Abstract
Placenta accreta is a condition of abnormal placental implantation in which the placental tissue invades beyond the decidua basalis. It may invade into or even through the myometrium and adjacent organs, such as the urinary bladder. The incidence has been rising in recent years. It is one of the important obstetric complications nowadays, leading to significant maternal morbidity and mortality. In the past, this condition was often diagnosed at the time of delivery when massive and unexpected hemorrhage occurred. Hysterectomy, associated with significant physical and psychological consequences, was usually the only management option. As more obstetricians have become aware of this condition, early identification with antenatal imaging diagnostic technology has become possible. Ultrasound scan plays an important role in the antenatal diagnosis. Various sonographic features with different specificity and sensitivity have been described in the literature. In equivocal cases, magnetic resonance imaging may be helpful. With such information, more accurate counseling can be offered to the mothers and their families before delivery. The delivery can also be arranged at a favorable time and in an institution where multidisciplinary support is available. Input from a hematologist, interventional radiologist, intensive care physician, urology surgeon, and/or other specialist are desirable. Apart from hysterectomy, various forms of conservative management can also be considered when the diagnosis is made prior to delivery. Fertility can therefore be preserved. After delivery, with or without hysterectomy performed, psychological support to the mothers and their families is essential.
Keywords:
Introduction
Morbidly adherent placenta represents a spectrum of disorders characterized by abnormal adherence or penetration of the placenta into the uterine wall. Histologically, it has been defined according to the degree of pathological penetration. Placenta accreta refers to a superficial attachment without invasion into the myometrium. Placenta increta occurs when placental villi extend into the myometrium. In placenta percreta, the invasions extend deep beyond the uterine serosa. From a clinicosurgical point of view, different degrees of invasion may coexist in the same patient. The three types of abnormal placentation and their management are often collectively described in the literature.Citation1,Citation2
The vast majority of women with placenta accreta have an identifiable risk factor.Citation3 Placenta previa and previous cesarean delivery are the major risk factors for placenta accreta. The risk increases with the number of previous cesarean sections.Citation4,Citation5 Myometrial trauma and scarring resulting from repeated dilatation and curettage, or other corrective surgeries also contribute to the risk of developing abnormal placental adherence. Advanced maternal age has also been identified as an independent risk factor. Others include smoking, grand multiparity, and recurrent miscarriages.Citation2,Citation6–Citation8
The incidence of placenta accreta has been escalating, from a reported occurrence of one in 30,000 deliveries in 1950 to one in 2500 deliveries (a tenfold increase) in 1997.Citation6,Citation9 This marked increase has been attributed to the increase in cesarean section rates worldwide.
Placenta accreta remains a leading cause of maternal hemorrhage and obstetric hysterectomy. Up to 38% of postpartum hysterectomies were found to be associated with placenta accreta in a review by the UK Obstetric Surveillance System.Citation10 Maternal morbidity and mortality are considerable. Related events and interventions include massive blood loss, dilutional or consumptive coagulopathy, blood transfusion, transfusion-related reaction or acute injury, postpartum hysterectomy, cystotomy, intensive care, and prolonged hospitalization. Not only is there concern for the high demands on health resources and expenditure, concern about litigation for an adverse obstetric outcome is inevitable.Citation8,Citation10–Citation13
A recent study has forecasted that a continued rise in Cesarean section rates could lead to substantial increase in incidence of placenta previa-accreta and maternal death.Citation14
Identification of risk factors, accurate antenatal and preoperative diagnosis, multidisciplinary management, and appropriate counseling will all aid in the overall management of women with placenta accreta and in reduction of maternal morbidity.
Ultrasonography
Ultrasonography remains a noninvasive, widely available and cost-effective modality of first-line diagnosis of placenta accreta in clinical practice.
Limitations to transabdominal ultrasound include the effect of maternal body habitus as well as its suboptimal visualization of the lower uterine cervix or area of placental invasion. The safety of transvaginal ultrasound in placenta previa has been accepted. It allows a closer view and more accurate examination of the lower uterine segment, leading to improved diagnostic accuracy in placenta previa-accreta.Citation15,Citation16
Since the 1980s, numerous ultrasound imaging techniques have been developed to assist in diagnosing morbidly adherent placenta antenatally. These include grayscale, color and/or three-dimensional power Doppler sonography. Various sonographic features and criteria for diagnosis have been suggested.
