Abstract
Neuromuscular electrical stimulation (NMES), specifically functional electrical stimulation (FES) that compensates for voluntary motion, and therapeutic electrical stimulation (TES) aimed at muscle strengthening and recovery from paralysis are widely used in stroke rehabilitation. The electrical stimulation of muscle contraction should be synchronized with intended motion to restore paralysis. Therefore, NMES devices, which monitor electromyogram (EMG) or electroencephalogram (EEG) changes with motor intention and use them as a trigger, have been developed. Devices that modify the current intensity of NMES, based on EMG or EEG, have also been proposed. Given the diversity in devices and stimulation methods of NMES, the aim of the current review was to introduce some commercial FES and TES devices and application methods, which depend on the condition of the patient with stroke, including the degree of paralysis.
Introduction
The clinical application of electrical stimulation is historical, with live torpedo fish being used to deliver electric current for pain treatment ~2,000 years ago. In more recent years, several implanted and non-implanted electrical stimulation devices have been widely used in a clinical setting. Examples of implanted devices include the following: artificial cardiac pacemakers, which are placed under the skin in the chest or belly to electrically stimulate cardiac muscle to control heart rhythms;Citation1 cochlear implants placed in the inner ear, which electrically stimulate the auditory nerve corresponding to the frequency of the sound;Citation2 deep brain stimulation, which delivers electrical impulses to specific brain areas to reduce tremor in Parkinson’s or other movement disorders;Citation3,Citation4 spinal cord stimulators, which send a mild electric current to nerves in the spinal cord to mask a pain signal;Citation5 and non-implanted devices, including transcutaneous electrical nerve stimulation (TENS) and transcranial direct current stimulation (tDCS), which deliver electrical stimulation via electrode pads on the skin and scalp, respectively. For TENS, electrodes are often placed on the area of skin where the pain is present, and a low-voltage electrical current is delivered to treat a variety of painful conditions.Citation6,Citation7 tDCS is a noninvasive brain stimulation technique in which a weak direct current (1–2 mA) is applied from electrodes to the scalp,Citation8 which excites or inhibits cortical excitability,Citation9 depending on the polarity of electrode. In recent years, tDCS has been extensively studied in clinical neuropsychiatry and rehabilitation.Citation10,Citation11
Artificially controlling human muscles or muscle nerves by neuromuscular electrical stimulation (NMES) is widely used in clinical rehabilitation for spinal cord injury and stroke, which often impair upper motor neurons and/or their neuronal pathways to lower motor neurons, consequently leading to paralysis of upper and/or lower limbs. Unilateral paralysis (ie, hemiparesis or hemiplegia) is particularly seen in many patients who survive a stroke. Recovery from the motor impairments may occur over weeks and months. The poststroke motor recovery is complex due to genetic, pathophysiologic, sociodemographic, and clinical factors.Citation12 NMES is one of the therapeutic interventions that has been developed to try to induce the motor recovery.Citation13 NMES can be used to stimulate the neuromuscular activity of the paretic limbs after stroke because normal electrical excitability often remains in lower motor neurons and their innervated muscles. Research on the use of NMES for rehabilitation has been increasing () since 1961, when Liberson et alCitation14 stimulated the tibialis anterior to dorsiflex the ankle joint of patients with hemiplegia.
Figure 1 Results of a PubMed (service of the US National Library of Medicine [https://www.ncbi.nlm.nih.gov/pubmed/]) search for (“electrical stimulation” OR “electrical muscle stimulation” OR “electrical nerve stimulation” OR FES OR NMES) AND (stroke OR “cerebrovascular disease” OR hemiplegic OR hemiparetic OR hemiparesis OR paralysis OR rehabilitation).
![Figure 1 Results of a PubMed (service of the US National Library of Medicine [https://www.ncbi.nlm.nih.gov/pubmed/]) search for (“electrical stimulation” OR “electrical muscle stimulation” OR “electrical nerve stimulation” OR FES OR NMES) AND (stroke OR “cerebrovascular disease” OR hemiplegic OR hemiparetic OR hemiparesis OR paralysis OR rehabilitation).](/cms/asset/f70414b5-4b11-4aac-8cbd-c21948ed9d00/dmde_a_123464_f0001_b.jpg)
The purpose of NMES can be broadly classified into the following categories in general: functional electrical stimulation (FES), which, in a narrow sense, compensates for voluntary motion, and therapeutic electrical stimulationCitation15 (TES), with the aim of muscle strengthening or recovery from paralysis. Although there are both implantedCitation16–Citation18 and non-implantedCitation19 NMES devices, this review mainly focused on the non-implanted type that uses surface electrodes for stimulation and is often applied for stroke rehabilitation.
