Abstract
Background: The primary objective of this systematic review was to identify the characteristics of physicians who prescribe opioids to adults with chronic pain. This review was limited to studies examining fully-trained physicians, as relevant characteristics of resident physicians and non-physician clinicians may differ.
Methods: A comprehensive search of databases from January 1, 1980 to December 5, 2017 was conducted. Eligible study designs included (1) randomized trials; (2) nonrandomized prospective and retrospective studies; and (3) cross-sectional observational studies. The risk of bias in the included studies was assessed using an adapted version of the Newcastle-Ottawa Scale for cross-sectional studies. A total of 2508 records were screened and 22 studies met inclusion criteria. The majority of studies were cross-sectional (n=20) and the total number of participants was 8433.
Results: The risk of bias was high overall. The majority of physicians were confident managing and prescribing opioids for chronic pain but had high levels of dissatisfaction. Physicians reported high awareness of the potential for opioid misuse and were concerned about inadequate prior training in pain management. The majority of physicians were less likely to prescribe for patients with a history of substance abuse and reported major concerns about regulatory scrutiny.
Conclusion: This systematic review provides the foundation for the development of prospective studies aimed at further elucidating the constellation of mechanisms that influence physicians who manage pain and prescribe opioids.
Introduction
Nonmedical use of prescription opioids remains a public health crisis.Citation1 Despite recent reductions in opioid prescribing, the quantity of prescribed opioids remains substantially elevated compared to the quantities prescribed prior the year 2000.Citation2,Citation3 The decline in opioid prescribing has been accompanied by a sharp rise in overdose deaths attributed to illicitly manufactured fentanyl while overdose deaths attributed to heroin have plateaued.Citation4 As national prescribing guidelinesCitation5 and public health campaignsCitation6 heighten awareness of the risks associated with long-term opioid therapy initiated for chronic pain, it is apparent that some opioid prescriptions originally intended for short-term use lead to unintended prolonged opioid use (UPOU).Citation7–Citation16
Our group has recently published a conceptual framework for understanding UPOU.Citation17 The overall goal of a conceptual framework is to provide a working schema to drive future hypothesis generation. In the absence of standardized methods for developing a conceptual framework, the process involves identifying corroborative evidence and coalescing expert opinion during the adjudication of factors intended for framework inclusion. The UPOU framework is comprised of 3 domains, including patient characteristics, practice environment characteristics, and opioid prescriber characteristics. The framework posited that characteristics of physicians that could influence prescribing behaviors include (1) training in pain management and opioid use; (2) personal attitudes and beliefs about opioids; and (3) perceived professional obligation to treat patients with chronic pain. As prescribers serve as the gatekeepers to prescription opioid access, the focal point of the framework is the opioid prescriber domain; the effects of the other two domains are ultimately mediated by individual prescribing behavior.
The primary objective of this systematic review was to identify the characteristics of physicians who prescribe opioids to adults with chronic pain. Secondary objectives included describing patient and practice environment factors that affect physicians who manage and prescribe opioids for chronic pain. This review was limited to studies examining fully-trained physicians, as relevant characteristics of resident physicians and non-physician clinicians may differ.
Methods
This systematic review was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.Citation18 An a priori protocol was followed.
Search strategy
A comprehensive search of databases from January 1, 1980 to December 5, 2017 was conducted. The databases included MEDLINE Epub Ahead of Print, Medline In-Process and Other Non-Indexed Citations, MEDLINE, EMBASE, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, and Scopus. The search strategy was designed and conducted by a medical reference librarian with input from the principal investigator. No language restrictions were applied. Controlled vocabulary supplemented with keywords was used to search for studies on practitioner characteristics influencing opioid prescribing practices. The actual search strategy is provided in Supplementary materials.
Study selection process
Eligible study designs included (1) randomized-, crossover-, and parallel-designed clinical trials; (2) nonrandomized prospective and retrospective longitudinal studies; and (3) cross-sectional observational studies. Based on our conceptual framework, inclusion criteria included all studies that reported information about (1) physician attitudes and beliefs about opioid use; (2) previous training in pain and opioid management; (3) professionalism; or (4) physician demographics. Exclusion criteria included (1) studies that mixed physician and non-physician data; (2) studies that reported data derived from physician responses to clinical vignettes; (3) data from medical students and residents-in-training; (4) studies of non-physicians and non-US physicians; and (5) qualitative studies that reported data from individual physician interviews.
The studies identified by the search strategy were screened in two phases. First, two independent pairs of reviewers screened all titles and abstracts. Second, the full text of all studies identified in the first phase were screened by two independent pairs of reviewers.
