Abstract
Introduction
Auditory hallucinations are defined as experiences of auditory perceptions in the absence of a provoking external stimulus. They are the most prevalent symptoms of schizophrenia with high capacity for chronicity and refractoriness during the course of disease. The transcranial direct current stimulation (tDCS) – a safe, portable, and inexpensive neuromodulation technique – has emerged as a promising treatment for the management of auditory hallucinations.
Objective
The aim of this study is to analyze the level of evidence in the literature available for the use of tDCS as a treatment for auditory hallucinations in schizophrenia.
Methods
A systematic review was performed, searching in the main electronic databases including the Cochrane Library and MEDLINE/PubMed. The searches were performed by combining descriptors, applying terms of the Medical Subject Headings (MeSH) of Descriptors of Health Sciences and descriptors contractions. PRISMA protocol was used as a guide and the terms used were the clinical outcomes (“Schizophrenia” OR “Auditory Hallucinations” OR “Auditory Verbal Hallucinations” OR “Psychosis”) searched together (“AND”) with interventions (“transcranial Direct Current Stimulation” OR “tDCS” OR “Brain Polarization”).
Results
Six randomized controlled trials that evaluated the effects of tDCS on the severity of auditory hallucinations in schizophrenic patients were selected. Analysis of the clinical results of these studies pointed toward incongruence in the information with regard to the therapeutic use of tDCS with a view to reducing the severity of auditory hallucinations in schizophrenia. Only three studies revealed a therapeutic benefit, manifested by reductions in severity and frequency of auditory verbal hallucinations in schizophrenic patients.
Conclusion
Although tDCS has shown promising results in reducing the severity of auditory hallucinations in schizophrenic patients, this technique cannot yet be used as a therapeutic alternative due to lack of studies with large sample sizes that portray the positive effects that have been described.
Introduction
Schizophrenia is a chronic mental disturbance characterized by dysfunctions in emotion, cognition, and perception of reality.Citation1 Due to the potential of affecting innumerable cerebral domains, schizophrenic patients present with a heterogeneity of symptoms and variation in their severity during the evolution of the disease.Citation2 The estimated prevalence of this disease is ~1% among the world population, and its incidence is ~1.5/10,000 that reveals the capacity for chronification of this disease.Citation3,Citation4
The habitual clinical expression of schizophrenia is the presence of psychotic (positive) and negative symptoms that may be associated with a cognitive compromise, which generally is subtle.Citation5 So-called “positive symptoms” comprised hallucinations, delusions, disturbances of thought, and bizarre behavior, whereas the “negative symptoms” include emotional dullness, anhedonia, alogia, and attention deficit.Citation1 Hallucinations are defined as experiences of perception that occur without the real presence of an external stimulus.Citation6 Although they may occur in any of the sensory modalities, the most common type is auditory verbal hallucination (AVH).Citation7,Citation8 Around 60%–80% of schizophrenic patients are estimated to present with this symptom during the course of the disease, and the perception of voices that talk to, comment, or issue commands to the individual has been reported.Citation8,Citation9 The majority of these hallucinations has a negative content, generally expressed by angry voices that use words or expressions of abuse to transmit information to the subject, and is associated with a high risk of suicide in schizophrenia.Citation10,Citation11
Recent advances in functional neuroimaging methods have enabled a better understanding of the disturbances of the neural circuits of neuropsychiatric diseases.Citation12 For this reason, a growing interest in interventions with potentials of neuromodulation has arisen with a view to rupturing patterns of neuronal activity that may be associated with symptoms of a base disease.Citation13
In the present context, transcranial direct current stimulation (tDCS) configures as a tool that potentiates cognitive and motor performance in healthy individuals and as an emergent treatment for a series of neuropsychiatric diseases.Citation12,Citation13 tDCS acts through the application of direct electrical currents of low amplitude on the scalp, modulating the cortical excitability.Citation14
tDCS long-term effects appear to be associated with neuroplasticity phenomena that promote the modulation of neuronal synapses.Citation14 Changes in the efficacy of activating NMDA receptors, GABAergic activity, and modulation of interneurons appear to be the main factors responsible for changes in long-term potentiation and depression.Citation15,Citation16 Another type of synaptic neuroplasticity that appears to be influenced by tDCS is the type dependent on the brain-derived neurotrophic factor, in which its dysfunction is associated with the maladaptive neuroplasticity phenomena present in various neuropsychiatric diseases, including schizophrenia.Citation1,Citation16,Citation17 During AVH, it is supposed that cerebral areas involved in the perception of the discourse, primary auditory cortex and associated areas of language in the left hemisphere, are pathologically hyperactive.Citation18,Citation19
Our aim is to analyze the available literature and, from it, determine the level of evidence of information for suggesting directions for future research and the indications for using tDCS in the therapeutic approach to auditory hallucinations in schizophrenia.
