Abstract
Background
Previous research has stressed the importance of early identification and intervention for children with autism spectrum disorders.
Methods
Children who had screened positive for autism at the age of 2.5 years in a general population screening and then received a diagnosis of autism spectrum disorder were enrolled in an intervention program provided by Swedish habilitation services. The following interventions were available: a comprehensive intervention based on Applied Behavior Analysis – Intensive Learning (IL) – in two settings, which included home- and preschool-based (IL Regular) and only home-based (IL Modified) and eclectic interventions.
Results
There was considerable variability in terms of outcome, but intervention group status was not associated with any of the chosen outcome variables.
Conclusion
The main finding was that the type of intervention was not critical for outcome of adaptive or global functioning. The variability in outcome demonstrates the need for continuous assessments and evaluation of the child’s function and behavior throughout the intervention period.
Introduction
Autism spectrum disorder (ASD) comprises conditions characterized by social communication impairments and behavioral restriction,Citation1,Citation2 which appear early in childhood and usually persist during life. There is general agreement that ASD should be identified early so that adequate intervention can be initiated.Citation3–Citation5 In 2007, the American Academy of Pediatrics issued a policy statement strongly recommending universal screening for autism in children by the age of 24 months.Citation6 The rationale of the US Academy of Pediatrics recommendation about general autism screening is to establish a coordinated and effective organization of services. When establishing an ASD diagnosis, medical/genetic counseling, medical management, family support, educational interventions, and guidance to appropriate intervention programs for the child should be initiated.Citation6 However, in a UK statement by the National Health Service, there is a recommendation against universal screening.Citation7 Allaby and SharmaCitation8 discussed many concerns against early screening for ASD; the main argument being that it is still unknown if interventions after early screening lead to significant improvements later in childhood, or greater independence and improved vocational and social functioning in adulthood. In addition, the U.S. Preventive Services Task ForceCitation9 concludes that there is insufficient evidence to assess the benefits of screening for ASD in children, that evidence is lacking for the population to be screened, and that the balance of benefits and harms cannot be determined.
The most disseminated comprehensive intervention programs for children with autism are based on Applied Behavior Analysis (ABA).Citation10–Citation13 The core elements of ABA include strategies such as discrete trail training, use of 1:1 adult to child interaction, implementation in either home or school settings for a range of 20 to 40 hours/week.Citation14
ABA is a frequently used intervention program within the Swedish Child Habilitation Services. The Early Start Denver Model integrates ABA with developmental and relationship-based approaches for improving cognitive and adaptive behaviorCitation15,Citation16 and emphasizes the role of parents in the intervention program. This model has given important ideas to the Swedish Child Habilitation Services.Citation17 Furthermore, the Picture Exchange Communication System (PECS), based on ABA, as an augmentative communication (ACC) system is frequently used in children with autism.Citation18
Another early intervention program focusing on autism, centered on structured education, is the Treatment and Education of Autistic and related Communication handicapped CHildren subsumed under the TEACCH acronym.Citation19 Up until recently, this was probably the most widely disseminated educational program for children, adolescents, and adults with autism and related social communication disorders.
Due to the heterogeneity of ASDs,Citation20 several factors will affect outcome. Ben-Itzchak et alCitation21 studied an Israeli research cohort of 46 children with ASD – without genetic syndromes and with different cognitive levels – who had received center-based intensive behavioral intervention (ABA) over a period of 2 years. When the impact of baseline cognitive ability on outcome trajectories was assessed, significant gains in adaptive skills were found only in the group of children with ASD and high cognitive scores (DQ ≥70). Also, a Swedish study evaluating the outcome of early intensive behavioral intervention found that the subgroup of ASD without intellectual disability had a better 2-year outcome with regard to adaptive functioning compared to the group with ASD and concomitant intellectual disability.Citation22 There was no association with intervention intensity either in this group or in the group with lower IQ.
Although randomized controlled trials are generally the most optimal method to evaluate treatment effects, there is also a need for outcome studies based on representative samples, studied in naturalistic settings.Citation23,Citation24
The aim of this prospective naturalistic study was to evaluate outcome in terms of adaptive behavior and global functioning. Another aim was to analyze the association with IQ and type of intervention (provided in a naturalistic setting within Child Habilitation Services) in a cohort of children who had been diagnosed with ASD after screening at the age of ~2.5 years and who had received 2 years of one of three different types of intervention.