Wave forms for NMES
In NMES therapy, various stimulation parameters are used in the devices. Generally, as shown in , the waveform of the stimulation pulse may be monophasic, biphasic, and burst (polyphasic) waves. The pulse width is usually 150–300 μs, while the current intensity is dozens of milliampere. The pulse waveforms can be subdivided into rectangular waves, sine waves, etc. Biphasic waves, in contrast, can be further distinguished as symmetrical/asymmetrical or balanced/imbalanced ().
Figure 2 Parameters of NMES.
Abbreviation: NMES, neuromuscular electrical stimulation.
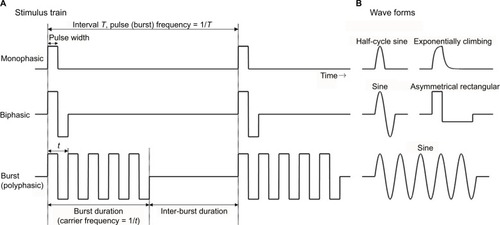
Muscle torque, fatigue, or pain induced by NMES depends on the wave parameters. Pain depends on the total amount of electrical charge delivered to the tissue.Citation20 Petrofsky et alCitation21 showed that sine wave stimulation produced greater muscle strength, with less pain, in comparison with rectangular or polyphasic waves. Laufer et alCitation22 also reported that monophasic and biphasic waveforms are more advantageous than burst waveforms and argued that the electrically induced fatigue is affected by the number of cycles per second, rather than the number of bursts per second.Citation23 Therefore, monophasic or biphasic waveforms, rather than burst waveforms, may be more suitable for the clinical use of NMES. In fact, many NMES devices for stroke rehabilitation use the former.
Functional electrical stimulation
Although FES is a method that compensates for voluntary motion in a narrow sense, it cannot strictly be distinguished from TES. Many studies have demonstrated that rehabilitation training with FES improves activity of patients with stroke.Citation24 The WalkAide system (Innovative Neurotronics, Inc., Austin, TX, USA)Citation25 and NESS L300 (Bioness Inc., Valencia, CA, USA)Citation26 are examples of typical commercial FES devices that are available for paralyzed lower limbs after stroke ( and , respectively). These devices are commonly used against forefoot dropping, which is a gait abnormality that occurs due to paralysis of the muscles of the lower leg (decreased ankle dorsiflexion). The drop foot during the swing phase (non-weight-bearing phase) of gait is one of the risk factors for a fall.Citation27 In these devices, surface electrodes for stimulation are fixed by a cuff to the leg below the knee. Electrical stimulation is delivered during the swing phase of gait, producing ankle dorsiflexion to keep leg clearance. The heel contact and off (stance and swing phases) are detected by a tilt sensor placed with the knee cuff (WalkAide) or by a pressure sensor placed under the insole of shoe to determine stimulation periods (WalkAide and NESS L300).
Figure 3 WalkAide system.

Figure 4 Commercial FES devices.
Abbreviation: FES, functional electrical stimulation.

Since NESS H200 (Bioness Inc.)Citation28,Citation29 is the only commercially available FES device for the upper limb and hand (), more robust and versatile devices are required for a wider group of people.Citation30 Since hand or upper limb motion is more diverse in comparison to lower limb motion, the electrical stimulation system associated with stimulating the former is also complicated. The NESS H200 has five electrodes, which stimulate the five muscle groups of forearm and hand (ie, the extensor digitorum, extensor pollicis brevis, flexor digitorum superficialis, flexor pollicis longus, and thenar muscles) and implement both key gripping and palmar grasping.
Therapeutic electrical stimulation
Although some parameters of electrical stimulation (ie, stimulus position, stimulus intensity, pulse width, etc.) are adjusted according to the motion or condition of patient during FES, the stimulation methods for TES are even more varied.
