Abstract
Objective
As pain during childbirth is very intense, several educational programs exist to help women prepare for the event. This study evaluates the efficacy of a specific pain management program, the Bonapace Method (BM), to reduce the perception of pain during childbirth. The BM involves the father, or a significant partner, in the use of several pain control techniques based on three neurophysiological pain modulation models: (1) controlling the central nervous system through breathing, relaxation, and cognitive structuring; (2) using non-painful stimuli as described in the Gate Control Theory; and (3) recruiting descending inhibition by hyperstimulation of acupressure trigger points.
Methods
A multicenter case control study in Quebec on pain perception during labor and delivery compared traditional childbirth training programs (TCTPs) and the BM. Visual analog scales were used to measure pain perception during labor. In all, 25 women (TCTP: n = 12; BM: n = 13) successfully reported their perceptions of pain intensity and unpleasantness every 15 minutes.
Results
A positive correlation between the progression of labor and pain was found (pain intensity: P < 0.01; pain unpleasantness: P < 0.01). When compared to TCTP, the BM showed an overall significant lower pain perception for both intensity (45%; P < 0.01) and unpleasantness (46%; P < 0.01).
Conclusion
These significant differences in pain perception between TCTP and the BM suggest that the emphasis on pain modulation models and techniques during labor combined with the active participation of a partner in BM are important variables to be added to the traditional childbirth training programs for childbirth pain management.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Pain is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage.Citation1 It consists of at least two components that are supported by independent neurophysiological pathways: the sensory-discriminative component (intensity) and the motivational-affective component (unpleasantness), which can be selectively modulated. Although the intensity of pain that women feel in childbirth is not usually associated with tissue damage, studies have ranked it as among the most severe forms of pain ever recorded using the McGill Pain Questionnaire or visual analog scales (VAS).Citation2,Citation3 The physiological and psychological effects of pain during labor and delivery are numerous and hardly trivial.Citation4,Citation5 Although new pharmacological procedures to relieve childbirth pain have proven effective in reducing pain,Citation6,Citation7 they are frequently associated with a higher incidence of dystocia, instrumental deliveries,Citation8,Citation9 and complications.Citation10 For example, women who use epidurals are more likely to need their labor contractions stimulated, to have a longer second stage of labor, the risk of instrumental delivery is increased (this is not associated with fetal distress) whereas the risk of caesarean section for fetal distress is increased.Citation11
Traditional childbirth training programs (TCTPs) aimed at preparing parents for childbirth are widely developed in Western countries. However, the true effects of such training on the perception of pain are still uncertain,Citation12 or controversial: some studies have found that training has no demonstrable effect on pain itself, but simply improves the reaction to pain.Citation13,Citation14 Others have found that women with adequate preparation experience from zero to 30% less pain during labor and delivery than women without preparation.Citation2,Citation15–Citation18
As we previously found for chronic pain measurement,Citation19 the primary explanation for this discrepancy regarding the perception of labor pain may be due to inadequate measurement methods, such as: (1) lack of sensitivity in pain measurement,Citation13 (2) inadequate measurement of the components of pain,Citation14 (3) measurement relying on the memory of pain,Citation13,Citation20 and (4) not accounting for pain modulation over time and context.Citation2,Citation17,Citation20
Because of potential side effects and complications of the epidural procedure and the limited effect of traditional childbirth programs in reducing labor pain, optimal and non-invasive pain relief approaches are needed. The Bonapace Method (BM) proposes to involve the father, or a significant partner, in reducing labor pain by practicing pain modulation techniques based on three neurophysiological endogenous pain modulation modelsCitation21 ( and ). First, the proposed method uses control of the central nervous system (CNSC) through breathing, relaxation, and cognitive structuring. Slow, deep breathing is often part of techniques frequently used to relieve pain, such as relaxation.Citation22,Citation27 Indeed, a recent study supports the use of slow breathing, by showing a reduction of experimental heat through the manipulation of breathing.Citation23 Another pain modulation technique used in this method is non-painful stimulation, such as light massage of the back, between labor contractions. The analgesia created by light massage is based on the Gate Control Theory proposed by Melzack and Wall,Citation24 where stimulation of non-nociceptive Aβ afferent fibers inhibit the nociceptive signal transmitted by Aδ and C fibers. Indeed, some studies have shown that one could obtain a reduction of pain through massage and ambulation.Citation25–Citation28 Finally, the BM uses analgesic hyperstimulation during contractions. Fathers or partners are asked to create a second pain in acupressure trigger points during contractions at all phases of labor and delivery. This type of stimulation seems to act by descending inhibitory projections that are coordinated in the rostroventral medulla and make up part of the spinal-bulbo-spinal diffuse noxious inhibitory control (DNIC) pathway.Citation29,Citation30 DNIC is a plausible mechanism by which acupressure to acupunctureCitation27,Citation31 points produces analgesia.Citation32,Citation33,Citation34,Citation35 From our perspective, a method combining these three neurophysiological endogenous pain modulation systems should demonstrate good efficacy in reducing both components of childbirth pain.
