Abstract
Objective
This study aimed to determine the following: 1) the proportion of women in the homeless population with schizophrenia (SZ) or bipolar disorder (BD), in addition to the trajectory of their homelessness (ie, homelessness history, number of nights spent without home during the 180 past nights) and the characteristics of their illnesses compared to men (ie, illness severity, suicide risk, physical health status, and quality of life [QoL]); 2) whether these women were victimized more frequently than similarly situated men; 3) the impact of victimization on these women in terms of illness severity, suicide risk, physical health status, and QoL; and lastly 4) the differences and overlap of homeless women with SZ and BD.
Methods
This study employed data at baseline from a multicenter randomized controlled trial conducted in the following four large French cities: Lille, Marseille, Paris, and Toulouse. Mobile mental health outreach teams recruited SZ/BD homeless patients in the street, emergency shelters, hospitals, and jails from August 2011 to April 2014. Evaluations were performed during face-to-face interviews by psychiatrists and research assistants in the offices of mobile mental health outreach teams that were located in the downtown area of each city. The quantitative data were analyzed using descriptive analyses, chi-square and Student’s t-tests, generalized estimating equation regression models, and path analysis.
Results
A total of 703 patients were included in this study. The proportion of women in the SZ/BD homeless population was 123/703 (17.5%). In this population, women were more likely than men to declare that they were subjected to physical or sexual assault during the past 6 months, that they had been diagnosed with posttraumatic stress disorder (PTSD), and that they had experienced more severe depressive symptoms. Moreover, these women presented a higher suicide risk, worse physical health status, and lower QoL than similarly situated men. Homeless women with BD were more vulnerable than women with SZ. A path analysis revealed that PTSD and violent victimization might explain the higher levels of depression and suicide risk and the lower levels of physical health status and QoL in homeless women.
Conclusion
SZ/BD homeless women experience more PTSD and victimization than men, which are both associated with poor clinical outcomes. These results confirm the vulnerability of homeless women in this high need population and should be considered by public health policy.
Introduction
Homelessness is a significant social, economic, and health issue in France. In 2012, 141,500 people were homeless and nearly two in five of these people were women.Citation1 The proportion of homeless women has increased substantially over recent years, reflecting shifts in the vulnerability and socioeconomic conditions of women’s lives. The National Institute for Demographic Studies (INED) and the French National Institute for Statistics and Economic Studies (INSEE) found that the percentage of women in the homeless population had been doubled in Paris between 1995 and 2012.Citation2 Despite the magnitude of this phenomenon, the individual circumstances, structural factors, and systemic failures underpinning this feminization are poorly understood and have not been considered in public policy. One of the most challenging issues is the relative invisibility of homeless women.Citation3 Typically, women without homes are accommodated by partners or members of their wider family or partners.Citation4 This type of homelessness is called “hidden” that stands in contrast with “visible” homelessness in public spaces and in institutions for the homeless (shelters, hostels, daytime facilities, etc).Citation5 This lack of visibility in the public space has translated into a lack of data for both researchersCitation6 and public authorities.Citation7 Organizations such as the European Federation of National Organizations Working with the Homeless (FEANTSA) have officially made a call for more research into this question.Citation8 According to a recent French work, actions toward homeless women should be implemented to promote their access to care.Citation9
“Victimization” is defined as the act of being a victim of any aggressive behaviorCitation10 and seems to be both a cause and an effect of homelessness.Citation11,Citation12 Victimization often precedes homelessness, and re-victimization is common in the street.Citation13,Citation14 Homeless women with severe mental illnesses represent an extreme vulnerable subgroup of victimization.Citation15,Citation16 Previous studies have underlined the omnipresence of victimization in the lives of homeless women,Citation17–Citation19 during their childhood (including physical and sexual abuse), with their intimate male partners, and in the street.Citation16 Experiences of institutional violence with objectification and infantilization are commonplace in traditional services for the homeless.Citation19 Moreover, more than one in four homeless people suffer from serious mental illness, such as schizophrenia (SZ) or bipolar disorders (BD),Citation20–Citation22 with considerable risk of violent victimization.Citation23,Citation24 These studies have unquestionably advanced our knowledge of the vulnerability in homeless women with severe mental illnesses, but several issues remain insufficiently explored. Understanding the characteristics of this extreme vulnerable subgroup and the impact of victimization in the homelessness process is necessary to formulate relevant targeted strategies to ensure rehabilitation and re-entry into the social mainstream. To date, most previous studies were cross-sectional and did not use analytical techniques that allow for an examination of the direction and the structure of the relations between the trajectory of homelessness (ie, homelessness history and number of nights spent without home during the 180 past nights), victimization, and illness characteristics. Path analysis is used to describe the directed dependencies among a set of variables, could be a useful statistical procedure to test the theories involving non-straightforward relationships, and would be well suited to the management of cross-sectional data for inferential purposes. In addition, the differences and overlap of the trajectory of homelessness, victimization, and illness characteristics between homeless women with SZ and BD have been rarely studied and may be useful for proposing tailored interventions.
