Abstract
Mood disorders are a major public health problem and are associated with considerable burden of disease, suicides, physical comorbidities, high economic costs, and poor quality of life. Approximately 30%–40% of patients with major depression have only a partial response to available pharmacological and psychotherapeutic interventions. Complementary and alternative medicine (CAM) has been used either alone or in combination with conventional therapies in patients with mood disorders. This review of the literature examines evidence-based data on the use of CAM in mood disorders. A search of the PubMed, Medline, Google Scholar, and Quertile databases using keywords was conducted, and relevant articles published in the English language in the peer-reviewed journals over the past two decades were retrieved. Evidence-based data suggest that light therapy, St John’s wort, Rhodiola rosea, omega-3 fatty acids, yoga, acupuncture, mindfulness therapies, exercise, sleep deprivation, and S-adenosylmethionine are effective in the treatment of mood disorders. Clinical trials of vitamin B complex, vitamin D, and methylfolate found that, while these were useful in physical illness, results were equivocal in patients with mood disorders. Studies support the adjunctive role of omega-3 fatty acids, eicosapentaenoic acid, and docosahexaenoic acid in unipolar and bipolar depression, although manic symptoms are not affected and higher doses are required in patients with resistant bipolar depression and rapid cycling. Omega-3 fatty acids are useful in pregnant women with major depression, and have no adverse effects on the fetus. Choline, inositol, 5-hydroxy-L-tryptophan, and N-acetylcysteine are effective adjuncts in bipolar patients. Dehydroepiandrosterone is effective both in bipolar depression and depression in the setting of comorbid physical disease, although doses should be titrated to avoid adverse effects. Ayurvedic and homeopathic therapies have the potential to improve symptoms of depression, although larger controlled trials are needed. Mind-body-spirit and integrative medicine approaches can be used effectively in mild to moderate depression and in treatment-resistant depression. Currently, although CAM therapies are not the primary treatment of mood disorders, level 1 evidence could emerge in the future showing that such treatments are effective.
Introduction
Treating mood disorders has become complex, given the many changes over the years in epidemiological trends, etiological models, classification systems and symptom clusters, diagnosis and diagnostic tools, types of interventions, and outcome studies. Despite psychopharmacological advances during the past six decades, the management of major depression and other mood disorders continues to challenge mental health providers. Many patients with mood disorders who are dissatisfied with conventional treatment seek other interventions, in particular complementary and alternative medicine (CAM). In general, CAM is safe and cost-effective, has limited comparative efficacy to modern allopathic treatments, and is well tolerated by patients with physical and mental disorders.Citation1 This evidence-based review summarizes recent advances in the use of CAM for mood disorders, mainly in the adult population.
Literature search
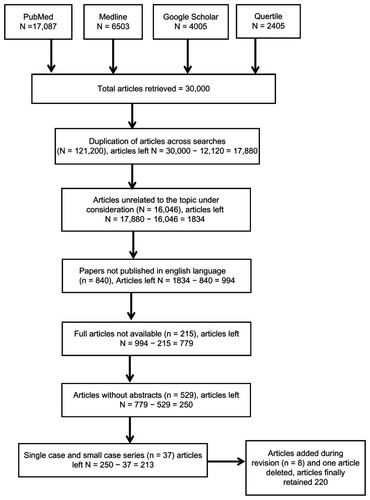
A search of the PubMed, Medline, Google Scholar, and Quertile databases was done using the key phrases “complementary and alternative medicine” and “integrative medicine combined with mood disorders and major depression”, and relevant articles published over the past two decades (1992–2012) in the peer-reviewed English language journals were retrieved. Other keywords, including “botanicals”, “phytomedicine”, “nutrients”, “herbs”, “dietary supplements”, “vitamins”, “fatty acids”, “folate”, “hormones”, “exercise”, “meditation”, “yoga”, “Ayurveda”, “homeopathy”, and “mind-body-spirit” were combined with “major depression” and “mood disorders” for more specific searches. More than 30,000 articles were retrieved using this method. Many articles were excluded, including articles without abstracts (n = 529), papers not published in the English language (n = 840), full articles not being available (n = 215), and duplication of articles across searches (n = 12,120), along with many papers unrelated to the topic under consideration (n = 16,046). Only 250 papers were retained for further review. Thirty-seven articles that described single cases and small case series (less than five subjects) were also excluded. In total, the authors selected 213 articles, which included open-label clinical trials, randomized controlled trials, systematic reviews, and meta-analyses addressing use of CAM in the management of major depression and other mood disorders. Eight references were added during revisions of this manuscript and one citation was deleted (see ).
Mood disorders
Mood disorders are common mental health problems, afflicting 154 million people around the world.Citation2 Major depression is currently the third leading cause of disability worldwide. Major depression is preferentially associated with female gender, with manic disorders distributed equally between males and females. Major depression is more common among people of low socioeconomic status, those with low education, those who are unmarried, separated, or divorced, those from a rural background, and those without intact families.Citation3 Major depression has adverse consequences, including increased absenteeism from work, reduced productivity, disruption of family life, and increased health care utilization and costs. Smoking, drug abuse, sexual dysfunction, crime, violence, and suicidal behavior are further consequences for many sufferers.Citation4–Citation6 In addition, mood disorders are the most common cause of premature mortality, acceleration of aging, and reduced life expectancy.Citation7
Mood disorders exist in many forms, including unipolar depression, bipolar depression, mania, mixed syndromes, and subsyndromes, and these conditions can co-occur with other psychiatric and physical disorders.Citation8–Citation10 Comorbid conditions complicate not only the diagnosis but also the management, prognosis, and outcome of major depression.Citation11
Psychopharmacological and nondrug therapies are effective in many patients with mood disorders. However, 30%–40% of patients with major depression become resistant to these treatments as a result of medical comorbidity, unavailability of appropriate services, and poor adherence with available therapies. These difficult-to-treat patients need specialized treatment strategies.Citation12,Citation13 The two major classifications of mental disorders provide a comprehensive view of mood disorders, but these have now been divided into more than 30 diagnostic categories.Citation14,Citation15 Major depression has a definite onset, is strongly influenced by biological and psychosocial factors,Citation3,Citation16,Citation17 and is also related to personality disorders.Citation18 Preclinical studies in animals and basic neurobiological research in human subjects have provided biological insights into the pathogenesis of major depression, and have helped in the development of drugs now used in major depression and other mood disorders.Citation19,Citation20
Nondrug interventions have also been developed to treat major depression, in view of the influence of psychosocial factors.Citation21 Dacher described four healing systems, ie, homeostatic, conventional, mind-body, and spiritual.Citation21 Sarris has also described an antidepressant-lifestyle-psychological-social model for treating depression that integrates conventional drug treatments with CAM, lifestyle changes, and psychosocial techniques.Citation22 A combination of biological and psychosocial treatment produces better outcomes and reduces the rates of relapse and suicide.Citation23 From a psychopharmacological perspective, there have been many controlled trials in mood disorders consistently reporting that 30% of patients achieve full remission, 30% are partial responders, and the rest are nonresponders.Citation24,Citation25 However, application of these results in the real-world setting is problematic because of the criteria used to select patients for entry into these trials. In a naturalistic study of 4000 patients with chronic depression and comorbid psychiatric or medical conditions treated with citalopram up to 60 mg/day, the remission rate was 27% and the response rate was 47%. When nonresponders were augmented or switched to another antidepressant, 30% remitted.Citation26 According to Bambauer et al, patients with treatment-resistant depression attributable to nonadherence with medicationCitation27 need augmentation strategies.Citation12,Citation13 Patients with treatment-resistant depression are also at higher risk for relapse.Citation28,Citation29
Complementary and alternative medicine
Increasing attention is being paid worldwide to more traditional medical systems, including Ayurveda, yoga, naturopathy, Unani medicine, Siddha, and homeopathy.Citation30 Use of CAM therapies in various illnesses is on the rise.Citation31 Perron et al found that barriers to conventional treatment have contributed to the increased use of CAM in mentally ill patients.Citation31 Another study found that use of CAM was unaffected by the perceived effectiveness of conventional treatment or compliance with medication among persons with bipolar disorder.Citation32 There are now more than 120 CAM treatments available (), all of which involve body, mind, and spiritual concepts. This classification of various therapies, and designated by mind, body, or spirit, is perceived as strict compartmentalization, but many of the therapies mentioned have double or triple designations in terms of our theoretical understanding of diagnosis, treatment, and causal mechanisms. Another reason for increasing use of CAM is the positive findings of studies in patients with major depression.Citation33 Many clinical trials of CAM are presently under way worldwide, and are expected to yield positive results in patients with major depression and other mood disorders.
Table 1 Complementary and alternative treatment modalitiesCitation34–Citation36
Role of CAM in mood disorders
Complementary and alternative medicine is the most practiced but least researched form of treatment because of the complexities inherent in assessment of its effectiveness in major depression and other mood disorders. These complexities include solo versus adjunctive treatments, the multiple facets of depression, design and methodological issues, and use of herbs with unknown bioactive ingredients. To address this conundrum, the Canadian Network Group has developed guidelines for the use of CAM in adults with major depression, suggesting efficacy using light therapy for seasonal affective disorder, St John’s wort for mild to moderate depression (level 1 evidence), and omega-3 fatty acids, yoga, exercise, sleep deprivation, and S-adenosylmethionine for major depression.Citation37 Level 1 evidence is that obtained from at least one appropriately designed randomized controlled trial. The American Task Force has also reported promising results with regard to omega-3 fatty acids, St John’s wort, folate, S-adenosylmethionine, acupuncture, light therapy, exercise, and mindfulness psychotherapies in major depression.Citation38 This report recommends the undertaking of more rigorous and larger studies in the future, and that each CAM treatment must be evaluated separately in adequately powered controlled trials. They suggested that further focus is needed on clinical, research, and educational initiatives with regard to CAM in psychiatry, and cautions that the greatest risk of pursuing CAM is possible delayed use of other well established treatments.Citation38 Dutch researchers have also developed a protocol for ensuring safe and effective use of CAM in the mental health setting.Citation39
Dietary supplements as CAM therapies
Over-the-counter dietary supplements (nutraceuticals) are used extensively by patients with depression, and are categorized as nutrients, herbal and dietary supplements, and traditional and nontraditional methods.Citation40 Nutraceuticals have also been used to promote mental and physical health, to prevent illness, and to treat diseases, with substantial benefits.Citation40 Nutraceuticals, in particular S-adenosylmethionine, have benefited patients with major depression and other mood disorders. This compound provides methyl and sulfate groups used in the synthesis of deoxyribonucleic acid, proteins, phospholipids, neurotransmitters, and the antioxidant, glutathione, that are disturbed in people with mood disorders.Citation41 In a critical review of the literature, Brown et al reported the results of 48 studies and found S-adenosylmethionine to be safe and effective for the treatment of depression.Citation42 A recent review further supports the use of this compound in mild-to-moderate depression, reporting that eight of 14 studies (57%) produced positive results.Citation43 Interestingly, like selective serotonin reuptake inhibitors (SSRIs), neither S-adenosylmethionine nor St John’s wort have been associated with an increased risk of suicide.Citation43 Several researchers have appraised the clinical and pharmacological benefits of S-adenosylmethionine in depression and as an adjunct in treatment-resistant depression.Citation44–Citation46 In a double-blind randomized study of patients with depression who were nonresponders to SSRIs, Papakostas et al reported preliminary beneficial effects from S-adenosylmethionine augmentation with good tolerability. S-adenosylmethionine appears to be a safe adjunctive treatment for patients with major depression who do not respond to SSRIs, but this needs confirmation in clinical trials.Citation47 S-adenosylmethionine alone or combined with other supplements has been shown to alleviate depression associated with musculoskeletal disease,Citation48,Citation49 liver disease,Citation50,Citation51 Parkinson’s disease,Citation52 and human immunodeficiency virus/acquired immune deficiency syndrome.Citation53 S-adenosylmethionine acts similarly to noradrenergic antidepressants, but with fewer side effects.Citation44
In a randomized clinical study of 30 women with postpartum depression, 1600 mg/day of S-adenosylmethionine resulted in a 70% reduction in symptoms of depression and anxiety compared with a 50% reduction in the placebo group by day 30.Citation54 S-adenosylmethionine is safe to use during pregnancy and breast-feeding. Infants naturally have 3–7 times higher S-adenosylmethionine levels than adults.Citation55 This is because they need more S-adenosylmethionine for methylation of the developing brain, especially the myelin sheaths critical for conduction of electrical impulses. A secondary analysis of clinical trial data for S-adenosylmethionine administered to patients with major depression nonresponsive to SSRIs found a positive impact on symptoms of depression and related cognitive dysfunction.Citation56 In summary, the primary and adjunctive role of S-adenosylmethionine in patients with major and treatment-resistant depression is gaining solid ground.