Data extraction
Data were extracted by four independent reviewers using a templated electronic database. Based on the study inclusion criteria and conceptual framework, abstracted data were initially organized into four main categories (attitudes and beliefs; previous training in pain management; professionalism; physician demographics). Following abstraction, data were reorganized into four main categories and several subcategories: (1) physician factors (main category) with subcategories including attitudes and beliefs about opioid use, pain training and knowledge, awareness of adverse events, and opioid management practices; (2) patient factors (main category) with subcategories including pain etiology and comorbid conditions, and patient satisfaction; (3) practice environment (main category) with subcategories including regulatory scrutiny and clinical resources; and (4) physician demographics. No information was identified about physician professionalism. Other data abstracted included (1) author and year of publication; (2) study design; (3) survey type; (4) total number of study participants targeted for recruitment; (5) number of participants completing the study; (6) overall response rate; and (7) physician demographics including age, sex, years of practice, practice environment (ie, group, solo, hospital-based) and practice location (ie, rural, urban); (8) source of study funding.
Risk of bias assessment
The risk of bias in the included studies was assessed by two independent reviewers using an adapted version of the Newcastle-Ottawa Scale for cross-sectional studies.Citation19 The adapted version is comprised of 3 domains (eg, selection, comparability and outcome) and has been
used in previous systematic reviews that involved cross-sectional studies.Citation20–Citation22 We did not calculate an overall score because this practice has been discouraged; rather, we made an overall judgement about the risk of bias focusing on the comparability domain. Reviewer discrepancy was resolved by consensus or by a third reviewer.
Evidence synthesis
Due to the heterogeneity in study characteristics, settings, and outcomes a meta-analysis was not feasible; thus, results are presented using a meta-narrative approach. A meta-narrative review can be used when an area in inquiry has been researched using disparate methods by different groups of investigators.Citation23,Citation24 This approach is particularly useful when the definition of key terms or clinical factors vary between studies. Meta-narrative methods have been used to study various populations of patients with chronic pain.Citation25–Citation29 Data were summarized using themes drawn from our conceptual framework and using descriptive statistics.
Results
Characteristics of included studies
A flow diagram of the study selection process is depicted in . A total of 22 studies met inclusion criteria (). The majority of studies were cross-sectional (n=20) where participants completed a survey at a single time point. Two studies used a repeated measures design; one study assessed participants pre-, post- and 6-months following a pain focused educational moduleCitation30 and one study assessed participants pre- and 2-years following an initiative to improve opioid prescribing safety.Citation31 The surveys were completed using email or internet-based software (n=10),Citation30,Citation32–Citation40 postal system (n=7),Citation41–Citation47 in-person completion of a paper version (n=2),Citation31,Citation48 and a combination of postal and email approaches (n=3).Citation49–Citation51 Three studies pilot tested surveys in small groups of physicians prior to useCitation41,Citation48,Citation49 and a single study used a validated survey.Citation39 A total of 23,726 physician participants [median =1042; 25th to 75th interquartile range (IQR), 271 to 2492; range, 46 to 6962] were targeted for study recruitment and 8433 (median =254; 25th to 75th IQR, 189 to 418; range, 33 to 1912) completed the surveys. Six studies did not report the total number of targeted participantsCitation32–Citation34,Citation39,Citation40,Citation50 and a single study did not report the number of participants completing the survey.Citation50 The median response rate for completion of the surveys was 35% (25th to 75th IQR, 26 to 58; range, 9 to 74); the response rate was not reported in 3 studies.Citation32–Citation34
Figure 1 Preferred reporting items for systematic reviews and meta-analyses flow chart of the study selection process.
Note: Reproduced from Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. Creative Commons license and disclaimer available from: http://creativecommons.org/licenses/by/4.0/legalcode “http://creativecommons.org/licenses/by/4.0/legalcode.Citation18
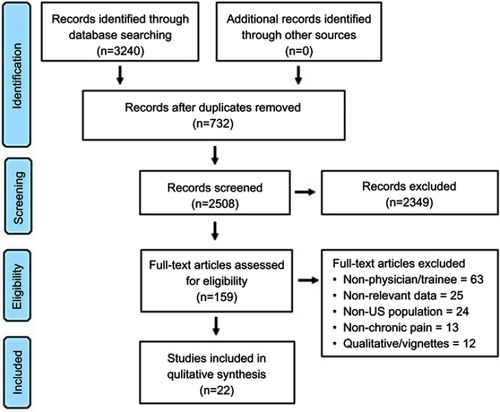
Table 1 Study characteristics
Study funding
The sources of funding were reported in 15 studies. Four studies received funding from the National Institutes of Health,Citation48,Citation49 or a combination of state and federal government agencies.Citation33,Citation37 Private foundations or universities provided funding for 5 studies.Citation30,Citation42,Citation45,Citation47,Citation51 A single study received funding from a state government agency and a private foundation.Citation50 Five studies received funding from industry; 4 of the 5 funding sources were from the pharmaceutical industryCitation32,Citation40,Citation41,Citation46 and the remaining study was funded by a health information company.Citation34 The funding source for 1 study was not reported but 2 co-authors were employed by a pharmaceutical company.Citation39
Risk of bias evaluation
contains the judgements made about each item of the Newcastle-Ottawa Scale for each study. The studies had major limitations in the comparability domain because of variations in study design and lack of study controls. Limitations were also noted in the selection domain due to variations in sample size and response rates. Similarly, limitations were noted in the outcome domain due to differences in methods used to perform the outcome assessment and variations in statistical analyses. Overall, the risk of bias was considered to be high across this body of evidence.