The aims of the present study were to determine 1) the proportion of women in the homeless population with SZ or BD in this French multicenter study and the trajectory of their homelessness and illness characteristics compared to those of men; 2) whether women were more frequently victimized than men; 3) the impact of victimization on women in terms of illness severity, suicide risk, physical health status, and quality of life (QoL); and lastly 4) the differences and overlap of homeless women with SZ and BD.
Methods
Study design and population
The French Housing First program is a multicenter randomized controlled trial conducted in the following French cities: Lille, Marseille, Paris, and ToulouseCitation25 and is designed to assess the impact of a Housing First intervention on health outcomes and costs over a period of 24 months on homeless people with severe mental illness compared to Treatment- As-Usual (five evaluations: baseline, 6, 12, 18 and 24 months). Baseline (t0) was the only data used in the present analysis, before any intervention. The Housing First program provides immediate access to independent housing and a recovery-oriented, assertive community treatment team that includes a doctor, a nurse, a social worker, and a peer worker. This team provides case management, mental health services, employment and housing assistance, substance abuse services, and other services to allow the individual to live successfully in the community. The inclusion criteria were as follows: over 18 years of age; homelessness (ie, no fixed place to stay for at least the past seven nights with little likelihood of finding a place in the upcoming month) or precariously housed (housed in a single-room occupancy, rooming house, or hotel/motel as a primary residence AND having a history of two or more episodes of being absolutely homeless in the past year OR one episode of being absolutely homeless for a duration of at least 4 weeks over the past year); living in the city in question for >6 months and intending to stay in that same city for the coming 2 years; possessing a high level of need, defined as: having a diagnosis of SZ or BD according to Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV-TR) criteria;Citation26 moderate to severe disability according to the Multnomah Community Ability Scale (score ≤62);Citation27,Citation28 and meet at least one of the following three criteria: 1) having been hospitalized two or more times in any 1 year over the last 5 years for mental illness or 2) having comorbid alcohol or substance use or 3) having been arrested or incarcerated over the last 2 years; being covered by French government health insurance including free state aid; and speaking French. The exclusion criteria (ie, characteristics that disqualify patients from inclusion in the study) were the absence of capacity to consent,Citation29 having young/dependent children at the time of evaluation, a current pregnancy, or irregular immigration status in accordance with French law on biomedical research. Mobile mental health outreach teamsCitation30 recruited patients from August 2011 to April 2014 in the street, emergency shelters, hospitals, and jails. Evaluations were performed during face-to-face interviews by psychiatrists and research assistants in the offices of mobile mental health outreach teams that were located in the downtown area of each city (for more details for setting information and recruitment, see the protocol article).Citation25
Data collection
The following data were collected:
Sociodemographic information.