Figure 1 The different levels of pain modulation mechanisms used by the Bonapace Method.
Abbreviations: NRM, nucleus raphe magnus; PAG, periaqueductal gray matter.
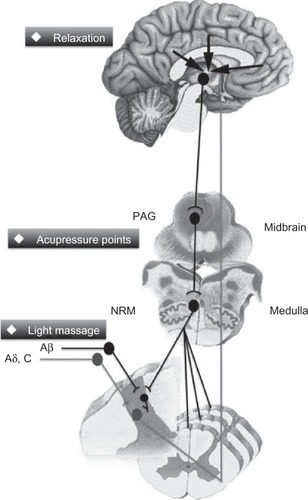
Table 1 Bonapace Method mechanisms and techniques
The aims of this multicenter case control study were: (1) to compare the effects on pain perception during labor and delivery between the BM, which specifically addresses pain modulation techniques, and TCTPs; (2) to better understand the relation between the progression of labor and pain, using validated measurement methods; and (3) to determine the potential for conducting a robust randomized controlled trial.
Methods
Subjects
Subjects for this study were recruited among patients of five medical clinics, affiliated with general hospitals, where no midwifery continuity of care programs were available, in the province of Quebec between 1995 and 1998. Subjects were informed of the nature of the study, which sought to better understand the perception of pain during childbirth, during their routine visit to the doctor, by a nurse or a research agent guided by a written protocol. Nothing was mentioned in relation to the correlation between the type of training and the perception of pain. All participating subjects were instructed on how to measure pain during labor and delivery using VAS. Each participant signed a consent form and received a pain management questionnaire to be completed during childbirth. After giving birth, they completed the demographic section of the questionnaire (age, parity, finances, education, onset of labor, and childbirth training). In accordance with the Université du Québec en Abitibi-Témiscamingue Human Subjects Ethics Committee, each subject was informed of her right to withdraw from the experiment at any time without prejudice. In consideration of the ethical problem involved in randomly imposing one type of treatment over another, the complexity involved in recruiting subjects for this study, and the need to determine the potential for a large, randomized controlled trial, we allowed subjects to assign themselves, during pregnancy, to the training program that best reflected their preferences: TCTP or the BM. All training programs were available at local community facilities, free of charge.
Treatment
The TCTP group consisted of women who had voluntarily chosen to follow that program with their partner. Training was started at approximately the 23rd week of pregnancy, and lasted a total of 8 hours over a 4-week period. The teaching curriculum of the TCTP was mostly based on a theoretical understanding of: (1) anatomy and physiology of childbirth; (2) physical well-being (exercises); (3) stages of labor and delivery; (4) variations in labor and birth; (5) pharmacological analgesia; and (6) caring for the newborn baby. Relaxation, visualization techniques, massages, and positions during labor were not taught in the TCTP. Only breathing techniques were practiced.
The BM group consisted of women who had voluntarily chosen to follow the specific pain management program with their partners. The curriculum of the BM incorporated the understanding of pain modulation mechanismsCitation21,Citation36 and the teaching of practical techniques related to those mechanisms. They included: (1) CNSC through breathing, relaxation, and cognitive structuring (origin of labor pain and endogenous pain modulating mechanisms); (2) non-painful stimuli, such as ambulation and light massage of the back by the partner between labor contractions, which activates non-nociceptive fibers and produces pain inhibition, as described in the Gate Control Theory;Citation24 and (3) DNIC analgesic hyperstimulation, by the partner during contractions, using deep painful massage of acupuncture trigger points in the lower back (namely, Shanglia BL 31, Cilia BL 32, Zhongliao BL 33 and Xialiao BL 34), alternating with trigger points in the hand (Hegu LI 4), the foot (Taichong L 3), and on the buttocks (Huantiao GB 30). Partners were taught to use whichever mechanisms suited them best during childbirth. The training program lasted eight hours over a four-week period. The women were approximately in their 30th week of pregnancy, and the entire program was dedicated to pain management and partner participation.
