSexuality and psychological wellbeing in women with polycystic ovary syndrome compared with healthy controlsEur J Obstet Gynecol Reprod Biol201115516116521232840
- Nasiri AmiriFRamezani TehraniFSimbarMMontazeriAMohammadpour ThamtanRAThe experience of women affected by polycystic ovary syndrome: a qualitative study from IranInt J Endocrinol Metab201412e1361224829583