Herbs and mood disorders
Numerous herbs are known to contain bioactive substances, although the clinical significance of these needs further investigation.Citation57 Research in phytomedicine has been generating considerable amounts of new data on the chemical, pharmacological, and clinical aspects of herbs in mood disorders.Citation58,Citation59
St John’s wort
St John’s wort contains two bioactive substances, ie, hyperforin and hypericin, and has been used effectively in the treatment of major depression.Citation57 Although initial reports of its use were hampered by inadequate concentrations of hyperforin,Citation60 subsequent comparative, randomized, double-blind, placebo-controlled trials using better standardized St John’s wort (Kira® [LI-160 extract], 1800 mg/day, Klosterfrau Healthcare Group, Germany; Remotiv®, Flordis Natural Medicines, Australia; or Ze 117®, 500 mg/day Zeller AG, Switzerland) found it to be as effective as imipramine 150 mg/day and fluoxetine 20 mg/day for all severity levels of depression, but with fewer gastrointestinal side effects.Citation61,Citation62 A widely cited randomized, multicenter, placebo-controlled study of inpatients with depression given St John’s wort Kira® (LI-160 extract) 900 mg/day for 4 weeks, then increased to 1200 mg/day for another 4 weeks, found Kira® (LI-160 extract) to be no better than placebo. However, this negative result could be explained by the use of subtherapeutic doses of the bioactive substances in St John’s wort.Citation63 The greater severity and resistant nature of depression might also have contributed to lack of effectiveness, but this is unlikely, given the results from Phase II of the study.Citation64 In another study of severely depressed patients given Kira® (LI-160, 900–1500 mg/day), sertraline (50–100 mg/day), or placebo, found that neither sertraline nor St John’s wort showed more efficacy than placebo.Citation65 In a randomized, placebo-controlled multicenter study of outpatients with mild-to-moderate depression, Kira® (LI-160 extract) and fluoxetine did not differ significantly with regard to efficacy measures except for remission rates (24% for Kira® [LI-160 extract], 28% for fluoxetine, and 7% for placebo). It was concluded that Kira® (LI-160 extract) and fluoxetine were no more effective than placebo in the short-term treatment of mild-to-moderate depression.Citation66 The results of this study are supported by other researchers.Citation67
In another randomized study of patients with major depression, Kira® (LI-160 extract, 900 mg/day) was more effective than fluoxetine (20 mg/day) and showed a trend towards superiority over placebo.Citation68 The remission rates were higher for Kira® (LI-160 extract) compared with fluoxetine and placebo.Citation68 A reanalysis of earlier data suggested that patients’ beliefs regarding treatment may have a stronger effect on clinical outcome than the actual medication received, depending on what treatment patients thought they were receiving and what they actually received.Citation69 Recent well controlled studies, meta-analyses, and consensus guidelines support the efficacy of St John’s wort in patients with mild-to moderate-depression in particular.Citation33,Citation37,Citation43,Citation70,Citation71
In another double-blind, randomized, placebo-controlled, long-term trial, Kasper et alCitation70 reported the beneficial effects of Hypericum extract (WS® 5570, Dr. Willmar Schwabe Pharmaceuticals, Germany) in adult outpatients who had recovered from an acute episode of moderate depression. Patients treated with WS® 5570 showed more favorable time courses to resolution of symptoms and greater overall improvement than those randomized to placebo. Used as long-term maintenance therapy, WS® 5570 was reported to have a prophylactic effect in patients with early-onset depression and in those with a high degree of chronicity. WS® 5570 also showed a beneficial effect in preventing relapse after recovery from acute depression.Citation70
St John’s wort has also been used in primary care psychiatric settings and in patients with seasonal affective disorder, and examined with regard to relapse rates in those who responded, all with good results. For example, Szegedi et al reported that 71% of patients with moderate-to-severe depression treated in primary care responded to 900 mg/day Hypericum extract WS® 5570, and that 900–1800 mg/day was as effective as paroxetine 20–40 mg/day, but without side effects.Citation72 Patients with mild seasonal affective disorder have also been reported to benefit from Kira® (LI-160 extract).Citation37,Citation73 With regard to relapse, reanalysis of data from 154 patients with mild-to-moderate depression treated with St John’s wort (STW 3-VI; Laif®, Steigerwald Arzneimittelwerk GmbH, Germany) 900 mg, citalopram 20 mg, or placebo once daily found that relapse rates were highest in the citalopram group, followed by the St John’s wort and placebo groups, with no difference in the severity of relapse.Citation74 Further, the duration of response was longest for the St John’s wort group, intermediate for the citalopram group, and shortest for the placebo group. Researchers concluded that 3-VI had the longest duration of response and was more effective than citalopram and placebo in decreasing relapse and recurrence rates.Citation74 However, in a 12-week study of minor depression, St John’s wort (Cederroth International, Sweden, 810 mg/day) was not superior to citalopram 20 mg/day or placebo, and the authors called for more research to identify better treatment options for patients with minor depression.Citation75 In a review of commonly used botanicals in the treatment of anxiety and mood disorders, St John’s wort (5 of 7 trials), black cohosh (all studies reviewed), and ginseng (1 trial) have been reported to improve symptoms of depression and anxiety in menopausal and postmenopausal women.Citation76
St John’s wort is generally used as a second-line option, except in women with a history of response to low doses of an SSRI.Citation57 St John’s wort has potential side effects that increase with higher doses. These include phototoxic rash, SSRI-like effects, serotonin syndrome, and induced mania.Citation77 The side effect profile and dropout rates in the range of 0%–5.7% for patients receiving St John’s wort are not different from placebo, and have been reported to be similar to those of tricyclic antidepressants and slightly lower than those of the SSRIs.Citation77 A study that reanalyzed data from four clinical trials found that St John’s wort extract (WS® 5570) was associated with fewer adverse events than SSRIs.Citation78 Nevertheless, St John’s wort reduces circulating levels of a large number of drugs, including digoxin, warfarin, and oral contraceptives, because it induces cytochrome P450 (CYP) 3A4 and CYP 1A2 enzymes as well as P-glycoprotein in the intestinal wall.Citation77,Citation79 According to one study, the information available on websites selling St John’s wort is not of good quality and consumers should bear this in mind when considering buying the product.Citation80 Another study that evaluated safety information provided in the labeling of St John’s wort products found that the majority of producers failed to address safety issues adequately.Citation81 Health care providers and consumers will benefit if the US Food and Drug Administration and similar regulatory bodies elsewhere re-examine the labeling requirements for dietary supplements.Citation81
Rhodiola rosea
The use of medicinal herbs had been widespread across many cultures since ancient times. A recent university student surveyCitation83 found that most herb use was self-prescribed (60%) and undisclosed to health providers (75%), 34% of users took herbs to treat a mood disorder, 13% of herb users were taking concurrent prescription medication, and those who took both herbs and prescription medications had higher depression and anxiety scores than other herb users. Detailed patient interviews are necessary to prevent adverse herb-drug interactions.Citation82
Rhodiola rosea, recommended in many conditions, including irregular menopause,Citation83,Citation84 has also been reported to be effective in the treatment of mild-to-moderate depression.Citation85 One trial used a standardized extract of Rhodiola rosea (SHR-5, Swedish Herbal Institute, Sweden) at doses of 340 mg and 680 mg daily for six weeks with no reports of side effects.Citation85 A systematic review has also supported the antidepressant effects of Rhodiola rosea.Citation86 Its mechanism of action in major depression is thought to be via beta-endorphins, tryptophan, and serotonin in the brain.Citation57,Citation88 Rosiridin is the bioactive ingredient of Rhodiola rosea, which is reported to inhibit monoamine oxidases A and B and may also be useful in dementia.Citation83
Having no addictive potential, Rhodiola rosea is a mild stimulant, so should be taken in the morning to avoid sleep problems. It may induce temporary vivid dreams and mild nausea. It also binds with the estrogen receptor, so women with a personal or family history of estrogen-sensitive breast cancer should exercise caution in using Rhodiola rosea, although this issue needs further study.Citation88 Products containing 3% rosavins and 1% salidrosides were found to be effective in a randomized controlled trial, and may be used to enhance the clinical effectiveness of Rhodiola rosea.Citation57 Panossian et al provide detailed information on its traditional use, chemical composition, pharmacology, side effect profile, and clinical efficacy.Citation84
Saffron and other herbs
A systematic review of herbs used in major depression and other mood disorders identified nine clinical trials that met all eligibility criteria.Citation89 Three of these trials found saffron stigma extract to be more effective than placebo and equivalent in effect to fluoxetine and imipramine. Two studies found that saffron petal extract was significantly more effective than placebo and was equivalent to fluoxetine and saffron stigma extract. Lavender was found to be less effective than imipramine, but the combination of lavender and imipramine was significantly more effective than imipramine alone. When compared with placebo, Echium extract was found to decrease depression scores markedly at week 4, although this effect had disappeared by week 6. According to this review, saffron, lavender, Echium, and Rhodiola rosea when used alone or in combination with antidepressants showed good results in mild-to-moderate depression.Citation89 Another critical review that identified 21 phytomedicines and 66 clinical trials involving 11 phytomedicines reported positive results of the aforementioned herbs in mild-to-moderate depression, anxiety, and sleep disorders.Citation90 In a clinical trial of Free and Easy Wanderer Plus (FEWP, Golden Flower, People’s Republic of China; a Chinese herbal extract formula), fluoxetine, and placebo, 150 patients with post-stroke depression showed significant improvement with both FEWP and fluoxetine compared with placebo.Citation91 At the end of the trial, subjects on FEWP showed greater improvement than those on fluoxetine at week 2 and performed better than patients receiving fluoxetine in activities of daily living. This study suggests that FEWP can be used safely with few side effects in patients with post-stroke depression.Citation91
Caution is important when using herbs and dietary supplements. Rai et alCitation92 analyzed the heavy metal content in nine plant species used for the preparation of herbs in India and found that most samples had a heavy metal content exceeding the upper limits set by the World Health Organization. Further, heavy metals and organochlorine pesticides have been found in some dietary supplements in the US.Citation93 In traditional Chinese medicine (), cases of heavy metal poisoning has been reported by several investigators.Citation94 There is a large body of literature concerning the heavy metal content of herbal supplements used in CAM, including mercury, lead, chromium, cadmium, arsenic, cobalt, and pesticides, including dioxin.Citation95–Citation100 Quality control measures, including standardized doses and regulations, are needed for herbal products used for health reasons.Citation40
Table 2 Herbal medicinal products: contaminants and adverse effectsCitation93–Citation101
Vitamins in mood disorders
Vitamins B and D, folate, and trace elements are essential for the functioning of neurons, and have been shown to afford protection against certain types of mental disorders, particularly depression.Citation101 These nutrients become depleted in the body for many reasons, including poor nutrition, chronic disease, old age, stress, and polymorphism. Low vitamin B12, vitamin D, and folate levels are also associated with poor memory and cognitive dysfunction.Citation102,Citation103 Folic acid and folate from the diet are converted into L-methylfolate in the body. In a randomized, double-blind, placebo-controlled trial, 123 patients with major depression and schizophrenia maintained on standard psychotropic medications were given augmentation therapy of methylfolate 15 mg/day or placebo. The investigators reported significant improvement in clinical and social symptoms with methylfolate compared with placebo.Citation104 However, treatment with folate or vitamin B12 alone has been associated with mixed results in depression. Geriatric patients with depression and cognitive dysfunction showed benefit when tricyclic antidepressants were augmented with vitamin B complex (B1, B6, and B12) and folate.Citation105 Nonresponse to antidepressants has been linked with low levels of folate. A study of 127 patients on fluoxetine supplemented with folate 400 mg/day or placebo reported a 94% response rate to fluoxetine plus folate compared with a 61% response to fluoxetine plus placebo.Citation106 However, a recent placebo-controlled study found little support for B12 (100 μg/day) with folate (400 μg/day) supplementation in community-dwelling adults already taking conventional antidepressants.Citation107 Another placebo-controlled trial of folate plus vitamin B12 supplementation given to older patients with depression also yielded negative results.Citation108
In summary, clinical trials of vitamin B and folate have yielded equivocal results in patients with major depression. Although methylfolate and vitamin B have favorable safety profiles, allergic reactions may occur using these substances. Folate and vitamin B reduce homocysteine levels, so may be cardioprotective. However, combination of these vitamins may cause restenosis of stents in men by stimulating endothelial proliferation, although this effect has not been seen in women.Citation109
Low levels of vitamin D have been identified in patients with major depressive and other mood disorders, but vitamin D supplementation in these patients has produced inconsistent results.Citation110 Supplemental use of vitamin D (800 International Units; IU) produced no positive results in a study of prevention of winter-time blues in elderly women.Citation111 In a placebo-controlled study, obese men and women with major depressive disorder were given high doses of vitamin D (20,000 or 40,000 IU) or placebo per week for one year. Depression scores were higher in patients with low serum 25-hydroxyvitamin D (<40 nmol L) levels than in those with normal levels of 25-hydroxyvitamin D (≥40 nmol L), and participants given the vitamin D supplement showed significant improvement in depression compared with those in the placebo group.Citation112 However, a recent placebo-controlled study of vitamin D3 supplementation in patients with low or high levels of 25-hydroxyvitamin D found that levels of 25-hydroxyvitamin D was significantly lower in patients with depression and that supplementation with vitamin D3 was not associated with improvement in symptoms compared with placebo.Citation113 Similarly negative results were reported for another placebo-controlled trial in elderly women with symptoms of depression given vitamin D3 supplementation at 400 IU/day and calcium.Citation114 However, a recent review suggests that the suicide risk associated with vitamin D deficiency might be reduced by supplementation with vitamin D.Citation115
Other nutrients commonly used in CAM include omega-3 fatty acids, choline, 5-hydroxy-L-tryptophan, inositol, and N-acetylcysteine. These substances are important in functioning of the neural networks involved in mood regulation.