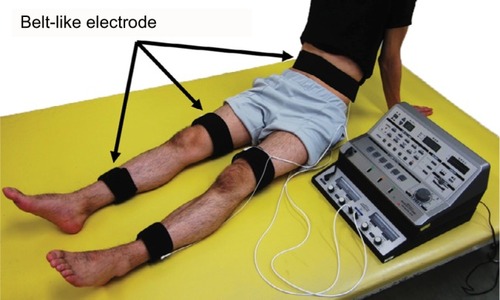
Patients who have survived a stroke sometimes undergo electrical stimulation for muscle strengthening, although its use is not particular to stroke rehabilitation. In general, NMES often stimulates specific muscles, but in the case of muscle strengthening in stroke rehabilitation, multiple muscles, including those on the non-paralyzed side, are stimulated to enhance muscle strength. The reason for muscle strengthening in the non-paralyzed limb is to improve muscle weakness due to hospitalization (for example, knee extension force of the unaffected side decreases by ~30% on the seventh day after the onset of stroke)Citation31 or to acquire the compensatory strategies using the non-paralyzed limb. The belt electrode skeletal muscle electrical stimulation (B-SES) was also recently developed (Auto Tens Pro; Hormer Ion Co. Ltd., Tokyo, Japan) for muscle strengthening (). For the B-SES, belt-like electrodes are wrapped around the waist, both knees, and both ankles to contract all lower limb skeletal muscles simultaneously.Citation32 Since it is desirable to induce stronger muscle contraction to obtain sufficient muscle strengthening effect, the stimulus intensity is set to the limit that patients can endure. Therefore, B-SES adopts the exponentially climbing wave form shown in , which can produce greater muscle strength with less pain.Citation33
Figure 5 B-SES by Auto Tens Pro (Hormer Ion Co. Ltd.).
Abbreviation: B-SES, belt electrode skeletal muscle electrical stimulation.
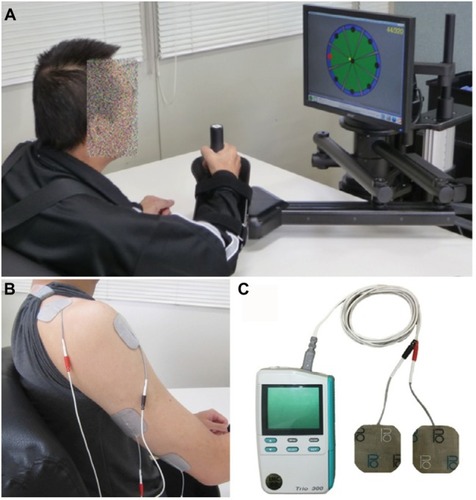
In contrast, weak current NMES, which is approximately at sensory threshold or below motor threshold, has also been proposed as a possible supplemental therapy to facilitate motor function in patients with stroke.Citation34 This is based on reports that somatosensory input enhances corticomotoneuronal excitability to the stimulated body parts.Citation35,Citation36 In this approach, rather than being used in isolation, NMES is applied in combination with rehabilitation training. The advantages of this approach are high safety, low pain, and high usability for various types of rehabilitation, including robot training ().Citation37
Figure 6 Robotic training for affected upper limb using MIT-Manus/InMotion2 system (Interactive Motion Technologies, Inc., Cambridge, MA, USA) (A) combined with NMES at sub-motor threshold intensity.Citation37 NMES was delivered to the anterior deltoid and triceps muscles (B) using the Trio300 system (Ito Co. Ltd., Tokyo, Japan). (C) These devices are currently used in Fujita Health University Nanakuri Memorial Hospital.
In the abovementioned TES approaches, the electrical stimulation is applied continuously and passively. However, for the motor recovery of paretic limbs after stroke, it is more common to perform NMES to encourage muscle contraction for an intended motion or to perform reciprocal NMES with agonists and antagonists. Rosewilliam et alCitation38 recruited patients with stroke with no upper limb function and demonstrated that repetitive NMES for 30 minutes (on and off periods = 15 s), which was applied twice in a working day for 6 weeks, to produce repetitive wrist extension, improved the wrist function of patients. Wu et alCitation39 developed bilateral arm training combined with NMES for the triceps brachii muscle and anterior deltoid muscle in the affected arm. During the training, patients were required to move both their paralyzed and non-paralyzed arms simultaneously in the same way, and the NMES was triggered by the difference in movement of both arms to assist the motion. Osu et alCitation40 used a surface electromyogram (EMG) of the unaffected hand as a clue for electrical stimulation of the paralyzed hand in a bilateral simultaneous motion. The EMG recorded by surface electrodes on the skin above skeletal muscle tissue is a common noninvasive method to assess the electrical activity that initiates muscle contraction and produces a physical force.Citation41,Citation42 For reciprocal NMES, alternate stimulation of dorsiflexors and plantarflexors according to the timing of gait improved the walking ability of patients with stroke.Citation43,Citation44 This therapeutic approach is similar to that of FES described earlier, which is triggered depending on the phase of gait. Essentially, there is little distinction between “TES” and “FES” in stroke rehabilitation.
