Abstract
Background
The reported prevalence of pain after stroke varies considerably, depending on how pain is measured, time after stroke, and characteristics of the selected population. The aims of this study were to investigate the prevalence and distribution of new-onset pain initially and three months after stroke in a general Norwegian cohort, and to examine whether symptoms of anxiety or depression were associated with new-onset pain after stroke.
Material and methods
Stroke patients were included from eleven different hospitals within 14 days after stroke onset. Pain was assessed at inclusion and three months after stroke, and the distribution of pain was marked on a body map. New-onset pain was defined as pain reported by the patients to have occurred after the stroke. Symptoms of anxiety and depression were evaluated using the Hospital Anxiety and Depression Scale.
Results
A total of 390 patients were included. Pain data were available in 142 patients at both inclusion and follow-up, while 245 patients had available data for the regression analysis. In patients with follow-up data, new-onset pain occurred in 14 (9.9%) patients at inclusion and in 31 (21.8%) patients three months later, P=0.005. New-onset pain in the affected upper limb and bilaterally in the lower limbs was more common at three months than initially after stroke. Symptoms of anxiety were associated with new-onset pain (OR=1.13, 95% CI 1.01–1.27, P=0.030).
Conclusion
This study shows that new-onset pain occurs in one out of ten patients initially after stroke and in one out of five patients three months after stroke, and it was associated with symptoms of anxiety. This raises the question of whether easing symptoms of anxiety might help to prevent or treat new pain after stroke.
Introduction
The reported prevalence of pain after stroke varies considerably, and range from 11% to 54%, depending on how pain is measured, time after stroke, and selection and characteristics of the population.Citation1–Citation3 Despite some inconsistencies, several studies have found that pain in stroke patients is associated with female gender, younger age, and more severe strokes.Citation4–Citation6
As pain is always subjective, the most obvious way of having it assessed is by structured interviews.Citation3,Citation7,Citation8 Structured questionnaires exist,Citation9 and different scales such as Numeric Rating Scale (NRS), Visual Analog Scale, and Verbal Rating Scale make it possible to describe pain with some accuracy.Citation10
The number of patients experiencing pain seems to increase during follow-up, at least within the first months after stroke.Citation2,Citation3 Previous research also indicates different patterns for different kinds of post-stroke pain.Citation3,Citation5,Citation11 While headache mainly develops as an acute problem declining with time, pain related to the muscular skeletal system seems to increase gradually and over time.Citation3
The nature of post-stroke pain is intricate, and it is difficult to grasp all aspects involved in its development and its influence on the lives of the affected patients. Even though pain does not seem to affect functional outcome three months after stroke,Citation12 the affected patients appear to have an increased risk of experiencing emotional distress.Citation4,Citation7,Citation13 Studies have found an association between pain and depression in stroke patients, but there are some inconsistencies indicating that this relationship is complex and not properly accounted for.Citation4,Citation7,Citation14,Citation15
The association between anxiety disorders and pain is established in several populations, indicating a bidirectional relationship between the two.Citation16–Citation19 Although anxiety is fairly common in stroke patients,Citation20 little is known about how it influences the occurrence of pain after stroke. One study has found that anxiety was more common in patients with pain than no pain. However, pain was not specified as new after the stroke, and the analyses were not adjusted for confounders.Citation21
Pain is also common in the general population.Citation22 It is therefore difficult to evaluate whether the pain existed prior to or occurred after the stroke, and even more difficult to establish whether the pain was caused by the stroke. Previous research has focused on the total burden of post-stroke pain,Citation2,Citation4 and even though some studies differentiate between pre-stroke and post-stroke pain, few studies follow the same group of patients over time to see how new pain evolves after the stroke. In the current study, we used data from a Norwegian multicenter study (the LEAST study)Citation23 to investigate the occurrence of pain initially and three months after stroke. We also wanted to distinguish between pre-stroke and post-stroke pain.