Omega-3 fatty acids in mood disorders
Fish-derived omega-3 fatty acids provide eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), which help to maintain fluidity of the cell membrane, reduce inflammatory eicosanoids, and prevent the release of proinflammatory cytokines.Citation57,Citation116 Alpha linoleic acid also converts differentially into omega-3 fatty acids, EPA, and DHA. However, omega-6 fatty acids from domesticated animals and cultivated vegetables is consumed in much larger quantities than omega-3 fatty acids. Therefore, cell membranes acquire increasing proportions of omega-6 fatty acids that adversely affect membrane fluidity and flexibility.Citation57,Citation116 In contrast, supplementation of omega-3 fatty acids from fish oil in liquid or capsule form maintains cell membrane fluidity. Substitution of omega-6 fatty acids for omega-3 fatty acids in the cell membrane has been associated with unipolar and bipolar depression, which is thought to be due to loss of membrane fluidity and flexibility. The latter results in disturbance of membrane proteins, such as enzymes, receptors, ion channels, and neurotransmitters, which in turn increases levels of inflammatory eicosanoids and proinflammatory cytokines.Citation57,Citation116 In fact, a study of 12 women with bipolar disorder found that those treated with omega-3 fatty acid supplements showed significant improvement in membrane fluidity and flexibility.Citation116 However, a review of the relevant literature on use of omega-3 fatty acids in depression yielded mixed results, although this could have been due to methodological differences between studies, the lower proportions of EPA and DHA used in those studies, and patient selection bias.Citation117 In another review of 19 relevant studies, 13 reported a positive effect of omega-3 fatty acids in patients with depression, whereas six studies found no such association.Citation118 In addition, a meta-analysis of relevant studies reported that >60% EPA (out of the total of EPA and DHA, where dose range of 200–2200 mg/day of EPA in excess of DHA) had a positive impact on symptoms of depression compared with studies that used doses containing <60% of total EPA and DHA.Citation119 Finally, a placebo-controlled trial of adding omega-3 fatty acids to citalopram in patients with depression found significant improvement in depression scores compared with a placebo plus citalopram group, although there was no improvement in the speed of the initial antidepressant response.Citation120
An increased risk of suicide, commonly associated with depression, has been linked with omega-3 fatty acid deficiency.Citation121 A case-controlled study at autopsy compared omega-3 fatty acid levels in the orbitofrontal cortex of patients with major depressive disorder (n = 15) and age-matched controls (n = 27). Lower DHA levels were found in the orbitofrontal cortex of 32% of female patients and 16% in male patients,Citation122 suggesting that lower levels of DHA could be a marker of increased suicide risk in patients with depression. Several other clinical trials support the adjunctive role of EPA and DHA in the treatment of both unipolar and bipolar depression.Citation123–Citation125 Omega-3 fatty acids are both safe during infant development and effective for the treatment of major depression in pregnant women. Notably, low fish consumption and omega-3 fatty acids have been linked with depression more in women than in men.Citation126 Finally, a placebo-controlled study of 45 patients with bipolar disorder given omega-3 fatty acids ± cytidine found no significant effect on symptoms of depression compared with the placebo group.Citation127 Cytidine, a pyrimidine, was reported to have antidepressant-like effects in preclinical studies. In summary, further research is needed before recommending use of omega-3 fatty acids as monotherapy in patients with major depressive and other mood disorders.
Omega-3 fatty acids also have a preventive role. Interestingly, a lower lifetime prevalence of bipolar II disorder has been associated with greater consumption of seafood.Citation128,Citation129 Further, a small open-label study of bipolar I patients (n = 10) who were given EPA at a daily dose of 1.5–2.5 g found that eight of ten (80%) had a 50% decrease in depression scores.Citation130 Subsequently, a randomized controlled trial has substantiated the adjunctive role of omega-3 fatty acids (6.2 g EPA plus 3.4 mg DHA and 1–2 g ethyl-EPA) in patients with bipolar II disorder receiving conventional mood stabilizers.Citation131 A randomized controlled study of patients with bipolar disorder and rapid cycling who were receiving conventional treatment found that those given EPA 6 mg/day showed no significant difference in depressive or manic symptoms after four months of intervention than the group receiving placebo.Citation132 These negative results might be due to the use of EPA without DHA and inclusion of patients with resistant rapid cycling. Thus, patients with dysphoria and rapid cycling should be given higher doses of EPA and DHA, probably 8–10 g/day.Citation133 A recent meta-analysis of five pooled databases related to use of omega-3 fatty acids in bipolar patients found a significant reduction in symptoms of depression, although scores for mania were unaffected, thus supporting the adjunctive role of omega-3 fatty acids in the treatment of symptoms of depression in bipolar patients.Citation134
Pregnant women often have depleted omega-3 fatty acid stores and are at higher risk for postpartum depression and bipolar depression.Citation135 Almost all psychotropic medications carry a risk of side effects in pregnant women and may also adversely affect fetal and infant development. CAM therapies are safe alternatives in pregnant women with major depression. In randomized studies that used fixed dosesCitation136 or a range of doses (0.5, 1.4, 2.8 g/day) with no placebo controls,Citation137 EPA and DHA (3–8 g/day) were found to be effective in pregnant women with major depression and postpartum depression, with no adverse effects on the fetus. However, researchers have suggested that these studies of omega-3 fatty acids need to be repeated in a larger sample of pregnant women with depression.Citation136–Citation137 S-adenosylmethionine, St John’s wort, bright light therapy, acupuncture, and exercise have also been reported to improve symptoms of depression in women.Citation138 Further studies are needed to delineate specific CAM therapies useful in premenstrual syndrome, premenstrual dysphoric disorder, antepartum and postpartum depression, lactation, and transition through menopause.Citation138–Citation139
Omega-3 fatty acids are also safe for use in children and adolescents with bipolar disorder. An 8-week open-label study of 20 children (aged 6–16 years) with bipolar disorder given EPA 1290 mg/day and DHA 4300 mg/day found that 35% of children had more than a 50% decrease in Young Mania rating scores,Citation140 consistent with results in pediatric depression.Citation141 Two-thirds of patients did not show improvement, indicating that omega-3 fatty acids are ineffective in pediatric bipolar disorder. However, larger studies are needed to confirm this. Pediatric bipolar disorder is a difficult condition to treat, and some pediatric bipolar patients may benefit from CAM therapies. One review has reported that omega-3 fatty acids and lecithin/choline have potential utility as CAM in pediatric bipolar disorder. S-adenosylmethionine and inositol have some data supporting their efficacy in the treatment of depressive symptoms. Some data suggest these compounds may be useful adjunctive treatments, but few data are available to support their use as stand-alone therapy in pediatric bipolar disorder.Citation142 Another small open-label trial of a multinutrient supplement (EMPower™) found that 70% of pediatric completers with bipolar spectrum disorder demonstrated a significant decrease in both depression and mania scores between baseline and the final visit (P < 0.05). Gastric discomfort was the only reported side effect. These researchers suggested that randomized, placebo-controlled trials of EMPower are warranted and feasible.Citation143 Evidently, omega-3 fatty acid treatment was associated with a very modest improvement in symptoms of mania in children with bipolar disorder. The most commonly observed side effects of omega-3 fatty acids in children are nausea, heartburn, stomach pain, belching, bloating, and diarrhea attributable to higher doses and use of unrefined fish oil preparations. Bleeding episodes due to reduction in platelet aggregation and triggering of mania are other side effects of high doses of omega-3 fatty acids. Use of omega-3 fatty acids should be strictly avoided in patients on anticoagulant therapy and antidiabetic medications. Some omega-3 fatty acids found in fish oil can increase low-density lipoprotein cholesterol, which is bad for the heart.Citation57
Choline in bipolar disorder
Choline has been used effectively in ameliorating symptoms of mania. A small, open-label study of six patients with treatment-resistant rapid cycling bipolar disorder and stabilized on lithium found that addition of free choline 2000–7200 mg/day resulted in improvement of manic symptoms, although the impact on depression was variable.Citation144 A randomized controlled trial of oral choline in rapid cycling bipolar patients treated with lithium reported significantly decreased purine levels in the brain over a 12-week period, which was related to the anti-manic effects of choline.Citation145 Oral administration of exogenous choline increased synthesis of phospholipids in the cell membrane and corrected the mitochondrial component of diathesis in patients with bipolar disorder inadequately meeting the demand for increased adenosine triphosphate production.Citation145 Thus, choline supplementation in small studies was effective for improving manic symptoms in bipolar patients, although larger studies are needed before recommending use of oral choline in the treatment of mania in bipolar I disorder.