Table 2 Quality assessment using the adapted Newcastle-Ottawa scale for cross-sectional studies
Prescriber characteristics
Demographics
A national sample was used in 9 studiesCitation32,Citation34,Citation35,Citation39–Citation41,Citation46,Citation49,Citation51 and the 13 studies with state-level data were drawn from Massachutes,Citation43 Michigan,Citation42 Minnesota,Citation31 Ohio,Citation45 Pennsylvania,Citation30,Citation38 Texas,Citation36 Utah,Citation37 Washington,Citation33,Citation50 West Virginia,Citation44 and Wisconsin.Citation47,Citation48 The majority of participants (range, 70% to 100%) were primary care physicians in 6 studies,Citation35–Citation38,Citation44,Citation48 and the participant samples were comprised of mixed specialties in 8 studies.Citation30,Citation32,Citation34,Citation39,Citation41–Citation43,Citation49 The mean or median age of participants was reported in 5 studiesCitation41,Citation42,Citation45,Citation48,Citation51 and ranged from 41 to 51 years. The age range was reported in 3 studiesCitation32,Citation39,Citation44 in which the majority of participants were 35 to 60 years of age. Participant sex was reported in 11 studiesCitation30,Citation32,Citation35,Citation36,Citation39,Citation41,Citation42,Citation44,Citation45,Citation48,Citation51 with the proportion of male participants ranging from 49% to 86%. Race was reported in 4 studiesCitation35,Citation36,Citation42,Citation51 with the majority of physicians identified as “white” (range, 70% to 84%). The mean years of practice reported in 5 studiesCitation30,Citation32,Citation43–Citation45 ranged from 16 to 20 years and the majority of physicians in a single study had been in practice greater than 15 years.Citation39 In 4 studies,Citation36,Citation38,Citation41,Citation49 the majority of participants resided in urban areas (range, 52% to 91%) and, in 3 studies,Citation39,Citation41,Citation44 the majority of participants were in private or group practice.
Attitudes about pain and opioids
The majority of participants (73% to 88%) in 4 studies,Citation32,Citation35,Citation43,Citation50 which represented a mixture of primary care physicians and specialists, reported feeling confident, comfortable or competent prescribing opioids and managing pain. Several studies described physician satisfaction treating patients with chronic pain. Five studies that reported information related to the physician’s beliefs about pain and opioids were published between 2011 and 2015Citation31,Citation35,Citation37,Citation38,Citation50 and 2 studies were published earlier in 2001Citation42 and 2005.Citation44 High levels of dissatisfaction treating chronic pain were reported in 2 studies where 81% were not satisfied prescribing opioidsCitation35 and 85% were frustrated treating patients with chronic pain.Citation44 In a single study of university-based community physicians in Utah, satisfaction treating patients with chronic pain was assessed using a zero to 100 point visual analog scale where zero indicated no satisfaction and 100 indicated “much” satisfaction.Citation37 The median response of the 47 physicians was 16.Citation37 Alternatively, the majority of participants in a physician sample from Michigan were satisfied treating patients with chronic pain,Citation42 and 42% to 52% of physicians from Washington were moderately to extremely satisfied treating chronic pain.Citation50
Pain training and knowledge
Information about training in pain management was reported in 12 studiesCitation30,Citation31,Citation33,Citation37,Citation38,Citation40,Citation42,Citation44–Citation48 but the level of detail about training varied. In 5 studiesCitation30,Citation31,Citation37,Citation47,Citation48 published between 2006 and 2016, 32% to 72% of participants reported previous training in pain management. More specifically, in a study that involved 47 physicians working in a university-based community clinic system, 39% reported previous training about opioids during medical school, 70% reported training during residency, and 72% reported receiving opioid-related continuing medical education (CME).Citation37 Despite previous training, 54% continued to report inadequate training about opioids and 85% reported the need for additional training in addiction.Citation37 Similarly, in another study, 51% reported previous pain management training but only 43% reported having “good” to “excellent” knowledge about pain management.Citation47 An earlier study published in 2001Citation42 reported that 10% of participants had received pain management training and younger age was associated with a greater likelihood of receiving previous training. In 3 studies that span 19 years,Citation40,Citation44,Citation46 the majority of participants reported that previous pain management training was inadequate.