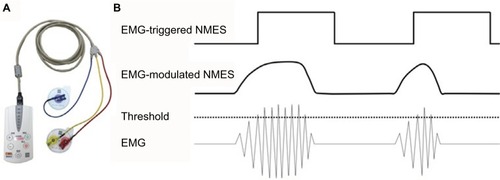
Since adjusting the NMES to the timing of motion means synchronizing it to motor intention, EMG-triggered NMES has been developed.Citation45–Citation47 In this system, electrical stimulation is voluntarily triggered by EMG in the affected limb (the residual muscle activity of the paralyzed muscle). In recent years, EMG-triggered NMES has been combined with robot-aided rehabilitation, which has demonstrated improved motor function in patients with stroke.Citation48,Citation49 Furthermore, EMG-modulated NMES devices have also been developed,Citation50–Citation52 which controls not only the timing but also the intensity of electrical stimulation in direct proportion to the amount of residual voluntary EMG. Since MuraokaCitation53 developed the device, where a pair of surface electrodes simultaneously records EMG from a muscle and stimulates the same muscle, EMG-modulated NMES can be applied even to a small muscle, in which it can be challenging to apply separate stimulating and recording electrodes. This NMES device, which is known as the integrated volitional control electrical stimulator (IVES), has been manufactured in Japan since 2008.Citation54 The commercial IVES devices (PAS System and IVES+ System, OG Wellness Technologies Co., Ltd., Okayama, Japan) have two modes, ie, EMG-triggered NMES and EMG-modulated NMES ().
Figure 7 (A) The IVES+ system (OG Wellness Technologies Co., Ltd.) that is currently used in Fujita Health University Nanakuri Memorial Hospital. (B) EMG-triggered and EMG-modulated modes can be used for this device. In the former mode, NMES is applied with a constant current intensity for a fixed time when an EMG that exceeds a predefined threshold is detected. In the latter mode, the intensity of the stimulation current is proportional to the amplitude of EMG.
In more recent years, there has also been an attempt to detect the motor intention using an electroencephalogram (EEG) instead of an EMG. Event-related desynchronization (ERD) and event-related synchronization (ERS), which respectively decrease and increase EEG frequency band power, are used to interpret the dynamics of brain oscillationsCitation55 and are well known to be associated with motor attempt, motor imagery, or voluntary movement.Citation56 A brain–computer interface (BCI) or brain–machine interface (BMI), a direct technological interface between the brain and a computer, based on the ERD and/or the ERS has recently been found to be a new tool to facilitate motor recovery after stroke.Citation57 Clinical reports of stroke rehabilitation using a BCI system to trigger NMES (EEG-triggered NMES) for finger function,Citation58 upperCitation59 and lowerCitation60 limb training, and gait rehabilitationCitation61 have been published. Similar to the EMG-modulated NMES described earlier, an EEG-modulated NMES system has also been reported, which controls the current intensity of the NMES in a stepwise manner according to the appearance or disappearance of ERD.Citation62 Although some of these BCI-NMES studies showed an improvement in paretic limbs of patients with stroke, currently, almost all are case reports or feasibility/safety studies. Thus, larger, controlled studies are warranted to validate the manufacture of commercial devices of EEG-modified NMES.
Conclusion
In stroke rehabilitation, NMES is used not only for muscle strengthening and motor recovery of paralyzed limbs as introduced in this review but also for reducing spasticityCitation63 and improving swallowing function.Citation64 With the development of electronic engineering and clinical neuroscience, the devices and stimulation methods of NMES are diversifying. The application method of NMES differs depending on the condition of the patient with stroke, including the degree of paralysis. For patients with mild paralysis, weak NMES at sensory threshold or below motor threshold, combined with rehabilitation, may promote functional improvement. For moderate paralysis, EMG-triggered/modulated NMES may be a potential rehabilitative treatment option to restore motor function and improve recovery. For severely affected patients in whom surface EMG is not detectable, EEG-triggered NMES may have therapeutic efficacy. Alternatively, in case of patients with severe paresis, in whom there is no motor intent, NMES aimed at muscle strengthening may be required to acquire compensatory movement in the non-paralyzed side.