Inositol in bipolar disorder
Inositol, a glucose isomer precursor of phosphatidyl inositol linked to the second messenger system, has been found to be more effective than placebo in the treatment of depression and other psychiatric illnesses, including panic disorder. Doses in the relevant studies have ranged from 12,000 to 20,000 mg/day.Citation146 Inositol, a vitamin-like substance found in many plants and animals, can be produced synthetically. A randomized controlled trial in 24 bipolar patients given inositol or placebo found no significant differences between the treatment groups. However, a trend towards improvement on inositol led researchers to recommend that larger studies be performed.Citation147–Citation148 Another study of 66 bipolar I or II patients with resistant depression examined the benefits of augmenting mood stabilizers with lamotrigine, inositol, or risperidone, and found that the rate of recovery was 23.8% with lamotrigine, 17.4% with inositol, and 4.6% with risperidone.Citation149 Nierenberg et al suggested that patients with treatment-resistant depression are suitable candidates for inositol augmentation. However, at therapeutic doses, inositol frequently causes flatulence and occasionally induces mania.Citation149
5-hydroxy-L-tryptophan in bipolar disorder
5-hydroxy-L-tryptophan is an immediate precursor in the synthesis of serotonin, and deficiency of serotonin can cause major depression. As a dietary supplement, 5-hydroxy-L-tryptophan is used widely as a self-medication for depression, and has replaced L-tryptophan, which caused eosinophilia myalgia syndrome and was taken off the market.Citation150 Use of L-tryptophan and Showa Denko KK have been shown to be the main causes of this syndrome, but 5-hydroxy-L-tryptophan is not associated with such toxicity.Citation150 There is some (albeit limited) support for 5-hydroxy-L-tryptophan 200–300 mg/day being more effective than placebo when given alone in adults with major depression, although the data are better when it is used to augment antidepressants.Citation151 The most common side effects include nausea, vomiting, diarrhea, headache, and insomnia. No case of serotonin syndrome has been reported in subjects taking 5-hydroxy-L-tryptophan alone or in combination with SSRIs. Further, no adverse interactions have been reported between 5-hydroxy-L-tryptophan and the monoamine oxidase inhibitors.Citation152 In their review, Sarris et al found that use of omega-3 fatty acids, S-adenosylmethionine, folic acid, 5-hydroxy-L-tryptophan, inositol, lavender, and traditional Chinese medicines were effective when used to supplement antidepressants and mood stabilizers in mood disorders.Citation134
N-acetylcysteine in bipolar disorder
N-acetylcysteine, a precursor of glutathione, is an important antioxidant in the brain and reduces oxidative stress. Increased oxidative stress and altered glutathione metabolism have been reported in bipolar and major depressive disorder.Citation153 A randomized controlled trial in bipolar patients on mood stabilizers found that those who were given adjunctive N-acetylcysteine 2 g/day showed a significant improvement in depression, mania, quality of life, and social and occupational functioning compared with placebo.Citation154 Dean et al reviewed the literature on the therapeutic effect of N-acetylcysteine in psychiatric disorders, including bipolar disorder, and found it to be beneficial in patients with bipolar depression.Citation155 It is well tolerated by patients with bipolar disorder, although it needs to be taken for 8 weeks (2 g/day) to achieve a positive response.
Hormones in mood disorders
Dehydroepiandrosterone (DHEA) is an androgen produced by the adrenal glands, levels of which tend to decrease during mid-life in men and women. Lower levels of DHEA have been reported in patients with major depression, and use of DHEA has been associated with improved mood. An increase in DHEA sulfate, the primary metabolite of DHEA, has also been associated with improvement in depression and dysthymia.Citation156–Citation157 In a randomized controlled trial, 23 men and 23 women with major or minor mid-life depression were given DHEA 90 mg/day for three weeks, then 450 mg/day for a further three weeks, or placebo for six weeks. A 50% or greater reduction in baseline Hamilton Depression Rating scores was observed in the 23 subjects who took DHEA and in 13 subjects who took placebo. Patients taking DHEA also showed improvement in sexual function.Citation158 DHEA has been used effectively in patients with human immunodeficiency virus/acquired immune deficiency syndrome and subsyndromal depression or chronic dysthymia. Of 145 such patients given DHEA 100–400 mg/day for 8 weeks, 64% showed a more than 50% reduction in depression scores compared with 38% of those given placebo.Citation159 The response was maintained for 8 months of follow-up, and was higher among those with increased levels of DHEA sulfate.Citation159 Arguably, subsyndromal depression and dysthymia are not the same as major depression. In a recent study, DHEA 100 mg/day or placebo was administered to 26 patients with anorexia nervosa, whose assessment included mood symptoms. Patients receiving DHEA experienced significant improvement in mood and body mass index, although there was no difference in bone marrow density. Thus, comorbid depression in patients with eating disorders may benefit from the use of DHEA.Citation160 DHEA should be used in low doses in bipolar patients because it may induce manic-like symptoms, irritation, and bouts of aggression, and increase testosterone and estrogen levels, resulting in an elevated risk of uterine or breast cancer, vaginal bleeding, endometrial hyperplasia, and venous thrombosis.Citation57
Ayurvedic medicine in mood disorders
Ayurvedic medicine is an ancient healing system used in India, which is now practiced worldwide.Citation161 Ayurveda denotes longevity. The theory of Ayurveda is based on balancing the individual’s three constitutional “doshas”, ie, vata, pitta, and kappa, which arise from five elements of ancient philosophy, being fire, water, air, earth, and space.Citation162–Citation163 It is believed that health or sickness depends on the presence or absence of a balanced state. Both intrinsic and extrinsic factors, such as an indiscriminate diet, undesirable habits, not observing the rules of healthy living, seasonal abnormalities, lack of exercise, and misuse of body and mind can result in lack of balance in the body.Citation164 Ayurvedic medicine includes several treatment options, which balance three disturbed doshas (). Diagnosis is based on a comprehensive history, detailed physical examination, measurement of vital signs including pulse, and relevant laboratory tests.Citation30 Ashwagandha, along with combinations of herbs, such as Amrit kalash and mentat, and antidepressants can be used in depressed patients.Citation30,Citation165–Citation168
Table 3 Treatment options in Ayurvedic medicine
There has been difficulty in conducting randomized controlled trials in Ayurvedic medicine because most treatments involve multiple herbs, changes in diet and lifestyle, and treatments are individualized and target the entire person.Citation169 Further, the effects of Ayurvedic herbs tend to be mild and slow in onset. Most Ayurvedic herbs do tend to work gradually and with increasing efficacy as the system habituates to consistent dosing. This is often true of herbs that are prescribed for mood disorders. However, the effect of Ayurvedic herbs is not always mild. With accurate tailoring of herbal preparations, herbal therapy can be powerful in effecting change in the balance of body and mind, eg, with mood disorders that often have complex multifactorial origins. Patients who are intolerant to prescription medications fare better with Ayurvedic interventions, including panchakarma detoxification.Citation162 Small preliminary studies of major depression treated with herbs, herbal mixtures, and Rasayanas (a special branch of Ayurveda aiming to rejuvenate and nourish the body at all levels and comprises several products manufactured from a combination of herbs) have demonstrated improvement in depression scores.Citation163 Sharma et al recommended larger controlled studies in major depression.Citation163 Berberine, a traditional alkaloid plant used in Ayurvedic and traditional Chinese medicine, is reported to improve depression.Citation170 Posmontier and Teitelbaum have discussed the use of Ayurvedic medicine to treat postpartum depression.Citation171
Homeopathy in mood disorders
Homeopathy is a traditional medical system that uses a holistic approach. Homeopathy means treating diseases with minute doses of substances which are capable of producing symptoms similar to the disease when taken by healthy people. In homeopathy, the natural law of healing is known as Similia Similibus Curantur, meaning “likes are cured by likes”.Citation163 Homeopathy is practiced in many places around the world. An audit of UK homeopathic clinics revealed that more than 84% of consultees reported improvement in mental health problems, including depression, and improvement in well-being. None of the 273 patients in that study reported deterioration, and use of conventional medicines was reduced in 25% of patients.Citation172 Homeopathic medicines have been shown to be safe in high dilutions.Citation57 In a systematic review of homeopathic studies in depression, Pilkington et al concluded that the different kinds of homeopathy, such as individualized prescribing, limited list prescribing, and standardized complexes used in these studies make interpretation of results more difficult.Citation173 According to one study,Citation174 the most commonly treated conditions in the practice of homeopathy were depression and anxiety disorders. Positive outcomes were most frequently observed in irritable bowel syndrome (73.9%), depression (63.6%), and anxiety (61.0%). Which components of the treatment were most responsible for the outcomes is unclear.Citation174 A systematic review of randomized placebo-controlled studies (25 eligible studies from an initial pool of 1431) of homeopathic treatments in psychiatry found beneficial effects in several mental health disorders, including functional fibromyalgia and chronic fatigue syndrome. No study of patients with major depression was found in a literature review,Citation175 which called for randomized controlled trials using homeopathic interventions in these disorders.
Mind-body-spirit approaches in mood disorders
There are a large number of mind-body-spirit practices that have been used effectively in major depression.Citation176 It is widely accepted that most conventional antidepressant drugs increase levels of the relevant neurotransmitters, such as serotonin, norepinephrine, and dopamine, in the synapse. Mind-body-spirit approaches are also likely to operate through the same mechanism as antidepressants, and do so in a manner similar to that of psychotherapy. Evidently, psychotherapy-induced neurotransmitter changes are similar to those caused by antidepressants. Common approaches such as yoga, meditation, exercise, and acupuncture are reviewed here.