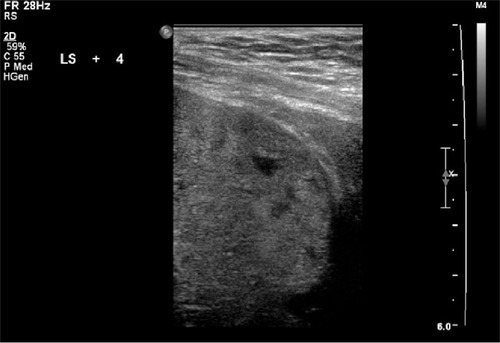
Retroplacental sonolucent zone
A normally occurring clear zone between the placenta and myometrium has been described.Citation17 This area is observed from 12 weeks and is believed to be associated with the dilated vessels of the decidua basalis. Deficiency and progressive loss of the decidua () has been proposed and confirmed histologically in placenta accreta.Citation18 Obliteration of this sonolucent zone between the placenta and myometrium was first observed in the 1980s and confirmed in subsequent studies.Citation19–Citation21 However, the sensitivity of this sign in isolation remains low. A false positive rate of up to 50% has been reported.Citation22
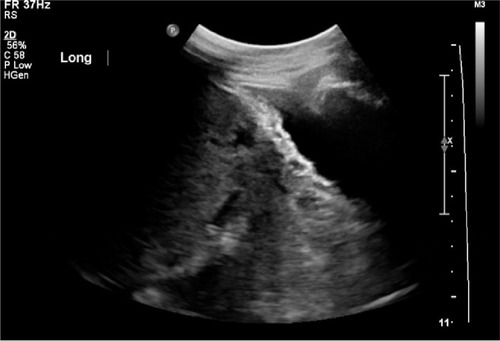
Vascular lacunae
Multiple venous structures occurring throughout the myometrium and placenta in accreta were first described by Kerr de Mendonça in 1988.Citation22 Subsequent observations of placental lakes were described as large and irregular (“Swiss cheese” appearance). These lacunae were not necessarily the areas of invasion. Presence of this sonographic sign has been reported to be associated with the highest positive predictive value for placenta accreta (). When identified in the second and third trimesters, the sensitivity of this sign is 79%, with a positive predictive value of 92%.Citation3,Citation15,Citation20,Citation23 The presence of lacunae was also found to be significantly associated with risks of disseminated intravascular coagulopathy, massive transfusions, and intensive care.Citation24
Figure 2 Vascular lacunae.
The presence of sonographic criteria is not pathognomonic and should be interpreted with caution in the clinical setting. Although found to be of high sensitivity and positive predictive value, the presence of placenta lacunae and lack of sonolucent zone have (not infrequently) been observed in placenta previa without morbid adherence of placenta.Citation25
Myometrial thinning
Progressive thinning of the retroplacental myometrium indicates the proximity of placental tissue to the peritoneal serosa or surrounding viscera, particularly the bladder. Segmental myometrial thinning of <1 mm is suggestive of an adherent placenta (). Combined with presence of large placental lacunae, the sensitivity of this sign reaches nearly 100% and specificity is 72%–79%, with a positive predictive value of 73%.Citation26,Citation27
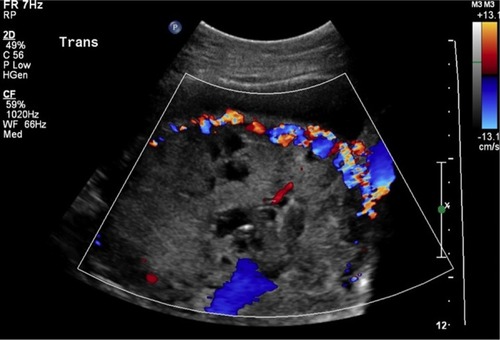
Interruption of bladder line
Lack of myometrial tissue could result in thinning or disruption of the vesicouterine interphase, which has been found to be associated with greater compromise (). In reality, distinguishing between irregularities of the bladder wall and placenta accreta may sometimes be difficult.Citation20,Citation21
Presence of exophytic masses
In extreme cases, the presence of extrauterine placental parenchyma can confirm the diagnosis of placenta percreta.