History of homelessness: Lifetime duration of homelessness, age at first homeless experience, location (street, emergency shelter, specific accommodation for homeless persons), and number of nights spent homeless over the past 6 months using a retrospective calendar. The location and the number of nights spent homeless over the past 6 months were recoded into the categories of the European Typology of Homelessness and Housing Exclusion, which describe all living situations, from sleeping in public spaces to living in extremely over-crowded spaces.Citation31
Clinical characteristics: The diagnosis of SZ and BD must have been based on the DSM-IV-TR criteria; psychiatric comorbidities, including current suicide risk and post-traumatic stress disorder (PTSD), were assessed using a structured diagnostic interview, the Mini-International Neuropsychiatric Interview (MINI);Citation26 perceived mental health was assessed using the Modified Colorado Symptom Index (MCSI).Citation33 The MCSI comprises 14 items inquiring about how often in the past month an individual has experienced a variety of mental health symptoms. Higher scores indicate a higher likelihood of mental health problems.
Health status: Physical and mental health status was assessed using the Medical Outcomes Study 36-item Short-Form Health Survey (SF-36) questionnaires, a self-administered questionnaire consisting of 36 items.Citation34 Two composite (also called summary) scores – the physical composite score and the mental composite score – are calculated. The index and composite scores range from 0, indicating the lowest health status, to 100, indicating the highest health status.
QoL was assessed using the Schizophrenia Quality of Life Scale (S-QoL) 18, which is a self-administered, multidimensional questionnaire developed and validated to specifically assess the QoL in patients with SZ and BDCitation35,Citation36 and validated in homeless individuals.Citation37 The total index scores range from 0, indicating the lowest QoL, to 100, indicating the highest QoL.
Victimization was defined by a self-reported history of violent (physical or sexual assault and attacks/fights) and non-violent (ie, stolen property, verbal assault, offensive behavior) victimization over the most recent 6-month period prior to the evaluation.
Utilization of health, justice, and social services was based on patients’ self-report data for the most recent 6-month period preceding the evaluation.
Ethical approval
The study was carried out in accordance with the principles of the Declaration of Helsinki, 6th revision. All participants gave written informed consent. The local ethics committee (Comité de Protection des Personnes Sud-Méditerranée V, France: trial number 11.050) and the French Drug and Device Regulation Agency (trial number 2011-A00668-33) approved the study. The current clinical trial number is NCT01570712 (first posted: April 4, 2012).
Analysis
Descriptive analyses were presented as frequencies and percentages for categorical variables and as means and standard deviations for continuous variables. Chi-square or Student’s t-tests were conducted to compare these characteristics between men and women. Generalized estimating equation (GEE) regression analyses were then performed to confirm the association between gender and each characteristic, after adjusting for the following main confounding factors: age, marital status, education level, length of homelessness, having SZ or BD, and a random effect for clusters (n=4 towns). Regression coefficients included adjusted odds ratios, and a standardized beta with a 95% confidence interval was reported. We also compared women with SZ and BD using chi-square, Student’s t-tests, and GEE. Given the numerous statistical tests, statistical significance was defined as p<0.01 in two-sided tests.
We conducted a path analysis using weighted least squares estimation to determine whether victimization of women might explain the poor clinical outcomes found in the previous analysis (ie, depression, suicide risk, physical status, and QoL). We constructed hypothetical relationships among these variables by examining previously published research and the results of univariate analyses. Coefficients are standardized path coefficients, that is, standardized versions of linear regression weights. The standardization involves multiplying the ordinary regression coefficient by the standard deviations of the corresponding explanatory variable. Model fit was evaluated using the chi-square test of model fit, the root mean square error of approximation (RMSEA), the comparative fit index (CFI), and the weighted root mean square residual (WRMR).Citation38 Statistical significance was defined as p<0.05 in two-sided tests.
The statistical analyses were performed using the SPSS version 20.0 software package and the R MCMC Generalised Linear Mixed Models package, and the path analysis was performed with Mplus version 6 software.
Results
Sociodemographic characteristics
Overall, 703 homeless people with SZ/BD, including 123 (17.5%) women, were recruited to participate in the trial. The mean age of the study participants was 38.8 years (standard deviation, SD =10.0). Most were French 575 (85.8%), single 521 (77.8%), and had no children 575 (85.8%) ().