Methods
A systematic review of the literature was performed based on “The Cochrane Collaboration” methodology and guided by the PRISMA protocol. Scientific articles that approached the use of tDCS for the treatment of auditory hallucinations resistant to treatment with antipsychotic drugs in schizophrenia were searched in the following electronic database sources: “MEDLINE/PubMed”, “Web of Science”, “LILACS”, “BIREME”, and “PsycINFO”, using the combination of descriptors, including terms from the Medical Subject Headings (MeSH) of descriptors of health sciences and contractions of descriptors. Therefore, the following terms were combined using the Boolean operator “AND”:
Outcome: “Schizophrenia” OR “Auditory Hallucinations” OR “Auditory Verbal Hallucinations” OR “Psychosis”.
Intervention: “Transcranial Direct Current Stimulation (tDCS)” OR “tDCS” OR “Brain Polarization”.
The research was conducted in an equal manner among all the databases relating each outcome to a type of intervention. The results of these combinations during the search were as follows: [Schizophrenia OR Auditory Hallucinations OR Auditory Verbal Hallucinations OR Psychosis] AND [Transcranial Direct Current Stimulation OR tDCS OR Brain Polarization].
The inclusion criteria applied to the studies were (1) use of tDCS in schizophrenic patients; (2) application of clinical scales in evaluating the severity of auditory hallucinations pre/post tDCS; (3) methodological design based on randomization, containing mean and standard deviation of outcomes analyzed; or data that would make it possible to deduce these values; (4) studies published in indexed periodicals; and (5) publications in Portuguese, English, or Spanish.
The exclusion criteria used were (1) studies containing samples of schizophrenic patients presenting neuropsychiatric comorbidities; (2) review articles; (3) studies that presented another cerebral stimulation technique; and (4) studies identified, but without full version available.
Two investigators independently conducted the search for and selection of articles. The titles and abstracts of all publications found were imported to the reference manager EndNote X7 that was responsible for eliminating the duplicates.
The titles and abstracts of studies found were read by each researcher for the purpose of finding potentially useful articles. Those that in principle fulfilled the selection criteria were read in full for better verification and then either included in this systematic review or not. The references of the articles found were consulted to seek new articles that may not have been found in the initial search.
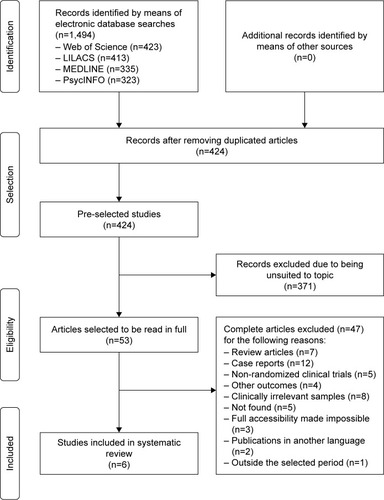
Initially, 1,494 publications were identified by means of electronic search. The databases that resulted in findings were Web of Science (n=423); LILACS (n=413); MEDLINE/PubMed (n=335), and PsycINFO (n=323). After eliminating duplicated articles, the titles and abstracts of 424 articles were read by both researchers (PHP, EPS), independently, totaling a number of 53 pre-selected manuscripts for reading in full. During this stage, another 371 articles were excluded because they were not suited to the topic.