The use of ultrasound greyscale has been shown to be capable of diagnosing placenta accreta with sensitivity ranging from 87%–95%, specificity of 76%–98%, and a positive predictive value of 82%–93%.Citation2,Citation28 The predictive value of ultrasound in the diagnosis of placenta accreta in the first trimester remains unclear.Citation29 summarizes the sonographic features of placenta accreta reported by various authors.
Table 1 Summary of sonographic features of placenta accrete
Color Doppler imaging
Color and power Doppler provide a higher specificity in the diagnosis of placenta accreta and in particular, the depth of invasion. A pattern of turbulent blood flow extending from the placenta into the surrounding tissues has been reported in placenta accreta.Citation16 Other criteria include focal or diffuse intraparenchymal placental lacunar flow, vesicouterine serosa interphase hypervascularity, prominent retroplacental venous complex, and loss of retroplacental Doppler vascular signals.Citation30 The diagnostic sensitivity reached 82%, while positive predictive value was 87% in one study looking at use of Doppler.Citation31
Three-dimensional Doppler
Reported features include numerous coherent vessels involving the whole vesicouterine serosa interphase on basal view; and hypervascularity, inseparable cotyledonal and intervillous circulations, chaotic branching, and detour vessels on lateral views.Citation29,Citation32
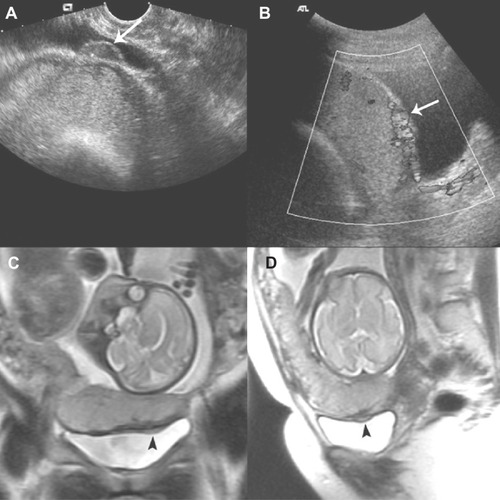
Magnetic resonance imaging (MRI)
Ultrasonography and MRI are comparable in diagnosing placenta accreta. The latter has additional value in detecting depth of placental invasion and depicting posterior placenta accreta. However, there is insufficient evidence to support routine MRI scanning of patients with sonographically suspected placenta accreta to improve management and outcome. MRI is often recommended when ultrasound findings are inconclusive.Citation29,Citation33–Citation36 MRI findings suggestive of placenta accrete include uterine bulging, heterogeneous signal intensity within the placenta, dark intraplacental bands on T2-weighted images, tenting of the bladder, and direct visualization of placental invasion into pelvic structures.Citation23 illustrates ultrasound examination with Doppler study showing a major anterior placenta previa accreta with bladder wall involvement. The MRI scan was also suggestive of deep myometrial invasion by placental tissue, but the bladder mucosa was intact.
Figure 5 Ultrasound examination with Doppler study showing a major anterior placenta previa accreta with bladder wall involvement.
Abbreviation: MRI, magnetic resonance imaging.
Obstetric management strategies
Antenatal
Anticipation and identification of risk factors is essential in developing safe management strategies. It has been recommended that women who had previous cesarean section should have placental localization to exclude placenta previa and further investigation to identify placenta accreta, if necessary.Citation37,Citation38
The management of morbidly adherent placenta is a real obstetric challenge and should be undertaken by a consultantled multidisciplinary team in a tertiary care institute. Delivery is ideally planned and arranged electively under controlled conditions with appropriate surgical and hematological facilities.