The primary aim of this study was to report the prevalence and distribution of new-onset pain in the early phase and three months after stroke in a group of stroke patients. Secondary aims were to examine whether symptoms of anxiety and depression were associated with new-onset pain after stroke and to describe how patients reported the pain to influence on activities of daily living and enjoyment of life.
Material and methods
Study design and setting
This was a prospective observational study recruiting stroke patients admitted to stroke units in 11 Norwegian hospitals. The participating hospitals were two university hospitals, seven middle-sized hospitals (treating 100–400 stroke patients per year), and two small hospitals (treating less than 100 patients per year). Hospitals were contacted once every fortnight, and inclusion was carried out if there were two or more eligible patients. Trained assessors performed the follow-up assessment three months later, mainly by telephone or face-to-face.Citation23
Participants
Patients were recruited from December 2011 to June 2013. Patients were eligible if they had been diagnosed with acute stroke according to the WHO’s definitionCitation24 within the last 14 days, were aged more than 18 years, not receiving palliative care, were able to understand the Norwegian language, and willing to sign informed consent. They had to stay in the hospital for the whole process of inclusion. Patients unable to consent for themselves were included if their next of kin consented to their inclusion. The study was approved by the Regional Committee for Medical and Health Research Ethics in Norway (REK no 2011/1428).
Baseline assessment
Baseline characteristics including gender and age were recorded immediate after inclusion. Stroke was classified as infarction or hemorrhage. Stroke severity was measured using the National Institutes of Health Stroke Scale (NIHSS) at inclusion.Citation25 Premorbid and post-stroke functional level was registered using the modified Rankin Scale (mRS).Citation26
Measures
Pain was assessed at three months after stroke, with a later protocol adjustment and implementation of pain assessment at inclusion to the study as well. At inclusion, patients were asked if they had any pain. Pain was defined according to the definition used in the Brief Pain Inventory, that is, ignoring pain that most of us have from time to time, such as minor headache, sprains, and toothache. Furthermore, patients were asked to locate the pain on the body map from the same questionnaire.Citation9 To decide if the pain was new after the stroke, patients were asked if it had occurred after the stroke.
Additionally to these pain questions, an extended questionnaire was implemented at three months after the stroke. Patients were asked if the pain required regular (>2 times per week) use of analgesics. NRS (0–10) was used to rate pain intensity. Patients with new-onset pain were asked to rate on the NRS how the pain influenced their daily activities and enjoyment of life. A score of 3 or less on NRS was categorized as “mild”, a score from 4 to 7 as “moderate”, and a score of more than 7 as “severe”.Citation27
Symptoms of anxiety and depression were measured at three months after stroke using the Hospital Anxiety and Depression Scale (HADS),Citation28 which has been validated for use in stroke patients.Citation29 It consists of seven questions related to depression and seven questions related to anxiety, and it generates a score for each of the two subscales (0–21) as well as a total score (0–42). It is recommended that the sub-scales are used separately.Citation30 Dichotomization of the score is possible,Citation31 but in this study, we used the total score for both subscales, symptoms of depression and anxiety.
Statistics
Baseline data were analyzed using the Pearson chi-squared test for dichotomous proportions, while the Mann–Whitney U test and Student’s t-test were used to compare groups on scale variables. Descriptive statistics were used to report the prevalence and distribution of new pain according to the body map. Distribution of pain on the body map was defined according to the following categories: head/neck, upper limb on the affected or unaffected side of the body, lower limb on the affected or unaffected side of the body, back, chest, and abdomen. The McNemar mid-P-test was used to analyze differences in new-onset pain in the acute phase and after three months.
Univariable logistic regression, with new-onset pain three months after stroke as the dependent variable, was used to analyze associations. Independent variables were gender, age, stroke severity assessed with the NIHSS, symptoms of anxiety, and symptoms of depression three months after stroke. A multivariable logistic regression analysis was performed with symptoms of anxiety and depression as independent variables. Adjustments for gender, age, and NIHSS were made as these variables are known to be associated with pain after stroke.Citation5,Citation6 This regression analysis was repeated three times, once with both “anxiety” and “depression” included in the model, once with “anxiety” alone and once with “depression” alone included in the model, in addition to gender, age, and NIHSS. A two-sided P-value <0.05 was considered significant. Statistical analyses were performed in SPSS 24 and Microsoft Excel 2016.
