Abstract
Combined oral contraceptives formulated to include estradiol (E2) have recently become available for the indication of pregnancy prevention. A combined estradiol valerate and dienogest pill (E2V/DNG), designed to be administered using an estrogen step-down and a progestin step-up regimen over 26 days of active treatment followed by 2 days of placebo (26/2-day regimen), has also undergone research to assess the potential for additional noncontraceptive benefits. Randomized, placebo-controlled studies have demonstrated that E2V/DNG is an effective treatment for heavy menstrual bleeding – a reduction in median menstrual blood loss approaching 90% occurs after 6 months of treatment. To date, E2V/DNG is the only oral contraceptive approved for this indication. Comparator studies have also demonstrated a reduction in hormone withdrawal-associated symptoms in users of E2V/DNG compared with a conventional 21/7-day regimen of ethinylestradiol/levonorgestrel. Other potential noncontraceptive benefits associated with E2V/DNG, like improvement in dysmenorrhea, sexual function, and quality of life, are comparable with those associated with other combined oral contraceptives and are discussed further in this review.
Introduction
Over the last 50 years, combined oral contraceptives (COCs) have become a widely accepted form of birth control. They have also undergone considerable evolution in the dose and type of estrogen, the type of progestins, and the variety of regimens used, as well as the inclusion of other pharmaceuticals that could be beneficial to menstruating women (eg, folic acid and iron). These developments have been driven, in part, to improve tolerability, meet women’s requirements, and provide additional benefits. Although the described noncontraceptive health benefits of COCs are numerous,Citation1 only a few noncontraceptive indications have been specifically approved by regulatory authorities for some formulations; these include: the treatment of acne and/or hirsutism as well as other signs of androgenization in women, such as androgenetic alopecia, with ethinyl estradiol (EE)/drospirenone (YAZ®; Bayer HealthCare Pharmaceuticals, Berlin, Germany), EE/cyproterone acetate (Dianette/Diane-35; Bayer Schering Pharma AG, Berlin, Germany), EE/norgestimate (Ortho Tri-Cyclen®; Janssen Pharmaceuticals Inc., Titusville, NJ, USA), and EE/norethindrone acetate with ferrous fumarate (Estrostep Fe®; Warner Chilcott Company, LLC, Rockaway, NJ, USA);Citation2–Citation6 treatment of premenstrual dysphoric disorder (PMDD) with EE/drospirenone (YAZ®);Citation2 and the treatment of heavy menstrual bleeding (HMB) with estradiol valerate (E2V)/dienogest (DNG) (Qlaira®/Natazia®; Bayer HealthCare Pharmaceuticals).Citation7 Epidemiologic studies have also demonstrated that COCs reduce the risk of endometrial, ovarian, and colon cancersCitation8,Citation9 and all cause mortality.Citation10
Previous attempts to improve the tolerability of COCs, by replacing EE with 17-beta-estradiol (E2), resulted in poor cycle control, particularly when E2 was administered as part of a monophasic or a biphasic regimen.Citation11,Citation12 A novel 26/2-day dynamic-dose regimen (26 days of hormone, followed by a 2-day hormone-free interval [HFI]) of E2V/DNG (Qlaira®/Natazia®), administered using an estrogen step-down and progestin step-up approach, has been developed to provide efficient ovulation inhibition, high contraceptive efficacy, and good cycle control, with an acceptable tolerability profile.Citation11 E2V/DNG has been approved for contraceptive use in Europe and North America,Citation11,Citation13,Citation14 and more recently, approved for the treatment of HMB, based on the results of two multicenter trials conducted in Europe/Australia and North America.Citation15,Citation16
Since its introduction, E2V/DNG has been assessed in a number of studies designed to better define its noncontraceptive benefits. This paper reviews the noncontraceptive therapeutic benefits associated with the use of E2V/DNG.