The presence of a consultant obstetrician and anesthesiologist at delivery, possible input from urology, gynecologic oncology, and vascular surgeons, blood products arrangement and prompt delivery, and access to intensive care constitute a care bundle in managing a patient with placenta accreta.Citation29,Citation32,Citation39
Optimal timing of a scheduled delivery depends on various clinical factors. Elective preterm delivery is often necessary because of pregnancy complications, like antepartum hemorrhage. The maternal benefits of earlier elective delivery must be balanced against the neonatal morbidity associated with premature birth. In the absence of antepartum hemorrhage or pregnancy complications, elective late-preterm delivery is acceptable to reduce the likelihood of emergency delivery at term.Citation13,Citation39
The adoption of conservative versus radical management is another important decision to be made in the planning process. Thorough preoperative counseling is crucial. The patient should be adequately counseled about the risks of catastrophic hemorrhage, blood transfusion, and visceral involvement. Possible interventions such as hysterectomy, ureteric stenting and cystotomy, or conservative measures (including leaving the placenta in situ, use of cell salvage, and interventional radiology) should also be discussed.
A preoperative checklist would be helpful in confirming necessary preparations and for identifying contact persons in case perioperative assistance is required.
Intrapartum
Anesthetic considerations include large-bore intravenous access, rapid replacement of fluid and blood, hemodynamic monitoring facilities, prevention of hypothermia, and thromboembolic prophylaxis.Citation29,Citation40
Dorsal lithotomy positioning with hip abduction but limited flexion can enable direct evaluation of intraoperative vaginal bleeding, and allow uterine balloon placement if needed.
Immediate preoperative ultrasound mapping of the placental location aids in determining the optimal approach to the abdominal wall and uterine incisions. It is recommended that uterine incision be made away from the placenta during entry to the uterine cavity. Incision through the placenta and attempt to deliver the placenta often result in significant hemorrhage. illustrates a thin and very vascular uterine lower segment at the time of cesarean section. The rich vascularity usually correlates with the position of placentation. Attempt to remove the placenta leads to disruption of the infiltrated bed and is associated with increased maternal morbidity. It has been suggested that it may be sensible to complete the delivery of the infant and proceed to an intended hysterectomy with the placenta left in situ.Citation13,Citation29,Citation38,Citation41,Citation42 A total rather than subtotal hysterectomy is advocated because of the risk of hemorrhage from lower-segment invasions. For the same reason, internal iliac artery ligation is associated with significant risk of failure in managing postpartum hemorrhage in placenta accreta because of the collateral arterial supplies. In cases where subtotal hysterectomy is performed, peritoneal closure over the cervical stump should be avoided as further hemorrhage may be concealed and unnoticed.Citation3
Figure 6 Thin and very vascular uterine lower segment at the time of cesarean section.

Interventional radiology does play an important role in offering prophylactic measures to reduce uterine flow and prevent ongoing hemorrhage. Preoperative placement of a catheter in the internal iliac or uterine arteries, with or without balloon inflation at the time of delivery, or embolization after cesarean section can be performed.Citation39,Citation43 Higher failure of embolization in placenta accreta was observed when compared with its use for postpartum hemorrhage due to other causes, like uterine atony or retained products of gestation. A recent systematic review of uterus-preserving treatment modalitiesCitation1 revealed that uterine artery embolization for placenta accreta could achieve a subsequent menstruation rate of 62% and pregnancy rate of 15%, and secondary hysterectomy rate of 18%. Most of the studies involved small numbers and we are still awaiting results from further larger prospective series.Citation44,Citation45
In selected groups of women, conservative management can be considered. The criteria for such an approach include the possibility of preoperative consultation, hemodynamic stability without significant blood loss, a wish to preserve fertility, and the availability of resources and expertise to follow up and manage late postpartum complications.Citation45 Conservative management aims to avoid hysterectomy by leaving the placenta in situ with or without additional measures, including arterial embolization, application of compression sutures, and segmental resection of the myometrial tissues followed by repair of the defect or uterine reconstruction. Lack of comparative studies on the different surgical techniques has resulted in wide variation in the approach adopted. Use of tissue sealants or even mesh has been reported, but to date, there is insufficient evidence on their effectiveness and safety.Citation45–Citation47
In a systematic review,Citation1 expectant management in patients with invasive placentation is associated with a 67% rate of achieving subsequent pregnancy and a 19% rate of secondary hysterectomy at the same time.