Results
Study population
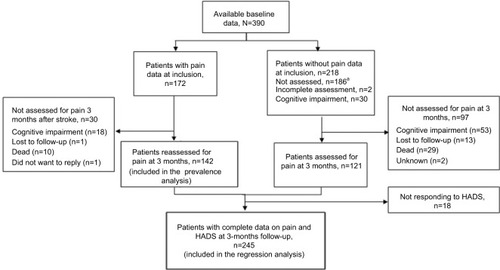
A total of 547 patients were screened for inclusion from December 2011 to June 2013. Fifty-one patients did not meet the inclusion criteria, while 60 patients were excluded due to early discharge and 26 patients did not want to par ticipate. Sixteen patients were later excluded because they did not have a stroke diagnosis, and one withdrew. Hence, 393 patients had available baseline data. Furthermore, three patients were excluded due to a lack of follow-up data, leaving a total of 390 patients to be included in the study. The flow of patients with and without pain data is described in . Assessment of pain at inclusion was implemented after the study had been in progress for a while. Hence, pain data were available in 174 patients at inclusion, while 142 patients had available pain data on both occasions, giving a sample of 142 patients available for the prevalence analysis. Out of 263 patients with available pain data at three months, 18 were lacking data on HADS, leaving a total of 245 patients available for the regression analysis. For patients alive, the main reasons for not responding when asked about pain were aphasia or dysarthria, other cognitive impairment, or loss to follow-up.
Figure 1 Illustration of patients assessed for pain at inclusion and three months after stroke.
Abbreviation: HADS, Hospital Anxiety and Depression Scale.
Baseline information of the patients included in prevalence analysis and the regression analysis is listed in .
Table 1 Baseline characteristics of all patients, patients responding to pain questionnaire, and patients with new-onset pain three months after stroke
Prevalence and distribution of pain
The prevalence analysis included 142 patients with complete pain data at both inclusion and three-month follow-up. Out of these, 45 patients (31.7%) reported pain at inclusion and 59 patients (41.5%) reported pain three months after stroke. Fourteen (9.9%) patients who reported pain at inclusion also reported that the pain had occurred after the stroke. Four of these patients still reported pain three months later, and 27 additional patients developed new pain, resulting in a total of 31 patients (21.8%) with new pain three months after stroke (), which constitutes a significant increase since inclusion, P=0.005. Of the 31 patients with new-onset pain three months after stroke, 18 (58.1%) used analgesics regularly.
Table 2 Prevalence and distribution of new-onset pain for patients with pain data at inclusion and three-month follow-up (n=142)
The anatomical distribution of new-onset pain is listed in . Patients could report pain from more than one location. New pain in the upper limb on the affected side of the body was significantly more common three months after stroke than at inclusion. New pain in the lower limb was also more common at three months, both in affected and unaffected parts of the body.
Associations between symptoms of anxiety or depression and new-onset pain three months after stroke
The regression analysis included all the 245 patients who responded to both the pain questionnaire and HADS three months after stroke. In the univariable regression analyses, female gender, higher score on the NIHSS, symptoms of anxiety, and depression were significantly associated with new-onset pain three months after stroke ().
Table 3 Univariable and multivariable logistic regression with new-onset pain at three months after strokeTable Footnotea as dependent variable, n=245
Results from the multiple regression model showed that anxiety, but not depression, was significantly associated with new pain, with an increased likelihood of concurrent pain as the score on the anxiety subscale of HADS increased. In a separate multivariable regression analysis (not shown in the table) not adjusted for depression, the association between anxiety and new-onset pain was slightly more pronounced (OR=1.16, 95% CI=1.06–1.27, P=0.001). When the analysis was not adjusted for anxiety, there was a significant association between depression and new-onset pain (OR=1.12, 95% CI=1.03–1.22, P=0.007).