Yoga
Pilkington et al reported a positive impact of yoga on depression, although methodological weaknesses make the study results hard to interpret.Citation177 A study of 71 normal adults compared visualization and relaxation techniques with 30 minutes of yoga postures and breathing exercises, and the results indicated that the participants in the yoga group became more energetic and alert with improved mood.Citation178 Kundalini yoga techniques have also been found to be effective in depression.Citation179 In another study, 113 psychiatric inpatients who attended Hatha yoga classes experienced a significant reduction in symptoms of depression. Improvements also occurred in anxiety, depression, hostility, fatigue, and confusion.Citation180 Lavey et al and Weintraub suggest that yoga has a considerable benefit for patients with depression.Citation180–Citation181
In another study, 28 patients with mild depression who participated in two one-hour Iyengar yoga classes showed a significant reduction in depression scores compared with a control group.Citation182 To benefit from Iyengar yoga, patients with treatment-resistant depression need long-term exposure to yoga practices.Citation183 Other variants of yoga, such as Shavasana and Sudarshan Kirya, are also effective in mild-to-severe depression, including in older adults.Citation184–Citation186 Brown and Gerberg have developed a neurophysiological model of Sudarshan Kirya and discussed its clinical usefulness in depressive disorder.Citation187,Citation188 Other yoga researchers have found LifeForce yoga to be effective in depression.Citation189 Sudarshan Kirya has been shown to increase serum levels of brain-derived neurotrophic factor, an indicator of neuroplasticity, which is correlated with improvement in depression.Citation190
Meditation
Meditation is a highly introspective practice that is used worldwide by people with and without health problems. Manocha et al assessed the effect of meditation on work stress, anxiety, and mood in 178 full-time workers who participated in a randomized, controlled, 8-week, three-arm trial comparing a mental silence meditation approach with an active “relaxation” control and a wait-list control. The study demonstrated a significant improvement in the meditation group compared with the relaxation control and wait-list groups. This and other research has shown that mental silence meditation, also known as Sahaga yoga, is a safe and effective strategy for dealing with work stress and depression.Citation191 Yoga can enhance wellnessCitation192 and also significantly decreases depressive symptoms.Citation193
Eisendrath et al reported a patient with treatment-resistant depression who was treated with mindfulness-based cognitive therapy, which is an 8-week intervention that uses mindfulness meditation. The focus of mindfulness-based cognitive therapy is on decreasing rumination, enhancing self-compassion, increasing acceptance, and decreasing avoidance.Citation194 Reiki, a related technique, is “a meditated state in which a practitioner channels Reiki energy from a universal source to another human being”.Citation195,Citation196 Bowden et al assessed the effect of Reiki on college students and found that it significantly reduced symptoms of depression and anxiety both immediately after treatment and 5 weeks post-treatment.Citation197
Exercise
Regular exercise is important for maintaining good physical and mental health. Engaging in exercise for 45 minutes on five days a week is associated with improvement in patients with moderate depression.Citation198 This effect is irrespective of age, gender, severity of depression, and type of exercise.Citation199 The positive impact of exercise on depression is mainly attributed to an increase in serotonin, norepinephrine, and endorphins in the brain. Numerous other studies support the benefits of moderate aerobic exercise on depression in various populations.Citation33,Citation200–Citation202 Exercise has been used as an adjunct and also as augmentation therapy with pharmacotherapy/psychotherapy in depressive symptoms, and in patients with mild-to-moderate depression and anxiety with good outcomes.Citation200 In addition, dance therapy has been shown to decrease depression to a greater extent than either music therapy or a movement-only control.Citation203
Biofeedback is based on the principle of using feedback from one’s body as a way of learning to control and change internal processes, with the intention of improving overall health and functioning. It is relatively safe and noninvasive, but could have an adverse effect on those with pacemakers.Citation204,Citation205 Use of biofeedback results in a significant reduction in symptoms of mild-to-moderate depression.Citation206
Acupuncture
Acupuncture is a traditional Chinese method used widely for treating a variety of physical and mental health problems. Kim reviewed the biological mechanisms of acupuncture and effectiveness of electroacupuncture stimulation on depression as part of Yin Tang and Bai Hui. Kim concluded that the results were inconsistent due to use of different acupuncture protocols.Citation207 In one pilot study, 30 subjects with treatment-resistant depression were randomized to receive 30 minutes of open acupuncture on a weekly and twice-weekly basis. The results indicated a significant improvement of depression scores in both groups, with no significant difference between them. Therefore, acupuncture may be an effective treatment for patients with treatment-resistant depression. It is safe and well tolerated with only mild side effects, ie, bruising, pain, and bleeding at the needle site.Citation208 Other studies also support the benefits of yoga, meditation, exercise, and acupuncture in mood disorders.Citation208–Citation211 Ventegodt and Merrick have suggested that nondrug CAM therapies appear to be safe, even for patients with serious physical and mental disorders.Citation212
Integrative approach
Integrative medicine uses a holistic approach, and is recommended in the management of depression. There are many clinical trials assessing integrative therapies for depression and other mood disorders, although they are yet to be consistently used in clinical practice, despite the need.Citation57,Citation209,Citation213 Internet-based integrative psychiatric interventions have been explored as a way to meet this need. Researchers have developed an integrative, web-based program (Deprexis®) that uses behavioral activation, cognitive restructuring, mindfulness/acceptance exercises, and social skills training. In a randomized clinical trial that included 396 subjects, researchers found a significant positive impact of this method on depression and on social functioning in those with mood disorders.Citation214 There are now many web-based programs that help people to overcome depression and other mental health problems.Citation215–Citation218
Discussion
CAM is not a primary treatment for mood or other psychiatric disorders. However, level 1 evidence is beginning to emerge. There are a variety of clinical scenarios in which a clinician might recommend CAM for a mood disorder, including:
patients who do not respond to antidepressant treatment
development of intolerable side effects to first-line antidepressants
a condition for which there are no effective treatments
patients who are resistant to standard treatments and augmentation strategies
patients on medications which are necessary but causing side effects that could be alleviated by CAM
mitigate effects of risk factors
those who want to explore the full range of services and options
a situation in which there is no access to standard treatment
when the patient is uncomfortable with modern medications
when the patient is more comfortable with CAM therapies
the patient cannot afford the cost of modern medication
multiple, complex comorbid medical conditions associated with depression.
Mood disorders present in many different ways and are associated with a variety of biological, psychological, social, and environmental factors that contribute to their pathogenesis. Co-occurring psychiatric and physical conditions further complicate the treatment of mood disorders.Citation8–Citation11 Standard pharmacological and psychotherapies used in patients with depression have resulted in the following outcomes: 30% of patients remit, another 30% show a partial response, and the rest are resistant to treatment.Citation12,Citation13 Overall, 30%–40% of patients with major depression would benefit from CAM.Citation12,Citation13 Open-label clinical trials of CAM are more abundant than randomized controlled trials. The American Psychiatric Association Task Force report on CAM in major depressive disorder recommends more rigorous and larger studies in major depression. Further, each type of CAM must be evaluated separately in adequately powered controlled trials. This report also suggests that several CAM treatments presently appear promising in major depression and deserve further study.Citation38 There are more than 120 CAM therapies used worldwide, yet their role in the treatment of mood disorders is limited because they have not all been studied scientifically.
Guidelines have been developed for using CAM in clinical practice. These emphasize the taking of a full patient history, conducting a complete physical examination, laboratory investigations, and a review of medications in order to make an accurate diagnosis and develop a treatment plan. All information gathered from the patient needs to be documented in the medical notes.Citation37,Citation39,Citation187,Citation188 Web-based CAM programs may help to meet the increasing demand for such treatments by patients with depression and mood disorders.Citation214–Citation218 Whether or not integrative medicine and CAMCitation57,Citation209,Citation213 can shift the therapeutic paradigm from conventional treatments to traditional therapies in the management of mood disorders is debatable.
Limitations
This narrative review of the literature has some limitations. For example, limiting the literature search to papers published in the English language could have missed many relevant publications. Other relevant articles could also have been missed because not all full articles and abstracts were available. The inclusion of small open-label studies among the references that provide “evidence-based data” is problematic because of the risk for over-interpretation of results collected with limited scientific rigor. Lack of replication studies further limits the interpretation of individual studies. The strength of this narrative review is that it has smoothly organized widely scattered data on the therapeutic effects of CAM in mood disorders.
Recommendations
CAM therapies are expanding in number and being tested with increasing scientific rigor, similar to the clinical trials that evaluate modern drugs for depression and other mood disorders. Solid evidence is emerging about the efficacy of several types of CAM in these conditions. There is even some evidence that nutraceuticals, botanicals, and nutrients could be used alone as first-line treatments in mild-to-moderate mood disorders. However, severe depression, including psychotic depression, bipolar disorder with rapid cycling, and treatment-resistant depression require antidepressants, mood stabilizers, and atypical antipsychotics. CAM may be useful as an adjunct to conventional therapies for both acute treatment and prevention of recurrence of these disorders, perhaps with a reduction in adverse effects. Patients suffering depression comorbid with liver disease can benefit from S-adenosylmethionine, which not only improves depression but also protects the liver and restores liver function. Levodopa is a well known treatment for Parkinson’s disease, and is known to deplete S-adenosylmethionine in the central nervous system, resulting in depression that can be improved by S-adenosylmethionine supplementation. Increased production of homocysteine due to genetic polymorphism of the methyltetrahydrofolate reductase gene (C/T and T/T instead of C/C) is associated with a greater risk of cardiovascular disease. Reduction in levels of both S-adenosylmethionine and folate may result in depression that responds poorly to antidepressants yet robustly to supplementation with S-adenosylmethionine and folate.Citation41,Citation42,Citation102,Citation103
Although St John’s wort alleviates depression in both men and women, it is particularly useful in women who cannot tolerate antidepressants. In addition to enhancing well-being, Rhodiola rosea is recommended for the treatment of mild-to-moderate depression, but needs to be used cautiously in women with a family or personal history of estrogen-sensitive breast cancer. Pregnant women are at higher risk for developing major depression, and all available antidepressants tend to cause adverse effects on the fetus or newborn, but omega-3 fatty acids are useful alternatives, and with no adverse effects. Further, adjunctive use of omega-3 fatty acids at 2–3 g/day with an EPA to DHA ratio of 2:1 is also recommended in bipolar disorder, given that it augments the response to antidepressants and mood stabilizers. Similarly, choline, inositol, 5-hydroxy-L-tryptophan, N-acetylcysteine, and DHEA are all reported to be more or less effective in bipolar depression. Ayurveda and homeopathic medicine need large-scale, randomized controlled trials to establish or refute their value in the treatment of mood disorders. Mind-body-spirit therapies, especially regular and long-term yoga practices, are critical for patients with moderate to-severe depression to sustain their benefits. A number of studies also support the effectiveness of meditation, exercise, and acupuncture in major depression. Integrative medicine with an underlying philosophy that involves a holistic approach to health care uses a combination of therapies to enhance the treatment of mood disorders. Randomized controlled trials continue to be needed to provide evidence for or against the use of CAM for mood disorders in the future.
Acknowledgments
The authors acknowledge the help of staff at the National Center for Complementary and Alternative Medicine, Riyadh, in searching for relevant literature on mood disorders and CAM. We also sincerely acknowledge the help of Harold Koenig, Duke University Medical Center and King Abdulaziz University, Jeddah, Kingdom of Saudi Arabia, in revising and editing the second draft of this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- HermanPMPoindexterBLWittCMEisenbergDMAre complementary therapies and integrative care cost-effective? A systematic review of economic evaluationsBMJ Open20122e001046
- World Health OrganizationWorld Mental Health Survey Consortium: prevalence, severity and unmet need for treatment of mental disorders in WHO world mental health surveysJAMA20042912581259015173149
- BrometEAndradeLHHwangICross-national epidemiology of DSM-IV major depressive episodeBMC Med201199021791035
- KesslerRCThe costs of depressionPsychiatr Clin North Am20123511422370487
- Fandino-LosadaAForsellYLundbergIDemands, skill discretion, decision authority and social climate at work as determinants of major depression in a 3-year follow-up studyInt Arch Occup Environ Health742012 [Epub ahead of print.]