Although the present review introduced some NMES devices and their clinical application, this was not a systematic review or a meta-analysis. The evidence of the applications of NMES in rehabilitation is still limited.Citation65 In particular, further research on recent new techniques, such as EEG-triggered/modulated NMES, using a controlled design is warranted.Citation66 From the viewpoint of device development, there are many devices in which various stimulation parameters can be set with one device; however, there are few commercial devices that correspond to complicated operations such as hand movements. Further development and evidence-based commercial manufacture of EMG/EEG-triggered/modulated NMES devices are expected in the future.
Disclosure
The authors report no conflicts of interest in this work.
References
- NielsenJCGerdesJCVarmaNInfected cardiac-implantable electronic devices: prevention, diagnosis, and treatmentEur Heart J201536372484249025749852
- RocheJPHansenMROn the horizon: cochlear implant technologyOtolaryngol Clin North Am20154861097111626443490
- LozanoAMGrossREIntroduction to deep brain stimulationNeurosurg Focus201742VideoSuppl2 Intro
- VolkmannJDeep brain stimulation for the treatment of Parkinson’s diseaseJ Clin Neurophysiol200421161715097290
- ForrestDMSpinal cord stimulator therapyJ Perianesth Nurs19961153493528970301
- ClaydonLSChestertonLSBarlasPSimJDose-specific effects of transcutaneous electrical nerve stimulation (TENS) on experimental pain: a systematic reviewClin J Pain201127763564721562411
- DeSantanaJMWalshDMVanceCRakelBASlukaKAEffectiveness of transcutaneous electrical nerve stimulation for treatment of hyperalgesia and painCurr Rheumatol Rep200810649249919007541
- FregniFPascual-LeoneATechnology insight: noninvasive brain stimulation in neurology-perspectives on the therapeutic potential of rTMS and tDCSNat Clin Pract Neurol20073738339317611487
- JacobsonLKoslowskyMLavidorMtDCS polarity effects in motor and cognitive domains: a meta-analytical reviewExp Brain Res2012216111021989847
- ElsnerBKuglerJPohlMMehrholzJTranscranial direct current stimulation (tDCS) for improving activities of daily living, and physical and cognitive functioning, in people after strokeCochrane Database Syst Rev20163CD00964526996760
- BrunoniARNitscheMABologniniNClinical research with transcranial direct current stimulation (tDCS): challenges and future directionsBrain Stimul20125317519522037126
- AlawiehAZhaoJFengWFactors affecting post-stroke motor recovery: implications on neurotherapy after brain injuryBehav Brain ResIn press2016
- LanghornePCouparFPollockAMotor recovery after stroke: a systematic reviewLancet Neurol20098874175419608100
- LibersonWTHolmquestHJScotDDowMFunctional electrotherapy: stimulation of the peroneal nerve synchronized with the swing phase of the gait of hemiplegic patientsArch Phys Med Rehabil19614210110513761879
- de KroonJRvan der LeeJHMJIJLankhorstGJTherapeutic electrical stimulation to improve motor control and functional abilities of the upper extremity after stroke: a systematic reviewClin Rehabil200216435036012061468
- ShimadaYDavisRMatsunagaTElectrical stimulation using implantable radiofrequency microstimulators to relieve pain associated with shoulder subluxation in chronic hemiplegic strokeNeuromodulation20069323423822151712
- MarsolaisEBKobeticRFunctional electrical stimulation for walking in paraplegiaJ Bone Joint Surg Am19876957287333496340
- PeckhamPHKeithMWFreehaferAARestoration of functional control by electrical stimulation in the upper extremity of the quadriplegic patientJ Bone Joint Surg Am19887011441483275671
- BroderickBJBreenPPÓLaighinGElectronic stimulators for surface neural prosthesisJ Automat Contr20081822533
- GracaninFTrnkoczyAOptimal stimulus parameters for minimum pain in the chronic stimulation of innervated muscleArch Phys Med Rehabil19755662432491137479
- PetrofskyJLaymonMProwseMGundaSBattJThe transfer of current through skin and muscle during electrical stimulation with sine, square, Russian and interferential waveformsJ Med Eng Technol200933217018119205995
