Abstract
Introduction
Despite numerous studies investigating personality disorder (PD) and childhood maltreatment (CM) characteristics in individuals with schizophrenia (SZ), there remains a scarcity of research focusing on sex differences in PD and CM within large samples of SZ patients.
Methods
A total of 592 participants (257 males, 335 females) were consecutively sampled from patients diagnosed with SZ at the psychiatric and psycho-counseling clinics at Shanghai Mental Health Center. PDs were assessed using a self-reported personality diagnostic questionnaire and a structured clinical interview, while CMs were evaluated using the Chinese version of the Child Trauma Questionnaire Short Form.
Results
Male patients exhibited a prominent self-reported trait of antisocial PD (t=1.972, p=0.049), while female patients demonstrated a notable emphasis on histrionic PD traits (t=−2.057, p=0.040). Structured interviews for PD diagnoses further indicated a higher comorbidity of schizotypal (χ2=4.805, p=0.028) and schizoid (χ2=6.957, p=0.008) PDs among male patients compared to female patients. Additionally, male patients reported a higher degree (t=2.957, p=0.003) and proportion (χ2=5.277, p=0.022) of experiences of physical abuse in their self-reported CM. Logistic regression analyses highlight distinct factors: higher antisocial PD traits and physical abuse are associated with male patients, while histrionic PD traits and emotional abuse are associated with female patients.
Discussion
These findings underscore the importance of recognizing and addressing sex-specific manifestations of personality pathology and the nuanced impact of CM in the clinical management of individuals with SZ. The study advocates for tailored interventions that consider the distinct needs associated with sex differences in both personality traits and CM experiences among SZ patients.
Introduction
In clinical psychiatric practice, Personality Disorders (PDs) are frequently overlooked,Citation1 particularly within the context of severe mental illnesses such as schizophrenia (SZ),Citation2–4 where assessments related to PDs are comparatively scarce.Citation5 Clinicians often prioritize the positive and negative symptoms as well as cognitive impairments associated with schizophrenia, while features indicative of PDs receive relatively less attention. On the other hand, the pronounced symptoms of illnesses like SZ, such as hallucinations and delusions, especially during acute phases, can significantly interfere with the assessment of PDs. Consequently, there exists a considerable gap in understanding the prevalence and characteristics of PDs in individuals with SZ.Citation6 In China, previous studiesCitation7 have shown that a significant proportion of individuals diagnosed with SZ meet criteria for at least one type of PD during the stable phase of the illness, with prevalence rates as high as 24.0%. Notably, there appears to be a higher prevalence of Cluster-A (odd and eccentric PD) and Cluster-C (anxious PD) PDs among individuals with SZ, accounting for around 12.0% of cases, while demonstrating lower rates of Cluster-B (emotional PD). Other findings have revealed potential etiological links between PDs and SZ in the Chinese population, such as the role of childhood trauma,Citation8 social support,Citation9 and shared biological pathogenesisCitation10 as potential contributors to the co-occurrence of these disorders.
Numerous studies have highlighted sex differences in the clinical features of SZ,Citation11–13 which can arise from the disease process itself, genetic and hormonal variations, disparities in brain maturation and morphology, and sex-specific behavioral patterns.Citation14 Simultaneously, sex differences are also commonly observed in PDs,Citation15 with variations in prevalence among different PDs. Notably, conditions like antisocial PD exhibit higher prevalence in men,Citation16 whereas borderline PD is more commonly diagnosed in women.Citation17,Citation18 Given this backdrop, a crucial question that remains inadequately addressed is whether sex differences in PDs demonstrate similar distribution patterns in individuals with severe mental illnesses like SZ.
A substantial body of research indicates that Childhood Maltreatment (CM) serves as a risk factor not only for SZCitation19–22 but also for PDs.Citation23,Citation24 However, the question of whether there are sex differences in self-reported CM among different populations remains inconclusive. For instance, a study by Caldirola et alCitation25 explored sex differences in retrospective self-reported CM in Italian adult patients with major depressive disorder or bipolar disorder, revealing that both women and men with MDD or BD experienced a similar and considerable burden of CM. Similarly, research conducted by Liu et alCitation26 investigated sex differences in the complex interconnections among various types of CM, post-traumatic stress disorder, and depression, identifying notable sex discrepancies in the relationship between different forms of maltreatment and psychopathological symptoms. However, such studies are relatively scarce within the SZ population. Consequently, whether sex differences in the experience of CM exist among individuals with SZ remains an open question that warrants further investigation.