Material and methods
Study area and original study cohort
The study area was the city of Gothenburg with ~500,000 inhabitants and about 6,000 births per year. Since 2009, an ASD screening program has been implemented at all Children’s Healthcare Centers (CHC) in Gothenburg. The screening takes place at the same time as a speech and language screening at 2.5 years of age.Citation25 Between 2009 and 2011, a total of 134 children younger than 4 years with suspected ASD were referred after such screening to the Child Neuropsychiatric Clinic (CNC) in Gothenburg for further ASD assessment (assessment 1= T1). Parents of 129 (102 boys, 27 girls) of the 134 children provided written informed consent to have their child participate in the assessment program at CNC. In addition to a broad multidisciplinary assessment, including cognitive/intellectual tests,Citation26 they had all been assessed by the Autism Diagnostic Observation Schedule-Generic.Citation27 For 72% of the children (93/129), at least one parent had been interviewed using the Diagnostic Interview for Social and Communication Disorders.Citation28,Citation29 One hundred of the children met criteria for a diagnosis of ASD at T1, and were referred to a habilitation center in Gothenburg for intervention.Citation26 A vast majority of these children received intervention at the habilitation center, either an intensive program, Regular Intensive Learning (Regular IL) or Modified Intensive Learning (Modified IL), or a non-intensive, eclectic program.
Present study group
Out of the 100 children referred to a habilitation center, 71 children (15 girls, 56 boys) had received interventions and participated in a follow-up at CNC after 2 years. Two families had moved from Gothenburg, two families did not take part in any of the intervention programs, five families declined contact with the habilitation center, and 20 families declined the 2-year follow-up at CNC.
No child was excluded from the intervention or follow-up because of low IQ or presence of comorbidities, or the parent(s) speaking another native language other than Swedish. Of the 71 children, 21 had average intellectual functioning (AIF) (IQ ≥85), 20 had borderline intellectual functioning (BIF) (IQ =71–84), and 30 had intellectual developmental disorder (IDD) (IQ ≤70)Citation1,Citation2 according to psychometric test results.Citation30–Citation32
Interventions given at the habilitation center
The habilitation professionals are organized as multidisciplinary teams consisting of several clinical professionals: neuropediatrician, psychologist, social worker, occupational therapist, physiotherapist, speech and language pathologist, nurse, and dietician. All professionals had prior experience working with typically developing children and long experience of working with parents and children with ASD. The teams offer different types and intensities of interventions. All interventions in the study were implemented according to conjoint parent request and professional assessments.
Introduction program for parents
An “introduction program” was offered at the habilitation centers, within 3 months after referral, to all parents with a child diagnosed with ASD. This program included three or four group sessions of 3 hours each. The parents were given information about ASD, the cognitive deficits characterizing ASD, and an overall description of treatment and interventions for children with ASD. Information was also given about social services support that parents could apply for.
Comprehensive programs
The specific comprehensive intervention program, based on ABA, used in the western parts of Sweden was the “Intensive Learning for young children with autism”.Citation33 This manual-based program provides a curriculum of imitation as learning-how-to-learn-skills, social skills, play, communication, language, and academic skills.Citation34 The supervisors are responsible for creating individual plans based on each student’s unique individual needsCitation34 and use written exercises to support parents and preschool teachers. Data collection was made weekly with a view to increase naturalistic training possibilities and the child’s need of support in 1:1 training. Protocols were used to control hours of training, based on individual plans and goals, and defined in collaboration with parents and preschool teachers. The intervention was planned and implemented for 2 years per child. IL was used in two different settings. The first was the regular form, which was implemented for parallel use at home and at the child’s preschool. This program included sessions twice a month with supervisors, and the “1:1 intervention” included 10 hours at home and 15 hours at preschool/week (total 25 hours/week). The second setting was the modified form, which was implemented only at home and offered sessions once a month with supervisors. The “1:1 intervention” included 10 hours at home/week (total 10 hours/week).