Table 1 Sociodemographic and homeless trajectory characteristics based on gender in 703 homeless individuals
Compared to men, women were less likely to be single (67.5% vs 80.0%; p=0.004) and more likely to have a high school diploma or achieved an academic level (40.0% vs 24.1%; p=0.001). Almost half of the women (46.7%) had children compared to only 35.3% of men (p=0.026). No significant association of gender with total monthly income was found (p>0.05).
Mean lifetime duration of homelessness was lower in women than in men (6.6±6.9 years for women vs 9.0±8.0 for men; p=0.002). During the 6 months preceding inclusion in the study, women spent fewer nights in the streets than men (38.1±61.7 nights vs 57.3±69.4 nights; p=0.003).
Clinical characteristics and QoL
Women were more often diagnosed with BD than men (43.9% vs 27.9%, p<0.001). Overall, 59.0% of women were diagnosed with a current major depressive episode, 51.2% with current high suicide risk, and 25.7% with current PTSD. Compared to men, women were found to have higher rates of PTSD (25.7% vs 16.4%, p<0.001), higher suicide risk (51.2% vs 41.8%, p<0.001), and impaired QoL (43.4±17.7 vs 48.3±17.3; p<0.001). Moreover, women had significantly lower physical health status scores than men (47.9±11.4 vs 51.3±10.3; p<0.001) and higher rates of fractures and sprains in the past 6 months than men (11.3% vs 7.5%, p=0.002 and 22.6% vs 10.0%, p<0.001) ().
Table 2 Gender differences in mental and physical health comorbidities and self-reported health status and quality of life between the 123 homeless women and the 580 homeless men with schizophrenia (SZ) or bipolar disorders (BD)
Almost half of the patients (46.3%) had substance dependence issues, and almost 40% were dependent on alcohol but with no difference between genders.
Victimization in the past 6 months
Women were more likely than men to declare having been assaulted verbally (40.8% vs 28.5%; p<0.001), physically (34.2% vs 20.9%, p<0.001), and sexually (10.0% vs 1.8%, p<0.001) in the past 6 months ().
Table 3 A comparison of victimization in the past 6 months between the 123 women and the 580 men
Table 4 Differences and overlap of homeless women with schizophrenia and bipolar disorder – sociodemographic and homelessness trajectory characteristics
Table 5 Differences and overlap of homeless women with schizophrenia and bipolar disorder – mental and physical health comorbidities, self-reported health status, quality of life, and victimization
The impact of PTSD and victimization in homeless women
The path analysis is illustrated in . Our general hypothesis was that current PTSD and violent victimization in the past 6 months explained the poor clinical outcomes found in women, that is, higher depression and suicide risk and lower QoL and physical health status than men.Citation11,Citation13,Citation14,Citation39 Conversely, we expected a weaker link between nonviolent victimization and clinical outcomes in comparison with violent victimization. Finally, we expected that PTSD and violent victimization were weakly associated, as PTSD often precedes the first reported homeless episode and often results from antecedent victimization,Citation14,Citation40 while violent victimization is recent and often a direct consequence of being homeless.
Figure 1 Path analysis with posttraumatic stress disorder, violent victimization, depression, suicide risk, physical health status, and quality of life in homeless women.
Abbreviations: DF, degrees of freedom; CFI, comparative fit index; WRMR, weighted root mean square residual.
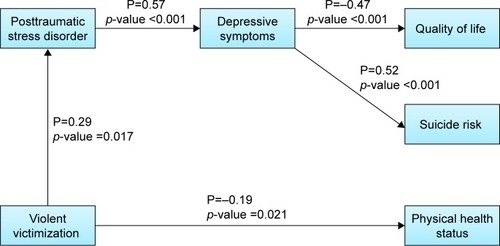
As expected, there was no effect of non-violent victimization on clinical outcomes. Conversely, the path analysis revealed moderate direct effects of violent victimization on PTSD (path coefficient =0.29, p=0.02) and impaired physical health status (path coefficient = −0.19, p=0.021). There was a direct and important effect of PTSD on depression (path coefficient =0.57, p<0.001), and depression was moderately associated with impaired QoL (path coefficient =−0.47, p<0.001) and higher suicide risk (path coefficient =0.52, p<0.001). Finally, the path analysis revealed several indirect effects from violent victimization on depression via PTSD (path coefficient =0.17), from PTSD to QoL (path coefficient =−0.27) and to suicide risk via depression (path coefficient =0.30).