Physician participation and support of CME for chronic pain varied. In a national study,Citation31 pain specialists had devoted an average of 76 hrs of CME to pain management in the past three years compared to an average of 10 hrs for primary care providers (PCPs). For PCPs, there was a significant correlation between the number of CME hours and the level of confidence in treating musculoskeletal and neuropathic pain, being in favor of mandatory pain education, and treating with NSAIDs and tramadol.Citation31 In a separate study,Citation37 72% of physicians in a Utah university-based community clinic system (70% were PCPs) reported participating in an average of 5.25 hrs of pain management CME activities over the past 2 years. In one study in Washington,Citation33 79% to 84% of participants agreed that internet-based CME about pain management would be helpful.
Awareness of adverse events
The majority of participants (54–87%) reported some level of concern about opioid misuse, addiction, overdose, or diversion.Citation32,Citation33,Citation35,Citation36,Citation43,Citation44,Citation47–Citation49,Citation51 Opioid tolerance was identified as an impediment to long-term efficacy in 3 studies.Citation40,Citation46,Citation48 In a single study, 81–92% of participants reported that lost medications, request for early refills, persistent requests for opioids, and modifying opioid prescriptions were predictive of abuse.Citation37 Concerns about other adverse effects were described in 2 studies including nausea and vomiting, constipation, dizziness, drowsiness, and drug interactions.Citation32,Citation48 In a study from Ohio’s Appalachian counties, 36–40% of physicians perceived that patient fear of addiction and other adverse opioid effects were barriers to successful management of chronic pain.Citation45
Opioid management
Important areas about opioid management included knowledge and use of prescription drug monitoring programs (PDMP), urine drug screen (UDS), and opioid contracts. In 3 studies published between 2011 and 2016,Citation33,Citation37,Citation51 77–91% endorsed use of PDMP. However, there was greater variability regarding the use of opioid contracts. In a study published in 2016, 98% of respondents “somewhat” or “strongly” supported use of opioid contracts.Citation51 A 2011 study demonstrated that 64% of participants reported requiring patients to sign agreementsCitation38 and 89% of participants in a 2013 study reported “always” or “sometimes” having documentation of a medication contract.Citation37 In 2 studies published in 2015,Citation34,Citation50 only 32–51% reported always requiring opioid contracts. Similarly, less consensus was observed for use of UDS. In 3 studies published between 2010 and 2016,Citation37,Citation38,Citation50 19–47% of participants reported use of UDS but in a single study published in 2016,Citation51 88% of a national sample “somewhat” or “strongly” support use of UDS.
Patient factors
Pain etiology and co-existing conditions
Pain etiology and comorbid conditions influenced physicians' prescribing practices. In 2 studies,Citation44,Citation47 over 90% endorsed not prescribing to patients with a substance abuse history, and 60% to 81% reported reviewing the patient’s history for a substance abuse disorder prior to prescribing opioids.Citation50 The majority of physicians were more likely to prescribe opioids to patients with cancer-related pain compared to individuals with chronic nonmalignant pain.Citation48,Citation49 In one study, 62% of physicians did not prescribe opioids for fibromyalgia and 49% did not prescribe opioids for chronic headache.Citation49
Patient satisfaction
Although 74% of physicians in a national survey reported that pain management was a priority, 62% were concerned about “disagreement” with patients about opioids.Citation35 In a study from a Veterans Affairs hospital, the majority of physicians reported concerns that lowering opioid doses would upset patients.Citation31 In a single study, other physician perceived barriers to chronic pain management included patient reluctance to make lifestyle changes (88%), financial burden for the patient (73%), and lack of patient transportation (57%).Citation45
Practice environment
Regulatory scrutiny
Varying levels of concern about regulatory scrutiny were reported to influence prescribing practices. For example, 53–68% of participants in 3 studies based on state level data from Ohio,Citation45 West Virginia,Citation44 and WisconsinCitation47 reported that regulatory concerns influenced opioid prescribing practices. Alternatively, in 2 studiesCitation35,Citation41 based on national samples, 16–32% reported that potential regulatory scrutiny influenced prescribing practices.