Procedure
Upon arrival at the hospital, each subject measured perceived pain intensity, and pain unpleasantness every 15 minutes immediately after a contraction, and at all phases of true labor and delivery. True labor was determined by contractions of increasing intensity, frequency, and length.Citation37 Measurements were recorded using two separate VAS, which had been found valid for non-pharmacological analgesia measurementCitation19 and for the measurement of labor pain.Citation2,Citation3,Citation38 The proposed methodology avoided the problems associated with pain measurements mentioned earlier. The pain VAS consisted of visual analog scales with verbal and numerical descriptors, whose end-points were designated as “no pain” and “the most intense imaginable”, for pain intensity, and “not unpleasant at all” and “the most unpleasant imaginable”, for pain unpleasantness. Cervical dilatation and medication were also recorded. Questionnaires were returned to hospital staff, then to research agents within days of the birth. Once the study was completed, data from subjects were grouped according to the training information they gave on their pain questionnaires.
In total, 39 women participated in this study. The TCTP group consisted of 19 women (ten multiparous and nine nulliparous); the BM group, 20 women (eight multiparous and twelve nulliparous). The criterion for determining parity was the number of times a woman had given birth to a foetus with a gestational age of 24 weeks or more, regardless of whether the child was born alive or was stillborn (none = nulliparous; once or more = multiparous). All data collected after the use of pharmacotherapy (epidural or sedatives) was eliminated. A total of 25 women (twelve of the TCTP group: eight multiparous and four nulliparous, and 13 of the BM group: seven multiparous and six nulliparous) met the following criteria (which were specified before the beginning of the study): (1) they were in active labor; and (2) had registered data for at least two of the four stages of labor and delivery. In total, 14 subjects were eliminated: two subjects for using sedatives (TCTP: one nulliparous; BM: one nulliparous), six subjects for reverting to an epidural (TCTP: three nulliparous; BM: three nulliparous), and six subjects for having stopped entering data (TCTP: two multiparous and one nulliparous; BM: one multiparous and two nulliparous). Subject age ranged between 19 and 40 (TCTP mean: 26 years; BM mean: 27 years), all had at least twelve years of education (TCTP mean: 14 years; BM mean: 16 years), each had a comparable average annual income per family, and comparable spontaneous onset of labor (TCTP: 75%; BM: 69.2%). No significant difference was found between the TCTP and BM groups for these variables ().
Table 2 Demographic characteristics
Statistical analysis
The first analysis (all participants, regardless of the method or the parity; n = 25) was made using pain ratings for the last six hours preceding delivery. A regression analysis compared the progression of pain with the progression of labor. The second series of analyses (all participants) separated labor and delivery in four phases:Citation3,Citation39 (1) early (one contraction every 5–20 minutes, cervical dilatation 0–4 cm at <0.5 cm/hr); (2) active (one contraction every 2–4 minutes, cervical dilatation 4–8 cm at >0.5 cm/hr); (3) transition (one contraction every 1–2 minutes, cervical dilatation 8–10 cm at >1.5 cm/hr); and (4) pushing (one contraction every 2–3 minutes, each lasting about 50–70 seconds, combined with effort). The number of evaluations per subject varied between 3 and 34, depending on the moment of arrival at the obstetrical unit, and on the length of labor (mean: 16, SD: 9.06). The main effects analyzed were group (BM versus TCTP) and the interaction between group and parity. Post-hoc analyses were made using planned contrasts. A probability of less than 5% was considered significant. Statistical analyses were performed using SuperANOVA (Abacus Concepts, Berkeley, CA, USA), a general linear modeling program, and StatView (SAS Institute, Cary, NC, USA). Missing values (twelve out of 100 values), for subjects having completed two or more of the four stages of labor, were obtained by adding the mean value of the subject’s total values to the mean value of their group’s moment, minus the mean total value of their group. The statistical degrees of freedom were adjusted accordingly.
Independent sample t-tests and chi-squared or Fisher’s exact tests were applied to determine if there were differences in demographic variables between experimental and control groups.