This model showed satisfactory fit based on RMSEA =0.059, CFI =0.96, and WRMR =0.510.
Differences and overlap of homeless women with SZ and BD
Compared to women with SZ, women with BD were found to have higher rates of substance dependence and more severe symptomatology including depressive symptoms and more violent victimization ( and ).
Discussion
The results of the present study may be summarized as follows: in a consecutive sample of 703 homeless people with SZ or BD, 17.5% were women. Although women have shorter lengths of homelessness and higher education levels than men, they were at higher risk than men for PTSD, depression, suicide risk, and fractures and sprains, as well as for having been verbally, physically, and/or sexually assaulted in the past 6 months. PTSD and violent victimization may explain the high levels of depression, suicide risk, impaired physical status, and impaired QoL in homeless women. Homeless women with BD appeared even more vulnerable than women with SZ with high level of addiction, impaired health status, and more violent victimization.
Compared to homeless men, homeless women with SZ or BD have been found to have more verbal, physical, and sexual assault; PTSD; sprains and fractures. This result is consistent with studies carried out in non-selected samples of homeless people reporting that the street is much more violent for women than for men.Citation2,Citation41 Our study highlights that homeless women with SZ or BD are extremely vulnerable and/or exposed to violence. In addition, the path analysis reveals that violent victimization has important consequences for women’s health, leading to impaired physical health, higher PTSD, and depression. Hence, there is an urgent need to provide protection for homeless women with SZ or BD to protect them from violent victimization.
Homeless women with SZ or BD have more PTSD than men. The path analysis suggests that PTSD is associated with increased depression and suicide risk and deteriorated QoL. This analysis is consistent with a prior study suggesting that PTSD was associated with increased suicide risk among homeless individuals with substance use disorders.Citation42 This finding confirms the need to attend to PTSD and its mental consequences when addressing the array of needs of homeless women with SZ or BD.Citation14 Notably, the higher rate of PTSD in women is moderately associated with violent victimization in the past 6 months in homeless women with SZ or BD. To avoid a memory bias, only violent victimization during the past 6 months has been explored in the present study, and older victimization exposure may have thus been implicated in the high rate of PTSD found in the present sample. Victimization has been described as the major precipitating event in homelessness and homelessness as a risk factor for victimization.Citation40 More specifically, domestic violence has been suggested as one of the major causal factors for homelessness in women regardless of their mental health status.Citation40 Some authors have suggested that confounding factors such as childhood trauma are implicated in PTSD onset in adulthood, as well as in the genesis of homelessness.Citation42–Citation44 Mental health professionals have thus played an important upstream role in tracking homelessness and then preventing victimization in patients with mental disorders.Citation23
The present study has confirmed very high rates of alcohol dependence and substance use in this high need population, almost twice as high as that in the general homeless population (for alcohol dependence, 39% for the sample in the present study, 21% for the general homeless population, and 8.5% for the French general population; whereas for substance dependence, 46% for the sample in the present study, 17.5% for the general homeless population, and no data available for the French general population).Citation45 The rate of alcohol dependence in the present homeless sample was similar to that of the meta-analysis of Fazel et al (37%).Citation21 However, the proportion of substance dependence in the present study is almost twice as high as that found in Fazel et al (46% vs 24%), and men were found at higher risk for addiction in the Fazel et al meta-analysis, while no gender effect was found in the present study. The absence of a gender effect has also been found in a previous study conducted in the USA in 2011.Citation33 In other words, the present results suggest that homeless individuals with SZ or BD are at a 200% higher risk of substance dependence than the general homeless population and that women diagnosed with these mental disorders are at much higher risk of alcohol and substance dependence than other homeless women. This risk is even higher in homeless women with BD (49.1% of alcohol dependence and 54.7% of substance dependence), confirming the findings reported in a recent study on patients with BD.Citation46,Citation47 Therefore, public health services should pursue efforts for the prevention and care of addictive behavior in high need homeless people with SZ or BD, particularly in women with BD.