Eclectic interventions
All eclectic interventions include strategies that are designated to be used in typical interactions and occur in natural settings, routines, and activities.Citation35 Mandell and StahmerCitation36 drew attention to the need to regard eclectic practice as a systematically determined process based on child and teaching characteristics, and careful, ongoing assessment rather than simply combining multiple methods into one program. The eclectic interventions in this study were planned and evaluated over a 2-year period with parents, and each child was only offered one parent-implemented intervention at the same time. Types of eclectic interventions used were PECSCitation18 and the ComAlong program, which is a Swedish parent-implemented Functional Communication Training,Citation37 using alternative and augmentative communication. Fidelity and implementation of ComAlong were evaluated through videos of the parents’ homework with their children. Another program used was TEACCH.Citation19 This latter program is mainly used for modification or manipulation of the environment to affect the child’s behavior with structured work systems and visual strategies ().
Table 1 Description and content of the intervention programs
The Regular IL group consisted of 31 children (4 girls, 27 boys) with a chronological mean age of 35.2 months and a mean cognitive score of IQ 78.0.
The Modified IL group consisted of 19 children (7 girls, 12 boys) with a chronological mean age of 35.7 months and a mean cognitive score of IQ 69.0.
The Eclectic group consisted of 21 children (4 girls, 17 boys) with a chronological age of 37.4 months and mean cognitive score of IQ 82.0.
All details, such as sex, age, intellectual levels of the children, and parents’ country of birth at T1 are arranged according to the three invention groups in .
Table 2 Three intervention groups in relation to sex, age, and intellectual levels of the children at T1 and parents’ country of birth
Cooperation with preschools
The preschools involved in the study usually had 18–24 children (aged 12–60 months) in each group. Each such group had three preschool teachers. The preschool authorities in Gothenburg decided about the need of assistance from habilitation services for children with developmental disorders, such as ASD.
Follow-up assessments at the clinic
All the children were assessed at CNC once again 2 years after their first assessment with regard to autistic behavior/ASD, intellectual, adaptive, and global functioning. The same tests used at T1 were used and professionals with long experience of assessing children with ASD administrated tests according to standard procedures. All the professionals were blinded to the type of intervention received by the children.
The ASD follow-up assessment encompassed clinically validated instruments: the Diagnostic Interview for Social and Communication Disorders,Citation28,Citation29 the Autism Diagnostic Interview,Citation38 and the Autism Diagnostic Observation Schedule.Citation27 Intellectual level was assessed according to at least one of the following: Griffiths’ test,Citation30 Wechsler Preschool and Primary Scale of Intelligence-III,Citation31 or Merrill–Palmer-Revised Scales of Development.Citation32
Outcome measures
Adaptive functions were measured with the Vineland Adaptive Behavior Scale, Second Edition (VABS-II),Citation39 which is an interview-based evaluation of the child’s adaptive skills. A psychologist conducted this interview with one or both parents. All the results are given as standard scores.
The Children’s Global Assessment Scale (C-GAS)Citation40,Citation41 is a clinical global judgment of the child’s total situation or overall severity of impairment, not just one particular symptom. The scale was originally developed for use in 4- to 20-year-old children and adolescents, but it has since been adapted for younger children by the CNC assessment team.Citation26 This scale used normed scores.
Statistics
The distribution of intellectual levels in the three intervention groups (Regular IL, Modified IL, and Eclectic groups) was examined with chi-square test. As main outcomes measures, adaptive composite score and C-GAS before vs after treatment were used as dependent variables in two separate mixed analysis of variance (ANOVA) and intellectual level as independent variables in the intervention groups.
Ethics
The Regional Ethics Committee of the Medical Faculty, University of Gothenburg, Sweden, approved the study with registration number 494-08. Informed consent was obtained from at least one of the parents or responsible caretaker for each child.
Results
Introduction program to parents
One or both parents of 47 of the 71 children (65%) completed the “introduction program”; 22 of the 31 parents (70%) in the Regular IL group, 11 of the 19 parents (57%) in the Modified IL group, and 14 of the 21 parents (67%) in the Eclectic intervention group participated. This was mainly due to the following reasons: 1) parents having already attended the program with an elder sibling with ASD or 2) parents had chosen to receive individual information about ASD.