Results
Increase in pain as a function of the progression of labor
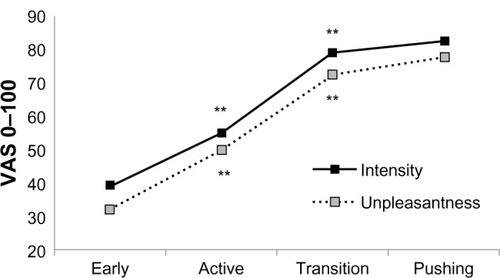
A positive correlation between pain and the progression of labor was found for both the TCTP and BM groups (pain intensity: R = 0.33, F = 12.96, P = 0.0005; pain unpleasantness: R = 0.24, F = 6.58, P = 0.01). Pain intensity and unpleasantness significantly increased between the early and active phases and between the active and transition phases, as shown in (F[3.72] = 23.957, P = 0.0001, and F[3.72] = 26.892, P = 0.0001, respectively).
Figure 2 Vas pain scores during phases of labor.
Abbreviation: VAS, visual analog scale.
Effect of the methods on pain
Overall, VAS pain scores revealed that there was a significant difference in pain perception between the BM and TCTP groups (). More specifically, the BM group perceived an average of 44.6% less pain intensity (F[1.25] = 22.00, P = 0.0001) and 46.5% less pain unpleasantness (F[1.25] = 11.26, P = 0.003), in comparison to the TCTP group (pain intensity: BM = 44.14 ± 16.08 versus TCTP = 79.13 ± 25.81; and pain unpleasantness: BM = 39.82 ± 17.04 versus TCTP = 74.42 ± 41.70). This difference was significant regardless of parity, for pain intensity (nulliparous: F[1.10] = 13.74, P = 0.0011; multiparous: F[1.15] = 8.269, P = 0.0083). For pain unpleasantness, however, this difference was found for nulliparous women only (nulliparous: F[1.10] = 10.74, P = 0.0032; multiparous: F[1.15] = 1.634, P = 0.2134) ( and ). A significant difference was also found between both programs for pain intensity during all four periods of labor, and for the active, transition, and pushing periods for pain unpleasantness ( and ). No difference was found for the use of pharmacological methods (sedatives and epidurals: TCTP = 4/39; BM = 4/39).
Figure 3 Mean comparison of VAS pain scores.
Abbreviations: VAS, visual analog scales; BM, Bonapace Method; TCTP, traditional childbirth training program; SD, standard deviation.
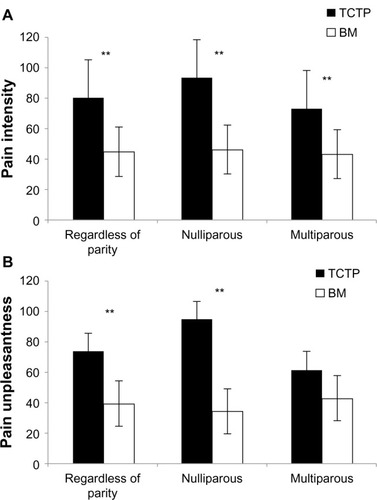
Figure 4 Mean comparison of VAS pain scores.
Abbreviations: VAS, visual analog scales; BM, Bonapace Method; TCTP, traditional childbirth training program; SD, standard deviation.
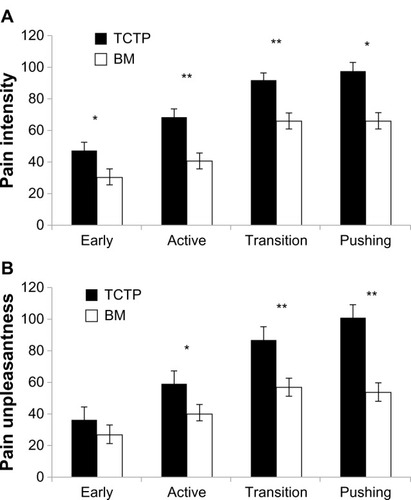
Table 3 Mean pain perception, standard deviation, and differences in pain reduction between the methods, according to parity
Table 4 Mean pain perception, standard deviation, and differences in pain reduction between the methods, according to training and different phases of labor and delivery
Discussion
To our knowledge, no other study has documented with precision the progression of pain during all phases of labor and delivery using a validated pain-measuring tool. Our findings show that pain increases in a predictable manner with the progression of labor. Although the perception of pain varied greatly from one woman to another, the mean pain ratings of both groups revealed a steady and significant increase in pain intensity and unpleasantness with the dilation of the cervix, consistent with descriptions in obstetrical booksCitation39 and previous research.Citation40 A regression analysis confirmed these findings.