Expanding upon the previously mentioned context, this study aims to explore and contrast self-reported PD traits and CM experiences among male and female individuals diagnosed with SZ. Furthermore, we seek to evaluate the prevalence of PD diagnoses through structured interviews within different gender groups. Our study hypothesis suggests that specific PD traits and particular CM experiences exhibit gender differences within the population of individuals diagnosed with SZ.
Methods
Sample and Setting
The survey, conducted at the Shanghai Mental Health Center (SMHC) between 2018 and 2023, involved participants selected from outpatients attending psycho-counseling and psychiatric clinics at SMHC, one of China’s largest healthcare facilities. The study was approved by the Research Ethics Committee at the SMHC (2018–14R). Participants gave written informed consent at the time of the recruitment stage. Our study, in its entirety, aligns with the principles outlined in the Declaration of Helsinki. This study aimed to assess the prevalence of PDs and CMs in a consecutive clinical sample of adult patients. A total of 647 outpatients were randomly selected from January 2018 to December 2023, meeting inclusion criteria such as age between 18 and 60 years, the ability to comprehend the study questionnaire, willingness to disclose information about PDs and CMs, compliance with the Diagnostic and Statistical Manual of Mental Disorders, Given that the Structured Clinical Interview for DSM-IV Axis II (SCID-II) was employed as the diagnostic tool for PDs in our study, which adheres to DSM-IV criteria, we opted for consistency in diagnostic criteria throughout our research. Fourth Edition (DSM-IV) criteria for the diagnosis of schizophrenia, and being under stable treatment conditions. Exclusion criteria included severe or unstable physical conditions, current pregnancy, and other factors identified by investigators as rendering the patient ineligible. A total of 55 individuals did not persist in completing the self-assessment scales or clinical interviews, resulting in incomplete data and their exclusion from the analysis. The primary reasons for non-completion included perceived assessment duration being too lengthy for 43 participants, 6 individuals providing entirely inconsistent responses, 3 participants refusing the researchers’ use of information provided after the interview, and 3 individuals requesting to withdraw from the study without providing a clear reason. Finally, 592 patients were included in the final analysis. In this study, we conducted a cross-sectional assessment at a single point in time, without repeated follow-up assessments.
Measurements and Variables
PD Traits and Diagnosis
A concise and well-structured self-report questionnaire, namely the Personality Diagnostic Questionnaire 4th Edition Plus (PDQ-4+),Citation27 as described in our previous publications,Citation1,Citation28,Citation29 is utilized for the assessment of PD traits. Comprising 107 true-false questions, this questionnaire is designed to evaluate 10 Axis II DSM-IV PDs, including Paranoid (PAR), Schizoid (SCH), Schizotypal (SCHT), Histrionic (HIS), Narcissistic (NAR), Borderline (BOR), Antisocial (ANT), Avoidant (AVO), Dependent (DEP), and Obsessive-compulsive (OBC). Personality Disorders (PDs) are commonly classified into three clusters, known as Cluster A (PAR, SCH, SCHT), Cluster B (HIS, NAR, BOR, ANT), and Cluster C (AVO, DEP, OBC), based on similar patterns of personality traits and behaviors. Each cluster encompasses a group of specific personality disorders that share certain characteristics. The primary objective of the PDQ-4+ is to distinguish individuals exhibiting characteristics associated with PDs from those who do not. It demonstrates high sensitivity (0.89) and acceptable specificity (0.65). Widely employed for screening DSM-IV PDs in Chinese psychiatric patients, the PDQ-4+ has shown a high test-retest reliability score (0.92) within the Chinese population, emphasizing the questionnaire’s result reliability.Citation7,Citation30,Citation31 For a more comprehensive clinical assessment, the SCID-II is employed. SCID-II is a semi-structured clinical interview that uses DSM-IV criteria for diagnosing PDs. Our team translated and implemented the Chinese version of SCID-II. The results obtained through SCID-II demonstrate a high level of consistency (0.90) with clinical diagnoses, and the test-retest reliability is also satisfactory (0.70).Citation32