Methods
A PubMed literature search for original research articles published between January 1, 2000 and May 7, 2014, using the terms “estradiol valerate” and “dienogest”, “Qlaira”, and “E2V/DNG”, yielded 206 unique citations. From the initial electronic search, 16 original research articles reporting the E2V/DNG oral contraceptive were identified based on abstract/title information and retrieved;Citation11,Citation13,Citation15–Citation28 the full articles were assessed, and eight articles that reported noncontraceptive benefits of E2V/DNG (loosely defined as any perceived benefit beyond safety and contraceptive efficacy, or related surrogate outcomes) were identified for inclusion.Citation13,Citation15–Citation18,Citation22,Citation24,Citation28 Of the other publications, one was a pooled study summarizing menstrual blood loss (MBL) data across two individual studies previously identified, and was included as appropriate.Citation23 The other seven articles reported on outcomes that were not the focus of this review but were included, where appropriate, as supportive references.Citation11,Citation19–Citation21,Citation25–Citation27 Ten other pertinent articles were identified from published manuscripts known to the authors or from unpublished manuscripts that were available to them and were included for discussion,Citation14,Citation29–Citation37 but three others were not included as the outcomes reported were not the focus of this review.Citation38–Citation40 Thus, 19 articles that reported some noncontraceptive benefits of E2V/DNG formed the main bulk of this narrative review.
Noncontraceptive benefits of E2V/DNG
Bleeding profile
The drive to develop E2-based oral contraceptives has, in part, been due to an interest in reducing the serious adverse effects related to the hepatic and hemostatic changes associated with EE. However, early attempts at producing E2-based oral contraceptives have been limited by poor cycle stability, attributed to the rapid metabolism of E2 to the weaker estrogen, estrone, which is unable to maintain stable endometrial proliferation. Moreover, the rate of E2 metabolism may be influenced by the progestin, and as such, those progestins with minimal impact on E2 metabolism and endometrial stroma stability would be expected to improve cycle stability. DNG is a 19-norprogestin derivative with high specificity for the progesterone receptor, antiandrogenic properties, and minimal impact on lipid and carbohydrate metabolism. It has no glucocorticoid, antimineralocorticoid, or antiestrogenic activity.Citation41 In addition, DNG has potent antiproliferative effects on the endometrium, as well as anti-inflammatory and antiangiogenic properties.Citation42
The E2V/DNG 26/2 cycle consists of E2V 3 mg on days 1–2, E2V 2 mg/DNG 2 mg on days 3–7, E2V 2 mg/DNG 3 mg on days 8–24, E2V 1 mg on days 25–26, and placebo on days 27–28.Citation11 This regimen has been shown to effectively inhibit ovulation and provide extraovarian contraceptive effects (such as reducing endometrial thickness and cervical mucus production).Citation11,Citation20 The phased delivery of hormones was designed to provide estrogen dominance at the start of the cycle and progestin dominance during the mid and later part of the cycle. The early estrogenic dominance allows for initial endometrial proliferation, thereby enhancing sensitivity to progestin action at midcycle and endometrial stroma stability.Citation28 Endometrial stroma stability ensures a predictable bleeding profile with E2V/DNG. Administration of E2 only at the end of the cycle, along with a short (2 day) HFI, results in E2 levels that remain relatively stable throughout the cycle.Citation27
E2V/DNG is an established contraceptive with a reduced-bleed profile.Citation16,Citation28,Citation35 In a seven-cycle, multicenter, double-blind, double-dummy, randomized, controlled trial (RCT) in healthy women aged 18–50 years, E2V/DNG was shown to achieve shorter and lighter bleeding and resulted in a higher proportion of women without withdrawal bleeding compared with the monophasic combination of EE 20 μg/levonorgestrel (LNG) 100 μg administered in a 21/7-day regimen (21 days of hormone, followed by a 7-day HFI) (the proportion who experienced withdrawal bleeding per cycle through cycles 1–7 was 77.7%–83.2% with E2V/DNG and 89.5%–93.8% with EE/LNG [P<0.0001 per cycle]).Citation28 For some women, however, this might be considered a disadvantage as withdrawal bleeding may reassure them that they are not pregnant. Although these data suggested that E2V/DNG may reduce MBL to a greater extent than EE/LNG, the study also showed that the incidence of intracyclic bleeding, adverse events, and satisfaction with therapy associated with the two COCs were similar.Citation28
Dysmenorrhea
COCs are widely used for the management of primary dysmenorrhea as the condition has long been shown to respond favorably to ovulation inhibition.Citation43 In addition, COCs suppress endometrial growth, thereby reducing the proliferation of endometrial tissue. In an RCT comparing E2V/DNG and EE/LNG in 507 women with primary dysmenorrhea over three cycles of treatment, both COCs alleviated dysmenorrhea and decreased the number of days with dysmenorrheic pain, compared with baseline, to a similar amount (−4.6±4.6 days and −4.2±4.2 days for the E2V/DNG and EE/LNG groups, respectively) (P=0.34).Citation29
Heavy menstrual bleeding
E2V/DNG is currently the only COC indicated for the treatment of HMB (defined as blood loss of at least 80 mL per menstrual cycleCitation44). Approval was based on two rigorous, identically designed, double-blind, placebo-controlled RCTsCitation15,Citation16 in women with heavy and/or prolonged menstrual bleeding without organic pathology (ie, HMB due to endometrial dysfunction, using International Federation of Gynecology and Obstetrics [FIGO] terminologyCitation45). Menstrual bleeding was recorded daily in electronic diaries throughout the study, and MBL was estimated from sanitary protection used by the women, using a modified version of the alkaline hematin method.Citation46 The primary efficacy end point across both studies (as requested by the USA Food and Drug Administration) was based on a previously unused composite of eight stringent criteria for “complete response” (ie, a return to “menstrual normality”) during a 90-day efficacy period, defined as the complete resolution of qualifying abnormal menstrual symptoms, including a reduction in MBL to below 80 mL and ≥50% reduction in MBL, in women with HMB ().