Patients’ perception of how new-onset pain influences activities of daily living and enjoyment of life
A description of the scores from patients ranging the intensity of new-onset pain and how they perceived this pain to influence their daily activities and enjoyment of life is listed in . A total of 51% found the pain to have a moderate to severe influence on daily activities, while 53.5% of patients reported pain to have moderate to severe influence on enjoyment of life.
Table 4 Description of how patients with new-onset pain three months after stroke reported pain to influence their lives
Discussion
This study has shown that pain occurred in about 30% of patients initially after stroke, and one-third of these reported the pain to have occurred after the stroke. Three months later, pain was reported by 40% of the patients, and half of these found that the pain had developed after the stroke. New pain in the affected limbs and the unaffected lower limb was more frequently reported at three months compared to initially after the stroke. Anxiety was significantly associated with new-onset pain three months after stroke. Finally, half of the patients found new-onset pain to have a moderate to severe influence on their daily activities and quality of life.
Only one out of ten patients experienced new-onset pain early after stroke. This contrasts with other research reporting a prevalence ranging from 20% to 37.8% in the early phase after stroke.Citation3,Citation32 New-onset pain in 20% of patients at three months after stroke is similar to what was found by Sommerfeld et al, but lower than reported by Hansen et al who found that new pain occurred in 41.8% at three months after stroke.Citation3,Citation32 Hansen et al asked specifically for different types of pain, which might be one reason for the higher number of patients reporting pain. They also performed a sensory examination, and it is hypothesized that more abnormalities are found when physical examination is performed.Citation33 On the other hand, examinations were also performed in the study by Sommerfeld et al, and they still found a lower prevalence of pain. Differences in the selection of patients between the studies might also explain some of the inconsistencies.
The trend toward more new-onset pain at three months than initially after stroke was more prominent in our study than in the studies by Sommerfeld et al and Hansen et al. Only four patients who reported pain at inclusion to our study still experienced pain at the follow-up. This could imply that a different type of pain develops over time after stroke. We found an increase in new-onset pain in the limbs affected by the stroke, which is in accordance with previous studies on painful shoulder.Citation3,Citation11 We also found that the prevalence of new pain in the hip and leg on both the affected and unaffected sides had increased at three months after stroke. We did not differentiate between nociceptive and neuropathic pain, which would have provided a deeper understanding of the pain that evolves after stroke. However, pain in the affected lower extremity could be caused by altered muscle force and tone,Citation32,Citation34 while increased pain in the unaffected lower extremity could possibly be caused by an alteration in balance or gait pattern.
A relatively small number of patients, 4.9%, experienced new-onset pain in the head/neck. This is less than what is described in the literature, as previous studies have found the occurrence to be around 30%,Citation35–Citation37 and frequency in later stages is found to range from 15.3% to 7.2%.Citation3,Citation4,Citation35 Patients were told to ignore light pain that can occur from time to time, which possibly could explain our low numbers of headache.
Slightly more than half of all patients with new-onset pain at three months after stroke used analgesics regularly. Similar consumption was found in one previous study,Citation3 while others have reported that only 20% of stroke patients with pain use analgesics.Citation4 Comparing this to patients with other chronic conditions, 55% of patients with low back pain in the US had analgesic claims.Citation38 Among community-dwelling elderly people with chronic pain in Finland, analgesics were used daily by approximately 15%, and as required by approximately 60%.Citation39 Hence, the consumption in our group was quite similar to other groups with chronic pain. However, it would have been interesting to know what types of analgesics were used.
Experiencing symptoms of anxiety three months after stroke was associated with simultaneously occurring new-onset pain. Symptoms of depression were also associated with new-onset pain, but the association disappeared after adjusting for anxiety in the multivariable regression model. Previous research has shown that depression and anxiety are correlated,Citation31 but our results indicate that anxiety has a stronger association with new-onset pain after stroke than depression. Our finding is supported by another study, which found that both anxiety and depression were associated with impaired health-related quality of life, but only anxiety was significantly associated with pain after stroke.Citation40 This is noteworthy, especially since anxiety has been sparsely investigated in relation to pain after stroke.