Regarding the overall effect of the BM, the present findings demonstrate an important reduction in pain intensity and unpleasantness perception with the BM, compared to TCTP. The significant effect of the BM on the reduction of pain intensity for both nulliparous and multiparous women indicates that an effective pain management program can be useful in increasing coping attitudes, regardless of previous experience with birth (). Differences are particularly important during the longest and the most difficult phases of parturition (active, transition, and pushing phases) (). The lack of difference for pain unpleasantness between multiparous women may be explained by “experience”. It is well known that one of the main concerns of nulliparous women is fear of the unknown (childbirth), which in turn increases the subjective dimension of pain. Multiparous women, because of their previous experience with labor pain, have a better understanding of what to expect during childbirth. It is this reduction of fear and anxiety that may be responsible for less pain unpleasantness during parturition.Citation2
Consistent with studies on massage,Citation26 ambulation,Citation28 support,Citation41 acupressure,Citation35 and yoga,Citation42 our results show that these methods help cope with pain. Yoga, acting on both the body (pain intensity) and the mind (pain unpleasantness), has proven to be effective in reducing pain perceptionCitation42 and improving fetal outcomes (increasing birth weight and reducing prematurity).Citation43 The literature on childbirth training programs is inconsistent.Citation12 While some studies show no increased outcomes with training,Citation44,Citation45 one study showed that women who participated in antenatal classes used less epidural analgesia during labor (relative risk [RR] = 0.84, 95% CI = 0.73–0.97; P < 0.01), but did not experience less pain relief overall (RR = 0.99, 95% CI = 0.94–1.04; P < 0.72).Citation46 Increasing competencies and abilities through practice, feedback, and positive example seems to be an important part of programs that provide positive outcomes.Citation17 Our study showed the importance of combining various techniques that influence both components of pain. Consistent with the findings of Price et al,Citation3 childbirth – a positive event in the life of a woman – was found to be a more intense than unpleasant experience. This may explain why only the intensity of pain was significantly reduced in multiparous women in our study.
The strengths of this multicenter case control study can be summarized as follows: a sensitive pain measurement tool (scoring range: 0–100) with verbal and numerical descriptors was used, allowing precise and nuanced data to be gathered. Two separate VAS were used, for evaluation of both the sensory and affective components of pain. Numerous assessments of pain perception were made by subjects during all phases of labor and delivery, thus preventing problems related to poor memory of pain and observer bias. Consistent briefing was provided to subjects with regard to the experimental design and the assessment of pain. Subjects were blind with respect to the aim of the study, in order to avoid motivation factors that could impact data (ie, subjects trying to justify the training they followed). Subjects were recruited from five typical regional general hospital maternities in the province of Quebec, which offer the same type of practice and services. When tested for age, finances, parity, and education, groups were found to be comparable ().
Limitations
Some confounding factors were not controlled for and may limit the scope of this study. However, it was essential to have data on the efficacy of the BM before ethically conducting a randomized controlled trial in a clinical situation. The data obtained in this study are supportive of a significant reduction of pain with the BM, and future studies are needed to confirm our results. A problem in evaluating the possible effects of preparation for childbirth is whether motivation is chiefly responsible for benefits conferred by preparation rather than the preparation itself. Because all women in this study sought preparation and were prepared to varying degrees, all women were motivated to prepare to some extent, which limits the impact of this variable.Citation47
The final sample size (n = 25) may appear small; it is due to the rigor of the protocol. Many subjects (n = 17) were eliminated from the initial sample (n = 42) because all data following the use of sedatives or epidural was eliminated, and because subjects needed to record at least two of the four stages of labor and delivery. This loss of subjects had been anticipated considering the popularity of pharmacotherapy. Fortunately, an average of 15 measurements or values were registered per subject, compensating for the size of the sample. As the loss of subjects was identical in both groups, the impact of this variable was limited, as the remaining subjects were evenly distributed in both groups. The number of women eliminated for seeking pharmacological pain relief was identical in both groups (n = 4). One may hypothesize that no matter what non-pharmacological method one chooses to use to cope with pain, a certain number of women will still prefer other types of support. Another factor which may have impacted the results of the study is not having accounted for some physical variances that have been known to influence pain, such as the weights of the mother and the child.Citation38 Although none of the participating subjects were part of midwifery continuity of care programs, this multicenter case control study, with so few women, could have introduced unaccounted-for variables, such as different models of care in the different hospitals.