Table 1 Primary efficacy outcomesTable Footnote* used in two identically designed, double-blind, placebo-controlled, randomized controlled studies with estradiol valerate/dienogest, in women with heavy and/or prolonged menstrual bleeding without organic pathology
In the first of these RCTs carried out in Europe and Australia,Citation15 231 otherwise healthy women with confirmed heavy, prolonged or frequent menstrual bleeding were randomized (2:1) to seven cycles of E2V/DNG or placebo. The proportion of women with a return to “menstrual normality” was significantly higher with E2V/DNG versus placebo (29.5% vs 1.2%) (P<0.0001). In the second RCT, carried out in 128 women in the United States and Canada,Citation16 the findings were similar (29.2% E2V/DNG vs 2.9% placebo) (P<0.001).
In a pooled analysis of data from these two RCTs, median MBL across both studies was found to have decreased by 88% with E2V/DNG compared with 24% with placebo, after 6 months of treatment. The onset of action of E2V/DNG was shown to be rapid, with the largest reductions in MBL achieved as early as the first withdrawal bleed after E2V/DNG initiation and maintained with no loss of effect (and even some further gradual improvement) with continued treatment.Citation36
The data from the two RCTs were reanalyzed in another pooled analysis, using the definition of treatment success that was previously employed in another RCT comparing the efficacy and safety of the levonorgestrel-releasing intrauterine system with that of oral medroxyprogesterone acetate in women with HMB.Citation47 Using these criteria, the proportions of patients successfully treated (ie, reduction in MBL to <80 mL and a ≥50% reduction compared with baseline) with seven cycles of E2V/DNG and placebo, respectively, were 63.6% and 11.9% (P<0.001).Citation23
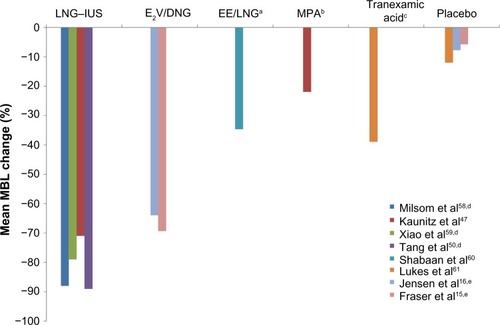
There are currently no head-to-head trials comparing E2V/DNG with other COCs or other medical treatment options in the management of HMB, and as such, only indirect comparisons can be made. Commonly used medical therapies for HMB include the levonorgestrel-releasing intrauterine system, tranexamic acid, EE-based COCs, oral progestins, and nonsteroidal anti-inflammatory drugs (NSAIDs). allows an indirect comparison of the reduction in MBL achieved with E2V/DNG relative to the other various medical therapies, in women with HMB without organic pathology. The reduction from baseline in MBL achieved with E2V/DNG (median 88% reduction after 6 months)Citation36 appears to approach that achieved with the levonorgestrel-releasing intrauterine system (median 91%–95% after 6 months) and appears superior to other oral treatments.Citation47–Citation50 However, the main limitations of such interstudy comparison include patient heterogeneity and deviations in the alkaline hematin method, which requires consistent use of validated sanitary materials, and as such, may mask variations in efficacy between studies.
Figure 1 Bleeding reduction after 6 months of treatment with selected medical therapies, measured using the alkaline hematin method (data from randomized control trial unless otherwise stated).Citation15,Citation16,Citation47,Citation50,Citation58–Citation61
Abbreviations: DNG, dienogest; E2V, estradiol valerate; EE, ethinyl estradiol; LNG–IUS, levonorgestrel-releasing intrauterine system; LNG, levonorgestrel; MBL, menstrual blood loss; MPA, medroxyprogesterone acetate; TID, three times daily.