Postpartum
Patients with placental accreta and especially those requiring hysterectomy for postpartum hemorrhage are at risk for complications in relation to intrapartum hypotension and persistent coagulopathy. Collaboration with intensive care physicians and the monitoring of vital signs and organ functions postoperatively is of paramount importance. Should there be hemodynamic instability or suspicion of hemoperitoneum, computed tomography (CT) or MRI should be undertaken and followed by exploratory laparotomy without delay. Persistent hematuria or anuria should alert clinicians of possible unrecognized urinary tract injury. Transient or permanent Sheehan syndrome is a known complication of massive postpartum hemorrhage. Hyponatremia may be an early sign for this.Citation29
Secondary infection, sepsis, postpartum hemorrhage, and disseminated intravascular coagulopathy are the major clinical concerns after leaving the placenta in situ. Close surveillance and ready access to medical assessment and resuscitation are the key prerequisites to conservative management. Prophylactic broad-spectrum antibiotics and uterotonic agents are often recommended, although a consensual guideline has yet to be established. Whether the placenta should be removed in the postpartum period or left to resorb or be expelled spontaneously remains controversial. Serum human chorionic gonadotropin and Doppler ultrasound may be utilized to assess the cessation of placental vascularity for consideration of interval removal, but the clinical correlation remains undetermined.Citation48
Methotrexate has been proposed as a conservative measure for retained placenta with morbid adherence. Methotrexate, being a folate antagonist, is not without side effects and is contraindicated in breastfeeding. It is effective against proliferating trophoblasts, but its action on degenerative placenta after delivery remains questionable and diverse in different series. In general, outcomes do not differ significantly with or without use of methotrexate.Citation49,Citation50
Adequate support and assessment of psychological well-being of the patient after major obstetric events are sometimes overlooked but indispensable. Debriefing sessions should be carried out with the patient and family at appropriate intervals. Adequate explanation and effective communication helps to reduce the risk of medical litigation.
Conclusion
Placenta accreta has been evolving into a more common complication in modern obstetrics. The rising incidence is partly caused by our changing obstetric practice in terms of cesarean delivery rate, and it is one of the consequences we have to encounter from now onwards. The identification of high-risk group mothers, based on history, during the antenatal period is important and facilitates the diagnosis of this condition by imaging techniques, mainly ultrasonography. Various sonographic features have been reported and a combination of these features may sharpen the accuracy of the diagnosis. The diagnostic value of magnetic resonance imaging for placenta accreta remains controversial. When the antenatal diagnosis of placenta accreta has been made, the mothers should be under care of a consultant obstetrician-led team throughout and receive informative counseling prior to delivery. Elective cesarean delivery should be arranged in an institution with multidisciplinary support. Conservative management can be considered mainly for mothers with the wish to preserve fertility, although delayed hysterectomy in the postnatal period is still a possibility. For mothers with a completed family, a lower threshold for hysterectomy may be desirable. Close monitoring after the operation, preferably in an intensive care unit or high dependency unit, is of paramount importance. Psychological support to the mothers, especially those who had a hysterectomy performed, and their families is essential.
Disclosure
All authors hereby declare that there is no conflict of interest related to the work for this paper.