CM Characteristics
CM was evaluated using the Chinese version of the Child Trauma Questionnaire Short Form (CTQ-SF).Citation8,Citation33,Citation34 Comprising 28 self-report items, the CTQ-SF categorizes childhood maltreatment into five subscales: emotional abuse (EA), physical abuse (PA), sexual abuse (SA), emotional neglect (EM), and physical neglect (PN). Participants rated the frequency of each event on a 5-point scale, ranging from 1 (never) to 5 (always), with higher scores indicating a greater extent of CMs. Participants scoring (i) 8 or above for PA subscale, SA subscale, and PN subscale; (ii) 10 or above for EA subscale; and/or (iii) 15 or above for EM subscale were considered as having experienced CM. The Chinese version of the CTQ-SF has demonstrated reliability and validity as an effective tool for assessing CMs in Chinese clinical samples.Citation35–37 In this study, Cronbach’s alpha for the overall CTQ-SF scale (28 items) was 0.663. Specifically, for each subscale, the Cronbach’s alpha values were as follows: 0.712 for the EA subscale, 0.718 for the PA subscale, 0.743 for the SA subscale, 0.754 for the EN subscale, and 0.166 for the PN subscale.
Data Analysis
Data analysis was conducted using SPSS version 20.0 (SPSS, Inc., Chicago, IL, USA). The data were entered into the database twice, and thorough data checking and cleaning were performed, considering both range and consistency, prior to analysis. Statistical significance was set at p<0.05. Quantitative variables are presented as mean ± standard deviation (SD), and qualitative variables as frequencies (%). Participants were stratified into male and female groups. Differences between means and proportions were assessed using the t-test and Chi-square test, respectively. To visually depict gender differences more intuitively, radar charts were employed, with the means transformed based on z-scores calculated for the entire sample, enhancing comparability. A multivariate logistic regression model with a stepwise (enter) method was constructed to identify factors associated with sex. Variables included in the logistic models were chosen based on age, duration of illness, 10 subtypes of personality disorders (PDs), and 5 subtypes of childhood maltreatments (CMs). Results were reported as β with corresponding 95% confidence intervals (CI), and P-values from Wald tests were provided for the logistic models.
Results
The sociodemographic and clinical information of the 592 participants are presented in . Participants’ ages ranged from 18 to 60 years, with a mean age of 30.1 ± 9.260 years. The percentage of unmarried individuals was higher among males than females (χ2 = 19.182, p < 0.001). Furthermore, the percentage of patients exhibiting extroversion as a pre-illness characteristic was higher among females than males (χ2 = 8.183, p = 0.017).
Table 1 Socio-Demographic Characteristics for Patients with Schizophrenia, Comparing Between Males and Females
Self-reported PD traits and PD frequencies assessed through the structured interviews were compared between male and female patients (). Male patients reported more ANT PD traits (t = 1.972, p = 0.049), while female patients reported more HIS PD traits (t = −2.057, p = 0.040). Based on the structured interview, the frequencies of SCH (χ2 = 6.957, p = 0.008) and SCHT PDs (χ2 = 4.805, p = 0.028) were higher among males than females.
Table 2 Self-Reported Personality Disorder (PD) Traits and Frequencies in Patients with Schizophrenia, Comparing Between Males and Females
presented the CM characteristics in male and female patients. The only significant difference was found in the severity (t = 2.957, p = 0.003) and frequency of PA (χ2 = 5.277, p = 0.022), where males were reported a higher level than females.
Table 3 Self-Reported Childhood Maltreatment (CM) Characteristics and Frequencies in Patients with Schizophrenia, Comparing Between Males and Females
As shown in , the sex differences in PD traits among patients with schizophrenia are mainly observed in Cluster B PDs. Specifically, male patients exhibit higher levels of ANT PD traits, while female patients show more pronounced traits in HIS, NAR, and BOR PDs. In terms of CM characteristics, gender differences are mainly observed in the experience of PA, with more male patients reporting childhood experiences of PA compared to females.