- NordentoftMPrevention of suicide and attempted suicide in Denmark. Epidemiological studies of suicide and intervention studies in selected risk groupsDan Med Bull20015430636918208680
- FreemanEJColpeLJStrineTWPublic health surveillance for mental healthPrev Chronic Dis20107A1720040232
- LauterbachERumpfHJAhrensBAssessing dimensional and categorical aspects of depression: validation of the AMDP Depression ScaleEur Arch Psychiatry Clin Neurosci2005255151915538595
- BaumeisterHHutterNBengelJPsychological and pharmacological interventions for depression in patients with coronary artery diseaseCochrane Database Syst Rev20119CD00801221901717
- National Health ServiceDepression in adults with a chronic physical health problemNICE clinical guideline 912010 Available from: http://www.nice.org.uk/guidance/CG91Accessed March 20, 2013
- MaesMKuberaMObuchowiczwaEGoehlerLBrzeszczJDepression’s multiple comorbidities explained by neuroinflammatory and oxidative and nitrosative stress pathwaysNeuro Endocrinol Lett20113272421407167
- Al-HarbiKSTreatment-resistant depression: therapeutic trends, challenges, and future directionsPatient Prefer Adherence2012636938822654508
- Al-HarbiKSQureshiNANeuromodulation therapies and treatment-resistant depressionMed Devices (Auckl)20125536523152710
- American Psychiatric AssociationDiagnostic and Statistical Mental Disorders, Fourth Edition, Text RevisionWashington, DCAmerican Psychiatric Association1994
- World Health OrganizationInternational Classification of Diseases-10Geneva, SwitzerlandWorld Health Organization1990
- WalpoleSCMcMillanDHouseACottrellDMirGInterventions for treating depression in Muslim patients: a systematic reviewJ Affect Disord2013145112022854098
- BartolomucciALeopardiRStress and depression: preclinical research and clinical implicationsPLoS One20094e426519180237
- FavaMFarabaughAHSickingerAHPersonality disorders and depressionPsychol Med2002321049105712214786
- ItoNHoriAYabeTInvolvement of neuropeptide y signaling in the antidepressant-like effect and hippocampal cell proliferation induced by kososan, a kampo medicine, in the stress-induced depression-like model miceBiol Pharm Bull2012351775178323037167
- WolkowitzOMReusVIMellonSHOf sound mind and body: depression, disease, and accelerated agingDialogues Clin Neurosci201113253921485744
- DacherEThe development of an integrated medical model: toward a postmodern medicineMicozziMSFundamentals of Complementary and Alternative MedicineNew York, NYChurchill Livingstone2001
- SarrisJClinical depression: an evidence-based integrative complementary medicine treatment modelAltern Ther Health Med201117263722314631
- PampallonaSBolliniPTibaldiGKupelnickBMunizzaCCombined pharmacotherapy and psychological treatment for depression: a systematic reviewArch Gen Psychiatry20046171471915237083
- ThaseMEEvaluating antidepressant therapies: remission as the optimal outcomeJ Clin Psychiatry200364 Suppl 13182514552652
- BaghaiTCMollerHJRupprechtRRecent progress in pharmacological and non-pharmacological treatment options of major depressionCurr Pharm Des20061250351516472142
- TrivediMHRushAJWisniewskiSREvaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practiceAm J Psychiatry2006163284016390886
- BambauerKZAdamsASZhangFPhysician alerts to increase antidepressant adherence: fact or fiction?Arch Intern Med200616649850416534035
- FavaMPharmacological approaches to the treatment of residual symptomsJ Psychopharmacol200620 Suppl 3293416644769
- PetersenTJEnhancing the efficacy of antidepressants with psychotherapyJ Psychopharmacol200620 Suppl 3192816644768
- Department of Ayush, Ministry of Health and Family Welfare Available from: http://indianmedicine.nic.in/Accessed October 10, 2012
- PerronBEJarmanCNKilbourneAMAccess to conventional mental health and medical care among users of complementary and alternative medicine with bipolar disorderJ Nerv Ment Dis200919728729019363387
- JarmanCNPerronBEKilbourneAMTehCFPerceived treatment effectiveness, medication compliance, and complementary and alternative medicine use among veterans with bipolar disorderJ Altern Complement Med20101625125520192909
- NahasRSheikhOComplementary and alternative medicine for the treatment of major depressive disorderCan Fam Physician20115765966321673208
- MuskinPRIntroduction: herbs and hermeneuticsComplementary and Alternative Medicine and PsychiatryArlington, VAAmerican Psychiatric Press Inc2005
- LaPatraJHealing: The Coming Revolution in Holistic MedicineNew York, NYMcGraw-Hill1978
- Al-BedahAPublic perspective: information and insights in complementary and alternative medicineOman Med J2012272022359720
- RavindranAVLamRWFilteauMJCanadian Network for Mood and Anxiety Treatments (CANMAT) Canadian Network for Mood and Anxiety Treatments (CANMAT)Clinical guidelines for the management of major depressive disorder in adults. V. Complementary and alternative medicine treatmentsJ Affect Disord2009117 Suppl 1S54S6419666194
- FreemanMPFavaMLakeJTrivediMHWisnerKLMischoulonDComplementary and alternative medicine in major depressive disorder: the American Psychiatric Association Task Force reportJ Clin Psychiatry20107166968120573326
- HoendersHJAppeloMTvan den BrinkEHHartogsBMAde JongJTVMThe Dutch Complementary and Alternative Medicine (CAM) protocol: to ensure safe and effective use of CAM within Dutch mental health careJ Complement Altern Med20111711971201
- GuptaSChauhanDMehlaKSoodPNairAAn overview of nutraceuticals: current scenarioJ Basic Clin Pharm201015562
- BottiglieriTS-Adenosyl-L-methionine (SAMe) from the bench to the bedside- molecular basis of pleiotrophic moleculeAm J Clin Nutr2002761151S1157S12418493
- BrownRPGerbargPLBottiglieriTS-Adenosylmethionine (SAMe) for depression: biochemical and clinical evidencePsychiatr Ann2002322944
- CarpenterDJSt John’s wort and S-adenosyl methionine as “natural” alternatives to conventional antidepressants in the era of the suicidality boxed warning: what is the evidence for clinically relevant benefit?Altern Med Rev201116173921438644
- PapakostasGICassielloCFIovienoNFolates and s-adenosylmethionine for major depressive disorderCan J Psychiatry20125740641322762295
- FreemanMPMischoulonDTedeschiniEComplementary and alternative medicine for major depressive disorder: a meta-analysis of patient characteristics, placebo-response rates, and treatment outcomes relative to standard antidepressantsJ Clin Psychiatry20107168268820573327
- AlpertJEPapakostasGMischoulanDS-adenosyl-L-methionine (SAMe) as an adjunct for resistant major depressive disorder: an open trial following partial or nonresponse to selective serotonin reuptake inhibitors or venlafaxineJ Clin Psychopharmacol20042466166415538131
- PapakostasGIMischoulonDShyuIAlpertJEFavaMS-adenosyl methionine (SAMe) augmentation of serotonin reuptake inhibitors for antidepressant nonresponders with major depressive disorder: a double-blind, randomized clinical trialAm J Psychiatry201016794294820595412
- ErnstEComplementary medicineCurr Opin Rheumatol20031515115512598804
- GrassettoMVarrattoAPrimary fibromyalgia is responsive to S-adenosyl-L-methionineCurr Ther Res199455797806
- LieberCSS-adenosyl-L-methionine: its role in the treatment of liver diseasesAm J Clin Nutr200276S1183S1187
- AleynikSILieberCSPolienylphosphatidylcholine corrects the alcohol-induced hepatic oxidative stress by restoring s-adenosylmethionineAlcohol Alcohol20033820821212711653
- Di RoccoARogersJDBrownRWernerPBottiglieriTS-adenosyl-L-methionine improves depression in patients with Parkinson’s disease in an open label clinical trialMov Disord2000151225122911104210
- ShippyRAMendezDJonesKCergnulIKarpiakSES-adenosyl-L-methionine (SAMe) for the treatment of depression in people living with HIV/AIDSBMC Psychiatry200443815538952
- CeruttiRSichelMPPerinMPsychological distress during puerperium: a novel therapeutic approach using S-adenosylmethionineCurr Ther Res199353707716
- SurteesRHylandKA method for the measurement of S-adenosylmethionine in small volume samples of cerebrospinal fluid or brain using high-performance liquid chromatography-electro chemistryAnn Biochem1989181333335
- LevkovitzYAlpertJEBrintzCEMischoulonDPapakostasGIEffects of S-adenosylmethionine augmentation of serotonin-reuptake inhibitor antidepressants on cognitive symptoms of major depressive disorderJ Affect Disord201231174117821911258
- BrownRPGerbergPLMuskinPRMood disordersHow to Use Herbs, Nutrients and Yoga in Mental HealthNew York, NYWW Norton & Company2009
- El-AlfyATAbourashedEAMatsumotoRRNature against depressionCurr Med Chem2012192229224122414105
- IovienoNDaltonEDFavaMMischoulonDSecond-tier natural antidepressants: review and critiqueJ Affect Disord201113034335720579741
- LindeKRamirezGMulrowCDPaulsAWesdenhammerWMelchartDSt John’s Wort for depression – an overview and metaanalysis of randomized clinical trialsBMJ19963132532588704532
- VorbachEUArnoldtKHHübnerWDEfficacy and tolerability of St John’s wort extract LI 160 versus imipramine in patients with severe depressive episodes according to ICD-10Pharmacopsychiatry199730 Suppl 281859342765
- SchraderEEquivalence of St John’s wort extract (Ze 117) and fluoxetine: a randomized, controlled study in mild-moderate depressionInt Clin Psychopharmacol200015616810759336
- SheltonRCKellerMBGelenbergAEffectiveness of St John’s wort in major depression: a randomized controlled trialJAMA20012851978198611308434
- GelenbergAJSheltonRCCrits-ChristophPThe effectiveness of St John’s wort in major depressive disorder: a naturalistic phase 2 follow-up in which nonresponders were provided alternate medicationJ Clin Psychiatry2004651114111915323598
- [No authors listed]Hypericum Depression Trial Study GroupEffect of Hypericum perforatum (St John’s wort) in major depressive disorder: a randomized controlled trialJAMA20022871807181411939866
- BjerkenstedtLEdmanGVAlkenRGMannelMHypericum extract LI 160 and fluoxetine in mild to moderate depression: a randomized, placebo-controlled multi-center study in outpatientsEur Arch Psychiatry Clin Neurosci2005255404715538592
- MorenoRATengCTAlmeidaKMTavares JuniorHHypericum perforatum versus fluoxetine in the treatment of mild to moderate depression: a randomized double-blind trial in a Brazilian sampleRev Bras Psiquiatr200628293216612487
- FavaMAlpertJNierenbergAAA double-blind, randomized trial of St John’s wort, fluoxetine, and placebo in major depressive disorderJ Clin Psychopharmacol20052544144716160619
- ChenJAPapakostasGIYounSJAssociation between patient beliefs regarding assigned treatment and clinical response: reanalysis of data from the Hypericum Depression Trial Study GroupJ Clin Psychiatry2011721669167622053942
- KasperSAnghelescuIGSzegediADienelAKieserMSuperior efficacy of St John’s wort extract WS 5570 compared to placebo in patients with major depression: a randomized, double-blind, placebo-controlled, multi-center trial [ISRCTN77277298]BMC Med200641416796730
- GastparMSingerAZellerKEfficacy and tolerability of hypericum extract STW3 in long-term treatment with a once-daily dosage in comparison with sertralinePharmacopsychiatry200538788615744631
- SzegediAKohnenRDienelAKieserMAcute treatment of moderate to severe depression with hypericum extract WS 5570 (St John’s wort): randomised controlled double blind non-inferiority trial versus paroxetineBMJ200533050315708844
- WheatleyDHypericum in seasonal affective disorder (SAD)Curr Med Res Opin199915333710216809
- SingerASchmidtMHaukeWStadeKDuration of response after treatment of mild to moderate depression with Hypericum extract STW 3-VI, citalopram and placebo: a reanalysis of data from a controlled clinical trialPhytomedicine20111873974221514125