Quality of life (QoL) implications of HMB treatment
While QoL was not directly assessed in the two RCTs assessing E2V/DNG in the treatment of HMB, the effect of treatment on HMB-related impairment of work productivity and activities of daily living has been assessed.Citation18,Citation32 These assessments showed that the benefits of E2V/DNG in reducing MBL could be translated into a consistent positive impact on work productivity and activities of daily living. Moreover, these improvements resulted in savings of US$22–62 and US$18–56 per month, associated with better work productivity and improvements in activities of daily living, respectively, in the study conducted in Europe and Australia.Citation32 In the US and Canadian study, improvements in work productivity and activities of daily living with E2V/DNG resulted in monthly saving of US$80.2 and Can$70.8, and US$84.9 and Can$73.5, respectively, in the two countries.Citation18
Hormone-associated withdrawal symptoms
Some users of conventional COCs with cyclical 21/7-day regimens experienced bothersome symptoms during the HFI.Citation51 These are generally believed to be the result of estrogen withdrawal/fluctuation during the HFI and can include headaches and pelvic pain, nausea or vomiting, bloating, and breast tenderness.Citation51,Citation52 Consequently, it is hypothesized that eliminating or reducing the HFI should reduce the frequency and/or severity of these hormone withdrawal-associated symptoms.Citation53
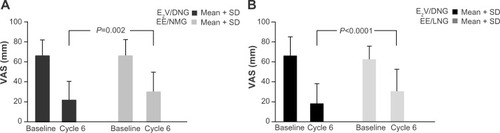
The effect of the 26/2-day dynamic-dosing E2V/DNG regimen in reducing the severity of hormone withdrawal-associated symptoms in women prone to these symptoms was evaluated in two Phase III RCTs using 21/7-day regimen COC comparators.Citation17,Citation31 The Phase III, multicenter, double-blind HARMONY I and II RCTs showed that E2V/DNG provided significantly greater reductions in the frequency and intensity of headache and pelvic pain during the HFI than did 21/7-day regimens with triphasic EE/norgestimate or EE/LNG, in otherwise healthy women aged 18–50 years ().Citation17,Citation31 The use of rescue medication was also significantly reduced with E2V/DNG compared with the triphasic EE/norgestimate or EE/LNG COCs. These studies suggest that E2V/DNG may be a good option for women who experience hormone withdrawal-associated symptoms with traditional 21/7-day regimen COCs. The 26/2-day dynamic dosing regimen of E2V/DNG, with its shortened HFI, has been shown to provide stable levels of E2 throughout the 28-day cycle, including during the HFI, which may, in part, explain its benefit with respect to these symptoms.Citation27
Figure 2 Change from baseline to cycle 6 in the average of the three highest VAS values on cycle days 22–28, for the hormone withdrawal-associated symptoms of headache or pelvic pain, in women who received treatment with E2V/DNG compared with (A) triphasic EE/NGM and (B) EE/LNG.
Abbreviations: DNG, dienogest; E2V, estradiol valerate; EE, ethinyl estradiol; LNG, levonorgestrel; NGM, norgestimate; SD, standard deviation; VAS, visual analog scale.
Other COCs taken in regimens that eliminate (ie, continuous use) or reduce the HFI (eg, 24/4-day regimens) have reported improvements in hormone withdrawal-associated symptoms.Citation53 There are currently no head-to-head data comparing the effect of E2V/DNG with these regimens.