Among the 53 articles initially selected, only 6 manuscripts fulfilled the eligibility criteria and were selected for final analysis and revision of their content, whereas the remainder were eliminated because they did not satisfy some of the pre-determined demands of the eligibility criteria (). The manual search strategy was also applied to the lists of references of the articles found, but added no new studies to the final analysis.
The clinical and stimulation parameters adopted by each study are described in and , respectively.
Table 1 Clinical parameters of studies obtained for systematic review
Table 2 tDCS parameters of studies obtained for systematic review
Results
Brunelin et al conducted a randomized, parallel, double-blind, sham-controlled tDCS trial placing the anode on the left dorsolateral prefrontal cortex (DLPFC) and cathode over left temporo-parietal junction (TPJ).Citation20 Thirty DSM-IV schizophrenic patients with drug-resistant AVH (15 active and 15 sham) were submitted to twice daily stimulation sessions for 5 days (20 minutes; 2 mA; electrode area of 35 cm2). The primary outcome was change in the severity of the AVH measured by the Auditory Hallucination Rating Scale (AHRS).Citation21 The active group had a significant mean improvement of 31% and the therapeutic effects lasted for 3 months. There was also a significant improvement in negative symptoms as measured by the Positive and Negative Syndrome Scale (PANSS).Citation22
In a randomized crossover trial, Fitzgerald et al investigated the therapeutic potential of unilateral and bilateral tDCS for the treatment of refractory AVH.Citation23 Patients with schizophrenia or schizoaffective disorder presenting persistent hallucinations and negative symptoms, with failure to respond to two adequate therapeutic attempts with antipsychotic agents, were randomly allocated to bilateral tDCS (anode on F3/F4 and cathode over TP3/TP4; n=11) and unilateral tDCS (anode over F3 and cathode on TP3; n=13).Citation24 Stimulation parameters were kept the same for both experiments: 15 sessions distributed throughout three consecutive weeks, 1×/day, with a voltage of 2 mA for 20 minutes/session. Both groups had no significant effects on AVH or other psychotic symptoms.
Patients with refractory AVH were enrolled in a randomized, double-blind, parallel trial performed by Mondino et al.Citation25 In that trial, 15 of 28 subjects were ex-participants of a previous study conducted by the same group.Citation20 Anode electrode was positioned over DLPFC and cathode on TPJ. Individuals underwent twice-daily stimulation sessions for five consecutive days, 2×/day with a current intensity of 2 mA for 20 minutes/session. Greater AVH frequency reduction was observed (mean: –46% vs +7.5%) after active versus sham tDCS.
Another randomized, double-blind, parallel group, sham-controlled trial evaluated the effects of tDCS over the left TPJ in a rest state.Citation26 Schizophrenia subjects with drug-resistant AVH (n=23) were randomly allocated to active (n=11) and sham interventions (n=12). Anodal stimulation was delivered on DLPFC and cathodal tDCS over TPJ. Stimulation sessions were performed for five consecutive days, 2 mA for 20 minutes/session. The primary outcome measure for AVH was the AHRS scale that was applied before the beginning of the 1st session and following the 10th session.Citation21 Greater AVH reduction (mean AHRS: –28% vs –10%) following active tDCS was observed, when compared with sham intervention.
In a trial, the effects of tDCS on cognition, psychiatric symptoms and fissure due to cigarettes were evaluated in smoker schizophrenic patients.Citation27 Thirty-three patients with schizophrenia or schizoaffective disorder were randomly allocated to the active (n=17) and sham groups (n=16), but only 29 of them completed the entire study. Stimulation sessions were performed for five consecutive days, 2×/day (anode over DLPFC; cathode on TPJ). Despite improvements in cognitive measures, no difference in PANSS scores, AVH, and cigarette craving was observed after active stimulation.
Fröhlich et al in a parallel, randomized, double-blind, sham-controlled trial evaluated the effects of tDCS applied once a day, on the severity of AVHs in 26 schizophrenic or schizoaffective subjects.Citation28 The stimulation parameters were 2 mA (anodal and cathodal) applied at the same time for 20 minutes/session/day for five consecutive days.Citation28 Anodal tDCS was delivered over DLPFC and cathodal on TPJ. Following the active stimulation, no difference in AVH reduction (mean AHRS: –24% vs –34%) was observed, when compared with sham group.