References
- Steins BisschopCNSchaapTPVogelvangTEScholtenPCInvasive placentation and uterus preserving treatment modalities: a systematic reviewArch Gynecol Obstet2011284249150221638046
- Palacios-JaraquemadaJMDiagnosis and management of placenta accretaBest Pract Res Clin Obstet Gynaecol20082261133114818815074
- DoumouchtsisSKArulkumaranSThe morbidly adherent placenta: an overview of management optionsActa Obstet Gynecol Scand20108991126113320804337
- ClarkSLKooningsPPPhelanJPPlacenta previa/accreta and prior cesarean sectionObstet Gynecol198566189924011075
- ToWWLeungWCPlacenta previa and previous cesarean sectionInt J Gynaecol Obstet199551125318582514
- MillerDACholletJAGoodwinTMClinical risk factors for placenta previa-placenta accretaAm J Obstet Gynecol199717712102149240608
- EsakoffTFSparksTNKaimalAJDiagnosis and morbidity of placenta accretaUltrasound Obstet Gynecol201137332432720812377
- GielchinskyYRojanskyNFasouliotisSJEzraYPlacenta accreta – summary of 10 years: a survey of 310 casesPlacenta2002232–321021411945088
- ReadJACottonDBMillerFCPlacenta accreta: changing clinical aspects and outcomeObstet Gynecol198056131346966777
- KnightMUKOSSPeripartum hysterectomy in the UK: management and outcomes of the associated haemorrhageBJOG2007114111380138717877772
- WilkinsonHTrustees and Medical AdvisorsSaving mothers’ lives. Reviewing maternal deaths to make motherhood safer: 2006–2008BJOG20111181114021403 discussion 3–4.21906238
- HullADMooreTRMultiple repeat cesareans and the threat of placenta accreta: incidence, diagnosis, managementClin Perinatol201138228529621645796
- EllerAGPorterTFSoissonPSilverRMOptimal management strategies for placenta accretaBJOG2009116564865419191778
- SolheimKNEsakoffTFLittleSEChengYWSparksTNCaugheyABThe effect of cesarean delivery rates on the future incidence of placenta previa, placenta accreta, and maternal mortalityJ Matern Fetal Neonatal Med201124111341134621381881
- OyeleseYSmulianJCPlacenta previa, placenta accreta, and vasa previaObstet Gynecol2006107492794116582134
- LernerJPDeaneSTimor-TritschIECharacterization of placenta accreta using transvaginal sonography and color Doppler imagingUltrasound Obstet Gynecol1995531982017788495
- CallenPWFillyRAThe placental-subplacental complex: a specific indicator of placental position on ultrasoundJ Clin Ultrasound19808121266766472
- Hoffman-TretinJCKoenigsbergMRabinAAnyaegbunamAPlacenta accreta. Additional sonographic observationsJ Ultrasound Med199211129341740829
- PastoMEKurtzABRifkinMDCole-BeugletCWapnerRJGoldbergBBUltrasonographic findings in placenta incretaJ Ultrasound Med1983241551596854719
- ComstockCHLoveJJJrBronsteenRASonographic detection of placenta accreta in the second and third trimesters of pregnancyAm J Obstet Gynecol200419041135114015118654
- FinbergHJWilliamsJWPlacenta accreta: prospective sonographic diagnosis in patients with placenta previa and prior cesarean sectionJ Ultrasound Med19921173333431522623
- Kerr de MendonçaLSonographic diagnosis of placenta accreta. Presentation of six casesJ Ultrasound Med1988742112153285025
- BaughmanWCCortevilleJEShahRRPlacenta accreta: spectrum of US and MR imaging findingsRadiographics20082871905191619001647
- YangJILimYKKimHSChangKHLeeJPRyuHSSonographic findings of placental lacunae and the prediction of adherent placenta in women with placenta previa totalis and prior Cesarean sectionUltrasound Obstet Gynecol200628217818216858740
- HamadaSHasegawaJNakamuraMUltrasonographic findings of placenta lacunae and a lack of a clear zone in cases with placenta previa and normal placentaPrenat Diagn201131111062106521800335
- HudonLBelfortMABroomeDRDiagnosis and management of placenta percreta: a reviewObstet Gynecol Surv19985385095179702791
- TwicklerDMLucasMJBalisABColor flow mapping for myometrial invasion in women with a prior cesarean deliveryJ Matern Fetal Med20009633033511243289
- ShihJCPalacios JaraquemadaJMSuYNRole of three-dimensional power Doppler in the antenatal diagnosis of placenta accreta: comparison with gray-scale and color Doppler techniquesUltrasound Obstet Gynecol200933219320319173239
- Publications CommitteeSociety for Maternal-Fetal MedicineBelfortMAPlacenta accretaAm J Obstet Gynecol2010203543043921055510
- AllahdinSVoigtSHtweTTManagement of placenta praevia and accretaJ Obstet Gynaecol20113111621280984
- ChouMMHoESLeeYHPrenatal diagnosis of placenta previa accreta by transabdominal color Doppler ultrasoundUltrasound Obstet Gynecol2000151283510776009
- rcog.org.uk [homepage on the Internet]. Placenta praevia, placenta praevia accreta and vasa praevia: diagnosis and management. London: Royal College of Obstetricians and Gynaecologists.Green-top Guideline No 27; 2011 [updated May 1, 2011]. Available from: http://www.rcog.org.uk/womens-health/clinical-guidance/placenta-praevia-and-placenta-praevia-accreta-diagnosis-and-manageme. Accessed September 28, 2012.