- LauferYRiesJDLeiningerPMAlonGQuadriceps femoris muscle torques and fatigue generated by neuromuscular electrical stimulation with three different waveformsPhys Ther20018171307131611444994
- LauferYElboimMEffect of burst frequency and duration of kilohertz-frequency alternating currents and of low-frequency pulsed currents on strength of contraction, muscle fatigue, and perceived discomfortPhys Ther200888101167117618703676
- HowlettOALanninNAAdaLMcKinstryCFunctional electrical stimulation improves activity after stroke: a systematic review with meta-analysisArch Phys Med Rehabil201596593494325634620
- EveraertDGSteinRBAbramsGMEffect of a foot-drop stimulator and ankle-foot orthosis on walking performance after stroke: a multicenter randomized controlled trialNeurorehabil Neural Repair201327757959123558080
- van SwigchemRVloothuisJden BoerJWeerdesteynVGeurtsACIs transcutaneous peroneal stimulation beneficial to patients with chronic stroke using an ankle-foot orthosis? A within-subjects study of patients’ satisfaction, walking speed and physical activity levelJ Rehabil Med201042211712120140406
- WeerdesteynVde NietMvan DuijnhovenHJGeurtsACFalls in individuals with strokeJ Rehabil Res Dev20084581195121319235120
- AlonGLevittAFMcCarthyPAFunctional electrical stimulation enhancement of upper extremity functional recovery during stroke rehabilitation: a pilot studyNeurorehabil Neural Repair200721320721517369518
- AlonGSunnerhagenKSGeurtsACOhryAA home-based, self-administered stimulation program to improve selected hand functions of chronic strokeNeuroRehabilitation200318321522514530587
- VenugopalanLTaylorPNCobbJESwainIDUpper limb functional electrical stimulation devices and their man-machine interfacesJ Med Eng Technol201539847147926508077
- HarrisMLPolkeyMIBathPMMoxhamJQuadriceps muscle weakness following acute hemiplegic strokeClin Rehabil200115327428111386397
- NumataHNakaseJInakiAEffects of the belt electrode skeletal muscle electrical stimulation system on lower extremity skeletal muscle activity: evaluation using positron emission tomographyJ Orthop Sci2016211535626755387
- TaninoGTomitaYOrandAEffect of rectangular and exponentially climbing waveforms on knee extension torque during neuromuscular electrical stimulationTechnol Disabil2016284139144
- IkunoKMatsuoAShomotoKSensory electrical stimulation for recovery of hand and arm function in stroke patients: a review of the literatureJ Nov Physiother2012S17
- Kaelin-LangALuftARSawakiLBursteinAHSohnYHCohenLGModulation of human corticomotor excitability by somatosensory inputJ Physiol2002540pt 262363311956348
- HamdySRothwellJCAzizQSinghKDThompsonDGLong-term reorganization of human motor cortex driven by short-term sensory stimulationNat Neurosci199811646810195111
- MiyasakaHOrandAOhnishiHTaninoGTakedaKSonodaSAbility of electrical stimulation therapy to improve the effectiveness of robotic training for paretic upper limbs in patients with strokeMed Eng Phys201638111172117527531071
- RosewilliamSMalhotraSRoffeCJonesPPandyanADCan surface neuromuscular electrical stimulation of the wrist and hand combined with routine therapy facilitate recovery of arm function in patients with stroke?Arch Phys Med Rehabil2012931017151721.e171122676906
- WuFCLinYTKuoTSLuhJJLaiJSClinical effects of combined bilateral arm training with functional electrical stimulation in patients with strokeIEEE Int Conf Rehabil Robot20112011597536722275571
- OsuROtakaYUshibaJA pilot study of contralateral homonymous muscle activity simulated electrical stimulation in chronic hemiplegiaBrain Inj20122691105111222571491
- MerlettiRAventaggiatoMBotterAHolobarAMaratebHVieiraTMAdvances in surface EMG: recent progress in detection and processing techniquesCrit Rev Biomed Eng201038430534521133837
- DieterichAVBotterAVieiraTMSpatial variation and inconsistency between estimates of onset of muscle activation from EMG and ultrasoundSci Rep201774201128176821
- KesarTMPerumalRReismanDSFunctional electrical stimulation of ankle plantarflexor and dorsiflexor muscles: effects on poststroke gaitStroke200940123821382719834018