Menstrual-related migraine
E2V/DNG has been shown to have a positive effect in women with menstrual-related migraine. A prospective pilot study in 32 women with menstrual-related migraine showed that six cycles of E2V/DNG significantly reduced the number of migraine attacks and the amount of analgesic used versus baseline.Citation33 In addition, in those with concomitant dysmenorrhea at baseline, complete remission of menstrual cramps was reported by 59% (17/29) and 61% (17/28) of these women at cycles 3 and 6, respectively. Persistence of dysmenorrhea was shown to be a potential feature associated with refractory head pain in a subgroup of women with dysmenorrhea. However, the open label, noncomparator nature of this study makes it impossible to draw robust conclusions as the study provides no reference for the observed changes.Citation33
It must be kept in mind that a cautious approach regarding any COC use is recommended for women with a history of headache. A clear diagnostic distinction between common headache and migraine, either with or without aura is needed, especially as both the American College of Obstetricians and Gynecologists and the World Health Organization list migraine with aura as an absolute contraindication to the use of COCs, due to the increased risk of stroke.Citation54,Citation55 In the absence of aura, other individual risk factors should be taken into account. Women who develop new onset migraine or a worsening of migraine symptoms while using COCs should discontinue use.Citation56
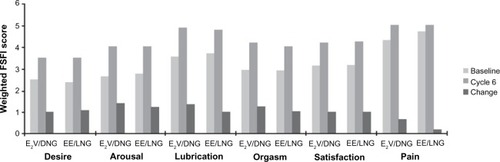
Sexual function and QoL
Oral contraceptives are not thought to improve sexual function, aside from the reduction in concern for risk of pregnancy. However, oral contraceptives containing progestins with antiandrogenic activity, such as DNG, may theoretically be associated with decreased libido,Citation57 and it is common for women with associated sexual dysfunction to be switched to oral contraceptives containing progestins with androgenic activity, such as LNG.Citation34 A preliminary study in 57 sexually active, healthy women showed that E2V/DNG improved QoL and had a positive effect on sexuality over six cycles of use;Citation24 however, this study was open label, and without a comparator. More recently, a multicenter, double-blind, noninferiority RCT compared the effects of six cycles of E2V/DNG with EE/LNG on sexual function, in 276 women with COC-associated sexual dysfunction.Citation34 Similar improvements in all domains of the Female Sexual Function Index (FSFI) were demonstrated with E2V/DNG and EE/LNG recipients, with no significant between-group differences (). The mean increase (improvement) in the sum of the FSFI Desire and Arousal component scores from baseline to cycle 6 were 5.90±5.45 for E2V/DNG and 5.79±6.17 for EE/LNG (both P<0.0001), and all other efficacy parameters were also equally improved with the two COCs. Overall, these results suggest that E2V/DNG does not have a detrimental effect on sexual function.
Figure 3 Scores of the Female Sexual Function Index subdomains, for E2V/DNG and EE/LNG, at baseline and cycle 6, and the change from baseline.
Abbreviations: DNG, dienogest; E2V, estradiol valerate; EE, ethinyl estradiol; FSFI, Female Sexual Function Index, LNG, levonorgestrel.
Other benefits
There is evidence to suggest that E2V/DNG may have a positive influence on acne and hyperandrogenism.Citation30 In a small 1-year preliminary observational study in 36 young women with polycystic ovary syndrome (PCOS) and mild or moderate acne, 12 cycles of E2V/DNG provided a significant improvement of acne in 53% of patients (P<0.01) and a significant increase in sex hormone-binding globulin levels at 6 and 12 months (P<0.001).Citation30 However, larger, longer-term RCTs that include a comparator are needed to confirm whether E2V/DNG offers any advantage over other COC formulations, for the treatment of acne. E2V/DNG has also been assessed as a strategy for endometrial preparation prior to operative hysteroscopy, with two small randomized studies supporting that pretreatment with E2V/DNG improved the subjective ease of the procedure.Citation22,Citation37 Again, larger RCTs are needed to confirm whether E2V/DNG pretreatment offers any advantage over other COC formulations with regard to operative hysteroscopy procedures.
Conclusion
E2V/DNG is an established contraceptive with a reduced-bleed profile and is currently the only COC approved for treatment of HMB. It may be a good alternative for women susceptible to hormone withdrawal-associated symptoms with COCs taken in the conventional 21/7-day regimen. Whether the reduction in hormone withdrawal-associated symptoms is due to the components of the formulation, the dosing regimen, or both, remains to be fully established. The available evidence does not suggest that E2V/DNG has a detrimental impact on sexual function compared with LNG combination pills.
Acknowledgments
Medical writing support during development of this manuscript was provided by Mary Hines and Richard Glover of inScience Communications, Springer Healthcare. This assistance was funded by Bayer HealthCare Pharmaceuticals.
Disclosure
During the past 2 years, Dr Nappi had financial relationship (lecturer, member of advisory boards, and/or consultant) with Bayer HealthCare Pharmaceuticals, Ely Lilly, Gedeon-Richter, HRA Pharma, Merck Sharpe and Dohme, Novo Nordisk, Pfizer Inc., Shionogi Limited, and TEVA/Theramex. Dr Serrani is an employee of Bayer HealthCare Pharmaceuticals. Dr Jensen has received payments for consulting, from Agile Pharmaceuticals, Abbvie Pharmaceuticals, Bayer HealthCare Pharmaceuticals, ContraMed, Evofem Inc., HRA Pharma, Merck Pharmaceuticals, Teva Pharmaceuticals, and the Population Council; and for lectures, from Bayer and Merck; he has also received research funding from Abbvie, Bayer HealthCare Pharmaceuticals, the Population Council, the National Institutes of Health, and the Bill and Melinda Gates Foundation. These companies and organizations may have a commercial or financial interest in the results of this research and technology. The authors report no other conflicts of interest.