Figure 1 Personality Disorder (PD) traits and Childhood Maltreatment (CM) characteristics profiles of sex groups.
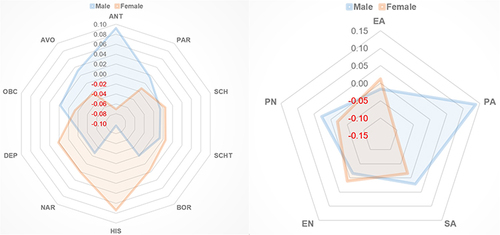
Logistic regression analyses were conducted with sex as the dependent variable, and age, course of illness, different types of self-reported PDs, and CMs as independent variables (). In males, having higher scores on the ANT PD (β = 0.778, 95% CI [0.669–0.905], χ2 = 10.567, p = 0.001), and experiencing PA were significant factors (β = 0.867, 95% CI [0.789–0.952], χ2 = 8.881, p = 0.003), while in females, having a higher self-reported score on the HIS PD (β =1.196, 95% CI [1.038–1.378], χ2 = 6.169, p = 0.013), and experiencing EA (β =1.088, 95% CI [1.009–1.173], χ2 = 4.749, p = 0.029) were significant factors.
Table 4 Associations Between Sex, Childhood Maltreatment (CM) and Personality Disorder (PD)
Discussion
Through a cross-sectional survey of a substantial clinical cohort, this study comprehensively delineates the sex differences in personality pathology and CM experiences among individuals diagnosed with schizophrenia. The results highlight that male patients exhibit a prominent self-reported trait of ANT PD, while female patients demonstrate a notable emphasis on HIS traits. Structured interviews for PD diagnoses further indicate a higher comorbidity of SCHT and SCH PDs among male patients compared to their female counterparts. Additionally, male patients report a higher degree and proportion of experiences of PA in their self-reported CM. These findings carry significant clinical implications, underscoring the need for tailored intervention strategies that address the distinct manifestations of personality pathology and trauma experiences based on sex in individuals with schizophrenia. The nuanced understanding of these differences enhances our ability to provide more effective and targeted therapeutic approaches for male and female patients within the clinical landscape.
The association between SZ and ANT PD has been a subject of interest since very early research.Citation38 The Epidemiological Catchment Area Study,Citation39 for instance, revealed a prevalence of schizophrenia 6.9 times higher among men with ANT PD and 11.8 times higher among women with ANT PD compared to the general population. Consistent with past research, our study finds that features of ANT PD are notably pronounced in male patients with SZ. Research by Crosby & Sprock (2004)Citation40 investigated the prevalence of ANT PD, highlighting that males were more frequently diagnosed with ANT PD compared to females (60.6% vs 45.7%, respectively). It is noteworthy that most studies on ANT PD have historically focused on men,Citation16,Citation41 contributing to a limited understanding of how sex differences manifest in this context. This discrepancy is evident in the prevalence rates between male and female prisoners, with nearly 50% of male prisoners diagnosed with antisocial PD, compared to 20% of female prisoners. In the general population, the male-to-female ratio of individuals with ANT PD is 3:1, making it one of the most striking sex differences observed in PDs.Citation42
Sex differences in the prevalence and manifestation of ANT PD may be attributed to diverse developmental trajectories. During childhood, boys often exhibit more externalizing impairments, including attention deficit disorder and conduct disorder, while girls tend to develop more internalizing symptoms, such as anxiety and affective symptoms. These early developmental differences contribute to the observed sex disparities in the criteria of ANT PD and its childhood precursor, conduct disorder, reflecting distinct trait profiles associated with each sex. Furthermore, one of the hallmark features of ANT PD, impulsive aggression, tends to be more prevalent in male This sex difference in impulsive aggression aligns with broader patterns of behavior observed in male and may be influenced by a combination of biological, environmental, and social factors.Citation43 The interplay of genetic predispositions, hormonal influences, and societal expectations may contribute to the heightened prevalence of impulsive aggression in men, consequently influencing the manifestation of ANT PD traits. The complex interaction of these factors underscores the importance of understanding the multifaceted nature of sex differences in personality pathology. Future research endeavors should explore these developmental trajectories and underlying mechanisms more comprehensively to provide a nuanced understanding of the psychological, biological, and social factors contributing to the observed sex differences in ANT PD traits.
