Abstract
Background
Surgical injury can frequently lead to chronic pain. Despite the obvious importance of this problem, the first publications on chronic pain after surgery as a general topic appeared only a decade ago. This study tests the hypothesis that chronic postsurgical pain was, and still is, represented insufficiently.
Methods
We analyzed the presentation of this topic in journal articles covered by PubMed and in surgical textbooks. The following signs of insufficient representation in journal articles were used: (1) the lack of journal editorials on chronic pain after surgery, (2) the lack of journal articles with titles clearly indicating that they are devoted to chronic postsurgical pain, and (3) the insufficient representation of chronic postsurgical pain in the top surgical journals.
Results
It was demonstrated that insufficient representation of this topic existed in 1981–2000, especially in surgical journals and textbooks. Interest in this topic began to increase, however, mostly regarding one specific surgery: herniorrhaphy. It is important that the change in the attitude toward chronic postsurgical pain spreads to other groups of surgeries.
Conclusion
Chronic postsurgical pain is still a neglected topic, except for pain after herniorrhaphy. The change in the attitude toward chronic postsurgical pain is the important first step in the approach to this problem.
Introduction
The recent report of the Institute of Medicine’s committee on pain relief in the US indicated that “more than 116 million Americans have pain that persists for weeks to years.”Citation1 The important part of this problem is chronic postsurgical pain. Aasvang and KehletCitation2 estimated the incidence of chronic pain after some surgical procedures: thoracotomy (approximately 50%), breast surgery (30%), cholecystectomy (10%–20%), and inguinal herniorrhaphy (10%). When the total number of patients who undergo these surgeries each year is taken into account, those figures are stunning. MacraeCitation3 tried to present some figures that reflect the magnitude of the chronic postsurgical pain problem. His calculations yielded at least 400,000 new cases of chronic pain each year (in the US). He also indicatedCitation4 that about 20% of patients attending chronic pain clinics name surgery as one of the causes of their chronic pain, and for about half of these patients it was the sole cause.
Despite the obvious importance of this problem, publications on chronic pain after surgery as a general topic began to appear only a decade ago.Citation4–Citation6 These authors analyzed more than 100 references related to chronic postsurgical pain, noting that several features were common to all publications: (1) they were strictly limited to specific operations, (2) they failed to give a detailed description of the operative approaches, and (3) they usually provided only superficial assessments of chronic pain.Citation4,Citation6 Their conclusion was that “chronic pain after surgery has been a neglected topic.”Citation4
The word “postsurgical” in the term “chronic postsurgical pain” already indicates the role of surgery in its genesis. The combination of two factors related to coping with this problem gives surgery an additional importance: (1) ineffective existing treatments of neuropathic pain and (2) the importance of surgical techniques avoiding nerve injuries in the prevention of this type of chronic pain. Unfortunately, treatments for neuropathic pain, including the majority of chronic postsurgical pain cases, are not very effective. No more than 40%–60% of patients obtain pain relief; in addition, the relief is only partial.Citation7 Existing evidence indicates that intraoperative nerve injury is the most important contributor to the development of chronic postsurgical pain.Citation8,Citation9 The analysis of all possible approaches for the prevention of postsurgical pain points to one reliable solution: surgical techniques that avoid nerve damage should be used wherever possible.Citation8 As a result, although chronic postsurgical pain is a topic relevant to many specialties (surgery, anesthesiology, neurology, pain medicine, rehabilitation medicine, and psychology), currently, the most promising approach to reducing the incidence and intensity of chronic postsurgical pain is almost completely in the hands of surgeons, who can select techniques that minimize the risk of nerve damage. Therefore, the adequate presentation of chronic postoperative pain in surgical journals and textbooks is especially important.
Our study tested the hypothesis that chronic pain after surgery was, and still is, represented insufficiently. We analyzed the presentation of this topic in journal articles covered by PubMed, especially in surgical journals, and also in surgery textbooks.
Methods
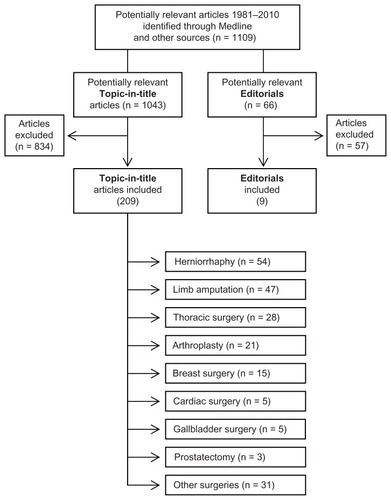
To test the study hypothesis with journal articles, we used the following three signs of insufficient representation: (1) the lack of journal editorials on chronic pain after surgery, (2) the lack of journal articles with titles clearly indicating that they are devoted to chronic postsurgical pain, and (3) the insufficient representation of chronic postsurgical pain in the top surgical journals. Concerning the analysis of textbooks, we followed the general approach used by Rabow et al.Citation10 The representation of chronic postsurgical pain in textbooks was assessed on the basis of the presence of this topic in general chapters and in the chapters on specific surgeries, as well as on the total content volume related to chronic pain after surgery. Journal articles were collected using the National Library of Medicine’s PubMed website (http://www.ncbi.nlm.nih.gov/PubMed). All types of articles published in English during 30 years (1981–2010) were included. Keywords related to the names of surgical interventions were added to the terms related to the chronic pain (“chronic pain” OR “neuropathy” OR “neuralgia”). Boolean operations were used in which the following variables were selected: keywords, years of publications, and type of publications. In addition to the electronic search of articles, related publications were also collected manually from the literature on chronic postsurgical pain ().
Figure 1 Flow chart of screened, excluded, and included articles on chronic postsurgical pain (1981–2010).
Editorials
The editorials (articles solicited by an editorial board to provide an editorial perspective on the article published in a journal) on chronic postsurgical pain were grouped into 5-year periods, starting with 1981–1985, separately for (1) all journals covered by PubMed and (2) only surgical journals.
Topic-in-title articles
To select journal articles with titles clearly indicating that they are devoted to chronic postsurgical pain (topic-in-title articles), the indication “[Title]” was added to all terms placed into PubMed search boxes. The topic-in-title type of articles were searched as representing chronic pain after surgery in general (when terms “surgery” [Title] OR “postoperative” [Title] were added to pain terms “chronic pain” [Title] OR “neuropathy” [Title]) or as representing chronic pain after specific surgeries (see ). The specific surgeries were selected on the basis of preliminary PubMed searches conducted with inclusion of various specific terms of surgical interventions and specific pain-related terms (indicated in ). In the preliminary searches, the indication “[Title]” in the PubMed search box was not used. The preliminary searches resulted in a total of 1043 references. The topic-in-title articles for a specific group of surgeries were counted only when a preliminary search for this group gave ten or more general (non-topic-in-title) references. Eight groups of surgeries were selected: herniorrhaphy, limb amputation, thoracic surgery, arthroplasty, breast surgery, cardiac surgery, gallbladder surgery, and prostatectomy. For inclusion as the topic-in-title publication, articles found in various searches were reviewed to make sure that they fit the definition of chronic pain after surgery. Articles with titles without certain indication of pain duration, such as “persistent,” “persisting,” “long-term,” “residual pain,” or “pain syndrome” were checked and included only if the duration of pain was 6 months or longer. If the duration of pain was indicated in the title of an article as 6 months or longer, it was also included in the database.