To our knowledge, this is one of few studies conducted in a stroke unit with follow-up data focusing on pain early after stroke. In addition to assessing follow-up data on new pain after stroke, it shows that anxiety interacts with new-onset pain. In line with previous research,Citation3,Citation14 our study confirms that patients report new-onset pain to influence their daily activities and quality of life.Citation3,Citation14 This emphasize the importance of identifying these patients in order to provide adequate help.
When comparing baseline data of patients responding to pain questionnaires in our study with patients registered in the annual report from the Norwegian Stroke Register 2016,Citation41 they were similar concerning the number of infarctions, median age, and median score on NIHSS at admission to hospital, indicating that patients responding were representative of the general Norwegian stroke population
Invited patients who did not respond to the questionnaires were not a random group; these patients were significantly older, had more severe strokes, and were more likely to be women compared to those responding. Severe strokes may impair the ability to communicate, making patient-reported outcomes difficult to measure. We also found that patients with very mild strokes were less likely to be included due to short length of stay in hospital.
The greatest limitation of this study was the late implementation of pain assessment at inclusion, leaving a limited number of patients with complete pain data from both inclusion and three months later. However, when looking at age, gender, premorbid function and stroke severity, it seems that this was a random selection of patients, and the reported frequencies should be regarded as valid.
Pain is, to some degree, constantly present in any population,Citation22 and as pain is a subjective experience, it is difficult to measure for use in research. It is also challenging to differentiate between pain that occurs in relation to the stroke and pain with other causes. We intended to differentiate between new-onset pain and previous pain by asking specifically if pain occurred after the stroke. However, the patients’ ability to evaluate whether the pain occurred after the stroke may not be reliable, as there is a risk of recall bias, in addition to the difficulties evaluating the causes of pain, which in many cases may be complex. This methodological limitation could possibly have been reduced by doing a more thorough examination of the pain and by evaluating different possible causes in each individual. Some previous studies investigating post-stroke pain have additionally investigated if the pain was caused by wounds, fractures, rheumatoid arthritis and so on, and excluded this type of pain.Citation7,Citation32 In future research, a reference group should be included to be able to distinguish between pain that is stroke related and the pain that is not stroke related.Citation14
A more thorough description of the history of pain, including previous or current treatment, such as physiotherapy or rehabilitation related to the pain would give a more thorough understanding of the types of pain that develop after stroke. In addition, when it comes to depression and anxiety, it would be interesting to know about previous history and current treatment, which is not measured by HADS. It is important to remember that HADS simply measures current symptoms and is not a diagnostic tool.
Conclusion
In this study, we found that new-onset pain occurred in one out of ten patients initially after stroke and one out of five patients three months later. In particular, new pain was more frequent in the upper limb on the affected side of the body and lower limbs on both sides at three-month follow-up. Symptoms of anxiety were associated with new-onset pain, and it would be interesting to investigate if interventions to reduce anxiety could have a therapeutic effect on pain. Finally, the finding that more than half of patients with new-onset pain reported the pain to have a moderate to severe influence on daily activities and enjoyment of life is clinically important. Further research should focus on the prevention and the treatment of pain after stroke, and it would be interesting to know more about how anxiety and the use of analgesics interfere with the relationship between new pain and daily activities and enjoyment of life.
Data availability
Because of Norwegian regulations and conditions for informed consent, the data set is not publicly available.
Author contributions
The study was conceived by MRB, TA, and BI. TA, BI, and AH conducted the study. MRB contributed in collecting data. SL and MRB performed the statistical analyses. SL, MRB, TA, and BI interpreted the results. MRB and TA drafted the manuscript. All the authors critically revised the manuscript for important intellectual content and gave final approval of the version to be published.