Clinical resources
In 2 studies, 78–85% of physicians reported that access to a pain specialist would be helpful.Citation32,Citation33 Lack of access to pain specialists was identified as a barrier to chronic pain management by 53–78% physicians in 3 studies.Citation35,Citation37,Citation45 The use of clinical guidelines and standardized approaches to manage opioids varied. In a 2013 study,Citation37 26% reported lack of agreement among physicians and clinic staff regarding prescription of opioids for chronic pain. However, 100% of physicians (n=48) working at a Veterans Affairs hospital agreed that it was important to have a consistent standard for prescribing opioids.Citation31 In 2 studies, 56–68% reported that opioid prescribing policies, guidelines, algorithms or an opioid tracking system were available in their clinical setting.Citation33,Citation48 The presence of a clinical system to track patients using opioids was associated with a 2.5 greater odds of performing UDS.Citation48 Managing chronic pain was considered time consuming by 89% of physicians in a single study from West Virginia,Citation44 and in a study from Texas, 65% reported that prescribing continuous release opioids lengthened clinic visits.Citation36 In one study, 21% of participants reported that time constraints and limited staff support was the greatest barrier affecting implementation of patient-provider agreements.Citation34
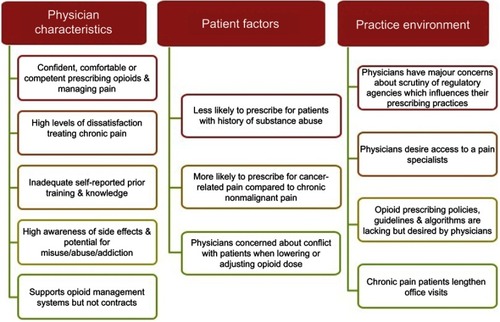
The main findings of this systematic review are summarized in which highlight physician views on chronic pain and opioids.
Discussion
This systematic review provides clinically relevant information and views of physicians who manage and prescribe opioids for chronic pain. Many physicians reported feeling at least somewhat confident or competent prescribing opioids and managing pain. In two studies,Citation25,Citation40 over 80% of respondents reported feeling confident and competent, while a much smaller proportion (19–52%) reported satisfaction treating pain and prescribing opioids. Further research is needed to elucidate how this dissatisfaction affects provider practices (eg prescriptions, care plans, communication, referrals) and to develop interventions to improve provider satisfaction treating chronic pain.
Inadequate training in pain management and opioids was also identified. For example, despite 51–70% of physicians reporting previous training in pain management and opioid prescribing, 54% reported that previous training was inadequate and only 43% reported having good to excellent knowledge about pain management. Other reports describing the associations between physician confidence and training in pain management and opioid prescribing have been mixed. These studies were not included in the systematic review because they included resident physicians and non-physician clinicians. In a study where the Opioid Therapy Provider Survey was completed by a mixed group of 69 clinicians (physicians =56%) attending a pain and opioid focused CME course, clinician confidence in managing chronic pain was not associated with previous training in pain management or mandated opioid-related CME.Citation52 However, in a study that involved 572 primary care physicians and residents-in-training, the intensity of post-residency education about pain management was associated with greater levels of comfort managing chronic pain.Citation53
Our findings suggest that despite perceived confidence, physicians could benefit from ongoing education and training about pain management and opioid prescribing. While one study reported a need for further training in addiction,Citation27 most of the studies in this review did not ask participants about the type of training needed. Because some of the findings suggest good knowledge about adverse events of opioids, additional research is needed to understand the specific training physicians would find beneficial. One study found that the number of CME hours correlated with greater levels of confidence in treating chronic pain.Citation41 Given this finding, voluntary participation in CME activities may be one approach to delivering ongoing pain-related education. The intensity of CME activity may need to be tailored to successfully meet the diverse expectations of individual physicians.
In addition to inherent prescriber characteristics, the results describe several patient and environmental factors that affect the physician. Patient diagnosis and patient satisfaction may play a role in physician decision to prescribe opioids. Physicians were more likely to prescribe opioids to patients with cancer than those with nonmalignant chronic pain. These provider views are in line with recent Centers for Disease Control and Prevention (CDC) guidelines that recommend opioids should be avoided for treatment of nonmalignant chronic pain when possible.Citation54 However, the two studies with these findings were published in 2006 and 2011, well before publication of the 2016 CDC guidelines.Citation38,Citation39 Further exploration is needed to understand how physicians perceive pain related to the patient’s diagnosis and whether these perceptions affect care management.
Physicians also reported that concern about regulatory scrutiny and limited resources influenced opioid prescribing practices. Regulatory scrutiny was found to negatively affect opioid prescribing. As regulatory oversight expands with the current opioid epidemic, it is important to understand the intended and unintended consequences on physician behavior.
This review found some factors which were directly reported to affect opioid prescribing but not to the extent anticipated in our original hypothesis. While we suspect that other physician-related factors affect opioid prescribing, more research is needed to specifically examine prescribing patterns of physicians by looking at actual prescription data. Although our conceptual framework was developed to better understand UPOU, the results of this review, which were centered around long-term opioid therapy, could be used to refine key components of the framework ().