IL programs
Fifty children (70%) participated in the IL programs: 31 (44%) in the regular IL and 19 (27%) children in a modified version of IL.
Eclectic interventions
The main types of eclectic programs described were given to 21 children and parents. Most children had been offered more than one intervention (mean [M] 2.76, standard deviation [SD] 1.48): ComAlong (16 children), PECS (four children), and TEACCH-based strategies (ten children). Six children participated in a playgroup, and three children joined a communication and motor group with other children.
Distribution of intellectual levels in the intervention groups
A cross-tabulation between intellectual level at T1 (IDD, BIF, AIF) and intervention (Regular IL, Modified IL, and Eclectic intervention) revealed a significant relation between intellectual level and type of intervention (χ24=11.99, P=0.017). Children with IDD were overrepresented in the Modified IL group (n=12, adjusted standardized residual =2.2), children with BIF were overrepresented in the Regular IL group (n=13, adjusted standardized residual =2.3), and children with AIF were overrepresented in the Eclectic intervention group (n=11, Adjusted standardized residual =2.7) (). The intellectual level/intervention group combination with the least children were BIF/Eclectic intervention and AIF/Modified IL with only three children in each. Combining BIF and AIF into one group to get groups of IDD vs BIF + AIF resulted in a weaker relationship between intellectual level and intervention (χ22=4.67, P=0.097). The largest number of children was in the BIF + AIF/Regular IL combination (n=20) and the smallest number was in the BIF + AIF/Modified IL combination (n=7) and in the IDD/Eclectic combination (n=7).
Outcome of adaptive functioning (VABS composite scores)
Of the 71 children, 64 children had VABS data at both T1 and T2. Despite quite large differences in cell sizes, a 2×2×3 mixed ANOVA with time (before and after intervention; ) as a within-subject factor, intellectual level (IDD vs BIF + AIF) and type of intervention (Regular IL, Modified IL, and Eclectic intervention) as between-subject factors, and adaptive composite score as the dependent variable was performed. Mean adaptive composite scores with 95% confidence intervals for each of the 12 investigated combinations of time × intellectual level × type of intervention are shown in . None of the interventions increased the adaptive composite scores from T1 to T2 more than any other (for the time × type of intervention interaction F2, 58=2.20, P=0.120, η2partial=0.071) nor did the adaptive composite scores increase significantly from T1 to T2 in general (F1, 58<1 for the main effect of time). shows that within each of the two groups of different intellectual level, there is considerable overlap between all confidence intervals. The only effect that became significant was the main effect of intellectual level (F1, 58=11.86, P=0.001, η2partial=0.170). Children with BIF or AIF had significantly higher adaptive composite scores compared to children with IDD (M =78.08, SD =8.07 for children with BIF or AIF vs M =69.63, SD =9.79 for children with IDD; ).
Figure 1 95% confidence intervals for the mean change in VABS composite scores between T1 and T2 for the three intervention groups and for the two cognitive levels, respectively.
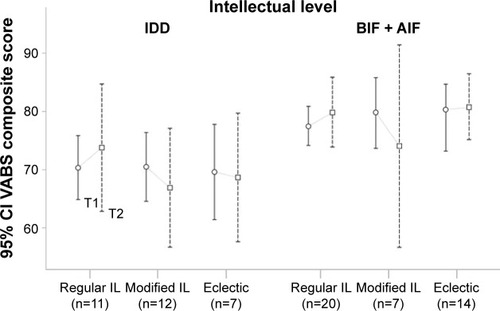
Variance of adaptive functioning (VABS composite scores)
The mean of adaptive composite scores did not change after intervention, but the variance in variables did; as can be seen in , all confidence intervals are larger at T2 than at T1. This was confirmed by Levene’s test for equality of variances showing a significant increase of variance in adaptive composite scores after intervention: F1,133=19.25, P<0.001, SDT1 =8.49, SDT2 =14.00.