- MasselliGBrunelliRCascianiEMagnetic resonance imaging in the evaluation of placental adhesive disorders: correlation with color Doppler ultrasoundEur Radiol20081861292129918239921
- DwyerBKBelogolovkinVTranLPrenatal diagnosis of placenta accreta: sonography or magnetic resonance imaging?J Ultrasound Med20082791275128118716136
- LevineDHulkaCALudmirJLiWEdelmanRRPlacenta accreta: evaluation with color Doppler US, power Doppler US, and MR imagingRadiology199720537737769393534
- WarshakCREskanderRHullADAccuracy of ultrasonography and magnetic resonance imaging in the diagnosis of placenta accretaObstet Gynecol20061083 Pt 157358116946217
- LewisGSaving Mothers’ Lives: Reviewing Maternal Deaths to Make Motherhood Safer – 2003–2005. The Seventh Report of the Confidential Enquiries into Maternal Deaths in the United KingdomLondonConfidential Enquiry into Maternal and Child Health (CEMACH)2007
- ACOG Committee on Obstetric PracticeACOG Committee opinion. Number 266, January 2002: placenta accretaObstet Gynecol200299116917011777527
- HullADResnikRPlacenta accreta and postpartum hemorrhageClin Obstet Gynecol201053122823620142659
- SnegovskikhDCleboneANorwitzEAnesthetic management of patients with placenta accreta and resuscitation strategies for associated massive hemorrhageCurr Opin Anaesthesiol201124327428121494133
- YapYYPerrinLCPainSRWongSFChanFYManual removal of suspected placenta accreta at cesarean hysterectomyInt J Gynaecol Obstet2008100218618717900586
- HayesEAyidaGCrockerAThe morbidly adherent placenta: diagnosis and management optionsCurr Opin Obstet Gynecol201123644845322002113
- OphirESinger-JordanJOdehMAbnormal placental invasion – a novel approach to treatment case report and reviewObstet Gynecol Surv2009641281182219939295
- rcog.org.uk [hompage on the Internet]. The role of emergency and elective interventional radiology in postpartum haemorrhage. London: Royal College of Obstetricians and Gynaecologists. Good Practice No 6; 2007 [updated June 1, 2007]. Available from: http://www.rcog.org.uk/womens-health/clinical-guidance/role-emergency-and-elective-interventional-radiology-postpartum-haem. Accessed September 28, 2012.
- WelshAWEllwoodDCarterJPedutoAJVedelagoJBennettMOpinion: integration of diagnostic and management perspectives for placenta accretaAust N Z J Obstet Gynaecol200949657858720070704
- WohlmuthCTDela MercedJGelatin-thrombin hemostatic matrix in the management of placental site postpartum hemorrhage: a case reportJ Reprod Med2011565–627127321682125
- Palacios-JaraquemadaJMFiorilloAvon PeteryFColaciDLeguizamónGUterine repair and successful pregnancy after myometrial and placental rupture with massive haemoperitoneumBJOG2009116345646019187380
- MatsumuraNInoueTFukuokaMSagawaNFujiiSChanges in the serum levels of human chorionic gonadotropin and the pulsatility index of uterine arteries during conservative management of retained adherent placentaJ Obstet Gynaecol Res2000262818710870298
- ArulkumaranSNgCSIngemarssonIRatnamSSMedical treatment of placenta accreta with methotrexateActa Obstet Gynecol Scand19866532852863739639
- MussalliGMShahJBerckDJElimianATejaniNManningFAPlacenta accreta and methotrexate therapy: three case reportsJ Perinatol200020533133410920795