Even though subjects were unaware of the purpose of the study, a potential placebo effect related to positive expectations could have occurred within the group that undertook BM training, because participants were told throughout their classes that the purpose of the method was to reduce pain in labor. Discussing pain, and building tools to cope with pain that are conducive to positive expectations is part of the Bonapace Method, as with other educational methods.
Recommendations
Randomized controlled trials should be conducted in order to determine the efficacy of this childbirth-training program, evaluating not only pain perception but also obstetric interventions, maternal, and neonatal outcomes. In order to better understand the impact of the three endogenous pain-modulating mechanisms and the role of each component of pain, a meta-analysis of non-pharmacological studies should pool together sufficient quality data to determine what works best. Based on the results of this study, which includes techniques from all three endogenous mechanisms that modulate both components of pain, it can be hypothesized that training programs should teach expecting parents techniques that modulate both components of pain. The implications of this study are important, considering the rising levels of medical intervention associated with pharmacological pain management techniques.Citation11
The use of a structured pain control program based on neurophysiological mechanisms shows an important effect on reducing pain during labor.
Acknowledgments
We wish to thank the nurses of the Hôpital Hôtel-Dieu d’Amos, Sister Claire Brisebois, and Paule Julien for their valuable collaboration in the collection of data, and Clare Lord for her invaluable revision of the final draft. Serge Marchand is supported by research grants from the Candadian Institute of Health Research and is a supported member of the Centre de Recherche Clinique Étienne le Bel. Julie Bonapace is the author of a book and training material on the Bonapace Method.
Disclosure
The authors report no conflicts of interest in this work.
References
- IASP Task Force on Taxonomy, Classification of Chronic Pain2nd edMerskeyHBogdukNSeattle, WAIASP Press1994
- MelzackRTaenzerPFeldmanPKinchRALabour Is still painful after prepared childbirth trainingCan Med Assoc J19811253573637272887
- PriceDDHarkinsSWBakerCSensory-affective relationships among different types of clinical and experimental painPain1987282973072952934
- BonicaJLabour painWallPDMelzackRTextbook of Pain3rd edNew YorkChurchill Livingstone1994615641
- BrownridgePThe nature and consequences of childbirth painEur J Obstet Gynecol Reprod Biol199559S9S157556828
- CollisREDaviesDWAvelingWRandomised comparison of combined spinal-epidural and standard epidural analgesia in labourLancet19943458962141314167760614
- McCoolWPackmanJZwerlingAObstetric anesthesia: Changes and choicesJ Midwifery Womens Health20044950551315544979
- LiebermanEO’DonoghueCUnintended effects of epidural analgesia during labor: A systematic reviewAm J Obstet Gynecol2002186S31S6812011872
- LucasMSharmaSMcIntireDA randomized trial of labor analgesia in women with pregnancy-induced hypertensionAm J Obstet Gynecol2001185S970S975
- WlodyDComplications of regional anesthesia in obstetricsClin Obstet Gynecol20034666767812972748
- Anim-SomuahMSmythRMDJonesLEpidural versus non-epidural or no analgesia in labourCochrane Database Syst Rev201112CD00033122161362
- GagnonAJSandallJIndividual or group antenatal education for childbirth or parenthood, or bothCochrane Database Syst Rev20073CD00286917636711
- Davenport-SlackBBoylanCHPsychological correlates of childbirth painPsychosomatics197436215223
- JavertCTHardyJDMeasurement of pain intensity in labor and its physiologic, neurobiologic, and pharmacologic implicationsAm J Obstet Gynecol19506055256314771145
- Bergstöm-WhalenMBEfficacy of education for childbirthJ Psychosom Res19637131146
- CattaniPSinaPPiccolboniGDell’AngeloMZanarottiREffect of autogenic respiratory training on labor pain. Use of the Vao Na AlgometersMinerva Ginecol1991435255281784410
- IpWYTangCSGogginsWBAn educational intervention to improve women’s ability to cope with childbirthJ Clin Nurs2009182125213519583645