References
- SchindlerAENon-contraceptive benefits of oral hormonal contraceptivesInt J Endocrinol Metab2013111414723853619
- YAZ® (drospirenone/ethinyl estradiol) tablets for oral use [prescribing information]Monteville, NJBayer HealthCare Pharmaceuticals, Inc2012
- Dianette® [summary of product characteristics]BerlinBayer Pharma AG2013
- Ortho Tri-Cyclen® tablets (norgestimate/ethinyl estradiol) tablets [prescribing information]Titusville, NJJanssen Pharmaceuticals, Inc2013
- ESTROSTEP® Fe (norethindrone acetate and ethinyl estradiol tablets, USP and ferrous fumarate tablets) tablets [prescribing information]Rockaway, NJWarner Chilcott Company LLC2009
- BayerScheringPharmaAGDiane-35Berlin-WeddingBayer Schering Pharma AG2010 Available from: http://www.pharmaline.co.il/images/newsletterregistration/bayer/11022011/dianedr.pdfAccessed March 20, 2014
- NATAZIA® (estradiol valerate and estradiol valerate/dienogest) tablets, for oral use [prescribing information]Monteville, NJBayer Health Care Pharmaceuticals, Inc2013
- VeljkovićMVeljkovićSThe risk of breast cervical, endometrial and ovarian cancer in oral contraceptive usersMed Pregl2010639–10657661 Serbian21446095
- DossusLAllenNKaaksRReproductive risk factors and endometrial cancer: the European Prospective Investigation into Cancer and NutritionInt J Cancer2010127244245119924816
- VesseyMYeatesDFlynnSFactors affecting mortality in a large cohort study with special reference to oral contraceptive useContraception201082322122920705149
- EndrikatJParkeSTrummerDSchmidtWDuijkersIKlippingCOvulation inhibition with four variations of a four-phasic estradiol valerate/dienogest combined oral contraceptive: results of two prospective, randomized, open-label studiesContraception200878321822518692612
- ÅgrenUMAnttilaMMäenpää-LiukkoKEffects of a monophasic combined oral contraceptive containing nomegestrol acetate and 17β-oestradiol in comparison to one containing levonorgestrel and ethinylestradiol on markers of endocrine functionEur J Contracept Reprod Health Care201116645846721942708
- PalaciosSWildtLParkeSMachlittARömerTBitzerJEfficacy and safety of a novel oral contraceptive based on oestradiol (oestradiol valerate/dienogest): a Phase III trialEur J Obstet Gynecol Reprod Biol20101491576219969409
- NelsonAParkeSMellingerUZampaglioneESchmidtAEfficacy and safety of a combined oral contraceptive containing estradiol valerate/dienogest: results from a clinical study conducted in North AmericaJ Womens Health (Larchmt)201423320421024279594
- FraserISRömerTParkeSEffective treatment of heavy and/or prolonged menstrual bleeding with an oral contraceptive containing estradiol valerate and dienogest: a randomized, double-blind Phase III trialHum Reprod201126102698270821784734
- JensenJTParkeSMellingerUMachlittAFraserISEffective treatment of heavy menstrual bleeding with estradiol valerate and dienogest: a randomized controlled trialObstet Gynecol2011117477778721422847
- JensenJTParkeSMellingerUSerraniMMabeyRGHormone withdrawal-associated symptoms: comparison of oestradiol valerate/dienogest versus ethinylestradiol/norgestimateEur J Contracept Reprod Health Care201318427428323638631
- WasiakRFilonenkoAVannessDJImpact of estradiol valerate/dienogest on work productivity and activities of daily living in women with heavy menstrual bleedingJ Womens Health (Larchmt)201322437838423586801
- RapsMRosendaalFBallieuxBResistance to APC and SHBG levels during use of a four-phasic oral contraceptive containing dienogest and estradiol valerate: a randomized controlled trialJ Thromb Haemost201311585586123410231
- EndrikatJParkeSTrummerDSerraniMDuijkersIKlippingCPituitary, ovarian and additional contraceptive effects of an estradiol-based combined oral contraceptive: results of a randomized, open-label studyContraception201387222723422995539
- BlodeHZeunSParkeSEvaluation of the effects of rifampicin, ketoconazole and erythromycin on the steady-state pharmacokinetics of the components of a novel oral contraceptive containing estradiol valerate and dienogest in healthy postmenopausal womenContraception201286433734422445438