Several actions may be suggested regarding the results of the present study. First, depression, suicidal ideation, PTSD, and victimization should be systematically assessed during psychiatric evaluations of homeless women. Targeted intervention programs should now be widely disseminated for homeless women, as proposed in the Housing First programs.Citation48–Citation51 Second, more intensive programs such as assertive community assessment with a special attention to alcohol and substance dependence should probably focus on homeless women with BD. Last, specific prevention programs should be undertaken to protect homeless women from violent victimization but also upstream of homelessness. If these proposals require the involvement of medical and social professionals, homeless women’s conditions will never be resolved without the guidance from the government.
Limitations
The present study was based on retrospective data. No causal inference can be formally proposed, and our model should be interpreted from an associational point of view. Moreover, women with dependent/young children were excluded from the present study, which may limit the representativeness of the sample and may underestimate the proportion of women in the homeless population. Data were mostly self-declared and may have been underreported by participants because of having been humiliated as a victim. Future work should explore hetero-assessment, including interviewer-assessed scales such as the Multnomah Community ability scale. Finally, although our study accounts for a large set of potentially relevant variables, other important data should be collected in future studies (eg, history of childhood). Due to ethical concerns, ethnicity has not been reported in the present study. However, French nationality has been reported on and was not associated with gender.
Conclusion
The present study has clearly shown that homeless women with SZ or BD were more exposed to verbal, physical, and sexual violence, which may strongly impact their mental and physical health and QoL and increase their risk of suicide. Future longitudinal studies should confirm these findings, but the urgency should be noted by policymakers to support the development of specific interventions to protect this particularly vulnerable subgroup.
Author contributions
AT, VG, and PA involved in conception and design of the study and study coordination. VG and AT contributed to inclusion and clinical data collection. AT, LB, SL, and MB analyzed the data. AT, LB, GF, and PA contributed to interpretation of data. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
We would like to thank the following people for their help: A Albisson, P Allenou, K Baumstark, E Beetlestone, J Billard, E Bourlier, JM Colucci, T Danel, J Debieve, A Djena, J Dupont, P Estecahandy, D Flahaut, C Fortanier, G Guetière, P Hérédia-Rodier, E Jouet, E Labeyrie, M Lefèbvre, JM Legagneux, A Loundou, F Olive, C Psarra, E Requier, D Sauze, E Simonnet, G Suderie, A Troisoeufs, PP Vandini, B Vincent, and R Wulfman.
Finally, we would like to thank the Canadian At Home/Chez Soi team for help and advice in developing the French Housing First program.
This work was supported by institutional grants from the 2011 Programme Hospitalier de Recherche Clinique National and the French Ministry of Health (Direction Générale de la Santé), as well as grants from Janssen Pharmaceutical Companies and the Fondation de France (PHRC-12-024-0278, Afssaps B110684-50, Comité de Protection des Personnes 2011-A00668-33).
Disclosure
The sponsor was represented by Assistance Publique, Hôpitaux de Marseille, France; its role was to control the appropriateness of the ethical and legal considerations. The authors report no other conflicts of interest in this work.