This review has limitations. The literature search strategy was limited to studies comprised of practicing physicians; thus, the study findings may not represent the opioid prescribing practices of resident physicians or non-physician clinicians. The majority of physician participants were white men greater than 40 years of age who had been in clinical practice greater than 15 years and self-identified as residing in urban areas. Therefore, the findings may not be generalizable beyond the sociodemographic parameters of the study participants. The median response rate to the various surveys was 35% and 3 studies did not report a response rate. The methodological quality of all studies was low. As a result, the study findings may not be fully representative of the opioid prescribing practices of all physicians targeted for recruitment in the 22 studies identified in our literature search. The majority of surveys used in the identified studies were not validated which could jeopardize the accuracy and reproducibility of individual study results. Similarly, the characteristics of physician prescribing practices were assessed and described using a variety of methods, which limited the ability to consistently compare outcomes across studies. Finally, although heroin and illicitly manufactured fentanyl are important public health problems,Citation4 investigating the potential relationships between prescriber characteristics and individual use of illicitly acquired opioids are beyond the scope of this review.
In summary, this systematic review leveraged a conceptual framework to investigate the characteristics of physicians who prescribe long-term opioid therapy for chronic pain. The long-term goal of this area of research is to develop, test, and deploy interventions to mitigate the risks of long-term opioid use. The summary data from this systematic review provides the foundation for the development of prospective studies aimed at further elucidating the constellation of mechanisms that influence physicians who manage pain and prescribe opioids. It is anticipated that the outcomes of future studies will reveal the need for a range of time-dependent interventions to effectively attenuate the various clinician factors that contribute to long-term opioid use.
Disclosure
The authors report no conflicts of interest in this study.
References
- Califf RM, Woodcock J, Ostroff S. A proactive response to prescription opioid abuse. N Engl J Med. 2016;374:1480–1485. doi:10.1056/NEJMsr160130726845291
- Guy GP Jr., Zhang K, Bohm MK, et al. Vital signs: changes in opioid prescribing in the United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66:697–704. doi:10.15585/mmwr.mm6626a428683056
- Jeffery MM, Hooten WM, Henk HJ, et al. Trends in opioid use in commercially insured and medicare advantage populations in 2007–16: retrospective cohort study. BMJ. 2018;362:k2833. doi:10.1136/bmj.k283330068513
- Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and opioid-involved overdose deaths - United States, 2013–2017. MMWR Morb Mortal Wkly Rep. 2018;67:1419–1427. doi:10.15585/mmwr.mm675152e130605448
- Chang HY, Lyapustina T, Rutkow L, et al. Impact of prescription drug monitoring programs and pill mill laws on high-risk opioid prescribers: A comparative interrupted time series analysis. Drug Alcohol Depend. 2016;165:1–8. doi:10.1016/j.drugalcdep.2016.04.03327264166
- Substance Abuse and Mental Health Services Administration. Substance Misuse Prevention Media Campaigns. Available from: https://www.samhsa.gov/capt/tools-learning-resources/prevention-media-campaigns Accessed 210, 2017.
- Hooten WM, St Sauver JL, McGree ME, Jacobson DJ, Warner DO. Incidence and risk factors for progression from short-term to episodic or long-term opioid prescribing: A population-based study. Mayo Clin Proc. 2015;90:850–856. doi:10.1016/j.mayocp.2015.04.01226141327
- Callinan CE, Neuman MD, Lacy KE, Gabison C, Ashburn MA. The initiation of chronic opioids: a survey of chronic pain patients characterizing chronic opioid use. J Pain. 2017;18:360–365.27919771
- Stumbo SP, Yarborough BJH, McCarty D, Weisner C, Green CA. Patient-reported pathways to opioid use disorders and pain-related barriers to treatment engagement. J Subst Abuse Treat. 2017;73:47–54. doi:10.1016/j.jsat.2016.11.00328017184
- Deyo RA, Hallvik SE, Hildebran C, et al. Association between initial opioid prescribing patterns and subsequent long-term use among opioid-naive patients: a statewide retrospective cohort study. J Gen Intern Med. 2017;32:21–27. doi:10.1007/s11606-016-3810-327484682
- Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN, Bell CM. Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med. 2012;172:425–430. doi:10.1001/archinternmed.2011.182722412106
- Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DN. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ. 2014;348:g1251. doi:10.1136/bmj.g125124519537
- Sun EC, Darnall BD, Baker LC, Mackey S. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016;176:1286–1293. doi:10.1001/jamainternmed.2016.329827400458
- Shah A, Hayes CJ, Martin BC. Characteristics of initial prescription episodes and likelihood of long-term opioid use - United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66:265–269. doi:10.15585/mmwr.mm6610a128301454
- Barnett ML, Olenski AR, Jena AB. Opioid-prescribing patterns of emergency physicians and risk of long-term use. N Engl J Med. 2017;376:663–673. doi:10.1056/NEJMsa161052428199807
- Brummett CM, Waljee JF, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017;152:e170504. doi:10.1001/jamasurg.2017.050428403427
- Hooten WM, Brummett CM, Sullivan MD, et al. A conceptual framework for understanding unintended prolonged opioid use. Mayo Clin Proc. 2017. doi:10.1016/j.mayocp.2017.10.010
- Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi:10.1136/bmj.b265119622551
- Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-analyses. Ottawa, ON: Ottawa Hospital Research Institute; 2011 Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed May 1, 2018.