- CicinelliEPintoVQuattrominiPEndometrial preparation with estradiol plus dienogest (Qlaira) for office hysteroscopic polypectomy: randomized pilot studyJ Minim Invasive Gynecol201219335635922322156
- FraserISJensenJSchaefersMMellingerUParkeSSerraniMNormalization of blood loss in women with heavy menstrual bleeding treated with an oral contraceptive containing estradiol valerate/dienogestContraception20128629610122240178
- CarusoSAgnelloCRomanoMPreliminary study on the effect of four-phasic estradiol valerate and dienogest (E2V/DNG) oral contraceptive on the quality of sexual lifeJ Sex Med20118102841285021810188
- JungeWMellingerUParkeSSerraniMMetabolic and haemostatic effects of estradiol valerate/dienogest, a novel oral contraceptive: a randomized, open-label, single-centre studyClin Drug Investig2011318573584
- KlippingCDuijkersIParkeSMellingerUSerraniMJungeWHemostatic effects of a novel estradiol-based oral contraceptive: an open-label, randomized, crossover study of estradiol valerate/dienogest versus ethinylestradiol/levonorgestrelDrugs R D201111215917021679006
- ZeunSLuMUddinAZeilerBMorrisonDBlodeHPharmacokinetics of an oral contraceptive containing oestradiol valerate and dienogestEur J Contracept Reprod Health Care200914322123219565420
- AhrendtHJMakalováDParkeSMellingerUMansourDBleeding pattern and cycle control with an estradiol-based oral contraceptive: a seven-cycle, randomized comparative trial of estradiol valerate/dienogest and ethinyl estradiol/levonorgestrelContraception200980543644419835717
- PetragliaFParkeSSerraniMMellingerURömerTEstradiol valerate plus dienogest versus ethinylestradiol plus levonorgestrel for the treatment of primary dysmenorrheaInt J Gynaecol Obstet2014125327027424713413
- Di CarloCGarganoVSpariceSTommaselliGABifulcoGNappiCEffects of an oral contraceptive containing estradiol valerate and dienogest on circulating androgen levels and acne in young patients with PCOS: an observational preliminary studyGynecol Endocrinol201329121048105024020909
- MacìasGMerki-FeldGSParkeSMellingerUSerraniMEffects of a combined oral contraceptive containing oestradiol valerate/dienogest on hormone withdrawal-associated symptoms: results from the multicentre, randomised, double-blind, active-controlled HARMONY II studyJ Obstet Gynaecol201333659159623919857
- WasiakRFilonenkoAVannessDJImpact of estradiol-valerate/dienogest on work productivity and activities of daily living in European and Australian women with heavy menstrual bleedingInt J Womens Health2012427127822927764
- NappiRETerrenoESancesGEffect of a contraceptive pill containing estradiol valerate and dienogest (E2V/DNG) in women with menstrually-related migraine (MRM)Contraception201388336937523453784
- DavisSRBitzerJGiraldiAChange to either a nonandrogenic or androgenic progestin-containing oral contraceptive preparation is associated with improved sexual function in women with oral contraceptive-associated sexual dysfunctionJ Sex Med201310123069307924034466
- NelsonAParkeSMakalovaDSerraniMPalaciosSMellingerUEfficacy and bleeding profile of a combined oral contraceptive containing oestradiol valerate/dienogest: a pooled analysis of three studies conducted in North America and EuropeEur J Contracept Reprod Health Care201318426427323651474
- FraserISParkeSMellingerUMachlittASerraniMJensenJEffective treatment of heavy and/or prolonged menstrual bleeding without organic cause: pooled analysis of two multinational, randomised, double-blind, placebo-controlled trials of oestradiol valerate and dienogestEur J Contracept Reprod Health Care201116425826921774563
- BifulcoGDi Spiezio SardoADe RosaNThe use of an oral contraceptive containing estradiol valerate and dienogest before office operative hysteroscopy: a feasibility studyGynecol Endocrinol2012281294995522571602
- De LeoVFruzzettiFMusacchioMCScolaroVDi SabatinoAMorganteGEffect of a new oral contraceptive with estradiol valerate/dienogest on carbohydrate metabolismContraception201388336436823769016