- EmbreyDGHoltzSLAlonGBrandsmaBAMcCoySWFunctional electrical stimulation to dorsiflexors and plantar flexors during gait to improve walking in adults with chronic hemiplegiaArch Phys Med Rehabil201091568769620434604
- CauraughJLightKKimSThigpenMBehrmanAChronic motor dysfunction after stroke: recovering wrist and finger extension by electromyography-triggered neuromuscular stimulationStroke20003161360136410835457
- KraftGHFittsSSHammondMCTechniques to improve function of the arm and hand in chronic hemiplegiaArch Phys Med Rehabil19927332202271543423
- von LewinskiFHoferSKausJEfficacy of EMG-triggered electrical arm stimulation in chronic hemiparetic stroke patientsRestor Neurol Neurosci200927318919719531874
- HuXLTongKYLiRPost-stroke wrist rehabilitation assisted with an intention-driven functional electrical stimulation (FES)-robot systemIEEE Int Conf Rehabil Robot20112011597542422275625
- HuXLTongRKHoNSXueJJRongWLiLSWrist rehabilitation assisted by an electromyography-driven neuromuscular electrical stimulation robot after strokeNeurorehabil Neural Repair201529876777625549656
- MuraokaYDevelopment of portable EMG-controlled electrical stimulatorProc 41st Soc Insturum Control Engnr Annu Conf2002Osaka, Japan320022007
- MuraokaYTomitaYHondaSTanakaNOkajimaYEMG-controlled hand opening system for hemiplegiaProc 6th Vienna Int Workshop Funct Electrostimulation Basics Technol Appl1998Vienna, Austria255258
- YeomHChangYHAutogenic EMG-controlled functional electrical stimulation for ankle dorsiflexion controlJ Neurosci Methods2010193111812520713086
- MuraokaYDevelopment of an EMG recording device from stimulation electrodes for functional electrical stimulationFront Med Biol Eng200211432333312735431
- MuraokaYTanabeSYamaguchiTTakedaKSpecifications of an electromyogram-driven neuromuscular stimulator for upper limb functional recoveryConf Proc IEEE Eng Med Biol Soc2013201327728024109678
- PfurtschellerGNeuperCFuture prospects of ERD/ERS in the context of brain-computer interface (BCI) developmentsProg Brain Res200615943343717071247
- ParkWKwonGHKimYHLeeJHKimLEEG response varies with lesion location in patients with chronic strokeJ Neuroeng Rehabil2016132126935230
- UshibaJSoekadarSRBrain-machine interfaces for rehabilitation of poststroke hemiplegiaProg Brain Res201622816318327590969
- DalyJJChengRRogersJLitinasKHrovatKDohringMFeasibility of a new application of noninvasive brain computer interface (BCI): a case study of training for recovery of volitional motor control after strokeJ Neurol Phys Ther200933420321120208465
- Marquez-ChinCMarquisAPopovicMREEG-triggered functional electrical stimulation therapy for restoring upper limb function in chronic stroke with severe hemiplegiaCase Rep Neurol Med20162016914621327882256
- DoAHWangPTKingCEAbiriANenadicZBrain-computer interface controlled functional electrical stimulation system for ankle movementJ Neuroeng Rehabil201184921867567
- McCrimmonCMKingCEWangPTCramerSCNenadicZDoAHBrain-controlled functional electrical stimulation therapy for gait rehabilitation after stroke: a safety studyJ Neuroeng Rehabil2015125726162751
- TakahashiMTakedaKOtakaYEvent related desynchronization-modulated functional electrical stimulation system for stroke rehabilitation: a feasibility studyJ Neuroeng Rehabil201295622897888
- SahinNUgurluHAlbayrakIThe efficacy of electrical stimulation in reducing the post-stroke spasticity: a randomized controlled studyDisabil Rehabil201234215115621999668
- PoorjavadMTalebian MoghadamSNakhostin AnsariNDaemiMSurface electrical stimulation for treating swallowing disorders after stroke: a review of the stimulation intensity levels and the electrode placementsStroke Res Treat2014201491805724804147
- SchuhfriedOCrevennaRFialka-MoserVPaternostro-SlugaTNon-invasive neuromuscular electrical stimulation in patients with central nervous system lesions: an educational reviewJ Rehabil Med20124429910522334346
- MukainoMOnoTShindoKEfficacy of brain-computer interface-driven neuromuscular electrical stimulation for chronic paresis after strokeJ Rehabil Med201446437838224590225