Previous research has consistently identified sex differences in clinical presentationsCitation44,Citation45 and cognitive functionsCitation46 between male and female patients with SZ. These differences in symptoms may be related to disparities in personality pathology. Our study aligns with these findings by revealing that female patients exhibit more pronounced emotional and anxious personality pathology, particularly in HIS PD trait, compared to male patients. The consideration of sex bias is crucial in interpreting these sex-related differences. Studies, such as the one by Samuel et alCitation47 utilizing the case vignette methodology, have indicated a gender bias in the diagnosis of HIS PD. In this study, 141 practicing clinicians rated either a male or a female version of a case vignette. The results supported the concern of gender bias, with the female case less likely to be diagnosed as antisocial and the male case less likely to be diagnosed as histrionic. Considering the influence of sex bias is paramount in understanding and interpreting gender differences in PD diagnoses. Furthermore, following structured interviews, we observed that male patients had a higher comorbidity ratio of PD types associated with the psychosis spectrum, specifically SCH and SCHT PDs, compared to female patients. This may be attributed to the more prevalent emotional and anxious personality traits in females, making them less likely to meet the criteria for PD diagnoses within the peculiar and eccentric cluster.
Numerous studies have consistently shown that individuals with SZ are more likely to have experienced CM compared to the general population. A meta-analysis conducted by Filippo Varese et alCitation48 which included 18 case-control studies, 10 prospective and quasi-prospective studies, and 8 population-based cross-sectional studies, found significant associations between adversity and SZ across all research designs. The overall effect size indicated an odds ratio (OR) of 2.78, suggesting that individuals with SZ were 2.72 times more likely to have experienced CM than controls. In our study, we observed that male patients with SZ self-reported a higher incidence of PA. This finding aligns with the sociocultural context, especially prevalent in Chinese society, where the cultural practice of “daughters should be raised with indulgence, while sons should be disciplined with strictness”. and the adage “spare the rod, spoil the son” may contribute to a higher likelihood of males self-reporting experiences of PA. The cultural nuances and social norms associated with male upbringing may create an environment where self-reporting PA is more socially acceptable for males. Cultural dynamics, traditional family structures, and societal expectations play a role in shaping the reporting patterns of CM, emphasizing the importance of considering sociocultural factors when interpreting and understanding the relationship between PA and the etiology of SZ.
The relatively lower Cronbach’s alpha value for the PN subscale compared to other CM components suggests potential challenges in the assessment of PN experiences. This discrepancy may arise from the lack of clarity in defining and operationalizing physical neglect, leading to variations in individuals’ interpretations and reporting of neglectful experiences. Additionally, the PN subscale items may encompass a wide range of behaviors and situations, contributing to substantial individual differences in perceived neglect. Furthermore, the absence of clinical symptom assessment in our study introduces another layer of complexity. Psychotic symptoms, such as hallucinations or delusions, can significantly impact an individual’s perception and recollection of past experiences, including instances of neglect. Consequently, variations in the severity of psychotic symptoms among participants may have influenced the reporting of PN experiences, contributing to the observed differences in Cronbach’s alpha values. These findings underscore the importance of refining definitions and assessment methods for PN in future research endeavors. Clear and standardized criteria for identifying and categorizing instances of physical neglect are crucial for ensuring consistency and reliability in reporting. Additionally, integrating comprehensive clinical assessments, including evaluations of psychotic symptom severity, can provide valuable insights into the interplay between CM experiences and psychiatric symptomatology.
Several limitations merit consideration in interpreting the findings of this study. Firstly, the cross-sectional design employed limits the ability to establish causal relationships; rather, the study provides descriptive comparisons. Future research could benefit from longitudinal designs, such as cohort studies, to delve deeper into causal connections. Secondly, recall bias is inherent in retrospective assessments, and the accuracy of recollections may be influenced by varying illness trajectories and ages in individuals with SZ. Moreover, the influence of psychotic symptoms on the recollection of childhood experiences may lead to the fabrication or misconstruction of abusive events. Additionally, it is important to acknowledge the limitation regarding the unavailability of data on the severity of psychotic symptoms in our study. Due to the extensive scope of assessments, focusing primarily on PD and CM, the study did not systematically evaluate the clinical symptoms of SZ patients. Consequently, the relationship between different symptom types and PD and CM remains unexplored. Future studies should aim to include measures of psychotic symptom severity to provide a more comprehensive understanding of these associations.