Tolerability and adverse events of tDCS
All patients included in the six randomized clinical trials (n=164) underwent at least one session of tDCS. Of these, a total of 160 completed all sessions and evaluations foreseen. Four individuals, who did not complete the stimulation protocols fully in one of the studies, dropped off for reasons of desisting.Citation27 Thus, no study needed to exclude any patient from a certain stimulation protocol as a result of adverse events.Citation20,Citation23,Citation25–Citation28
With the exception of two studies, which did not provide information on tolerability in their publications, adverse events secondary to tDCS were investigated by means of questionnaires that were applied at the end of each session.Citation25–Citation28 Another two studies also published the adverse events most common in their stimulation protocols, but did not specify the instrument used to obtain the tolerability data.Citation20,Citation23
Discussion
Auditory hallucinations may be considered the main symptom of schizophrenia, due to their high prevalence during the course of the disease in the population of patients. The treatment at present recommended by the American Psychiatric Association (APA) is mainly based on the use of antipsychotic drugs that sometimes may not guarantee an efficient therapeutic response to the reduction of these symptoms.Citation29 The daily persistence of hallucinatory experiences is related to compromise of the quality of life and also to socio-occupational damage to the individual’s life. In this challenging context, tDCS appears as an emergent treatment for the management of auditory hallucinations in schizophrenia, by means of the phenomenon of neuromodulation.
The present systematic review identified six randomized clinical trials, all at the experimental phase, which sought to evaluate the therapeutic effects of tDCS on auditory hallucinations in schizophrenia, and improvement in the stimulation parameters applied in this context. Analysis of the clinical results of these studies pointed toward incongruence in the information with regard to the therapeutic use of tDCS with a view to reducing the severity of auditory hallucinations in schizophrenia. Only three studies demonstrated a therapeutic benefit of tDCS for the treatment of AVHs, manifested by reductions in severity and frequency of these symptoms in schizophrenic patients.Citation20,Citation25,Citation26 Brunelin et al also revealed maintenance of tDCS acute effects on the AHRS scores in the first and third months of follow-up, after 10 sessions of tDCS (2×/day).Citation20 However, three other studies were unable to reproduce similar effects on the severity of AVHs.Citation23,Citation27,Citation28
Division of the clinical trials according to the therapeutic results of tDCS they presented (positive vs negative) also revealed another difference between these two groups: the baseline diagnosis of the individuals evaluated. Trials that demonstrated the therapeutic success of tDCS included only schizophrenic patients in their samples, whereas other studies also included schizoaffective individuals. Nevertheless, the therapeutic success of tDCS on auditory hallucinations cannot be justified by the mental disturbance because the inclusion of individuals in each trial required the fulfillment of eligibility criteria, thereby avoiding possible clinical differences among subjects.
All studies evaluating the therapeutic efficacy of tDCS on AVH adopted as inclusion criterion schizophrenic patients with AVH refractory to treatment, with exception of the study by Smith et al, which may also explain the discrete changes observed in the severity of hallucinations post interventions, in this study.Citation20,Citation23,Citation25–Citation28 These findings may also be related to aspects of the sample population. Nicotine-related smoking – inclusion criteria of the schizophrenic patients included in this experiment – is associated with a reduction in the clinical efficacy of tDCS in individuals with schizophrenia.Citation30 Another important factor that appears to have contributed to the negative response presented in this study was the montage used. Cathodal electrode was placed over the contralateral supraorbital area, different from the other studies that applied cathodal stimulation on TPJ. Neurophysiological studies have shown hyperactivity in left parietal areas of patients with schizophrenia, which is associated with the presence of positive symptoms.Citation18,Citation19,Citation31–Citation34 Therefore, the possible reduction of excitability in this area in addition to anodal stimulation on DLPFC may result in a better control of symptoms.