Outcome of global functioning (C-GAS)
A 2×2×3 mixed ANOVA with time (before and after intervention) as a within-subject factor, intellectual level (IDD vs BIF + AIF) and type of intervention (Regular IL, Modified IL, and Eclectic intervention) as between-subject factors, and C-GAS score as the dependent variable was performed. Mean C-GAS with 95% confidence intervals for each of the 12 investigated combinations of time × intellectual level × type of intervention is shown in . A main effect of time (F1, 65=4.00, P=0.050, η2partial=0.058) showed that C-GAS in the children in general increased from T1 (M =40.04, SD =9.31) to T2 (M =43.66, SD =12.10). As can be seen in , with the exception of children in the Modified IL group with BIF or AIF, for all three interventions and both intellectual levels, C-GAS increased in the children from T1 to T2. There was, however, no time × type of intervention interaction (F2, 65<1); so, there was no evidence for any particular intervention to have increased C-GAS than the rest of the intervention. Finally, there was a main effect of intellectual level. The children with BIF or AIF (M =45.18, SD =6.98) had significantly higher score on C-GAS than the children with IDD (M =37.30, SD =10.21; F1,65=10.01, P=0.002, η2partial=0.133; ).
Figure 2 95% confidence intervals for the mean change in Global functioning scores between T1 and T2 for the three intervention groups and for the two cognitive levels, respectively.
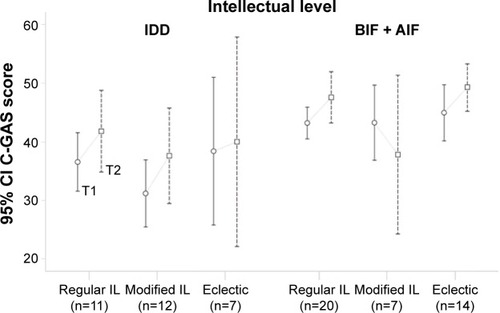
Variance of global functioning (C-GAS)
As for the adaptive composite scores, the variance of the C-GAS scores increased from T1 to T2 (). However, the increase was not significant, according to Levene’s test for equality of variances (F1, 140=12.85, P=0.094, SDT1 =9.31, SDT2 =12.10).
ASD diagnostic stability between T1 and T2
Five of the 71 children (7%) no longer met criteria for ASD at T2. Three of these children were in the Regular IL group and one child each in the two other groups.
Discussion
All the children in the present study had screened positive for ASD in a general population surveillance program at the age of ~2.5 years, and the study group can be considered representative of children with an early diagnosis of ASD. The study had the advantages of ecological validityCitation23 and consisted of the typical clinical process where cases referred from CHC had a comprehensive assessment and had been offered intervention within a short period from their first visit to the habilitation center.
The main finding of this study was that the type of intervention was not critical for outcome of adaptive and global functioning according to the results of Vineland adaptive composite score and C-GAS. Thus, treatment based on ABA did not differ from other types of interventions provided by the habilitation center or preschool. This is in accordance with the finding from a previous Swedish study, ie, type and intensity of intervention were not decisive for adaptive functioning outcome.Citation22 However, this is somewhat in contrast to a review by Leaf et alCitation34 highlighting the effects of early intensive behavioral intervention with regard to meaningful outcomes.
Our results differ from studies by Howard et alCitation42 comparing early ABA and eclectic interventions, reporting ABA to produce substantial improvements in young children with autism compared to common eclectic interventions, even when intensive. However, our findings accord with conclusions put forward by Odom et al in their review.Citation43 They reported a comparison of intensive behavioral treatment programs with eclectic interventions and concluded that eclectic programs had a positive impact on development, learning, and life outcomes in children and youth with autism when being well implemented. The recent large systematic review, including 65 unique studies of behavioral intervention for children with ASD, by Weitlauf et alCitation44 summarized that a growing evidence base suggests that behavioral interventions are associated with some positive outcomes in children with ASD; however, they also suggested that there is a need for studies of interventions across settings and with continued improvements in methodological rigor. The Cochrane report by Reichow et alCitation14 on early intensive behavioral intervention for young children with ASD emphasized the importance of different designs when studying outcomes, and that randomized controlled trials may not always be the optimal, or only, design (also refer Fernell et alCitation24 for further details).