- RapaportMHNierenbergAAHowlandRDordingCSchettlerPJMischoulonDThe treatment of minor depression with St John’s Wort or citalopram: failure to show benefit over placeboJ Psychiatr Res20114593194121632064
- GellerSEStudeeLBotanical and dietary supplements for mood and anxiety in menopausal womenMenopause2007143 Pt 154154917194961
- BorrelliFIzzoAAHerb-drug interactions with St John’s wort (Hypericum perforatum): an update on clinical observationsAAPS J20091171072719859815
- KasperSGastparMMöllerHJBetter tolerability of St John’s wort extract WS 5570 compared to treatment with SSRIs: a reanalysis of data from controlled clinical trials in acute major depressionInt Clin Psychopharmacol20102520421320568656
- KnüppelLLindeKAdverse effects of St John’s wort: a systematic reviewJ Clin Psychiatry2004651470147915554758
- ThakorVLeachMJGillhamDEstermanAThe quality of information on websites selling St John’s wortComplement Ther Med20111915516021641521
- ClausonKASantamarinaMLRutledgeJCClinically relevant safety issues associated with St John’s wort product labelsBMC Complement Altern Med200884218637192
- McCreaCEPritchardMEConcurrent herb-prescription medication use and health care provider disclosure among university studentsComplement Ther Med201119323621296265
- EdwardsDHeufelderAZimmermannATherapeutic effects and safety of Rhodiola rosea extract WS® 1375 in subjects with life-stress symptoms – results of an open-label studyPhytother Res2012261220122522228617
- PanossianAWikmanGSarrisJRosenroot (Rhodiola rosea): traditional use, chemical composition, pharmacology and clinical efficacyPhytomedicine20101748149320378318
- DarbinyanVAslanyanGAmroyanEGabrielyanEMalmströmCPanossianAClinical trial of Rhodiola rosea L. extract SHR-5 in the treatment of mild to moderate depressionNord J Psychiatry20076134334817990195
- ChanSWPanax ginseng, Rhodiola rosea and Schisandra chinensisInt J Food Sci Nutr201263 Suppl 1758122039930
- KellyGSRhodiola rosea: a possible plant adaptogenAltern Med Rev2001629330211410073
- van DiermenDMarstonABravoJReistMCarruptPAHostettmannKMonoamine oxidase inhibition by Rhodiola rosea L. rootsJ Ethnopharmacol200912239740119168123
- DwyerAVWhittenDLHawrelakJAHerbal medicines, other than St John’s wort, in the treatment of depression: a systematic reviewAltern Med Rev201116404921438645
- SarrisJPanossianASchweitzerIStoughCScholeyAHerbal medicine for depression, anxiety and insomnia: a review of psychopharmacology and clinical evidenceEur Neuropsychopharmacol20112184186021601431
- LiLTWangSHGeHYChenJYueSWYuMThe beneficial effects of the herbal medicine Free and Easy Wanderer Plus (FEWP) and fluoxetine on post-stroke depressionJ Altern Complement Med20081484184618721085
- RaiVKattarPKhatoonSRawatAKSMehrotraSHeavy metal accumulation in some herbal drugsPharm Biol200139384387
- HuggetDBKahnIAAllgoodJCBlockDSSchlenkDOrganochlorine pesticides and metals in select botanical dietary supplementsBull Environ Contam Toxicol20016615015511116308
- ErnstECoonJTHeavy metals in traditional Chinese medicine: a systematic reviewClin Pharmacol Ther20017049750411753265
- RaiVKakkarPSinghJMisraCKumarSMehrotraSToxic metals and organochlorine pesticides residue in single herbal drugs used in important Ayurvedic formulation- ‘Dashmoola’Environ Monit Assess200814327327717922233
- GasserUKlierBKühnAVSteinhoffBCurrent findings on the heavy metal content in herbal drugsPharmeur Sci Notes20091375019275871
- SullivanJGreenfieldJCumberfordGGrantJStewartJExtraction efficiencies of heavy metals in hydroethanolic solvent from herbs of commerceJ AOAC Int20109349649820480895
- RosecransRDohnalJCThe effect of complimentary and alternative medicine products on laboratory testingSemin Diagn Pathol200926384819292027
- SadovskyRCollinsNTigheAPBruntonSASafeerRPatient use of dietary supplements: a clinician’s perspectiveCurr Med Res Opin2008241209121618348745
- PosadzkiPWatsonLErnstEContamination and adulteration of herbal medicinal products (HMPs): an overview of systematic reviewsEur J Clin Pharmacol20136929530722843016
- Ellsworth-BowersERCorwinEJNutrition and the psychoneuroimmunology of postpartum depressionNutr Res Rev20122518019222853878
- BottiglieriTFolate, vitamin B12, and neuropsychiatric disordersNutr Rev1996543823909155210
- CrellinRBottiglieriTReynoldsEHFolates and psychiatric disorders. Clinical potentialDrugs1993456236367686459
- ProcterAEnhancement of recovery from psychiatric illness by methylfolateBr J Psychiatry19911592712721773245
- BellIREdmanJSMorrowFDBrief communication. Vitamin B1, B2, and B6 augmentation of tricyclic antidepressant treatment in geriatric depression with cognitive dysfunctionJ Am Coll Nutr1992111591631578091
- CoppenABaileyJEnhancement of the antidepressant action of fluoxetine by folic acid: a randomised, placebo controlled trialJ Affect Disord20006012113010967371
- ChristensenHAikenABatterhamPJNo clear potentiation of antidepressant medication effects by folic acid + vitamin B12 in a large community sampleJ Affect Disord2011130374520805005
- WalkerJGMackinnonAJBatterhamPMental health literacy, folic acid and vitamin B12, and physical activity for the prevention of depression in older adults: randomised controlled trialBr J Psychiatry2010197455420592433
- LangeHSuryapranataHDe LucaGFolate therapy and in-stent restenosis after coronary stentingN Engl J Med20043502673268115215483
- HainesSTParkSKVitamin D supplementation: what’s known, what to do, and what’s neededPharmacotherapy20123235438222461123
- DumvilleJCMilesJNPorthouseJCockayneSSexonLKingCCan vitamin D supplementation prevent winter-time blues? A randomized trial among older womenJ Nutr Health Aging20061015115316554952
- JordeRSneveMFigenschauYSvartbergJWaterlooKEffects of vitamin D supplementation on symptoms of depression in overweight and obese subjects: randomized double blind trialJ Intern Med200826459960918793245
- KjærgaardMWaterlooKWangCEEffect of vitamin D supplement on depression scores in people with low levels of serum 25-hydroxyvitamin D: nested case-control study and randomised clinical trialBr J Psychiatry201220136036822790678
- Bertone-JohnsonERPowersSISpanglerLVitamin D supplementation and depression in the women’s health initiative calcium and vitamin D trialAm J Epidemiol201217611322573431
- TariqMMStreetenEASmithHAVitamin D: a potential role in reducing suicide risk?Int J Adolesc Med Health20112315716522191178
- HirashimaFParowAMStollALOmega-3 fatty acid treatment and T(2) whole brain relaxation times in bipolar disorderAm J Psychiatry20041611922192415465995
- ParkerGGibsonNABrotchieHHerucGReesAMHadzi-PavlovicDOmega-3 fatty acids and mood disordersAm J Psychiatry200616396997816741195
- Rocha AraujoDMVilarimMMNardiAEWhat is the effectiveness of the use of polyunsaturated fatty acid omega-3 in the treatment of depression?Expert Rev Neurother2010101117112920586692
- SubletteMEEllisSPGeantALMannJJMeta-analysis of the effects of eicosapentaenoic acid (EPA) in clinical trials in depressionJ Clin Psychiatry2011721577158421939614
- GertsikLPolandREBreseeCRapaportMHOmega-3 fatty acid augmentation of citalopram treatment for patients with major depressive disorderJ Clin Psychopharmacol201232616422198441
- SubletteMEHibbelnJRGalfalvyHOquendoMAMannJJOmega-3 polyunsaturated essential fatty acid status as a predictor of future suicide riskAm J Psychiatry20061631100110216741213
- McNamaraRKHahnCGJandacekRSelective deficits in the omega-3 fatty acid docosahexaenoic acid in the postmortem orbitofrontal cortex of patients with major depressive disorderBiol Psychiatry200762172417188654
- FreemanMPHibbelnJRWisnerKLOmega-3 fatty acids: evidence basis for treatment and future research in psychiatryJ Clin Psychiatry2006671954196717194275
- SuKPHuangSYChiuCCShenWWOmega-3 fatty acids in major depressive disorder. A preliminary double-blind, placebo-controlled trialEur Neuropsychopharmacol20031326727112888186
- NemetsBStahlZBelmakerRHAddition of omega-3 fatty acid to maintenance medication treatment for recurrent unipolar depressive disorderAm J Psychiatry200215947747911870016
- TimonenMHorrobinDJokelainenJLaitinenJHervaARäsänenPFish consumption and depression: the Northern Finland 1966 birth cohort studyJ Affect Disord20048244745215555697
- MurphyBLStollALHarrisPQOmega-3 fatty acid treatment, with or without cytidine, fails to show therapeutic properties in bipolar disorder: a double-blind, randomized add-on clinical trialJ Clin Psychopharmacol20123269970322926607
- McNamaraRKEvaluation of docosahexaenoic acid deficiency as a preventable risk factor for recurrent affective disorders: current status, future directions, and dietary recommendationsProstaglandins Leukot Essent Fatty Acids20098122323119515544
- NoaghiulSHibbelnJRCross-national comparisons of seafood consumption and rates of bipolar disordersAm J Psychiatry20031602222222714638594
- OsherYBersudskyYBelmakerRHOmega-3 eicosapentaenoic acid in bipolar depression: report of a small open-label studyJ Clin Psychiatry20056672672915960565
- FrangouSLewisMMcCronePEfficacy of ethyl-eicosapentaenoic acid in bipolar depression: randomised double-blind placebo-controlled studyBr J Psychiatry2006188465016388069
- KeckPEJrMintzJMcElroySLDouble-blind, randomized, placebo-controlled trials of ethyl-eicosapentanoate in the treatment of bipolar depression and rapid cycling bipolar disorderBiol Psychiatry2006601020102216814257
- OsherYBelmakerRHOmega-3 fatty acids in depression: a review of three studiesCNS Neurosci Ther20091512813319499625
- SarrisJMischoulonDSchweitzerIOmega-3 for bipolar disorder: meta-analyses of use in mania and bipolar depressionJ Clin Psychiatry201273818621903025
- HibbelnJRSeafood consumption, the DHA content of mothers’ milk and prevalence rates of postpartum depression: a cross-national, ecological analysisJ Affect Disord200269152912103448
- SuKPHuangSYChiuTHOmega-3 fatty acids for major depressive disorder during pregnancy: results from a randomized, double-blind, placebo-controlled trialJ Clin Psychiatry20086964465118370571
- FreemanMPHibbelnJRWisnerKLBrumbachBHWatchmanMGelenbergAJRandomized dose-ranging pilot trial of omega-3 fatty acids for postpartum depressionActa Psychiatr Scand2006113313516390366
- DeligiannidisKMFreemanMPComplementary and alternative medicine for the treatment of depressive disorders in womenPsychiatr Clin North Am20103344146320385346
- LustykMKBGerrishWGPremenstrual syndrome and premenstrual dysphoric disorder: issues of quality of life, stress and exercisePreedyVWatsonRRHandbook of Disease Burdens and Quality of Life MeasuresHeidelberg, GermanySpringer Science + Business Media LLC2010
- WozniakJBiedermanJMickEOmega-3 fatty acid monotherapy for pediatric bipolar disorder: a prospective open-label trialEur Neuropsychopharmacol20071744044717258897
- LooMIntegrative Medicine for ChildrenSt Louis, MOSaunders Elsevier Inc2009
- BogarapuSBishopJRKruegerCDPavuluriMNComplementary medicines in pediatric bipolar disorderMinerva Pediatr20086010311418277369
- FrazierEAFristadMAArnoldLEFeasibility of a nutritional supplement as treatment for pediatric bipolar spectrum disordersJ Altern Complement Med20121867868522747095
- StollALSachsGSCohenBMLaferBChristensenJDRenshawPFCholine in the treatment of rapid-cycling bipolar disorder: clinical and neurochemical findings in lithium-treated patientsBiol Psychiatry1996403823888874839
- LyooIKDemopulosCMHirashimaFAhnKHRenshawPFOral choline decreases brain purine levels in lithium-treated subjects with rapid-cycling bipolar disorder: a double-blind trial using proton and lithium magnetic resonance spectroscopyBipolar Disord2003530030612895208
- BenjaminJAgamGLevineJBersudskyYKofmanOBelmakerRHInositol treatment in psychiatryPsychopharmacol Bull1995311671757675981