Different definitions of refractoriness were adopted for composition of the inclusion criteria of each study. Fitzgerald et al and Fröhlich et al were the only researchers who followed the refractoriness criteria proposed by the APA for refractory schizophrenia, although the evaluation of AVHs severity of their samples differed.Citation23,Citation28,Citation29 Fitzgerald et al used the PANSS scale, what may explain the lack of therapeutic response to tDCS, in this study. The PANSS scale is unable to measure the severity of hallucinations in a detailed manner, and its severity scores for the item of hallucinations are difficult to differentiate from one another.Citation35 The more appropriate scale for population samples containing schizophrenic patients with hallucinations refractory to treatment is the AHRS scale, as it presents a high capacity for investigating the hallucinatory symptoms experienced by the individual.Citation21 This was the method applied by Fröhlich et al, Brunelin et al and Mondino et al for quantifying the severity of AVH, which in these samples was shown to be of similar dimensions.Citation20,Citation26,Citation28 However, the lack of therapeutic efficacy of tDCS on the AVH described by Fröhlich et al, a result contrary to that obtained by the other two trials, reveals the significant importance of adopting an adequate stimulation protocol for obtaining successful therapy in a population with the potential for symptomatic improvement by means of tDCS.Citation20,Citation26,Citation28 Although this trial applied the same current density observed in other studies presenting positive findings, the number of sessions and montage was different. Previous studies revealed better and longer-lasting modulatory response when applying a greater number of sessions and/or a shorter interval among them.Citation20,Citation25 The same cannot be affirmed regarding montage, due to still controversial findings. A recent study has even questioned the polarity-specific effects when different current intensities are applied.Citation36 Despite an effort having been made to standardize the application of tDCS in different neuropsychiatric and pain conditions, to date there is no established definition as to the optimal protocol in any of these nosological conditions. In addition, another explanation suggested by the authors regarding the non-significant findings observed in their clinical trial is based on the occurrence of a possible placebo effect because all subjects were aware that a new and potentially effective therapy would be investigated in that study. Furthermore, patients were on continuous therapy during the trial with different antipsychotics, some still in combination with other psychotropic drugs.
Although the ideal parameters of tDCS are as yet not completely established in the literature, few but relevant differences were found between the stimulation protocols applied by the clinical trials included in this review, as previously mentioned. The studies that demonstrated a therapeutic benefit of tDCS on AVH refractory to treatment with antipsychotic agents in schizophrenic patients presented identical stimulation parameters.Citation20,Citation25,Citation26 All the studies performed anodal stimulation on the left DLPFC with a view to increasing the cortical excitability in this area, since schizophrenic patients possibly present a cortical hypoac-tivity in this region during the state of rest or when they are submitted to working memory (WM) tasks.Citation37,Citation38 Prefrontal cortex dysfunction is associated with development of negative symptoms and compromise of cognitive functions in schizophrenia.Citation17 The use of high-frequency repetitive trans-cranial magnetic stimulation (rTMS), a non-invasive brain stimulation technique that applies magnetic field to modulate brain excitability, for the treatment of negative symptoms encouraged the first tDCS studies to be conducted with a view to modulate DLPFC.Citation39 The recent discovery that anodal stimulation could improve the performance of working memory, a function involved in the executive control of information, generated speculations about the possibility of left DLPFC stimulation helping to control AVH by inhibiting irrelevant verbal information.Citation17,Citation40 In addition, the placement of cathodal electrode over the left parietal area possibly plays an important role as it may decrease the hyperactivity of this area, which is a physiological mechanism associated with positive symptoms in this population, as commented before.Citation18,Citation19,Citation31–Citation34 Studies using functional neuroimaging methods have demonstrated that hyperactivity of the left TPJ plays a crucial role in the physiopathology of auditory hallucinations, and it is therefore a target region of cathodal stimulation in all randomized clinical trials that presented AVH as the primary outcome.Citation18–Citation20,Citation23,Citation25,Citation26,Citation28 Those trials were motivated by the positive results of studies involving low-frequency rTMS on the left TPJ, which revealed an attenuation of auditory hallucinations refractory to treatment with antipsychotic drugs.Citation41,Citation42