Table 1 Numerical representation of topic-in-title articles on chronic pain after specific surgeries, 1981–2010Table Footnotea
To quantitatively evaluate the response of surgical journals to the problem of chronic postsurgical pain, we analyzed the publications of topic-in-title articles in the top 20 surgical journals. It has been observed that the number of journal articles on a new and important topic rises much faster in the top specialty journals than it does in all other journals covered by PubMed.Citation11 We also calculated the Top Journal Selectivity Index (TJSI). This index represents the ratio of the number of articles in the top 20 surgical journals to the number of articles in all journals covered by PubMedCitation11,Citation12 (see Discussion). We counted only articles with titles clearly announcing that they are devoted to chronic pain after surgery (topic-in-title articles). The selection of the top 20 surgical journals was based on the rank of a journal sorted by the impact factor, as indicated by Journal Citation Reports for year 2010 (http://science.thomsonreuters.com). The following surgical journals were included: the American Journal of Surgery, American Journal of Surgical Pathology, American Journal of Transplantation, Annals of Surgery, Annals of Surgical Oncology, Archives of Surgery, British Journal of Surgery, Dermatologic Surgery, Endoscopy, Journal of the American Academy of Orthopaedic Surgeons, American Journal of Bone and Joint Surgery, Journal of Gastrointestinal Surgery, Journal of Shoulder and Elbow Surgery, Journal of Surgical Oncology, Journal of Vascular Surgery, Journal of Thoracic and Cardiovascular Surgery, Surgical Endoscopy, Surgery, Transplantation, and World Journal of Surgery.
Textbooks
The assessment of representation of chronic postsurgical pain in the surgical textbooks was based on the analysis of three texts selected on the basis of two factors: the text should be eponymously titled (named texts) and also should be sorted as one of the top three surgical texts held in libraries as listed in the meta-catalog WorldCat (worldcat.org). The following textbooks were selected: Sabiston Textbook of Surgery, 18th ed, 2008;Citation13 Schwartz’s Principles of Surgery, 9th ed, 2009;Citation14 and Greenfield’s Surgery, 5th ed, 2010.Citation15 For comparison, an anesthesiology textbook was also analyzed: Miller’s Anesthesia, 7th ed, 2010.Citation16 All textbooks were inspected on the presence of materials related to chronic postsurgical pain (number of lines of text, tables, figures, references). The data were collected in three steps: (1) review of chapters on basic principles (examination of the table of contents, identification of chapters devoted to general topics, inspection of all pages of identified chapters), (2) review of specific surgeries (examination of text index for keywords concerning specific surgeries: limb amputation, thoracotomy, coronary artery bypass grafting, mastectomy, cholecystectomy, herniorrhaphy, and arthroplasty; inspection of all pages of identified chapters), and (3) examination of the text index (keywords concerning specific chronic pain syndromes: causalgia, complex regional pain syndrome, neuralgia, neuropathy, pain chronic, pain neuropathic, phantom pain; inspection of all pages indicated for these terms.) Each textbook was assessed by two reviewers (SG and IK). Discrepancies in the count were resolved by consensus.
Results
Editorials
The results on the representation of chronic postsurgical pain in journal editorials are presented in . Since 1981 only nine editorials were published (two in 2001–2005 and seven in 2006–2010). Seven of them appeared in anesthesiological journals (four in Anesthesiology) and none in surgical journals.
Table 2 Editorials on chronic postsurgical pain
Topic-in-title articles
Topic-in-title articles (clearly announcing the problem of chronic postsurgical pain) are presented in . This table reflects only the number of articles that represent chronic pain after surgery in general. It indicates that the topic-in-title articles began to appear in significant numbers only relatively late, especially in surgical journals (2001–2010). compares the numbers of topic-in-title articles on chronic and acute postsurgical pain represented as a percentage of all articles on chronic or acute pain (without the indication “surgery” and “postoperative”). The percentage of the topic-in-title type of articles on chronic postsurgical pain was 0% in 1981–1990 and rose to 0.8% in 2001–2010. Nevertheless, even in 2001–2010 it was one-seventh the number on acute postsurgical pain.
Table 3 Topic-in-title articles on chronic postsurgical pain, 1981–2010
Table 4 Comparisons of topic-in-title articles on chronic and acute postsurgical pain
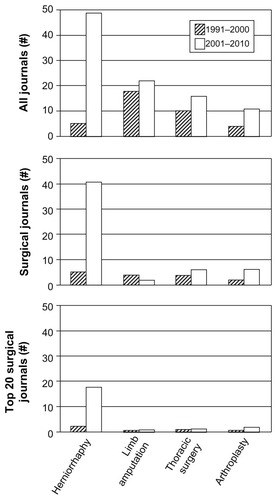
The summary of the results with the topic-in-title articles for eight specific groups of surgeries is presented in . The most publications were on herniorrhaphy (54 articles), then, in decreasing order, amputation (47), thoracic surgery (28), arthroplasty (21), breast surgery (15), and cardiac surgery (13). There were only five topic-in-title articles on gallbladder surgery and three on prostatectomy. The distribution of articles among journals of different specialties depended on the type of specific surgeries. With herniorrhaphy it was mostly surgical journals, with limb amputation mostly pain journals and disability/rehabilitation journals, and with all other surgeries mostly anesthesiology and pain journals. presents the time-related progress in numerical representation of topic-in-title articles on chronic pain after specific surgeries in all journals and separately in all surgical journals. In surgical journals the only impressive rise was for herniorrhaphy, from five articles in 1991–2000 to 41 in 2001–2010.
Table 5 Time-related progress in numerical representation of topic-in-title articles on chronic pain after specific surgeries
The publication of topic-in-title articles on chronic pain after surgery in the top 20 surgical journals is represented in . In 1991–2000 only two articles were published in the top surgical journals, but that dramatically increased (to 18) in 2001–2010. The TJSI calculated for herniorrhaphy (only for topic-in-title articles) was 36.7% in 2001–2010. That means that these articles published in the top 20 surgical journals constitute almost one-third of all articles published in journals covered by PubMed (>5000). However, the same index for the other seven surgeries was only 2.9%.
Table 6 Top Journal Selectivity Index (TJSI) for representation of chronic pain as an adverse effect of surgery
Textbooks
The textbook analysis is presented in . Only chronic pain after inguinal herniorrhaphy was present in all three surgical texts (but not in Miller’s Anesthesia). Greenfield’s Surgery mentioned chronic pain after three specific surgeries (more than the other texts in this regard); however, it did not include anything on chronic postsurgical pain in the chapters on basic principles. Orthopedic surgeries in general were included only in one of the three surgical texts; therefore, chronic pain after arthroplasty is not in the table. The number of chronic pain-related references varied from two to five in the surgical texts, and there were 12 references in Miller’s Anesthesia. The chronic pain-related figures or tables were absent in Sabiston Textbook of Surgery and Greenfield’s Surgery. There were two chronic pain-related tables in Schwartz’s Principles of Surgery. Miller’s Anesthesia included two figures and two tables related to chronic postsurgical pain. The total number of lines on chronic postsurgical pain was more or less similar: from 85 to 64 lines in the surgical texts and 100 lines in Miller’s Anesthesia. Taking into account that one page of the texts has approximately 120 lines and the total volume of the texts varies from 2000 to 3000 pages, the presentation of chronic pain after surgeries is almost negligible.