References
- YaouancqFLebrèreAMarpsatMRégnierVLegleyeSQuagliaML’hébergement des sans-domicile en 2012. Des modes d’hébergement différents selon les situations familiales [Accommodation of the homeless people in 2012. Different types of accommodation depending on the family situation]INSEE Première2013145514 French
- Pierre-MarieERogerSChausseMLabradorJLes sans-domicile dans l’agglomération parisienne: une population en très forte croissance [The homeless people in the Parisian metropolitan area: a very strong growth population]Population201442314 French
- SikichKWGlobal woman homelessness: a multi-faceted problemGend Issues2008253147156
- WatsonSWomen and housing or feminist housing analysis?Hous Stud198611110
- WhitzmanCMaking the invisible visible: Canadian women, homelessness, and health outside the “big city”Finding Home: Policy Options for Addressing Homelessness in Canada2010 Available from: http://www.homelesshub.ca/sites/default/files/4.3%20Whitzman%20Homelessness%20Outside%20the%20Big%20City.pdfAccessed December 15, 2017
- NealeJHomelessness and theory reconsideredHous Stud19971214761
- SandercockLMaking the Invisible Visible: A Multicultural Planning HistoryUniversity of California PressOakland, California1998294
- EdgarBDohertyJWomen and Homelessness in Europe: Pathways, Services and ExperiencesPolicy PressBristol, UK2001
- Gomes do Espirito SantoMEPerrineALBonaldiCGuseva-CanuICaractéristiques et état de santé des femmes sans-domicile nées en France et à l’étranger : résultats de l’enquête Insee–Ined 2012 [Characteristics and health status of homeless women born in France and abroad: results of Insee-Ined 2012 survey]Rev Epidemiol Sante Publique2018662135144 French29429602
- HodginsSLincolnTMakTExperiences of victimisation and depression are associated with community functioning among men with schizophreniaSoc Psychiatry Psychiatr Epidemiol200944644845719030767
- NorthCSSmithEMSpitznagelELViolence and the homeless: an epidemiologic study of victimization and aggressionJ Trauma Stress199471951108044446
- GoodmanLSaxeLHarveyMHomelessness as psychological trauma. Broadening perspectivesAm Psychol19914611121912251772159
- NorthCSSmithEMPosttraumatic stress disorder among homeless men and womenHosp Community Psychiatry19924310101010161398564
- TaylorKMSharpeLTrauma and post-traumatic stress disorder among homeless adults in SydneyAust N Z J Psychiatry200842320621318247195
- RoyLCrockerAGNichollsTLLatimerEAAyllonARCriminal behavior and victimization among homeless individuals with severe mental illness: a systematic reviewPsychiatr Serv201465673975024535245
- BrowneAFamily violence and homelessness: the relevance of trauma histories in the lives of homeless womenAm J Orthopsychiatry19936333703848372904
- Association Femmes SDFVanneuvilleMCFemmes en errance: De la survie au mieux-être [Women in wandering: from survival to well-being]Chronique Sociale2004118 French
- JasinskiJLWeselyJKWrightJDMustaineEEHard Lives, Mean Streets: Violence in the Lives of Homeless WomenFirst editionBostonSage Publications2010208
- HoffmanLCoffeyBDignity and indignation: how people experiencing homelessness view services and providersSoc Sci J200845207222
- BreakeyWRFischerPJKramerMHealth and mental health problems of homeless men and women in BaltimoreJAMA198926210135213572761036
- FazelSKhoslaVDollHGeddesJThe prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysisPLoS Med2008512e22519053169
- FolsomDJesteDVSchizophrenia in homeless persons: a systematic review of the literatureActa Psychiatr Scand2002105640441312059843
- WalshEMoranPScottCPrevalence of violent victimisation in severe mental illnessBr J Psychiatry200318323323812948997
- TeplinLAMcClellandGMAbramKMWeinerDACrime victimization in adults with severe mental illnessArch Gen Psychiatry20056291192116061769
- TinlandAFortanierCGirardVEvaluation of the Housing First program in patients with severe mental disorders in France: study protocol for a randomized controlled trialTrials20131430924063556
- American Psychiatric AssociationDiagnostic and Statistical Manual of Mental Disorders4th ed. Text revisedWashington, DCAmerican Psychiatric Association2000