The studies of Brunelin et al and Mondino et al were the only ones of this review that exhibited significant results of both anodal stimulation over DLPFC and cathodal stimulation on left TPJ, which strengthen the hypothesis of the importance of these areas for the control of AVH in refractory patients.Citation17,Citation20,Citation26 Another study from the same group of researchers has demonstrated only the efficacy of cathodal stimulation with TPJ as the target region for promoting changes in the severity of AVH.Citation25 The absence of therapeutic response to negative symptoms of the patients analyzed may be explained by the unavailability of the PANSS scale data at the end of the last tDCS session, or due to the fact that the study did not present strict eligibility criteria, compromising the quality of the sample.Citation25 Moreover, the use of a scale based only on the evaluation of the frequency of AVH, in which the evaluation criteria of the score and the reasons for the use of this method by the authors were not mentioned, may have produced errors in the evaluation of the AVH, such as lack of precision.Citation25
The studies of Fitzgerald et al, Smith et al and Fröhlich et al presented a total number of daily tDCS sessions differing from those of previous studies, as previously mentioned.Citation20,Citation23,Citation25–Citation28 Stimulation of the motor cortex with tDCS is dependent on a complex maintenance of its effects that are capable of exceeding the period of time of the sessions.Citation43 Therefore, stimulation protocols containing only one daily session do not appear to be ideal when the aim is to obtain a therapeutic effect. Moreover, studies with rTMS have recommended treatments of longer duration (around 4–6 weeks) for depressive disorders.Citation44 Therefore, the need for conducting further studies in this area becomes evident, with a view to establishing the ideal tDCS protocol.
Unfortunately, not all studies provide data on antipsy-chotic use, which is a very important issue to discuss as potential moderator of the therapeutic effect of tDCS. In a recent study, Agarwal et al assessed the influence of the type of antipsychotic drug in tDCS effects in individuals with schizophrenia, finding a significant effect in the control of auditory hallucinations, mainly among individuals using low-affinity antipsychotics or a combination of it with high-affinity ones.Citation45 Regarding the trials included in this review, although some of them correctly enrolled only patients with stable antipsychotic dose for a minimum period of time, for example 3 months, some relevant information such as type of drug and dose was not present and also was not analyzed by most of them.
All of the tDCS interventions evaluated presented recommended safety measures: electrical current ⩽2.5 mA, duration of session between 20 and 60 minutes, frequency of sessions ≤2 daily sessions, and electrodes that did not come into contact with the skin.Citation23,Citation25–Citation28,Citation30,Citation46 The adverse events frequently related in studies such as itching in the location of electrode, headache, and tingling corroborate pre-existent data in the literature.Citation47 No stimulation protocol analyzed needed to be interrupted, thus strengthening the safety profile of this technique.Citation48
Conclusion
tDCS – a safe, portable, and simple neuromodulation technique – has been shown to be promising as a therapeutic approach for auditory hallucinations, particularly the type refractory to treatment with antipsychotic drugs in schizophrenic patients. Nevertheless, only six randomized clinical trials with limited sample sizes have been published and, of these, only three demonstrated therapeutic benefits with the use of this technique. The body of information found in the current literature has been shown to be insufficient for determining the effectiveness of treatment with tDCS for reducing the severity of auditory hallucinations. Randomized clinical trials containing large population samples are expected to investigate whether the positive results can be replicated. Moreover, the stimulation parameters and methods of evaluating the clinical outcomes need to be better defined, so that there will be advances in the sense of consolidating tDCS as a therapeutic possibility for auditory hallucinations in schizophrenia.
Disclosure
The authors report no conflicts of interest in this work.