Conclusion
Our study reveals significant sex differences in self-reported PD traits among individuals with SZ. Male patients tend to exhibit personality pathology characterized by coldness and withdrawal, while female patients show a predilection for emotional and unstable traits. In the realm of CM, only PA is reported more frequently by male patients, with no significant disparities observed in other types of CM. These findings highlight the importance of recognizing and addressing sex-specific manifestations of personality pathology and the nuanced impact of CM in the clinical management of individuals with SZ.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
All authors confirm that there are no competing interests to disclose for this work.
Additional information
Funding
References
- Zhang T, Wang L, Good MJ, et al. Prevalence of personality disorders using two diagnostic systems in psychiatric outpatients in Shanghai, China: a comparison of uni-axial and multi-axial formulation. Soc Psychiatry Psychiatr Epidemiol. 2012;47(9):1409–1417. doi:10.1007/s00127-011-0445-x
- Simonsen E, Newton-Howes G. Personality Pathology and Schizophrenia. Schizophr Bull. 2018;44(6):1180–1184. doi:10.1093/schbul/sby053
- Donmezler S, Iskender G, Fistikci N, Altunkaynak Y, Ulusoy S, Berkol TD. Exploring the “Insight Paradox” in Treatment-Resistant Schizophrenia: correlations Between Dimensions of Insight and Depressive Symptoms in Patients Receiving Clozapine. Alpha Psychiatry. 2023;24(3):102–107. doi:10.5152/alphapsychiatry.2023.221030
- Charernboon T. Season of Birth in Patients with Schizophrenia in Thailand. Alpha Psychiatry. 2023;24(5):200–204.
- Belohradova Minarikova K, Prasko J, Holubova M, et al. Hallucinations and Other Psychotic Symptoms in Patients with Borderline Personality Disorder. Neuropsychiatr Dis Treat. 2022;18:787–799. doi:10.2147/NDT.S360013
- Boberg M, Felding S, Jansson L, Nordgaard J. Differential diagnosis: schizophrenia and personality disorder. Schizophr Res. 2022;248:171–172. doi:10.1016/j.schres.2022.08.010
- Wei Y, Zhang T, Chow A, et al. Co-morbidity of personality disorder in schizophrenia among psychiatric outpatients in China: data from epidemiologic survey in a clinical population. BMC Psychiatry. 2016;16(1):224. doi:10.1186/s12888-016-0920-8
- Zhang T, Chow A, Wang L, Dai Y, Xiao Z. Role of childhood traumatic experience in personality disorders in China. Compr Psychiatry. 2012;53(6):829–836. doi:10.1016/j.comppsych.2011.10.004
- Yang F, Hong X, Tao J, Chen Y, Zhang Y, Xiao H. Hair cortisol, social support, personality traits, and clinical course: differences in schizophrenia and bipolar disorder. Brain Behav. 2021;11(12):e2412. doi:10.1002/brb3.2412
- Zhu YK, Li CB, Jin J, et al. The 2D:4D ratio of the hand and schizotypal personality traits in schizophrenia patients and healthy control persons. Asian J Psychiatr. 2014;9:67–72. doi:10.1016/j.ajp.2014.01.005
- De portugal E, Gonzalez N, Miriam V, Haro JM, Usall J, Cervilla JA. Gender differences in delusional disorder: evidence from an outpatient sample. Psychiatry Res. 2010;177(1–2):235–239. doi:10.1016/j.psychres.2010.02.017
- Zhu R, Wang D, Zhou H, et al. Sex differences in prevalence and clinical correlates of insomnia in Chinese patients with chronic schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2023;273(3):601–611. doi:10.1007/s00406-022-01473-x
- Singh OP. Suicide Attempts in Schizophrenia and Their Relationship to Depression, Insight and Stigma. Alpha Psychiatry. 2022;23(1):26. doi:10.5152/alphapsychiatry.2022.2201011
- Hafner H. Gender differences in schizophrenia. Psychoneuroendocrinology. 2003;28 Suppl 2:17–54. doi:10.1016/S0306-4530(02)00125-7
- Schulte Holthausen B, Habel U. Sex Differences in Personality Disorders. Curr Psychiatry Rep. 2018;20(12):107. doi:10.1007/s11920-018-0975-y