ASDs are complex and heterogeneous disorders and in the majority of children other coexisting developmental disorders are present, ie, “autism plus”,Citation45 and sometimes these disorders are of greater importance for prognosis than the ASD per se. This means that outcome will be dependent on the total clinical presentation, including intellectual level,Citation21,Citation46,Citation47 and on the underlying medical etiology. The diagnostic complexities were discussed by Volkmar and ReichowCitation48 who emphasized that even though the evidence-based research on treatment has increased in this young age group, the state of knowledge is limited.
Although the mean adaptive composite score did not change significantly between T1 and T2, the variance increased significantly. This probably reflects that gain and loss of adaptive skills varied considerably between children at the follow-up. This finding underscores the need for regular monitoring of the child’s functioning and developmental progress/no progress during the intervention period and the necessity to consider a change or modification of the program in use.
Five of the children (7% of the total group) no longer met criteria for ASD at the 2-year-follow-up. However, it is important to note that these children were not necessarily less impaired than those who still met such criteria.Citation49 To minimize the stress of parents and children, it would be preferable to give children with developmental disorder access to clinical support for long periods regardless of diagnosis affiliation.
There are considerable clinical experiences and research supporting the importance of early identification, information to parents and preschool staff, and the need for appropriate interventions in all children with ASD to provide support to children and families, ie, an autism-friendly environment.Citation50,Citation51
In our original cohort of children assessed at CNC after their 2.5-year screening at CHC, the group of children not meeting full criteria for ASD, but who had other Early Symptomatic Syndromes Eliciting Neurodevelopmental Clinical Examinations problems,Citation52 did not get access to habilitation services. These children have also been followed up clinically and a substantial number have been found to meet ASD criteria at their T2 assessment (data will be detailed in a forthcoming study). This highlights the importance of providing all children with developmental disorders/problems/Early Symptomatic Syndromes Eliciting Neurodevelopmental Clinical Examinations problems with targeted interventions by a multi-professional team, along with clinical and medical follow-up, first of all to school age but also into school age.
Strengths and limitations
The strengths of this study lie in the representativeness of the sample that was not selected, and that the study was conducted in a naturalistic setting. Moreover, all the children were assessed by the same research team using the same test methods at both T1 and T2, and the research group was blinded to the type of intervention given within the habilitation services. The limitations are mainly due to the relatively small intervention groups, attrition, and some parents declining intervention from habilitation services and/or declining the follow-up assessment. Other limitations are that the children were not randomized to the type of intervention, but the intervention was implemented according to clinical considerations and to parents’ and professionals’ assessment of the child’s needs. Moreover, the therapists, ie, licensed child psychologists and licensed speech and language pathologists at the habilitation centers, provided interventions in a naturalistic clinical setting and there was no procedure in place to specifically assess treatment integrity.
Conclusion
The present study of children, diagnosed with ASD after screening at the age of 2.5 years and assessed before and after intervention, showed a wide variability in terms of outcomes of adaptive and global functioning. Intervention group status was not associated with any of the chosen outcome variables. The variability in outcomes demonstrates the need for continuous assessments and evaluation of the child’s function and behavior throughout the intervention period, and that programs and methods may need modification.
Acknowledgments
The authors are grateful to the children and their parents for participating in the study. They are also indebted to the colleagues at CNC and Health & Habilitation, Gothenburg, Sweden, for their help in making the study possible. The study received financial support from The Health & Medical Care Committee of the Regional Executive Board, Region Västra Götaland (BSJ).
Disclosure
The authors report no conflicts of interest in this work.