References
- KuoMFPaulusWNitscheMATherapeutic effects of non-invasive brain stimulation with direct currents (tDCS) in neuropsychiatric diseasesNeuroimage201485Pt 394896023747962
- FrangouSSchizophreniaMedicine2008368405409
- McGrathJSahaSChantDWelhamJSchizophrenia: a concise overview of incidence, prevalence, and mortalityEpidemiol Rev200830677618480098
- PicchioniMMMurrayRMSchizophreniaBMJ20073357610919517626963
- HowesODMurrayRMSchizophrenia: an integrated sociodevelop-mental-cognitive modelLancet201438399291677168724315522
- DavidASThe cognitive neuropsychiatry of auditory verbal hallucinations: an overviewCogn Neuropsychiatry200491–210712316571577
- American Psychiatric AssociationSchizophrenia spectrum and other psychotic disordersDiagnostic and Statistical Manual of Mental Disorders5th edWashington DC, MDAmerican Psychiatric Publishing201387122
- AndreasenNCFlaumMSchizophrenia: the characteristic symptomsSchizophr Bull199117127492047788
- KuberaKMBarthAHirjakDThomannPAWolfRCNoninvasive brain stimulation for the treatment of auditory verbal hallucinations in schizophrenia: methods, effects and challengesFront Syst Neurosci2015913126528145
- Harkavy-FriedmanJMKimhyDNelsonEAVenardeDFMalaspinaDMannJJSuicide attempts in schizophrenia: the role of command auditory hallucinations for suicideJ Clin Psychiatry200364887187412927000
- McCarthy-JonesSTrauerTMackinnonASimsEThomasNCopolovDLA new phenomenological survey of auditory hallucinations: evidence for subtypes and implications for theory and practiceSchizophr Bull201440123123523267192
- DayanECensorNBuchERSandriniMCohenLGNoninvasive brain stimulation: from physiology to network dynamics and backNat Neurosci201316783884423799477
- WagnerTValero-CabreAPascual-LeoneANoninvasive human brain stimulationAnnu Rev Biomed Eng2007952756517444810
- NitscheMACohenLGWassermannEMTranscranial direct current stimulation: state of the art 2008Brain Stimul20081320622320633386
- KoopsSvan den BrinkHSommerIETranscranial direct current stimulation as a treatment for auditory hallucinationsFront Psychol2015624425798123
- AgarwalSMShivakumarVBoseATranscranial direct current stimulation in schizophreniaClin Psychopharmacol Neurosci201311311812524465247
- BrunoniARShiozawaPTruongDUnderstanding tDCS effects in schizophrenia: a systematic review of clinical data and an integrated computation modeling analysisExpert Rev Med Devices201411438339424754366
- SilbersweigDASternEFrithCA functional neuroanatomy of hallucinations in schizophreniaNature199537865531761797477318
- ShergillSSBrammerMJWilliamsSCMurrayRMMcGuirePKMapping auditory hallucinations in schizophrenia using functional magnetic resonance imagingArch Gen Psychiatry200057111033103811074868
- BrunelinJMondinoMGassabLExamining transcranial direct-current stimulation (tDCS) as a treatment for hallucinations in schizophreniaAm J Psychiatry2012169771972422581236
- HaddockGMcCarronJTarrierNFaragherEBScales to measure dimensions of hallucinations and delusions: the Psychotic Symptom Rating Scales (PSYRATS)Psychol Med199929487988910473315
- KaySRFiszbeinAOplerLAThe Positive and Negative Syndrome Scale (PANSS) for schizophreniaSchizophrenia Bull1987132261276
- FitzgeraldPBMcQueenSDaskalakisZJHoyKEA negative pilot study of daily bimodal transcranial direct current stimulation in schizophreniaBrain Stimul20147681381625442152
- SheehanDVLecrubierYSheehanKHThe mini-international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10J Clin Psychiatry199859Suppl 202233
- MondinoMHaesebaertFPouletESuaud-ChagnyMFBrunelinJFronto-temporal transcranial direct current stimulation (tDCS) reduces source-monitoring deficits and auditory hallucinations in patients with schizophreniaSchizophr Res20151612–351551625468175
- MondinoMJardriRSuaud-ChagnyMFSaoudMPouletEBrunelinJEffects of fronto-temporal transcranial direct current stimulation on auditory verbal hallucinations and resting-state functional connectivity of the left temporo-parietal junction in patients with schizophreniaSchizophr Bull201642231832626303936