- Sher L, Siever LJ, Goodman M, et al. Gender differences in the clinical characteristics and psychiatric comorbidity in patients with antisocial personality disorder. Psychiatry Res. 2015;229(3):685–689. doi:10.1016/j.psychres.2015.08.022
- Qian X, Townsend ML, Tan WJ, Grenyer BFS. Sex differences in borderline personality disorder: a scoping review. PLoS One. 2022;17(12):e0279015. doi:10.1371/journal.pone.0279015
- Wang L, Ross CA, Zhang T, et al. Frequency of borderline personality disorder among psychiatric outpatients in Shanghai. J Pers Disord. 2012;26(3):393–401. doi:10.1521/pedi.2012.26.3.393
- Alkema A, Marchi M, van der Zaag JAJ, et al. Childhood abuse v. neglect and risk for major psychiatric disorders. Psychol Med;2023. 1–12. doi:10.1017/S0033291723003471
- Weitkamper A, Kellner M, Iffland JR, et al. Childhood Maltreatment in Individuals With Schizophrenia Spectrum Disorders: the Impact of Cut-Off Scores on Prevalence Rates. Front Psychiatry. 2021;12:692492. doi:10.3389/fpsyt.2021.692492
- Read J, van Os J, Morrison AP, Ross CA. Childhood trauma, psychosis and schizophrenia: a literature review with theoretical and clinical implications. Acta Psychiatr Scand. 2005;112(5):330–350. doi:10.1111/j.1600-0447.2005.00634.x
- Morgan C, Fisher H. Environment and schizophrenia: environmental factors in schizophrenia: childhood trauma--a critical review. Schizophr Bull. 2007;33(1):3–10. doi:10.1093/schbul/sbl053
- Herzog P, Kube T, Fassbinder E. How childhood maltreatment alters perception and cognition - the predictive processing account of borderline personality disorder. Psychol Med. 2022;52(14):2899–2916. doi:10.1017/S0033291722002458
- Hock RS, Bryce CP, Fischer L, et al. Childhood malnutrition and maltreatment are linked with personality disorder symptoms in adulthood: results from a Barbados lifespan cohort. Psychiatry Res. 2018;269:301–308. doi:10.1016/j.psychres.2018.05.085
- Caldirola D, Torti T, Cuniberti F, et al. No Sex Differences in Self-Reported Childhood Maltreatment in Major Depressive and Bipolar Disorders: a Retrospective Study. Brain Sci. 2022;12(6):804. doi:10.3390/brainsci12060804
- Liu A, Liu M, Ren Y, Lin W, Wu X. Exploring gender differences in the relationships among childhood maltreatment, PTSD, and depression in young adults through network analysis. Child Abuse Negl. 2023;146:106503. doi:10.1016/j.chiabu.2023.106503
- Hyler SE, Skodol AE, Oldham JM, Kellman HD, Doidge N. Validity of the Personality Diagnostic Questionnaire-Revised: a replication in an outpatient sample. Compr Psychiatry. 1992;33(2):73–77. doi:10.1016/0010-440X(92)90001-7
- Zhang T, Li H, Tang Y, et al. Screening schizotypal personality disorder for detection of clinical high risk of psychosis in Chinese mental health services. Psychiatry Res. 2015;228(3):664–670. doi:10.1016/j.psychres.2015.04.049
- Zheng Y, Severino F, Hui L, Wu H, Wang J, Zhang T. Co-Morbidity of DSM-IV Personality Disorder in Major Depressive Disorder Among Psychiatric Outpatients in China: a Further Analysis of an Epidemiologic Survey in a Clinical Population. Front Psychiatry. 2019;10:833. doi:10.3389/fpsyt.2019.00833
- Wang J, Sun W, Tang X, et al. Transdiagnostic Dimensions towards Personality Pathology and Childhood Traumatic Experience in a Clinical Sample: subtype Classification by a Cross-sectional Analysis. Sci Rep. 2019;9(1):11248. doi:10.1038/s41598-019-47754-9
- Wang J, Chen Z, Sun W, et al. A Strategy to Address High Comorbidity of Personality Disorders in a Chinese Population: a Principal and Subordinate Diagnostic Model. Psychiatry. 2019;82(3):272–282. doi:10.1080/00332747.2019.1600218
- Dai Y, Xiao Z, Wang Z, Zhang H, Chen J. The reliability and validity of a Chinese version of the structured clinical interview for DSM-IV personality disorders. Shanghai ArchPsychiatry. 2006;18:1–4.