Table 7 Presentation of chronic postsurgical pain in surgical textbooks
Discussion
The indices that were used in this study indicated that the topic of chronic postsurgical pain is represented insufficiently, especially in surgical journals. Only nine editorials on chronic postsurgical pain were published in 1981–2010, all in nonsurgical journals. The articles clearly announcing the problem of chronic postsurgical pain (topic-in-title articles) began to appear in significant numbers only relatively late, in 2001–2010; however, even during the last decade they were sevenfold fewer than articles on acute postsurgical pain. In 1991–2000 only two topic-in-title articles on chronic pain after surgery were published in the top 20 surgical journals. There was a clear sign that the interest in chronic postsurgical pain began to increase in 2001–2010, but only in one group of surgeries: herniorrhaphy. The topic-in-title articles in all journals with this type of surgery increased from five (1991–2000) to 49 (2001–2010). The increase in postherniorrhaphy pain reporting is in stark contrast to publications regarding other types of postsurgical pain, especially in surgical journals ().
Figure 2 Number of topic-in-title articles published in 1991–2000 and 2001–2010 periods on chronic pain after the four types of specific surgeries.a Notes: aAlong the vertical axis, the number (#) of articles published in all journals (including surgical journals), the number of articles published in surgical journals (including top 20 surgical journals), and the number of articles published in top 20 surgical journals (listed in the method section). Along the horizontal axis, the four types of specific surgeries with the highest number of published articles.
The most significant sign of insufficient representation of chronic postsurgical pain is found in the presentation of this topic in surgical textbooks (2008–2010 editions). The presentation of chronic postsurgical pain in less than a page for various groups of surgeries per 2000–3000 pages of a textbook is clearly inadequate. However, chronic pain after herniorrhaphy is reflected in all three surgical texts analyzed (mostly very briefly).
Over the 10 years since the publication of seminal papers presenting postsurgical chronic pain,Citation4–Citation6 an important change has occurred but only in one area: chronic pain after herniorrhaphy. TJSI for herniorrhaphy has reached 36.7% (). It means that approximately one-third of all articles on herniorrhaphy in all journals covered by PubMed were published in the top 20 surgical journals. TJSI represents the ratio of the number of articles in the top 20 journals of the specialty to the number of articles in all journals covered by PubMed (>5000). A surge of this index is the sign of rising interest in a publication topic. For some reason, the top journals respond more rapidly to new and important developments in a specialty.Citation11,Citation12,Citation17 At a time when TJSI for chronic pain after herniorrhaphy was so high, it was ten times lower for seven other surgeries (2.9%), reflecting insignificant attention to chronic pain after these types of surgeries. Hopefully, the increased TJSI for herniorrhaphy indicates the initial change in the attitude toward chronic postsurgical pain in general and that it will soon spread to other groups of surgeries.
Such a change in attitude is necessary because of the vast number of patients with chronic postsurgical pain. MacraeCitation3 gave some insight into the magnitude of the problem by taking the number of operations performed in the US in 1994 (only for seven groups of surgeries) and multiplying it by the lowest figures for the incidence of chronic pain for these surgeries. His calculations yielded a possible 394,000 cases of chronic postsurgical pain each year. The complete absence of editorials related to this problem in the 1990–2000 period clearly indicates that the attention of the medical community was not focused on this type of pain.
The main reason for the neglect of chronic postsurgical pain in surgical journals and textbooks was well described by Macrae in 2001: “It is hard for any doctor to accept that the treatments they offer may cause morbidity, especially if they feel that they may be to blame.”Citation4 An additional reason might be that surgeons are less exposed to patients with developed chronic postsurgical pain than physicians in other specialties (eg, family medicine, pain medicine, neurology). At the same time, surgeons do have good reasons to feel that they are not to be blamed for chronic postsurgical pain. Although iatrogenic neuropathic pain caused by intraoperative nerve injury is the most common type of chronic postsurgical pain, this type of pain may also happen without any damage to a nerve trunk.Citation8,Citation9 In addition, nerve damage alone is usually not sufficient to cause chronic pain, because most of the cases of intraoperative nerve damage result in motor and sensory changes without the development of chronic pain. Chronic postsurgical pain is complex and poorly understood; there are many possible factors in its development (see reviewsCitation3,Citation8,Citation9).
It is accepted that chronic postsurgical pain is an inevitable consequence of surgery in a certain proportion of cases, like wound infection.Citation3 Chronic postsurgical pain should be discussed openly, and correct information on risk should be given to prospective patients. The incidence of chronic postsurgical pain varies very widely, up to 80% with limb amputations.Citation18 The Stabiston Textbook of SurgeryCitation13 indicates that chronic pain after open inguinal hernia repair has incidence ranging from 29% to 75%. A systematic review by Aasvang and KehletCitation2 reported that the overall incidence of chronic pain after open inguinal herniorrhaphy is 18%. In a recent large prospective study, Aasvang et alCitation19 found that the incidence of substantial pain 6 months after groin hernia repair was 12%. If patients had accurate information on their risk of chronic pain, they at least would be in the position to decide against an operation.
According to Kehlet et al,Citation8 the analysis of all possible approaches for the prevention of chronic postsurgical pain yields only one reliable solution: to use surgical techniques that avoid nerve damage. In a subsequent study,Citation19 these authors provided a rationale for selecting surgical techniques with a lower risk of chronic pain after groin hernia repair. They demonstrated that the incidence of “substantial pain” was significantly lower with laparoscopic than with open surgery (8.1% vs 16.0%, P < 0.02). A similar conclusion regarding chronic pain after laparoscopic versus open surgery was reached regarding cholecystectomy. Stiff et alCitation20 indicated that right upper quadrant chronic pain was less common after laparoscopic surgery (3.4% vs 9.7%, P < 0.05).
Although chronic postsurgical pain is relevant to many specialties (eg, surgery, anesthesiology, neurology, pain medicine, and rehabilitation medicine), risk can be decreased only by surgeons, because only they can choose to use techniques with lower risk of nerve damage. Chronic postoperative pain can also include anesthesia-related nerve injuries. Cheney et alCitation21 analyzed claims against anesthesiologists and found that 670 (16% of 4183) claims were for anesthesia-related nerve injury, including nerve injuries due to positioning of the patient after anesthesia induction. The most frequent sites of injury were the ulnar nerve (28%) and brachial plexus (20%).
Conclusion
In conclusion, chronic postsurgical pain is still insufficiently represented, especially in surgical journals and textbooks. However, there is an indication (rise in TJSI) that the interest in this topic began to increase. At present, the increase is mostly related to one specific group of surgeries: herniorrhaphy. However, it is likely that the change in the attitude toward chronic postsurgical pain will spread to other specific groups of surgeries.