- Brady JE, Giglio R, Keyes KM, DiMaggio C, Li G. Risk markers for fatal and non-fatal prescription drug overdose: a meta-analysis. Inj Epidemiol. 2017;4:24. doi:10.1186/s40621-017-0118-728762157
- Herzog R, Alvarez-Pasquin MJ, Diaz C, Del Barrio JL, Estrada JM, Gil A. Are healthcare workers’ intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health. 2013;13:154. doi:10.1186/1471-2458-13-15423421987
- Patra J, Bhatia M, Suraweera W, et al. Exposure to second-hand smoke and the risk of tuberculosis in children and adults: a systematic review and meta-analysis of 18 observational studies. PLoS Med. 2015;12:e1001835; discussion e1001835. doi:10.1371/journal.pmed.1001809
- Wong G, Greenhalgh T, Westhort G, Pawson R. Development of methodological guidance, publication standards and training materials for realist and meta-narrative reviews: the RAMESES (Realist And Meta-narrative Evidence Syntheses - Evoling Standards) project. Health Serv Deliv Res. 2014;2:1–278. doi:10.1177/1742395313476901
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O, Peacock R. Storylines of research in diffusion of innovation: a meta-narrative approach to systematic review. Soc Sci Med. 2005;61:417–430. doi:10.1016/j.socscimed.2004.12.00115893056
- MacNeela P, Doyle C, O’Gorman D, Ruane N, McGuire BE. Experiences of chronic low back pain: a meta-ethnography of qualitative research. Health Psychol Rev. 2015;9:63–82. doi:10.1080/17437199.2013.84095125793491
- Sim J, Madden S. Illness experience in fibromyalgia syndrome: a metasynthesis of qualitative studies. Soc Sci Med. 2008;67:57–67. doi:10.1016/j.socscimed.2008.03.00318423826
- Snelgrove S, Liossi C. Living with chronic low back pain: a metasynthesis of qualitative research. Chronic Illn. 2013;9:283–301. doi:10.1177/174239531347690123585633
- Toye F, Seers K, Allcock N, et al. Patients’ experiences of chronic non-malignant musculoskeletal pain: a qualitative systematic review. Br J Gen Pract. 2013;63:e829–e841. doi:10.3399/bjgp13X67541224351499
- Wong AYL, Forss KS, Jakobsson J, Schoeb V, Kumlien C, Borglin G. Older adult’s experience of chronic low back pain and its implications on their daily life: study protocol of a systematic review of qualitative research. Syst Rev. 2018;7:81. doi:10.1186/s13643-018-0742-529793522
- Donovan AK, Wood GJ, Rubio DM, Day HD, Spagnoletti CL. Faculty communication knowledge, attitudes, and skills around chronic non-malignant pain improve with online training. Pain Med. 2016;17:1985–1992. doi:10.1093/pm/pnw02927036413
- Westanmo A, Marshall P, Jones E, Burns K, Krebs EE. Opioid dose reduction in a VA health care system-implementation of a primary care population-level initiative. Pain Med. 2015;16:1019–1026. doi:10.1111/pme.1269925645538
- Duensing L, Eksterowicz N, Macario A, Brown M, Stern L, Ogbonnaya A. Patient and physician perceptions of treatment of moderate-to-severe chronic pain with oral opioids. Curr Med Res Opin. 2010;26:1579–1585. doi:10.1185/0300799100378374720429822
- Franklin GM, Fulton-Kehoe D, Turner JA, Sullivan MD, Wickizer TM. Changes in opioid prescribing for chronic pain in Washington State. J Am Board Fam Med. 2013;26:394–400. doi:10.3122/jabfm.2013.04.12027423833154
- Kraus CN, Baldwin AT, Curro FA, McAllister RG. Clinical implications of patient-provider agreements in opioid prescribing. Curr Drug Saf. 2015;10:159–164.25986037
- Macerollo AA, Mack DO, Oza R, Bennett IM, Wallace LS. Academic family medicine physicians’ confidence and comfort with opioid analgesic prescribing for patients with chronic nonmalignant pain. J Opioid Manag. 2014;10:255–261. doi:10.5055/jom.2014.021325162605