- SmithRCBoulesSMattiuzSEffects of transcranial direct current stimulation (tDCS) on cognition, symptoms, and smoking in schizophrenia: a randomized controlled studySchizophr Res20151681–226026626190299
- FröhlichFBurrelloTNMellinJMExploratory study of once-daily transcranial direct current stimulation (tDCS) as a treatment for auditory hallucinations in schizophreniaEur Psychiatry201633546026866874
- LehmanAFLiebermanJADixonLBAmerican Psychiatric Association, Steering Committee on Practice GuidelinesPractice guideline for the treatment of patients with schizophrenia, second editionAm J Psychiatry2004161Suppl 2156
- BrunelinJHasanAHaesebaertFNitscheMAPouletENicotine smoking prevents the effects of frontotemporal transcranial direct current stimulation (tDCS) in hallucinating patients with schizophreniaBrain Stimul2015861225122726316227
- WibleCGPreusAPHashimotoRA cognitive neuroscience view of schizophrenic symptoms: abnormal activation of a system for social perception and communicationBrain Imaging Behav2009318511019809534
- RainsLSFallicaGO’DalyOExploring psychotic symptoms: a comparison of motor related neuronal activation during and after acute psychosisBMC Psychiatry20121210222871335
- MolinaVReigSPascauJAnatomical and functional cerebral variables associated with basal symptoms but not risperidone response in minimally treated schizophreniaPsychiatry Res2003124316317514623068
- FranckNO’LearyDSFlaumMHichwaRDAndreasenNCCerebral blood flow changes associated with Schneiderian first-rank symptoms in schizophreniaJ Neuropsychiatry Clin Neurosci200214327728212154151
- SantorDAAscher-SvanumHLindenmayerJPObenchainRLItem response analysis of the Positive and Negative Syndrome ScaleBMC Psychiatry200776618005449
- BatsikadzeGMoliadzeVPaulusWKuoMFNitscheMAPartially non-linear stimulation intensity-dependent effects of direct current stimulation on motor cortex excitability in humansJ Physiol201359171987200023339180
- KuhnSGallinatJResting-state brain activity in schizophrenia and major depression: a quantitative meta-analysisSchizophr Bull201339235836522080493
- LawrieSMBuechelCWhalleyHCFrithCDFristonKJJohnstoneECReduced frontotemporal functional connectivity in schizophrenia associated with auditory hallucinationsBiol Psychiatry200251121008101112062886
- Dlabac-de LangeJJKnegteringRAlemanARepetitive transcranial magnetic stimulation for negative symptoms of schizophrenia: review and meta-analysisJ Clin Psychiatry201071441141820361909
- FregniFBoggioPSNitscheMAnodal transcranial direct current stimulation of prefrontal cortex enhances working memoryExp Brain Res20051661233015999258
- AlemanASommerIEKahnRSEfficacy of slow repetitive transcranial magnetic stimulation in the treatment of resistant auditory hallucinations in schizophrenia: a meta-analysisJ Clin Psychiatry200768341642117388712
- Montagne-LarmurierAEtardOMaizaODollfusSRepetitive transcranial magnetic stimulation in the treatment of auditory hallucinations in schizophrenic patientsCurr Opin Psychiatry201124653354021941181
- Monte-SilvaKKuoMFLiebetanzDPaulusWNitscheMAShaping the optimal repetition interval for cathodal transcranial direct current stimulation (tDCS)J Neurophysiol201010341735174020107115
- CarpenterLLJanicakPGAaronsonSTTranscranial magnetic stimulation (TMS) for major depression: a multisite, naturalistic, observational study of acute treatment outcomes in clinical practiceDepress Anxiety201229758759622689344
- AgarwalSMBoseAShivakumarVImpact of antipsychotic medication on transcranial direct current stimulation (tDCS) effects in schizophrenia patientsPsychiatry Res20162359710326699879
- FregniFNitscheMALooCKRegulatory considerations for the clinical and research use of transcranial direct current stimulation (tDCS): review and recommendations from an expert panelClin Res Regul Aff2015321223525983531
- PoreiszCBorosKAntalAPaulusWSafety aspects of transcranial direct current stimulation concerning healthy subjects and patientsBrain Res Bull2007724–620821417452283
- RossiSHallettMRossiniPMPascual-LeoneASafety of TMS Consensus GroupSafety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and researchClin Neurophysiol2009120122008203919833552