Supplementary material
- AasvangEKehletHSurgical management of chronic pain after inguinal hernia repairBr J Surg20059279580115962258
- AasvangEKBay-NeilsenMKehletHPain and functional impairment 6 years after inguinal herniorrhaphyHernia20061031632116710627
- AasvangEKBrandsborgBJensenTSKehletHHeterogeneous sensory processing in persistent postherniotomy painPain201015023724220403664
- AasvangEKGmaehleEHansenJBGmaehleBFormanJLSchwarzJPredictive risk factors for persistent postherniotomy painAnesthesiology201011295796920234307
- AasvangEKJensenKEFiirgaardBKehletHMRI and pathology in persistent postherniotomy painJ Am Coll Surg20092081023102819476886
- AasvangEKKehletHChronic pain after childhood groin hernia repairJ Pediatr Surg2007421403140817706504
- AasvangEKKehletHThe effect of mesh removal and selective neurectomy on persistent postherniotomy painAnn Surg200924932733419212190
- AlfieriSRotondiFDi GiorfioAFumagalliUSalzanoADi MiceliDGroin Pain Trial GroupInfluence of preservation versus division of ilioinguinal, iliohypogastric, and genital nerves during open mesh herniorrhaphy: prospective multicentric study of chronic painAnn Surg200624355355816552209
- AmidPKHiattJRNew understanding of the cause and surgical treatment of postherniorrhaphy inguinodynia and orchalgiaJ Am Coll Surg200720538138517660088
- AsnisSEHanleySSheltonPDSciatic neuropathy secondary to migration of trochanteric wire following total hip arthroplastyClin Orthop Relat Res19851962262283888469
- BachSNorengMFTjelldenNUPhantom limb pain in amputees during the first 12 months following limb amputation, after preoperative lumbar epidural blockadePain1988332973013419837
- Bay-NielsenMPerkinsFMKehletHPain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire studyAnn Surg20012331711141218
- BisgaardTRosenbergJKehletHFrom acute to chronic pain after laparoscopic cholecystectomy: a prospective follow-up analysisScan J Gastroenterol20054013581364
- BittnerRGmähleEGmähleBSchwarzJAasvangEKehletHLightweight mesh and noninvasive fixation: an effective concept for prevention of chronic pain with laparoscopic hernia repair (TAPP)Surg Endosc2010242958296420526620
- BosmansJCSuurmeijerTPHulsinkMvan der SchansCPGeertzenJHDijkstraPUAmputation phantom pain and subjective well-being: a qualitative studyInt J Rehabil Res2007301817293714
- BowerSMooreBBWeissSMNeuralgia after inguinal hernia repairAm Surg1996626646678712565
- BozukMSchusterRStewartDHicksKGreaneyGWaxmanKDisability and chronic pain after open mesh and laparoscopic inguinal hernia repairAm Surg20036983984114570359
- BrandsborgBNikolajsenLHansenCTKehletHJensenTSRisk factors for chronic pain after hysterectormy: a nationwide questionnaire and database studyAnesthesiology20071061003101217457133
- BruceJDruryNPoobalanASJeffreyRRSmithWCChambersWAThe prevalence of chronic chest and leg pain following cardiac surgery: a historical cohort studyPain200310426527312855337
- BuvanendranAKroinJSDella ValleCJKariMMoricMTumanKJPerioperative oral pregabalin reduces chronic pain after total knee arthroplasty: a prospective, randomized, controlled trialAnesth Analg201011019920719910619
- CallesenTBechKKehletHProspective study of chronic pain after groin hernia repairBr J Surg1999861528153110594500
- CarleCAshworthARoscoeAA survey of post-sternotomy chronic pain following cardiac surgeryAnaesthesia200964138720092536
- CasscellsCDLindseyRWEbersoleJLiBUlnar neuropathy after median sternotomyClin Orthop Relat Res19932912592658389262
- CatchloveRFPhantom pain following limb amputation in a paraplegic. A case reportPsychother Psychosom19833989936878596
- ChauhanBMKimDJWainapelSFSaphenous neuropathy following coronary artery bypass surgeryN Y State J Med1981812222236258112
- ClarkeHPereiraSKennedyDAndrionJMitsakakisNGollishJAdding gabapentin to a multimodal regimen does not reduce acute pain, opioid consumption or chronic pain after total hip arthroplastyActa Anaesthesiol Scand2009531073108319572933
- ConacherIDPercutaneous cryotherapy for post-thoracotomy neuralgiaPain1986252272283725411
- ConacherIDTherapists and therapies for post-thoracotomy neuralgiaPain1992484094121594264
- CourtneyCADuffyKSerpellMGO’DwyerPJOutcome of patients with severe chronic pain following repair of groin herniaBr J Surg2002891310131412296903
- CrombieIKDaviesHTMacraeWACut and thrust: antecedent surgery and trauma among patients attending a chronic pain clinicPain1998761671719696470
- DajczmanEGordonAKreismanHWolkoveNLong-term postthoracotomy painChest1991992702741989781
- De KockMExpanding our horizons: transition of acute postoperative pain to persistent pain and establishment of chronic postsurgical pain servicesAnesthesiology200911146146319672181
- deJongePLloydAHorsfallLTanRO’DwyerPJThe measurement of chronic pain and health-related quality of life following inguinal hernia repair: a review of the literatureHernia20081256156918716856
- DennisRO’RiordanDRisk factors for chronic pain after inguinal hernia repairAnn R Coll Surg Engl20078921822017394701
- DesmondDMMaclachlanMPrevalence and characteristics of phantom limb pain and residual limb pain in the long term after upper limb amputationInt J Rehabil Res20103327928220101187
- DeVitaMARobinsonLRRehderJHattlerBCohenCIncidence and natural history of phrenic neuropathy occurring during open heart surgeryChest19931038508568449080
- DijkstraPUGeertzenJHStewartRvan der SchansCPPhantom pain and risk factors: a multivariate analysisJ Pain Symptom Manage20022457858512551807
- DijkstraPUReitmanJSGeertzenJHPhantom breast sensations and phantom breast pain: a 2-year prospective study and a methodological analysis of literatureEur J Pain2007119910816487732
- DualéCSibaudFGuastellaVValletLGimbertYATaheriHPerioperative ketamine does not prevent chronic pain after thoracotomyEur J Pain20091349750518783971
- DucicIMesbahiANAttingerCEGrawKThe role of peripheral nerve surgery in the treatment of chronic pain associated with amputation stumpsPlast Reconstru Surg2008121908914
- EggersKAAsaiTPostoperative brachial plexus neuropathy after total knee replacement under spinal anaesthesiaBr J Anaesth1995756426447577297
- EhdeDMCzernieckiJMSmithDGChronic phantom sensations, phantom pain, residual limb pain, and other regional pain after lower limb amputationArch Phys Med Rehabil2000811039104410943752
- EklundAMontgomeryABergkvistLRudbergCSwedish Multicentre Trial of Inguinal Hernia Repair by Laparoscopy (SMIL) study groupChronic pain 5 years after randomized comparison of laparoscopic and Lichtenstein inguinal hernia repairBr J Surg20109760060820186889
- EllisKA review of amputation phantom pain and nursing responsibilitiesBr J Nurs20021115515711865232
- ErdekMAStaatsPSChronic pain and thoracic surgeryThorac Surg Clin20051512313015707350
- ErhanYErhanEAydedeHMereanMTokDChronic pain after Lichtenstein and periotoneal (posterior) hernia repairCan J Surg20085138338718841221
- FainsingerRLdeGaraCPerezGAAmputation and the prevention of phantom painJ Pain Symptom Manage20002030831211027913
- FassoulakiAMelemeniAStaikouCTrigaASarantopoulosCAcute postoperative pain predicts chronic pain and long-term analgesic requirements after breast surgery for cancerActa Anaesthesiol Belg20085924124819235522
- FassoulakiASarantopoulosCMelemeniAHoganQEMLA reduces acute and chronic pain after breast surgery for cancerReg Anesth Pain Med20002535035510925929
- FassoulakiATrigaAMelemeniASarantopoulosCMultimodal analgesia with gabapentin and local anesthetics prevents acute and chronic pain after breast surgery for cancerAnesth Analg20051011427143216244006
- FerzliGSEdwardsEDKhouryGEChronic pain after inguinal herniorrhaphyJ Am Coll Surg200720533334117660082
- FischerSRChristDJRoehrBASciatic neuropathy secondary to total hip arthroplasty wear debrisJ Arthroplasty19991477177410512454
- FisherKHanspalRSPhantom pain, anxiety, depression, and their relation in consecutive patients with amputated limbs: case reportsBMJ19983169039049552839
- FlexmanANgJGelbAAcute and chronic pain following craniotomyCurr Opin Anaesthesiol20102355155720717011
- FlorHBirbaumerNPhantom limb pain: cortical plasticity and novel therapeutic approachesCurr Opin Anaesthesiol20001356156417016358
- FlorHPhantom-limb pain: characteristics, causes, and treatmentLancet Neurol2002118218912849487
- FokterSKRepse-FokterATakacICase report: femoral neuropathy secondary to total hip arthroplasty wear debrisClin Orthop Relat Res20094673032303519452234
- FrannebyUGunnarssonUAnderssonMValidation of an inguinal pain questionnaire for assessment of chronic pain after groin hernia repairBr J Surg20089548849318161900
- FrannebyUSandblomGNordinPNyrenOGunnarssonURisk factors for long-term pain after hernia surgeryAnn Surg200624421221916858183
- GallagherPAllenDMaclachlanMPhantom limb pain and residual limb pain following lower limb amputation: a descriptive analysisDisabil Rehabil20012352253011432649
- GerbershagenJHOzgurEDagtekinOPreoperative pain as a risk factor for chronic post-surgical pain – six month follow-up after radical prostatectomyEur J Pain2009 [Epub ahead of print.]