- BarkerSBarronNMcFarlandBHBigelowDAA community ability scale for chronically mentally ill consumers: Part I. Reliability and validityCommunity Ment Health J19943043633837956112
- BarkerSBarronNMcFarlandBHBigelowDACarnahanTA community ability scale for chronically mentally ill consumers: Part II. ApplicationsCommunity Ment Health J19943054594727851100
- JesteDVSaksEDecisional capacity in mental illness and substance use disorders: empirical database and policy implicationsBehav Sci Law20062460762816883611
- GirardVSarradon-EckAPayanNThe analysis of a mobile mental health outreach team activity: from psychiatric emergencies on the street to practice of hospitalization at home for homeless peoplePresse Med2012415e226e237 French22244723
- AmoreKBakerMHowden-ChapmanPThe ETHOS definition and classification of homelessness: an analysisEur J Homelessness2011521937
- SheehanDVLecrubierYSheehanKHThe Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10J Clin Psychiatry199859Suppl 202233 quiz 4–57
- ConradKJYagelkaJRMattersMDRichARWilliamsVBuchananMReliability and validity of a Modified Colorado Symptom Index in a national homeless sampleMent Health Serv Res20013314115311718206
- LeplegeAEcosseEVerdierAPernegerTVThe French SF-36 Health Survey: translation, cultural adaptation and preliminary psychometric evaluationJ Clin Epidemiol19985111101310239817119
- BoyerLSimeoniMCLoundouAThe development of the S-QoL 18: a shortened quality of life questionnaire for patients with schizophreniaSchizophr Res20101211–324125020541912
- GirardVTinlandABoucekineMValidity of a common quality of life measurement in homeless individuals with bipolar disorder and schizophreniaJ Affect Disord201620413113727344622
- AuquierPTinlandAFortanierCToward meeting the needs of homeless people with schizophrenia: the validity of quality of life measurementPLoS One2013810e7967724205390
- GamborgMJensenGBSorensenTIAndersenPKDynamic path analysis in life-course epidemiologyAm J Epidemiol20111731131113921415031
- WhitbeckLBArmentaBEGentzlerKCHomelessness-related traumatic events and PTSD among women experiencing episodes of homelessness in three U.S. CitiesJ Trauma Stress201528435536026184885
- FischerPJVictimization and homelessness: cause and effectN Engl J Public Policy199281229246
- GoodmanLSaxeLHarveyMHomelessness as psychological trauma. Broadening perspectivesAm Psychol19914611121912251772159
- BenderKBrownSMThompsonSJFergusonKMLangenderferLMultiple victimizations before and after leaving home associated with PTSD, depression, and substance use disorder among homeless youthChild Maltreat201520211512425510502
- SundinECBaguleyTPrevalence of childhood abuse among people who are homeless in Western countries: a systematic review and meta-analysisSoc Psychiatry Psychiatr Epidemiol201550218319425178273
- SlesnickNZhangJBrakenhoffBHomeless youths’ caretakers: the mediating role of childhood abuse on street victimization and housing instabilitySoc Work201661214715427180525
- LaporteALe MénerEChauvinPLa santé mentale et les addictions chez les personnes sans logement: phantasmes et réalités [Mental health and addictions in people without housing: fantasies and realities]Soins à domicile201022113032 French
- MaremmaniAGBacciardiSGehringNDThe impact of mood symptomatology on pattern of substance use among homelessJ Affect Disord201517616417025723559
- MaremmaniAGBacciardiSGehringNDSubstance use among homeless individuals with schizophrenia and bipolar disorderJ Nerv Ment Dis2017205317317726785056
- AubryTGoeringPVeldhuizenSA multiple-city RCT of housing first with assertive community treatment for homeless Canadians with serious mental illnessPsychiatr Serv201667327528126620289
- GoeringPNStreinerDLPutting housing first: the evidence and impactCan J Psychiatry2015601146546626720503
- HwangSWBurnsTHealth interventions for people who are homelessLancet201438499531541154725390579
- LyALatimerEHousing first impact on costs and associated cost offsets: a review of the literatureCan J Psychiatry2015601147548726720505