Acknowledgments
The authors want to thank Mari Gunnes and Christine Sandø Lundemo for their contribution in collecting data. We thank Gitta Rohweder for feedback on the manuscript. Finally, we thank all the hospitals and personnel who helped in recruiting patients to this study. The study was funded by the Liaison Committee between the Central Norway Regional Health Authority and the Norwegian University of Science and Technology and the Research Council of Norway.
Disclosure
The authors report no conflicts of interest in this work.
References
- AppelrosPPrevalence and predictors of pain and fatigue after stroke: a population-based studyInt J Rehabil Res200629432933317106351
- IndredavikBRohwederGNaalsundELydersenSMedical Complications in a Comprehensive Stroke Unit and an Early Supported Discharge ServiceStroke200839241442018096834
- HansenAPMarcussenNSKlitHAndersenGFinnerupNBJensenTSPain following stroke: a prospective studyEur J Pain20121681128113622407963
- NaessHLundeLBroggerJWaje-AndreassenUPost-stroke pain on long-term follow-up: the Bergen stroke studyJ Neurol201025791446145220352249
- JonssonA-CLindgrenIHallstromBNorrvingBLindgrenAPrevalence and intensity of pain after stroke: a population based study focusing on patients’ perspectivesJ Neurol Neurosurg Psychiatry200677559059516354737
- O’DonnellMJDienerH-CSaccoRLChronic Pain Syndromes After Ischemic Stroke: PRoFESS TrialStroke20134451238124323559265
- LundströmESmitsATeréntABorgJRisk factors for stroke-related pain 1year after first-ever strokeEur J Neurol200916218819319138338
- Pain terms: a list with definitions and notes on usage. Recommended by the IASP Subcommittee on TaxonomyPain197963249460932
- CleelandCSRyanKMPain assessment: global use of the Brief Pain InventoryAnn Acad Med Singapore19942321291388080219
- HjermstadMJFayersPMHaugenDFStudies Comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for Assessment of Pain Intensity in Adults: A Systematic Literature ReviewJ Pain Symptom Manage20114161073109321621130
- RatnasabapathyYBroadJBaskettJPledgerMMarshallJBonitaRShoulder pain in people with a stroke: a population-based studyClin Rehabil200317330431112735538
- RohwederGEllekjaerHSalvesenONaalsundEIndredavikBFunctional Outcome After Common Poststroke Complications Occurring in the First 90 DaysStroke2015461657025395415
- van AlmenkerkSDeplaMFIASmalbruggeMEefstingJAHertoghCMPMPain among institutionalized stroke patients and its relation to emotional distress and social engagementInt J Geriatr Psychiatry201530101023103125581472
- KlitHFinnerupNBOvervadKAndersenGJensenTSPain Following Stroke: A Population-Based Follow-Up StudyPLoS One2011611e2760722102914
- NaessHLundeLBroggerJThe Triad of Pain, Fatigue and Depression in Ischemic Stroke Patients: The Bergen Stroke StudyCerebrovasc Dis201233546146522488041
- GurejeOSimonGEvon KorffMA cross-national study of the course of persistent pain in primary carePain200192119520011323140
- CastenRJParmeleePAKlebanMHLawtonPMKatzIRThe relationships among anxiety, depression, and pain in a geriatric institutionalized samplePain19956122712767659437
- BondessonEPardoFLStigmarKComorbidity between pain and mental illness - evidence of a bidirectional relationshipEur J Pain20182271304131129577509
- CastilloRCWegenerSTHeinsSEHaythornthwaiteJAMackenzieEJBosseMJLongitudinal relationships between anxiety, depression, and pain: results from a two-year cohort study of lower extremity trauma patientsPain2013154122860286623994104
- BurtonCACMurrayJHolmesJAstinFGreenwoodDKnappPFrequency of Anxiety after Stroke: A Systematic Review and Meta-Analysis of Observational StudiesInt J Stroke20138754555923013268