- GillionJFFagniezPLChronic pain and cutaneous sensory changes after inguinal hernia repair: comparison between open and laparoscopic techniquesHernia199937580
- GjeiloKHKlepstadPWahbaALydersenSStensethRChronic pain after cardiac surgery: a prospective studyActa Anaesthesiol Scand201054707819681771
- GotodaYKambaraNSakaiTThe morbidity, time course and predictive factors for persistent post-thoracotomy painEur J Pain20015899611394926
- GottschalkAOchrochEAClinical and demographic characteristics of patients with chronic pain after major thoracotomyClin J Pain20082470871618806536
- GranotMCan we predict persistent postoperative pain by testing preoperative experimental pain?Curr Opin Anaesthesiol20092242543019352173
- GrantAMScottNWO’DwyerPJFive-year follow-up of a randomized trial to assess pain and numbness after laparoscopic or open repair or groin herniaBr J Surg2004911570157415515112
- GrantPReiseOOvreSObturator neuropathy due to intrapelvic extrusion of cement during total hip replacement – report of 2 patientsActa Orthop Scand20017253754011728084
- HanleyMAJensenMPEhdeDMHoffmanAJPattersonDRRobinsonLRPsychosocial predictors of long-term adjustment to lower-limb amputation and phantom limb painDisabil Rehabil20042688289315497917
- HanleyMAJensenMPSmithDGPreamputation pain and acute pain predict chronic pain after lower extremity amputationJ Pain2007810210916949876
- HardenRNBruehlSStanosSProspective examination of pain-related and psychological predictors of CRPS-like phenomena following total knee arthroplasty: a preliminary studyPain200310639340014659522
- HardyPAPost-thoracotomy intercostal neuralgiaLancet198616266272869342
- HarviePGieleHFangCThe treatment of femoral neuropathy due to pseudotumour caused by metal-on-metal resurfacing arthroplastyHip Int20081831332019097010
- HassanIJacobsAGBaigMEVan der MeydenCHBilateral axillary and suprascapular neuropathy after coronary artery bypass surgeryCardiovasc J S Afr20061725926117117233
- HayesCArmstrong-BrownABurstalRPerioperative intravenous ketamine infusion for the prevention of persistent post-amputation pain: A randomized, controlled trialAnaesth Intensive Care20043233033815264726
- HazelriggSRCetindagIBFullertonJAcute and chronic pain syndromes after thoracic surgerySurg Clin North Am20028284986512472133
- HillAPhantom limb pain: a review of the literature on attributes and potential mechanismsJ Pain Symptom Manage19991712514210069153
- Hinricha-RockerASchulzKJarvinenIPsychosocial predictors and correlates for chronic postsurgical pain (CPSP): a systematic reviewEur J Pain20091371973018952472
- HompesRVansteenkisteFPottelHDevriendtDVan RooyFChronic pain after Kugel inguinal hernia repairHernia20081212713218026896
- HoughtonADSaadahENichollsGMcCollLHoughtonALPhantom pain: natural history and association with rehabilitationAnn R Coll Surg Engl19947622258117013
- HuseELarbigWBirbaumerNFlorHCortical reorganization and pain: empirical findings and therapeutic implication using example of phantom painSchmerz20011513113711810344
- HuseELarbigWFlorHBirbaumerNThe effect of opioids on phantom limb pain and cortical reorganizationPain200190475511166969
- HuseEPreisslHLarbigWBirbaumerNPhantom limb painLancet2001358101511586989
- IaconoRPSandykRBamfordCRAwerbuchGMaloneJMPost-amputation phantom pain and autonomous stump movements responsive to doxepinFunct Neurol198723433483692275
- IohomGAbdallaHO’BrienJThe associations between severity of early postoperative pain, chronic postsurgical pain and plasma concentration of stable nitric oxide products after breast surgeryAnesth Analg2006103995100017000819
- JahangiriMJayatungaAPBradleyJWDarkCHPrevention of phantom pain after major lower limb amputation by epidural infusion of diamorphine, clonidine and bupivacaineAnn R Coll Surg Engl1994763243267979074
- JensenTSKrebsBNeilsenJRasmussenPImmediate and long-term phantom limb pain in amputees: incidence, clinical characteristics and relationship to pre-amputation limb painPain1985212672683991231
- JensenTSKrebsBNielsenJRasmussenPPhantom limb, phantom pain and stump pain in amputees during the first 6 months following limb amputationPain1983172432566657285
- JessPJessTBeckHBechPNeuroticism in relation to recovery and persisting pain after laparoscopic cholecystectomyScand J Gastroenterol1998335505539648998
- JorgensenTTeglbjergJSWille-JorgensenPBilleTThorvaldsenPPersisting pain after cholecystectomy. A prospective investigationScand J Gastroenterol1991261241282006393
- KairaluomaPMBachmannMSRosenbergPHPerePJPreincisional paravertebral block reduces the prevalence of chronic pain after breast surgeryAnesth Analg200610370370816931684
- KalliomäkiMLMeyersonJGunnarssonUGordhTSandblomGLong-term pain after inguinal hernia repair in a population-based cohort; risk factors and interference with daily activitiesEur J Pain20081221422517606392
- KalsoEMennanderSTasmuthTNilssonEChronic post-sternotomy painActa Anaesthesiol Scand20014593593911576042
- KatzJPhantom limb painLancet1997350133813399365444
- KatzJPrevention of phantom limb pain by regional anaesthesiaLancet19973495195209048786
- KatzJAsmundsonGJMcRaeKHalketEEmotional numbing and pain intensity predict the development of pain disability up to one year after lateral thoracotomyEur J Pain20091387087819027333
- KatzJCohenLPreventive analgesia is associated with reduced pain disability 3 weeks but not 6 months after major gynecologic surgery by laparotomyAnesthesiology200410116917415220787
- KatzJJacksonMKavanaghBPSandlerANAcute pain after thoracic surgery predicts long-term post-thoracotomy painClin J Pain19961250558722735
- KatzJMelzackRPain ‘memories’ in phantom limbs: review and clinical observationsPain1990433193362293143
- KatzJSeltzerZTransition from acute to chronic postsurgical pain: risk factors and protective factorsExpert Rev Neurother2009972374419402781
- KatzJSchmidRSnijdelaarDGCoderreTJMcCartneyCJWowkAPre-emptive analgesia using intravenous fentanyl plus low-dose ketamine for radical prostatectomy under general anesthesia does not produce short-term or long-term reductions in pain or analgesic usePain200411070771815288412
- KehletHJensenTSWoolfCJPersistent postsurgical pain: risk factors and preventionLancet20063671618162516698416
- KehletHChronic pain after groin hernia repairBr J Surg20089513513618196556
- KellerJEStefanidisDDolceCJIannittiDAKercherKWHenifordBTCombined open and laparoscopic approach to chronic pain after inguinal hernia repairAm Surg20087469570018705569
- KellerSMCarpNZLevyMNRosenSMChronic post thoracotomy painJ Cardiovasc Surg1994351611647775532
- KempsterPGatesPByrneEWilsonAPainful sciatic neuropathy following cardiac surgeryAust N Z J Med1991217327351662042