- MelzackRLabour pain as a model of acute painPain1993531171208336982
- MarchandSBushnellMCMolina-NegroPMartinezSNDuncanGHThe effects of dorsal column stimulation on measures of clinical and experimental pain in manPain1991452492571876434
- NettelbladtPFagerströmCFUddenbergNThe significance of reported childbirth painJ Psychosom Res197620215221985618
- MarchandSThe Phenomenon of PainSeattle, WAIASP Press2012
- SmithCALevettKMCollinsCTCrowtherCARelaxation techniques for pain management in labourCochrane Database Syst Rev201112CD00951422161453
- ChalayePGoffauxPLafrenayeSMarchandSRespiratory effects on experimental heat pain and cardiac activityPain Medicine2009101334134019671085
- MelzackRWallPDPain mechanisms: a new theoryScience19651509719795320816
- TsaoJCEffectiveness of massage therapy for chronic, non-malignant pain: a reviewEvid Based Complement Alternat Med2007416517917549233
- SmithCALevettKMCollinsCTJonesLMassage, reflexology and other manual methods for pain management in labourCochrane Database Syst Rev20122CD00929022336862
- JonesLOthmanMDowswellTPain management for women in labour: an overview of systematic reviewsCochrane Database Syst Rev20123CD00923422419342
- LawrenceALewisLHofmeyrGJDowswellTStylesCMaternal positions and mobility during first stage labourCochrane Database Syst Rev20092CD00393419370591
- Le BarsDDickensonAHBessonJMDiffuse noxious inhibitory controls (DNIC). I. Effects on dorsal horn convergent neurones in the ratPain19796283304460935
- Le BarsDDickensonAHBessonJMDiffuse noxious inhibitory controls (DNIC). II. Lack of effect on non-convergent neurones, dupraspinal involvement and theoretical implicationsPain19796305327460936
- SmithCACollinsCTCynaAMCrowtherCAComplementary and alternative therapies for pain management in labourCochrane Database Syst Rev20109CD003521
- BingZVillanuevaLLe BarsDAcupuncture and diffuse noxious inhibitory controls: naloxone-reversible depression of activities of trigeminal convergent neuronsNeuroscience1990378098182247225
- HashimotoTAikawaSManual acupuncture and its central mechanisms: involvement of propriospinal and descending pain inhibitory systemJ Jpn Soc Acupunct199444181190
- HjelmstedtAShenoySTStener-VictorinEAcupressure to reduce labor pain: a randomized controlled trialActa Obstet Gynecol Scandinavica2010891114531459
- SmithCACollinsCTCrowtherCALevettKMAcupuncture or acupressure for pain management in labourCochrane Database Syst Rev20117CD00923221735441
- BonapaceJAccoucher sans stress avec la méthode Bonapace. [Childbirth without stress with the Bonapace Method]MontréalEditions de l’Homme2009 French
- CunninghamFGWilliams Obstetrics19th edNorwalk, CTAppleton Lange1993
- MelzackRThe myth of painless childbirth (the John J Bonica lecture)Pain1984193213376384895
- FriedmanEANormal laborFriedmanEALaborClinical Evaluation and Management2nd edNew YorkAppleton-Century-Crofts1978158
- MelzackRKinchRDobkinPLebrunMTaenzerPSeverity of labor pain: influence of physical as well as psychologic variablesCan Med Assoc J19841305795846697268
- HodnettEDGatesSHofmeyrGJSakalaCWestonJContinuous support for women during childbirthCochrane Database Syst Rev20112CD00376621328263
- ChuntharapatSPetpichetchianWHatthakitUYoga during pregnancy: effects on maternal comfort, labor pain and birth outcomesComplement Ther Clin Pract20081410511518396254
- NarendranSNagarathnaRNarendranVGunasheelaSNagendraHREfficacy of yoga on pregnancy outcomeJ Altern Complement Med200511223724415865489
- Artieta-PinedoIPaz-PascualCGrandesGThe benefits of antenatal education for the childbirth process in SpainNurs Res20105919420421842
- BergströmMKielerHWaldenströmUEffects of natural childbirth preparation versus standard antenatal education on epidural rates, experience of childbirth and parental stress in mothers and fathers: a randomised controlled multicentre trialBJOG20091161167117619538406
- MaimburgRDVaethMDürrJHvidmanLOlsenJRandomised trial of structured antenatal training sessions to improve the birth processBJOG201011792192820536430
- EntwistleDRDoeringSGThe First Birth. A Family Turning PointBaltimore, MAJohns Hopkins University Press1981