- SarrisJKavanaghDJByrneGAdjuvant use of nutritional and herbal medicines with antidepressants, mood stabilizers and benzodiazepinesJ Psychiatr Res201044324119616220
- ChengappaKNLevineJGershonSInositol as an add-on treatment for bipolar depressionBipolar Disord20002475511254020
- NierenbergAAOstacherMJCalabreseJRTreatment-resistant bipolar depression: a STEP-BD equipoise randomized effectiveness trial of antidepressant augmentation with lamotrigine, inositol, or risperidoneAm J Psychiatry200616321021616449473
- BackEEHenningKJKallenbachLRBrixKAGunnRAMeliusJMRisk factors for developing eosinophilia myalgia syndrome (EMS) among L-tryptophan users in New YorkJ Rheumatol1993206666728496862
- DasYTBagchiMBagchiDPreussHGSafety of 5-hydroxy-L-tryptophanToxicol Lett200415011112215068828
- GijsmanHJvan GervenJMde KamMLPlacebo-controlled comparison of three dose-regimens of 5-hydroxytryptophan challenge test in healthy volunteersJ Clin Psychopharmacol20022218318911910264
- SmagaIPomiernyBKrzyżanowskaWN-acetylcysteine possesses antidepressant-like activity through reduction of oxidative stress: behavioral and biochemical analyses in ratsProg Neuropsychopharmacol Biol Psychiatry20123928028722820675
- SarrisJMischoulonDSchweitzerIAdjunctive nutraceuticals with standard pharmacotherapies in bipolar disorder: a systematic review of clinical trialsBipolar Disord20111345446522017215
- DeanOGiorlandoFBerkMN-acetylcysteine in psychiatry: current therapeutic evidence and potential mechanisms of actionJ Psychiatry Neurosci201136788621118657
- BlochMSchmidtPJDanaceauMAAdamsLFRubinowDRDehydroepiandrosterone treatment of midlife dysthymiaBiol Psychiatry1999451533154110376113
- WolkowitzOMReusVIKeeblerADouble-blind treatment of major depression with dehydroepiandrosteroneAm J Psychiatry199915664664910200751
- SchmidtPJDalyRCBlochMDehydroepiandrosterone monotherapy in midlife-onset major and minor depressionArch Gen Psychiatry20056215416215699292
- RabkinJGMcElhineyMCRabkinRMcGrathPJFerrandoSJPlacebo-controlled trial of dehydroepiandrosterone (DHEA) for treatment of nonmajor depression in patients with HIV/AIDSAm J Psychiatry2006163596616390890
- BlochMIsh-ShalomSGreenmanYKleinELatzerYDehydroepiandrosterone treatment effects on weight, bone density, bone metabolism and mood in women suffering from anorexia nervosa-a pilot studyPsychiatry Res201220054454922858403
- SatowYEKumarPDBurkeAInciardiJFExploring the prevalence of Ayurveda use among Asian IndiansJ Altern Complement Med2008141249125319123878
- PrathikantiSAyurvedic treatmentsLakeJSpiegelDComplementary and Alternative TreatmentsWashington, DCAmerican Psychiatric Publishing2007
- SharmaHChandolaHMSinghGBasishtGUtilization of Ayurveda in health care: an approach for prevention, health promotion, and treatment of disease. Part 2 – Ayurveda in primary health careJ Altern Complement Med2007131135115018166127
- Ven MurthyMRRanjekarPKRamassamyCDeshpandeMScientific basis for the use of Indian ayurvedic medicinal plants in the treatment of neurodegenerative disorders: AshwagandhaCent Nerv Syst Agents Med Chem20101023824620528765
- ShresthaBGTakagiYIshiiTWadhwaRKaulSCSelective killing of cancer cells by leaf extract of Ashwagandha: identification of a tumor-inhibitory factor and the first molecular insights to its effectClin Cancer Res2007132298230617404115
- MaityTAdhikariABhattacharyaKBiswasSDebnathPKMaharanaCSA study on evaluation of antidepressant effect of imipramine adjunct with Aswagandha and BramhiNepal Med Coll J20111325025323016473
- BhattacharyaSKBhattacharyaASairamKGhosalSAnxiolytic-antidepressant activity of Withania somnifera glycowithanolides: an experimental studyPhytomedicine2000746346911194174
- [No authors listed]Monograph. Withania somniferaAltern Med Rev2004921121415253680
- RiouxJA complex, nonlinear dynamic systems perspective on Ayurveda and Ayurvedic researchJ Altern Complement Med20121870971822830972
- VuddandaPRChakrabortySSinghSBerberine: a potential phytochemical with multispectrum therapeutic activitiesExpert Opin Investig Drugs20101912971307
- PosmontierBTeitelbaumMAn Ayurvedic approach to postpartum depressionHolist Nurs Pract20092320121419574756
- BawdenSRunning an NHS community homeopathy clinic – 10-year anniversary 2001–2011Homeopathy2012101515622226315
- PilkingtonKKirkwoodGRampesHFisherPRichardsonJHomeopathy for depression: a systematic review of the research evidenceHomeopathy20059415316316060201
- MathieRTRobinsonTWOutcomes from homeopathic prescribing in medical practice: a prospective, research-targeted, pilot studyHomeopathy20069519920517015190
- DavidsonJRCrawfordCIvesJAJonasWBHomeopathic treatments in psychiatry: a systematic review of randomized placebo-controlled studiesJ Clin Psychiatry20117279580521733480
- SelhubEMind-body medicine for treating depression: using the mind to alter the body’s response to stressAlternative and Complementary Therapies20071349
- PilkingtonKKirkwoodGRampesHRichardsonJYoga for depression: the research evidenceJ Affect Disord200589132416185770
- WoodCMood change and perceptions of vitality: a comparison of the effects of relaxation, visualization and yogaJ R Soc Med1993862542588505745
- Shannahoff-KhalsaDSKundalini yoga meditation techniques for the treatment of obsessive-compulsive and OC spectrum disordersBrief Treat Crisis Interv20033369382
- LaveyRShermanTMueserKTOsborneDDCurrierMWolfeRThe effects of yoga on mood in psychiatric inpatientsPsychiatr Rehabil J20052839940215895926
- WeintraubAYoga for Depression: A Compassionate Guide to Relieve Suffering Through YogaNew York, NYThree Rivers Press2004
- WooleryAMyersHSternliebBZeltzerLA yoga intervention for young adults with elevated symptoms of depressionAltern Ther Health Med200410606315055096
- ShapiroDCookIADavydovDMOttavianiCLeuchterAFAbramsMYoga as a complementary treatment of depression: effects of traits and moods on treatment outcomeEvid Based Complement Alternat Med2007449350218227917
- KhumarSSKaurPKSEffectiveness of Shavasana on depression in university studentsIndian J Clin Psychol1993208287
- TsangHWFungKMChanASLeeGChanFEffect of a qigong exercise programme on elderly with depressionInt J Geriatr Psychiatry20062189089716955451
- JanakiramaiahNGangadharBNNagaVenkatesha MurthyPJHarishMGSubbakrishnaDKVedamurthacharAAntidepressant efficacy of Sudarshan Kriya Yoga (SKY) in melancholia: a randomized comparison with electroconvulsive therapy (ECT) and imipramineJ Affect Disord20005725525910708840
- BrownRPGerbergPLSudarshan Kirya Yogic breathing in the treatment of stress, anxiety and depression: Part 1 Neurophysiologic modelJ Altern Complement Med20051118920115750381
- BrownRPGerbergPLSudarshan Kirya Yogic breathing in the treatment of stress, anxiety and depression: Part I1 Clinical applications and guidelinesJ Altern Complement Med20051171171716131297
- BennettSMWeintraubAKhalsaSSInitial evaluation of the LifeForce yoga program as a therapeutic intervention for depressionInt J Yoga Therap2008184957
- PanNLJiangMJPoonPWFHuangAMThe role of brain-derived neurotrophic factor in the antidepressant effects of Sudarshan Kriya YogaMaster’s thesis2006 Available from: http://ethesys.lib.ncku.edu.tw/ETD-db/ETD-search/view_etd?URN=etd-0808107-104238Accessed October 18, 2012
- ManochaRBlackDSarrisJStoughCA randomized, controlled trial of meditation for work stress, anxiety and depressed mood in full-time workersEvid Based Complement Alternat Med2011201196058321716708
- KjellgrenABoodSAAxelssonKNorlanderTSaatciogluFWellness through a comprehensive Yogic breathing program – controlled pilot trialBMC Complement Altern Med200774318093307
- MehtaPSharmaMYoga as a complementary therapy for clinical depressionComplement Health Pract Rev201015156170
- EisendrathSChartierMMcLaneMAdapting mindfulness-based cognitive therapy for treatment-resistant depressionCogn Behav Pract20111836237022211062
- PlodekJReiki: an ancient therapy in modern timesFreemanLMosby’s Complementary and Alternative Medicine: A Research-Based Approach3rd ed2009
- Available from: http://nccam.nih.gov/health/reiki/introduction.htmAccessed March 22, 2013
- BowdenDGoddardLGruzelierJA randomised controlled single-blind trial of the efficacy of Reiki at benefiting mood and well-beingEvid Based Complement Alternat Med2011201138186221584234
- BlumenthalJABabyakMAMooreKAEffects of exercise training on older patients with major depressionArch Intern Med19991592349235610547175
- CraftLLandersDThe effect of exercise on clinical depression and depression resulting from medical illness. A meta-analysisJ Sport Exerc Psychol199820339357
- OttoMWChurchTSCraftLLGreerTLSmitsJATrivediMHExercise for mood and anxiety disordersJ Clin Psychiatry20076866967617503975
- DunnALTrivediMHKampertJBClarkCGChamblissHOExercise treatment for depression: efficacy and dose responseAm J Prev Med2005281815626549
- RichardsonCRAvripasSANealDLMarcusSMIncreasing lifestyle physical activity in patients with depression or other serious mental illnessJ Psychiatr Pract20051137938816304506
- KochSMorlinghausKFuchsTThe joy dance: specific effects of a single dance intervention on psychiatric patients with depressionArts Psychother200734340349
- [No authors listed]. Available from: https://thequantumalliance.zendesk.com/entries/21055146-indigo-contraindications-for-biofeedbackAccessed April 8, 2013
- [No authors listed]. Available from: http://www.electrostimulateurs-manuels.fr/fichiers/publications/Contraindications-et-Precautions/contraindications.pdfAccessed April 8, 2013
- KaravidasMLehrerPVaschilloEPreliminary results of an open label study of heart rate variability biofeedback for the treatment of major depressionAppl Psychophysiol Biofeedback2007321193017333315
- KimYHJThe effectiveness of acupuncture for treating depression: a reviewAlternative and Complementary Therapies2007
- YeungASAmeralVEChuziSEFavaMMischoulonDA pilot study of acupuncture augmentation therapy in antidepressant partial and non-responders with major depressive disorderJ Affect Disord201113028528920692042
- MontiDABeitmanBDIntegrative PsychiatryOxford, UKOxford University Press2010
- MuskinPRComplementary and Alternative Medicine and PsychiatryArlington, VAAmerican Psychiatric Press Inc2000
- MischoulanDRosenbaumJFNatural Medications for Psychiatric Disorders2nd edPhiladelphia, PALippincott Williams & Wilkins2008
- VentegodtSMerrickJA review of side effects and adverse events of non-drug medicine (nonpharmaceutical complementary and alternative medicine): psychotherapy, mind-body medicine and clinical holistic medicineJ Complement Integr Med2009616
- MintzDLIntegrative approaches to depression and its treatmentPsychiatr Clin North Am201235xiiixvi22370502
- MeyerBBergerTCasparFBeeversCGAnderssonGWeissMEffectiveness of a novel integrative online treatment for depression (Deprexis): randomized controlled trialJ Med Internet Res200911e1519632969
- van StratenACuijpersPSmitsNEffectiveness of a web-based self-help intervention for symptoms of depression, anxiety, and stress: randomized controlled trialJ Med Internet Res20082510:e7
- WarmerdamLvan StratenATwiskJRiperHCuijpersPInternet-based treatment for adults with depressive symptoms: randomized controlled trialJ Med Internet Res200810e4419033149
- ClarkeGEubanksDReidEOvercoming Depression on the Internet (ODIN) (2): a randomized trial of a self-help depression skills program with remindersJ Med Internet Res20057e1615998607
- HoekWSchuurmansJKootHMCuijpersPPrevention of depression and anxiety in adolescents: a randomized controlled trial testing the efficacy and mechanisms of Internet-based self-help problem-solving therapyTrials2009109319821984