- KöningerJRedeckeJButtersMChronic pain after hernia repair: a randomized trial comparing Shouldice, Lichtenstein and TAPPLangenbecks Arch Surg200438936136515243743
- KraneEJKellerLBThe prevalence of phantom limb sensation and pain pediatric amputeesJ Pain Symptom Manage19951021297714344
- KristensenADPedersenTAHjortdalVEJensenTSNikolajsenLChronic pain in adults after thoracotomy in childhood or youthBr J Anaesth2010104757919915188
- KronerKKrebsBSkovJJorgensenHSImmediate and long-term phantom breast syndrome after mastectomy: incidence, clinical characteristics and relationship to pre-mastectomy breast painPain1989363273342785259
- LambertADashfieldACosgroveCRandomized prospective study comparing preoperative epidural and intraoperative perineural analgesia for the prevention of postoperative stump and phantom limb pain following major amputationReg Anesth Pain Med20012631632111464349
- LandreneauRJMackMJHazelriggSRNaunheimKDowlingRDRitterPPrevalence of chronic pain after pulmonary resection by thoracotomy or video-assisted thoracic surgeryJ Thorac Cardiovasc Surg1994107107910858159030
- LauHPatilNGYuenWKLeeFPrevalence and severity of chronic groin pain after endoscopic totally extraperitoneal inguinal hernioplastySurg Endosc2003171620162312874688
- LautenbacherSHuberCSchoferDKunzMParthumAWeberPGAttentional and emotional mechanisms related to pain as predictors of chronic postoperative pain: a comparison with other psychological and physiological predictorsPain201015172273120850220
- Lavand’hommePDe KockMThe use of intraoperative epidural or spinal analgesia modulates postoperative hyperalgesia and reduces residual pain after major abdominal surgeryActa Anaesthesiol Belg200857373379
- LeslieTAIllingROCranstonDWGuillebaudJThe incidence of chronic scrotal pain after vasectomy: a prospective auditBJU Int20071001330133317850378
- LoftusLSLarongaCEvaluating patients with chronic pain after breast cancer surgery: the search for reliefJAMA20093022034203519903928
- LoosMJScheltingaMRMuldersLGRoumenRMThe Pfannensteil incision as a source of chronic painObstet Gynecol200811183984618378742
- LoosMJVerhagenTScheltingaMRRoumenRMA randomised controlled trial of injection therapy versus neurectomy for post-herniorrhaphy inguinal neuralgia: rationale and study designHernia20101459359720640584
- LundbladHKreicbergsAJanssonKAPrediction of persistent pain after total knee replacement for osteoarthritisJ Bone Joint Surg Br20089016617118256082
- MacraeWAChronic pain after sternotomyActa Anaesthesiol Scand20014592792811576040
- MacraeWAChronic pain after surgeryBr J Anaesth200187889811460816
- MacraeWAChronic post-surgical pain: 10 years onBr J Anaesth2008101778618434337
- MaguireMFLatterJAMahajanRBeggsDDuffyJPA study exploring the role of intercostal nerve damage in chronic pain after thoracic surgeryEur J Cardiothorac Surg20062987387916675262
- MaguireMFRavenscroftABeggsDDuffyJPA questionnaire study investigating the prevalence of the neuropathic component of chronic pain after thoracic surgeryEur J Cardiothorac Surg20062980080516581259
- ManikandanRSrirangamSJPearsonECollinsGNEarly and late morbidity after vasectomy: a comparison of chronic scrotal pain at 1 and 10 yearsBJU Int20049357157415008732
- MannyTBGorbachinskyIHemalAKLower extremity neuropathy after robot assisted laparoscopic radical prostatectomy and radical cystectomyCan J Urol2010175390539320974033
- MazzoleniRVokaerMMavroudakisNBartholoméEJBierJCAntiphospholipid antibodies and ischemic neuropathy following cardiac surgeryActa Neurol Belg200310317617814626699
- McMahonAJBuckleyJTaylorALloydSNDeanRFKirkDChronic testicular pain following vasectomyBr J Urol1992691881911537032
- MelamedNBStya-MurtiSObturator neuropathy after total hip replacementAnn Neurol1983135785796870210
- MeyersonJThelinSGordhTKarlstenRThe incidence of chronic post-sternotomy pain after cardiac surgery – a prospective studyActa Anaesthesiol Scand20014594094411576043
- MikkelsenTWernerMULassenBKehletHPain and sensory dysfunction 6 to 12 months after inguinal herniotomyAnesth Analg20049914615115281521
- MilesJPrevention of phantom pain after major lower limb amputation by epidural infusion of diamorphine, clonidine and bupivacaineAnn R Coll Surg Engl199577717717655
- ModirianEShojaeiHSoroushMRMasoumiMPhantom pain in bilateral upper limb amputationDisabil Rehabil2009311878188119925321
- MulveyMRBagnallAMJohnsonMIMarchantPRTranscutaneous electrical nerve stimulation (TENS) for phantom pain and stump pain following amputation in adultsCochrane Database Syst Rev201012CD00726420464749
- MyersMAHarmonRLSacral plexopathy and sciatic neuropathy after total knee arthroplastyElectromyogr Clin Neurophysiol1998384234269809230
- NienhuijsSStaalEStrobbeLRosmanCGroenewoudHBleichrodtRChronic pain after mesh repair of inguinal hernia: a systemative reviewAm J Surg200719439440017693290
- NikolajsenLBrandsborgBLuchtUJensenTSKehletHChronic pain following total hip arthroplasty: a nationwide questionnaire studyActa Anaesthesiol Scand20065049550016548863
- NikolajsenLIlkjaerSChristensenJHKronerKJensenTSRandomised trial of epidural bupivacaine and morphine in prevention of stump and phantom pain in lower-limb amputationLancet19973509088135313579365449
- NikolajsenLIlkjaerSKronerKChristensenJHJensenTSThe influence of preamputation pain on postamputation stump and phantom painPain1997723934059313280
- NikolajsenLKristensenADThillemannTMPain and somatosensory findings in patients 3 years after total hip arthroplastyEur J Pain20091357658118760945
- NikolajsenLSorensenHCJensenTSKehletHChronic pain following Caesarean sectionActa Anaesthesiol Scand20044811111614674981
- NunchuckSKeenanRJFersonPFPrevalence of chronic pain after pulmonary resection by thoracotomy or video-assisted thoracic surgeryJ Thorac Cardiovasc Surg1994107107910858159030
- O’DwyerPJKingsnorthANMolloyRGSmallPKLammersBHoreyseckGRandomized clinical trial assessing impact of a lightweight or heavyweight mesh on chronic pain after inguinal hernia repairBr J Surg20059216616715584057
- ObataHSaltoSFujitaNFuseYIshizakiKGotoFEpidural block with mepivacaine before surgery reduces long-term post-thoracotomy painCan J Anaesth1999461127113210608205
- ObergEJacobsenBRosenbergJChronic pain and recurrence after laparoscopic inguinal herniorrhaphySurg Laparosc Endosc Percutan Tech20051526726916215484
- OchrochEAGottschalkAAugostidesJLong-term pain and activity during recovery from major thoracotomy using thoracic epidural analgesiaAnesthesiology2002971234124412411810
- PaajanenHA single-surgeon randomized trial comparing three composite meshes on chronic pain after Lichtenstein hernia repair in local anesthesiaHernia20071133533917492341
- PailyAThorntonMChronic pain following a Lichtenstein inguinal hernia repair: a clinical and legal dilemmaANZ J Surg20097951752019694658