- TangW-KLauCGMokVUngvariGSWongK-SThe impact of pain on health-related quality of life 3 months after strokeTop Stroke Rehabil201522319420025906672
- LandmarkTRomundstadPDaleOBorchgrevinkPCKaasaSEstimating the prevalence of chronic pain: Validation of recall against longitudinal reporting (the HUNT pain studyPain201215371368137322575226
- HokstadAIndredavikBBernhardtJHospital Differences in Motor Activity Early after Stroke: A Comparison of 11 Norwegian Stroke UnitsJ Stroke Cerebrovasc Dis20152461333134025906937
- AhoKHarmsenPHatanoSMarquardsenJSmirnovVEStrasserTCerebrovascular disease in the community: results of a WHO collaborative studyBull World Health Organ19805811131306966542
- BrottTAdamsHPOlingerCPMeasurements of acute cerebral infarction: a clinical examination scaleStroke19892078648702749846
- BanksJLMarottaCAOutcomes Validity and Reliability of the Modified Rankin Scale: Implications for Stroke Clinical Trials: A Literature Review and SynthesisStroke20073831091109617272767
- CollinsSLMooreARMcquayHJThe visual analogue pain intensity scale: what is moderate pain in millimetres?Pain199772195979272792
- ZigmondASSnaithRPThe Hospital Anxiety and Depression ScaleActa Psychiatr Scand19836763613706880820
- AbenIVerheyFLousbergRLodderJHonigAValidity of the Beck Depression Inventory, Hospital Anxiety and Depression Scale, SCL-90, and Hamilton Depression Rating Scale as Screening Instruments for Depression in Stroke PatientsPsychosomatics200243538639312297607
- HerrmannCInternational experiences with the Hospital Anxiety and Depression Scale – a review of validation data and clinical resultsJ Psychosom Res199742117419055211
- BjellandIDahlAAHaugTTNeckelmannDThe validity of the Hospital Anxiety and Depression Scale. An updated literature reviewJ Psychosom Res2002522697711832252
- SommerfeldDKWelmerA-KPain following stroke, initially and at 3 and 18months after stroke, and its association with other disabilitiesEur J Neurol201219101325133022568638
- DromerickAWEdwardsDFKumarAHemiplegic Shoulder Pain Syndrome: Frequency and Characteristics During Inpatient Stroke RehabilitationArch Phys Med Rehabil20088981589159318597737
- TaniYOtakaYKudoMKurayamaTKondoKPrevalence of Genu Recurvatum during Walking and Associated Knee Pain in Chronic Hemiplegic Stroke Patients: A Preliminary SurveyJ Stroke Cerebrovasc Dis20162551153115726907679
- HansenAPMarcussenNSKlitHKaschHJensenTSFinnerupNBDevelopment of persistent headache following stroke: a 3-year followupCephalalgia201535539940925164919
- VerdelhoAFerroJMMeloTCanhãoPFalcãoFHeadache in Acute Stroke. A Prospective Study in the First 8 DaysCephalalgia200828434635418241222
- TentschertSWimmerRGreiseneggerSLangWLalouschekWHeadache at Stroke Onset in 2196 Patients With Ischemic Stroke or Transient Ischemic AttackStroke2005362e1e315604424
- VogtMTKwohCKCopeDKOsialTACulybaMStarzTWAnalgesic Usage for Low Back Pain: Impact on Health Care Costs and Service UseSpine20053091075108115864162
- KarttunenNMTurunenJHAhonenRSHartikainenSAPersistence of noncancer-related musculoskeletal chronic pain among community-dwelling older people: a population-based longitudinal study in FinlandClin J Pain2015311798524577431
- MorrisJHvan WijckFJoiceSDonaghyMPredicting health related quality of life 6 months after stroke: the role of anxiety and upper limb dysfunctionDisabil Rehabil201335429129922691224
- The Norwegian Stroke RegisterAnnual Report 2016201720-21 Available from: https://stolav.no/Medisinskekvalitetsregistre/Norsk-hjerneslagregister/%C3%85rsrapport2016-Norsk-hjerneslagregister.pdfAccessed December 14, 2017