- BitzerJParkeSRoemerTSerraniMEndometrial safety of an oral contraceptive containing estradiol valerate and dienogestInt J Womens Health2011312713221573149
- Di CarloCGarganoVSpariceSShort-term effects of an oral contraceptive containing oestradiol valerate and dienogest on bone metabolism and bone mineral density: an observational, preliminary studyEur J Contracept Reprod Health Care201318538839323859010
- MueckAOSeegerHBühlingKJWhy use of dienogest for the first contraceptive pill with estradiol?Gynecol Endocrinol201026210911319672744
- MueckAODinogest: an oral progestogen for the treatment of endometriosisExpert Rev Obstet Gynecol201161515
- LefebvreGPinsonneaultOAntaoVSOGCPrimary dysmenorrhea consensus guidelineJ Obstet Gynaecol Can200527121117114616524531
- HallbergLHögdahlAMNilssonLRyboGMenstrual blood loss – a population study. Variation at different ages and attempts to define normalityActa Obstet Gynecol Scand19664533203515922481
- MunroMGCritchleyHOBroderMSFraserISFIGO Working Group on Menstrual DisordersFIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive ageInt J Gynaecol Obstet2011113131321345435
- HallbergLNilssonLDetermination of menstrual blood lossScand J Clin Lab Invest19641624424814161862
- KaunitzAMBissonnetteFMonteiroILukkari-LaxEMuysersCJensenJTLevonorgestrel-releasing intrauterine system or medroxyprogesterone for heavy menstrual bleeding: a randomized controlled trialObstet Gynecol2010116362563220733445
- AnderssonJKRyboGLevonorgestrel-releasing intrauterine device in the treatment of menorrhagiaBr J Obstet Gynaecol19909786906942119218
- ReidPCVirtanen-KariSRandomised comparative trial of the levonorgestrel intrauterine system and mefenamic acid for the treatment of idiopathic menorrhagia: a multiple analysis using total menstrual fluid loss, menstrual blood loss and pictorial blood loss assessment chartsBJOG200511281121112516045528
- TangGWLoSSLevonorgestrel intrauterine device in the treatment of menorrhagia in Chinese women: efficacy versus acceptabilityContraception19955142312357796588
- SulakPJScowRDPreeceCRiggsMWKuehlTJHormone withdrawal symptoms in oral contraceptive usersObstet Gynecol200095226126610674591
- SulakPWillisSKuehlTCoffeeAClarkJHeadaches and oral contraceptives: impact of eliminating the standard 7-day placebo intervalHeadache2007471273717355491
- BitzerJHormone withdrawal-associated symptoms: overlooked and under-exploredGynecol Endocrinol201329653053523421366
- World Health OrganizationMedical Eligibility Criteria for Contraceptive Use4th edGenevaWorld Health Organization2010 Available from: http://whqlibdoc.who.int/publications/2010/9789241563888_eng.pdfAccessed January 22, 2014
- Centers for Disease Control and PreventionUS medical eligibility criteria for contraceptive use 2010MMWR201059186
- EdlowAGBartzDHormonal contraceptive options for women with headache: a review of the evidenceRev Obstet Gynecol201032556520842283
- Sitruk-WareRNew progestagens for contraceptive useHum Reprod Update200612216917816291771
- MilsomIAnderssonKAnderschBRyboGA comparison of flurbiprofen, tranexamic acid, and a levonorgestrel-releasing intrauterine contraceptive device in the treatment of idiopathic menorrhagiaAm J Obstet Gynecol199116438798831900665
- XiaoBWuSCChongJZengTHanLHLuukkainenTTherapeutic effects of the levonorgestrel-releasing intrauterine system in the treatment of idiopathic menorrhagiaFertil Steril200379496396912749438
- ShaabanMMShabaanMMZakherahMSEl-NasharSASayedGHLevonorgestrel-releasing intrauterine system compared to low dose combined oral contraceptive pills for idiopathic menorrhagia: a randomized clinical trialContraception2011831485421134503
- LukesASMooreKAMuseKNTranexamic acid treatment for heavy menstrual bleeding: a randomized controlled trialObstet Gynecol2010116486587520859150
- Center for Drug Evaluation and ResearchApplication number: 22-252, Original 1 Statistical Review(s)http://www.accessdata.fda.gov/drugsatfda_docs/nda/2010/022252_Orig-1_StatR.pdfU.S. Department of Health and Human Services, Food and Drug Administration2010Accessed July 7, 2014