- PerttunenKTasmuthTKalsoEChronic pain after thoracic surgery: a follow-up studyActa Anaesthesiol Scan199943563567
- PessGMLusskinRWaughTRBattistaAEFemoral neuropathy secondary to pressurized cement in total hip replacement: treatment by decompression and neurolysis. Report of a caseJ Bone Joint Surg Am1987696236253032982
- PinzurMSSciatic nerve block for residual limb pain following below-knee amputationContemp Orthop19912229029210147554
- PluijmsWASteegersMAVerhagaenAFSchefferGJWilder-SmithOHChronic post-thoracotomy pain: a retrospective studyActa Anaesthesiol Scan200650804808
- PoleshuckELKatzJAndrusCHRisk factors for chronic pain following breast cancer surgery: a prospective studyJ Pain2006762663416942948
- PoobalanASBruceJKingPMChambersWAKrukowskiZHSmithWCChronic pain and quality of life following open inguinal hernia repairBr J Surg2001881122112611488800
- PoobalanASBruceJSmithWCKingPMKrukowskiZHChambersWAA review of chronic pain after inguinal herniorrhaphyClin J Pain200319485412514456
- PorterSSBlackDLRechlingFWMasonJIntraoperative cortical somatosensory evoked potentials for detection of sciatic neuropathy during total hip arthroplastyJ Clin Anesth198911701762627384
- RhoRHLamerTJFulmerJTTreatment of genitofemoral neuralgia after laparoscopic inguinal herniorrhaphy with fluoroscopically guided tack injectionPain Med2001223023315102257
- RichardsonCGlennSHorganMNurmikkoTA prospective study of factors associated with the presence of phantom limb pain six months after major lower limb amputation in patients with peripheral vascular diseaseJ Pain2007879380117631056
- RichardsonCGlennSNurmikkoTHorganMIncidence of phantom phenomena including phantom limb pain 6 months after major lower limb amputation in patients with peripheral vascular diseaseClin J Pain20062235335816691088
- RichardsonJSabanathanSMearnsAJSidesCGouldenCPPost-thoracotomy neuralgiaPain Clin199478797
- RichardsonJChronic pain after thoracic surgeryActa Anaesthesiol. Scand20004422010695918
- RomundstadLBreivikHRoaldHChronic pain and sensory changes after augmentation mammoplasty: long term effects of preincisional administration of methylprednisolonePain2006124929916650580
- RosenMJNovitskyYWCobbWSKercherKWHenifordBTCombined open and laparoscopic approach to chronic pain following open inguinal hernia repairHernia200610202416501867
- RozenDAhnJPulsed radiofrequency for the treatment of ilioinguinal neuralgia after inguinal herniorrhaphyMt Sinai J Med20067371671816878278
- SchleyMNTopofnerSWeichKContinuous brachial plexus blockade in combination with the NMDA receptor antagonist-memantine prevents phantom pain in acute traumatic upper limb amputeesEur J Pain20071129930816716615
- SchwabRWillmsAKrogerABeckerHPLess chronic pain following mesh fixation using a fibrin sealant in TEP inguinal hernia repairHernia20061027227716554980
- SearleRDSimpsonMPSimpsonKHMiltonRBennettMICan chronic neuropathic pain following thoracic surgery be predicted during the postoperative period?Interact Cardiovasc Thorac Surg20099999100219767301
- SeidASAmosEEntrapment neuropathy in laparoscopic herniorrhaphySurg Endosc19948105010537992173
- SenHSizlanAYanaratesOSenolMGInangilGSücüllüIThe effects of gabapentin on acute and chronic pain after inguinal herniorrhaphyEur J Anaesthesiol20092677277619424073
- SenturkMOzcanPETaluGKThe effects of three different analgesia techniques on long-term postthoracotomy painAnesth Analg200294111511772793
- SheridanPHJrCheriyanADoudJDornseifSEMontoyaAHouckJIncidence of phrenic neuropathy after isolated lung transplantation. The Loyola University Lung Transplant GroupJ Heart Lung Transplant1995146846917578176
- ShermanRAShermanCJParkerLChronic phantom and stump pain among American veterans: results of a surveyPain19841883956709380
- SimmonsCJrIzantTHRothmanRHBoothREJrBalderstonRAFemoral neuropathy following total hip arthroplasty. Anatomic study, case reports and literature reviewJ Arthroplasty19916557566
- SinghKPhillipsFMKuoECampbellMA prospective, randomized double-blind study of the efficacy of postoperative continuous local anesthetic infusion at the iliac crest bone graft site after posterior spinal arthrodesis: a minimum of 4-year follow-upSpine2007322790279618245999
- SkandalakisJESkandalakisLJColbornGLTesticular atrophy and neuropathy in herniorrhaphyAm Surg1996627757828751775
- SmedsSKaldALöfströmLChronic pain after open inguinal hernia repair: a longitudinal self-assessment studyHernia20101424925220052509
- SmithDGEhdeDMHanleyMAEfficacy of gabapentin in treating chronic phantom limb and residual limb painJ Rehabil Res Dev20054264565416586190
- SmithDGEhdeDMLegroMWReiberGEdel AguilaMBooneDAPhantom pain, residual limb, and back pain after lower extremity amputationsClin Orthoped Relat Res19993612938
- SmithJThompsonJMPhantom limb pain and chemotherapy in pediatric amputeesMayo Clinic Proc199570357364
- SmithWCSBourneDSquairJPhillipsDOChambersWAA retrospective cohort study of post mastectomy pain syndromePain199983919510506676
- SolakOMetinMEsmeHEffectiveness of gabapentin in the treatment of chronic post-thoracotomy painEur J Cardiothorac Surg20073291217442584
- StaerkleRFBuchliCVilligerPPatient satisfaction, hernia recurrence rate, and chronic pain. 10 years after endoscopic total extraperitoneal inguinal hernia repairSurg Laparosc Endosc Percutan Tech20091940540919851272
- SteegersMASnikDMVerhagenAFvan der DriftMAWilder-SmithOHOnly half of the chronic pain after thoracic surgery shows a neuropathic componentJ Pain2008995596118632308
- StevensPEDibbleSLMiaskowskiCPrevalence, characteristics, and impact of postmastectomy pain syndrome: an investigation of women’s experiencesPain19956161687644250
- StiffGRhodesMKellyATelfordKArmstrongCPReesBILong-term pain: Less common after laparoscopic than open cholecystectomyBr J Surg199481136813707953418
- StremmelCHornCEderSDimmlerALangWThe impact of immunological parameters on the development of phantom pain after major amputationEur J Vasc Endovasc Surg200530798215933988
- SwansonAJGThe incidence of prepatellar neuropathy following medial meniscectomyClin Orthop Rel Res1983181151153
- SwensonJDBullDAPostoperative ulnar neuropathy associated with prolonged ischemia in the upper extremity during coronary artery bypass surgeryAnesth Analg199785127512779390593
- TaniYMiyawakiHFemoral neuropathy caused by reinforcement ring malposition and extruded bone-cement after revision total hip arthroplastyJ Arthroplasty20021751651812066287
- TasmuthTKatajaMBlomqvistCvon SmittenKKalsoETreatment-related factors predisposing to chronic pain in patients with breast cancer – a multivariate approachActa Oncol1997366256309408154
- TasmuthTvon SmittenKKalsoEPain and other symptoms during first year after radical and conservative surgery for breast cancerBr J Cancer199674202420318980408