References
- American Psychiatric Association (APA)Diagnostic and Statistical Manual of Mental Disorders4th edWashington (DC)American Psychiatric Association2000
- American Psychiatric Association (APA)Diagnostic and Statistical Manual of Mental Disorders5th edWashington (DC)American Psychiatric Association2013
- EikesethSOutcome of comprehensive psycho-educational interventions for young children with autismRes Dev Disabil200930115817818385012
- FernellEErikssonMAGillbergCEarly diagnosis of autism and impact on prognosis: a narrative reviewClin Epidemiol20135334323459124
- WebbSJJonesEJKellyJDawsonGThe motivation for very early intervention for infants at high risk for autism spectrum disordersInt J Speech Lang Pathol2014161364224410019
- JohnsonCPMyersSMAmerican Academy of Pediatrics Council on Children With DisabilitiesIdentification and evaluation of children with autism spectrum disordersPediatrics200712051183121517967920
- The UK NSC recommendation on Autism screening in children, 2012 Available from: http://www.screening.nhs.uk/autismAccessed March 1, 2016
- AllabyMSharmaMScreening for autism spectrum disorders in children below the age of 5 yearsA Draft Report for the UK National Screening CommitteeSolutions for Public Health, NHS2011
- Autism Spectrum Disorder in Young Children: ScreeningU.S Preventive Services Task Force2016 Available from: http://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/autism-spectrum-disorder-in-young-children-screening?ds=1&s=autism%20spectrum%20disorder%20in%20young%20children%20screeningAccessed March 1, 2016
- MauriceCGreenGLuceSCBehavioural Intervention for Young Children With Autism: A Manual for Parents and ProfessionalsAustin (TX)Pro-Ed1996
- LeafRMcEachinJA Work in ProgressNew York (NY)DRL Books1999
- FovelJTThe ABA Program Companion: Organizing Quality Programs for Children With Autism and PDDNew YorkDRL Books2002
- LovaasOITeaching Individuals With Developmental Delays; Basic Intervention TechniquesAustin (TX)PRO-ED2002
- ReichowBBartonEEBoydBAHumeKEarly intensive behavioral intervention (EIBI) for young children with autism spectrum disorders (ASD)Cochrane Database Syst Rev201210CD00926023076956
- VismaraLAColombiCRogersSCan one hour per week therapy lead to lasting changes in young children with autism?Autism20091319311519176579
- DawsonGRogersSMunsonJRandomized, controlled trial of intervention for toddlers with autism: the Early Start Denver ModelPediatrics20101251e17e2319948568
- Mångsidiga intensiva insatser för barn med autism i förskoleåldern, 2012 [Interventions for children with autism in the preschool age] Available from: http://www.habiliteringschefer.se/ebh/autism/autism.htmlAccessed March 1, 2016 Swedish
- FrostLBondyAThe Picture Exchange Communication System training manual2nd edNewark (DE)Pyramid Educational Products2002
- MesibovGBSheaVThe TEACCH program in the era of evidence-based practiceJ Autism Dev Disord201040557057919937103
- ColemanMGillbergCThe AutismsOxfordOxford University Press2012
- Ben-ItzchakEWatsonLRZachorDACognitive ability is associated with different outcome trajectories in autism spectrum disordersJ Autism Dev Disord20144492221222924710810
- FernellEHedvallÅWesterlundJEarly intervention in 208 Swedish preschoolers with autism spectrum disorder. A prospective naturalistic studyRes Dev Disabil20113262092210121985993
- SchmucklerMAWhat is ecological validity? A dimensional analysisInfancy20012419436
- FernellEWilsonPHadjikhaniNScreening, intervention and outcome in autism and other developmental disorders: the role of randomized controlled trialsJ Autism Dev Disord20144482074207624554162
- NygrenGSandbergEGillstedtFEkerothGArvidssonTGillbergCA new screening programme for autism in a general population of Swedish toddlersRes Dev Disabil20123341200121022502846
- KantzerAKFernellEGillbergCMiniscalcoCAutism in community pre-schoolers: developmental profilesRes Dev Disabil20133492900290823816626
- LordCRisiSLambrechtLThe Autism Diagnostic Observation Schedule-Generic: a standard measure of social and communication deficits associated with the spectrum of autismJ Autism Dev Disord200030320522311055457