- Zhao X, Zhang Y, Li L, Zhou Y, Li H, Yang S. Reliability and validity of the Chinese version of childhood trauma questionnaire. Chin J Clin Rehabil. 2005;9:105–107.
- He J, Zhong X, Gao Y, Xiong G, Yao S. Psychometric properties of the Chinese version of the Childhood Trauma Questionnaire-Short Form (CTQ-SF) among undergraduates and depressive patients. Child Abuse Negl. 2019;91:102–108. doi:10.1016/j.chiabu.2019.03.009
- Fink LA, Bernstein D, Handelsman L, Foote J, Lovejoy M. Initial reliability and validity of the childhood trauma interview: a new multidimensional measure of childhood interpersonal trauma. Am J Psychiatry. 1995;152(9):1329–1335.
- Bernstein DP, Fink L, Handelsman L, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry. 1994;151(8):1132–1136.
- Wu Y, Zheng Y, Wang J, Zhang T. Specific type of childhood trauma and borderline personality disorder in Chinese patients. Front Psychiatry. 2022;13:936739. doi:10.3389/fpsyt.2022.936739
- Moran P, Hodgins S. The correlates of comorbid antisocial personality disorder in schizophrenia. Schizophr Bull. 2004;30(4):791–802. doi:10.1093/oxfordjournals.schbul.a007132
- Robins LN, Price RK. Adult disorders predicted by childhood conduct problems: results from the NIMH Epidemiologic Catchment Area project. Psychiatry. 1991;54(2):116–132. doi:10.1080/00332747.1991.11024540
- Crosby JP, Sprock J. Effect of patient sex, clinician sex, and sex role on the diagnosis of Antisocial Personality Disorder: models of underpathologizing and overpathologizing biases. J Clin Psychol. 2004;60(6):583–604. doi:10.1002/jclp.10235
- Cale EM, Lilienfeld SO. Sex differences in psychopathy and antisocial personality disorder. A review and integration. Clin Psychol Rev. 2002;22(8):1179–1207. doi:10.1016/S0272-7358(01)00125-8
- Alegria AA, Blanco C, Petry NM, et al. Sex differences in antisocial personality disorder: results from the National Epidemiological Survey on Alcohol and Related Conditions. Personal Disord. 2013;4(3):214–222. doi:10.1037/a0031681
- Paris J. Gender differences in personality traits and disorders. Curr Psychiatry Rep. 2004;6(1):71–74. doi:10.1007/s11920-004-0042-8
- Xiang YT, Wang CY, Weng YZ, et al. Sex differences in patients with schizophrenia: a prospective, multi-center study. Psychiatry Res. 2010;177(3):294–298. doi:10.1016/j.psychres.2010.03.014
- Hu Q, Chen Z, Lin Z, et al. Gender differences in screening self-reported psychotic symptoms in a first help-seeking population. Arch Womens Ment Health. 2022;25(2):291–299. doi:10.1007/s00737-021-01170-z
- Torniainen M, Suvisaari J, Partonen T, et al. Sex differences in cognition among persons with schizophrenia and healthy first-degree relatives. Psychiatry Res. 2011;188(1):7–12. doi:10.1016/j.psychres.2010.11.009
- Samuel DB, Widiger TA. Comparative gender biases in models of personality disorder. Personality and Mental Health. 2009;3(4):12–25. doi:10.1002/pmh.61
- Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38(4):661–671. doi:10.1093/schbul/sbs050