- van Hanswijck de JongePLloydAHorsfallLTanRO’DwyerPJThe measurement of chronic pain and health-related quality of life following inguinal hernia repair: a review of the literatureHernia20081256156918716856
- van VeenRNWijsmullerARVrijlandWWHopWCLangeJFJeekelJRandomized clinical trial of mesh versus non-mesh primary inguinal hernia repair: long-term chronic pain at 10 yearsSurgery200714269569817981189
- VikHAndersenKJJulshamnKTodnemKNeuropathy caused by silver absorption from arthroplasty cementLancet198584338722858727
- VilholmOJColdSRasmussenLSindrupSHThe postmastectomy pain syndrome: an epidemiological study on the prevalence of chronic pain after surgery for breast cancerBr J Cancer20089960461018682712
- VisserEChronic postsurgical pain: epidemiology and clinical implications for acute pain managementAcute Pain200687381
- VuilleumierHHübnerMDemartinesNNeuropathy after herniorrhaphy: indication for surgical treatment and outcomeWorld J Surg20093384184519156462
- WangJSinghAHigginsLWarnerJSuprascapular neuropathy secondary to reverse shoulder arthroplasty: a case reportJ Shoulder Elbow Surg201019e5e820056451
- WartanSWHamannWWedleyJRMcCollIPhantom pain and sensation among British veteran amputeesBr J Anaesth1997786526599215014
- WassenaarEBRaymakersJTRakicSRemoval of transabdominal sutures for chronic pain after laparoscopic ventral and incisional hernia repairSurg Laparosc Endosc Percutan Tech20071751451618097312
- WeissSALindellBPhantom limb pain and etiology of amputation in unilateral lower extremity amputeesJ Pain Symptom Manage1996113178815147
- WicksellRKOlssonGLPredicting and preventing chronic postsurgical pain and disabilityAnesthesiology20101131260128120966742
- WijsmullerARLangeJFMvan GeldereDSimonsMPKleinrensinkGJHopWCSurgical techniques preventing chronic pain after Lichtenstein hernia repair: state-of-the-arts daily practice in the NetherlandsHernia20071114715117171234
- Wilder-SmithOHSchreyerTSchefferGJArendt-NeilsenLPatients with chronic pain after abdominal surgery show less preoperative endogenous pain inhibition and more postoperative hyperalgesia: a pilot studyJ Pain Palliat Care Pharmacother20102411912820504133
- WildgaardKIversenMKehetHChronic pain after lung transplantation: a nationwide studyClin J Pain20102621722220173435
- WilsonJANimmoAFFleetwood-WalkerSMColvinLAA randomised double blind trial of the effect of pre-emptive epidural ketamine on persistent pain after lower limb amputationPain200813510811817583431
- WrightDPatersonCScottNHairAO’DwyerPJFive-year follow-up of patients undergoing laparoscopic or open groin hernia repair: a randomized controlled trialAnn Surg200223533333711882754
- YarnitskyDCripselYEisenbergEPrediction of chronic post-operative pain: pre-operative DNIC testing identifies patients at riskPain2008138222818079062
Disclosure
The authors report no conflicts of interest in this work.
References
- PizzoPAClarkNMAlleviating suffering 101 – pain relief in the United StatesN Engl J Med201236619719922256802
- AasvangEKehletHSurgical management of chronic pain after inguinal hernia repairBr J Surg20059279580115962258
- MacraeWAChronic post-surgical pain: 10 years onBr J Anaesth2008101778618434337
- MacraeWAChronic pain after surgeryBr J Anaesth200187889811460816
- CrombieIKDaviesHTMacraeWACut and thrust: antecedent surgery and trauma among patients attending a chronic pain clinicPain1998761671719696470
- PerkinsFMKehletHChronic pain as an outcome of surgery. A review of predictive factorsAnesthesiology2000931123113311020770
- DworkinRHO’ConnorABBackonjaMFarrarJTFinnerupNBJensenTSPharmacologic management of neuropathic pain: evidence-based recommendationsPain200713223725117920770
- KehletHJensenTSWoolfCJPersistent postsurgical pain: risk factors and preventionLancet20063671618162516698416
- KatzJSeltzerZTransition from acute to chronic postsurgical pain: risk factors and protective factorsExpert Rev Neurother2009972374419402781
- RabowMWHardieGEFairJMMcPheeSJEnd-of-life care content in 50 textbooks from multiple specialtiesJAMA200028377177810683056
- KissinICan a bibliometric indicator predict the success of a drug?Scientometrics201186785795
- KissinIBradleyELJrTop Journal Selectivity Index: is it acceptable for drugs beyond the field of analgesia?Scientometrics201188589597
- TownsendCMJrBeauchampRDEversBMMattoxKLSabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice18th edPhiladelphia, PASaunders/Elsevier2008
- BrunicardiFAndersenDBilliarTSchwartz’s Principles of Surgery9th edNew York, NYMcGraw-Hill Medical Pub Division2009
- MulhollandMWLillemoeKDDohertyGMMaierRVSimeoneDMUpchurchGRGreenfield’s Surgery: Scientific Principles and Practice5th edPhiladelphia, PAWolters Kluwer Health/Lippincot Williams & Wilkins2010
- MillerRDErikssonLIFleisherLAWeiner-KronishJPMiller’s Anesthesia7th edPhiladelphia, PAChurchill Livingstone Elsevier2010
- KissinIBradleyELJrTop Journal Selectivity Index and ‘me-too’ drugsScientometrics201291131142
- ShermanRAShermanCJParkerLChronic phantom and stump pain among American veterans: results of a surveyPain19841883956709380
- AasvangEKGmaehleEHansenJBGmaehleBFormanJLSchwarzJPredictive risk factors for persistent postherniotomy painAnesthesiology201011295796920234307
- StiffGRhodesMKellyATelfordKArmstrongCPReesBILong-term pain: less common after laparoscopic than open cholecystectomyBr J Surg199481136813707953418
- CheneyFWDominoKBCaplanRAPosnerKLNerve injury associated with anesthesia: a closed claims analysisAnesthesiology1999901062106910201678
- MacraeWAChronic pain after sternotomyActa Anaesthesiol Scand20014592792811576040
- GottschalkARajaSNSevering the link between acute and chronic pain: the anesthesiologists role in preventive medicineAnesthesiology200410110831085
- EisenachJCPreventing chronic pain after surgery: who, how and when?Reg Anesth Pain Med2006311316418016
- RomundstadLStubhaugAGlucocorticoids for acute and persistent postoperative neuropathic pain: what is the evidence?Anesthesiology200710737137317721239
- LoftusLSLarongaCEvaluating patients with chronic pain after breast cancer surgery: the search for reliefJAMA20093022034203519903928
- De KockMExpanding our horizons: transition of acute postoperative pain to persistent pain and establishment of chronic postsurgical pain servicesAnesthesiology200911146146319672181
- Lavand’hommePChronic pain after vaginal and cesarean delivery: a reality questioning our daily practice of obstetric anesthesiaInt J Obstet Anesth2010191219959352
- RappaportBACemyISanhaiWRAction on the prevention of chronic pain after surgery: public-private partnerships, the future of analgesic drug developmentAnesthesiology201011250951020124974
- EnckREPostsurgical chronic painAm J Hosp Palliat Care20102730130220466940