- Nwokeji ED, Rascati KL, Brown CM, Eisenberg A. Influences of attitudes on family physicians’ willingness to prescribe long-acting opioid analgesics for patients with chronic nonmalignant pain. Clin Ther. 2007;29(Suppl):2589–2602. doi:10.1016/j.clinthera.2007.12.00718164924
- Porucznik CA, Johnson EM, Rolfs RT, Sauer BC. Opioid prescribing knowledge and practices: provider survey following promulgation of guidelines-Utah, 2011. J Opioid Manag. 2013;9:217–224. doi:10.5055/jom.2013.016223771571
- Slevin KA, Ashburn MA. Primary care physician opinion survey on FDA opioid risk evaluation and mitigation strategies. J Opioid Manag. 2011;7:109–115.21561034
- Turk DC, Dansie EJ, Wilson HD, Moskovitz B, Kim M. Physicians’ beliefs and likelihood of prescribing opioid tamper-resistant formulations for chronic noncancer pain patients. Pain Med. 2014;15:625–636. doi:10.1111/pme.1235224612185
- Wilson HD, Dansie EJ, Kim MS, Moskovitz BL, Chow W, Turk DC. Clinicians’ attitudes and beliefs about opioids survey (CAOS): instrument development and results of a national physician survey. J Pain. 2013;14:613–627. doi:10.1016/j.jpain.2013.01.76923541067
- Breuer B, Cruciani R, Portenoy RK. Pain management by primary care physicians, pain physicians, chiropractors, and acupuncturists: a national survey. South Med J. 2010;103:738–747. doi:10.1097/SMJ.0b013e3181e74ede20622716
- Green CR, Wheeler JR, Marchant B, LaPorte F, Guerrero E. Analysis of the physician variable in pain management. Pain Med. 2001;2:317–327. doi:10.1046/j.1526-4637.2001.01045.x15102236
- Nishimori M, Kulich RJ, Carwood CM, Okoye V, Kalso E, Ballantyne JC. Successful and unsuccessful outcomes with long-term opioid therapy: a survey of physicians’ opinions. J Palliat Med. 2006;9:50–56. doi:10.1089/jpm.2006.9.5016430344
- Ponte CD, Johnson-Tribino J. Attitudes and knowledge about pain: an assessment of West Virginia family physicians. Fam Med. 2005;37:477–480.15988631
- Remster EN, Marx TL. Barriers to managing chronic pain: perspectives of Appalachian providers. Osteopathic Family Physician. 2011;3:141–148. doi:10.1016/j.osfp.2010.07.003
- Turk DC, Brody MC, Okifuji EA. Physicians’ attitudes and practices regarding the long-term prescribing of opioids for non-cancer pain. Pain. 1994;59:201–208.7892017
- Wolfert MZ, Gilson AM, Dahl JL, Cleary JF. Opioid analgesics for pain control: wisconsin physicians’ knowledge, beliefs, attitudes, and prescribing practices. Pain Med. 2010;11:425–434. doi:10.1111/j.1526-4637.2009.00761.x20002590
- Bhamb B, Brown D, Hariharan J, Anderson J, Balousek S, Fleming MF. Survey of select practice behaviors by primary care physicians on the use of opioids for chronic pain. Curr Med Res Opin. 2006;22:1859–1865. doi:10.1185/030079906X13239816968589
- Chen L, Houghton M, Seefeld L, Malarick C, Mao J. Opioid therapy for chronic pain: physicians’ attitude and current practice patterns. J Opioid Manag. 2011;7:267–276.21957826
- Howell D, Kaplan L. Statewide survey of healthcare professionals: management of patients with chronic noncancer pain. J Addict Nurs. 2015;26:86–92. doi:10.1097/JAN.000000000000007526053081
- Hwang CS, Turner LW, Kruszewski SP, Kolodny A, Alexander GC. Primary care physicians’ knowledge and attitudes regarding prescription opioid abuse and diversion. Clin J Pain. 2016;32:279–284. doi:10.1097/AJP.000000000000026826102320
- Pearson AC, Moman RN, Moeschler SM, Eldrige JS, Hooten WM. Provider confidence in opioid prescribing and chronic pain management: results of the opioid therapy provider survey. J Pain Res. 2017;10:1395–1400. doi:10.2147/JPR.S13647828652805
- O’Rorke JE, Chen I, Genao I, Panda M, Cykert S. Physicians’ comfort in caring for patients with chronic nonmalignant pain. Am J Med Sci. 2007;333:93–100.17301587
- Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain–United States, 2016. JAMA. 2016;315:1624–1645. doi:10.1001/jama.2016.146426977696