- WingLLeekamSRLibbySJGouldJLarcombeMThe Diagnostic Interview for Social and Communication Disorders: background, inter-rater reliability and clinical useJ Child Psychol Psychiatry200243330732511944874
- NygrenGHagbergBBillstedtESkoglundAGillbergCJohanssonMThe Swedish version of the Diagnostic Interview for Social and Communication Disorders (DISCO-10). Psychometric propertiesJ Autism Dev Disord200939573074119148741
- Alin-ÅkermanBNordbergLGriffiths’ Developmental Scales I and IIStockholmHogrefe Psykologiförlaget AB1980
- WechslerDWechsler Preschool and Primary Scale of Intelligence, revised, Swedish versionStockholmHogrefe Psykologiförlaget AB2004
- RoidGHSampersJLMerrill-Palmer Revised Scales of Development. Swedish versionStockholmHogrefe Psykologiförlaget AB2005
- Spjut JanssonBLindahlUNilsson RutbergMManual for Intensivin-lärning för små barn med autism [Manual for Intensive learning for young children with autism]GöteborgHabilitering & Hälsa2011 Swedish
- LeafJBLeafRMcEachinJApplied behaviour analyses is a science and, therefore, progressiveJ Autism Dev Disord201646272073126373767
- OdomSLCollet-KlingenbergLRogersSJHattonDDEvidence-based practices in interventions for children and youth with autism spectrum disordersPrev Sch Fail2010544275282
- MandellDSStahmerACState infant/toddler program policies for eligibility and services provision for young children with autismAdm Policy Ment Health2007341293716758329
- ThunbergGCarlstrandAClaessonBRensfeldt FlinkAKomIgång – en föräldrakurs om kommunikation och kommunikationsstöd. Kursbok [GetStarted: a parenting course on communication and communication support: textbook]GöteborgHabilitering & Hälsa2011 Swedish
- LordCRutterMLe CouteurAAutism Diagnostic Interview-Revised – a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disordersJ Autism Dev Disord19942456596857814313
- SparrowSSCichettiDVBallaDAVineland Adaptive Behaviour Scales2nd edCircle Pines (MN)American Guidance Service2005
- SchorreBEVandvikIHGlobal assessment of psychosocial functioning in child and adolescent psychiatry. A review of three unidimensional scales (C-GAS, GAF, GAPD)Eur Child Adolesc Psychiatry200413527328615490275
- ShafferDGouldMSBrasicJA children’s global assessment scale (CGAS)Arch Gen Psychiatry19834011122812316639293
- HowardJSStanislawHGreenGSparkmanCRCohenHGComparison of behaviour analytic and eclectic early interventions for young children with autism after three yearsRes Dev Disabil201435123326334425190094
- OdomSHumeKBoydBStabelAMoving beyond the intensive behavior treatment versus eclectic dichotomy: evidence-based and individualized programs for learners with ASDBehav Modif201236327029722645398
- WeitlaufASMcPheetersMLPetersBTherapies for Children With Autism Spectrum Disorder: Behavioral Interventions Update [Internet]Rockville (MD)Agency for Healthcare Research and Quality (US)2014
- GillbergCFernellEAutism plus versus autism pureJ Autism Dev Disord201444123274327624958434
- BillstedtEGillbergICGillbergCAutism in adults: symptom patterns and early childhood predictors. Use of the DISCO in a community sample followed from childhoodJ Child Psychol Psychiatry2007481102111017995486
- HowlinPSavageSMossPTempierARutterMCognitive and language skills in adults with autism: a 40-year follow-upJ Child Psychol Psychiatry2014551495823848399
- VolkmarFRReichowBInfants and toddlers with autism: the promise and the challengesInt J Speech Lang Pathol2014161111424345000
- OlssonMBWesterlundJLundströmSGiacobiniMFernellEGillbergC“Recovery” from the diagnosis of autism – and then?Neuropsychiatr Dis Treat201511999100525897237
- RyanSSalisburyH‘You know what boys are like’: pre-diagnosis experiences of parents of children with autism spectrum conditionsBr J Gen Pract201262598e378e38322546598
- MitchellCHoldtNThe search for a timely diagnosis: parents’ experiences of their child being diagnosed with an Autistic spectrum disorderJ Child Adolesc Ment Health2014261496225391570
- GillbergCThe ESSENCE in child psychiatry: early symptomatic syndromes eliciting neurodevelopmental clinical examinationsRes Dev Disabil2010311543155120634041

