Abstract
Purpose
To compare change of macular thickness after uneventful cataract surgery and after cataract surgery complicated with vitreous loss, using optic coherence tomography (OCT).
Methods
Twenty eyes of 20 patients who underwent cataract surgery complicated with posterior capsular tear participated in this retrospective study (Group 2). The fellow eyes of those patients who underwent uneventful cataract surgery served as the control group (Group 1). Best spectacle-corrected visual acuity (BCVA), refraction, keratometry, axial length measurement, intraocular lens power calculation, intraocular pressure, and biomicroscopic and posterior segment examinations were done preoperatively. BCVA was evaluated at the postoperative 1st day, 1st week, 1st month, and 3rd month. Macular thickness and volumetric measurements with OCT with MM5 protocol were conducted at the postoperative 3rd month.
Results
Logarithm of the minimum angle of resolution BCVA of Group 1 was significantly better than Group 2 at all intervals (P < 0.05). Foveal, parafoveal (superior and temporal), and perifoveal (superior and temporal) macular thickness measurements were significantly higher in Group 2 at month 3 (P < 0.05). Foveal volume was also significantly higher in Group 2 when compared with Group 1 (P < 0.05). In Group 2, two eyes (10%) were diagnosed with clinically significant cystoid macular edema at the 1-month visit.
Conclusion
Macular thickness was found to be significantly high in eyes undergoing complicated cataract surgery (with posterior capsular tear) when compared with uneventful cataract surgeries of fellow eyes.
Keywords:
Introduction
Cystoid macular edema (CME) remains an important cause limiting favorable visual outcomes following cataract surgery. Although incidence of CME decreased within the small-incision phacoemulsification era, it has been reported that incidence of CME (affecting visual outcome) after small-incision uneventful cataract surgery is between 0% and 9%.Citation1–Citation3 Furthermore, incidence of angiographic leakage following uneventful cataract is reported to be between 9.1% and 20.4%.Citation2–Citation4
Angiographic CME is diagnosed in asymptomatic patients who have detectable leakage from the perifoveal capillaries on fluorescein angiography (FA). Clinical CME is diagnosed in patients who have visual impairment as well as angiographic findings. Clinical diagnosis of CME is confirmed by using optical coherence tomography (OCT) and FA.Citation1–Citation4
Proposed causative factors for development of CME following cataract surgery includes surgical trauma (especially to the iris), postoperative inflammation, and tractional forces on macula.Citation1,Citation3,Citation4 The pathophysiology is not fully understood, but disruption of blood aqueous barrier following surgical trauma and release of prostaglandins may cause unstable blood retinal barrier and increased permeability in perifoveal capillaries, and liquid accumulation in extracellular spaces, leading to increased macular thickness and CME.Citation4
In the last decade, OCT has been established as a practical method for examining retinal architecture. OCT, with its noninvasive nature, has been proven to be an indispensable tool for diagnosing retinal pathologies including CME. Many studies have reported incidences of CME and macular thickness changes determined by OCT following uneventful cataract surgeries.Citation5,Citation6
An uneventful cataract surgery with intraocular lens implantation in-the-bag is not supposed to cause aforementioned factors. However, complicated cataract surgery (with posterior capsular tear) could be closely involved with proposed mechanisms, but to the authors’ knowledge, no study has evaluated macular thickness and volume determined by OCT following complicated cataract surgery.
The aim of this study was to compare macular thickness and macular volume using OCT as well as incidences of CME between eyes which underwent cataract surgery complicated by posterior capsular tear and the fellow eyes which underwent uneventful cataract surgery.
Materials and method
Twenty patients who had undergone bilateral cataract surgery (one eye with uneventful small-incision phacoemulsification, the fellow eye with small-incision phacoemulsification complicated by posterior capsular tear) between September 2009 and September 2011 were included in the study.
Patients with (1) previous ocular surgery history, (2) significant eye trauma history, (3) any coexisting ocular pathology that could affect visual acuity or macular thickness (eg, corneal opacity, age-related macular degeneration, glaucoma), (4) diagnosis of diabetes mellitus, or (5) history of uveitis were not included in the study. A 19-year-old patient was diagnosed with congenital cataract; the remainder of the study population was diagnosed with senile cataract.
All eyes underwent routine preoperative evaluation before cataract surgeries, including best-corrected visual acuity (BCVA), slit lamp biomicroscopy, measurement of intraocular pressure by applanation tonometry, and fundus examination. All surgeries were performed under subtenon anesthesia.
Phacoemulsification was carried out in a standard fashion through a 3.0-mm clear corneal tunnel incision with a foldable hydrophobic acrylic intraocular lens implantation in the capsular bag. Eyes with posterior capsule tear had comprehensive anterior vitrectomy prior to implantation of a foldable hydrophobic three-piece intraocular lens with polymethylmethacrylate haptics into ciliary sulcus (posterior chamber).
Signs of vitreous in the anterior chamber, including a peaked pupil or presence of vitreous at the wound on assessment with a dry methylcellulose sponge were evaluated before surgeries were finished. Patients with complicated surgeries who were managed by enlarging main incision and/or needed suturing of corneal incisions, or did not have intra-ocular lens implantation, were not included in the study. At the end of the surgeries, all eyes received subconjunctival dexamethasone injection.
Postoperatively, all patients received the same standard medication regimen of antibiotic (Exocin; Allergan, France SA) and corticosteroid drops (Predforte; Allergan, Markham, Canada) five times daily, tapered over 4 weeks.
Follow-up appointments were at the postoperative 1st day, 1st week, 1st month, and 3rd month. At each visit, BCVA, slit-lamp biomicroscopy f indings, intraocular pressure measured by applanation tonometry, and dilated fundus examinations were performed and recorded. At the postoperative 3rd month visit, OCT scans were conducted in addition to abovementioned examinations. Imaging was performed by OCT (RTVue-100; Optovue, Fremont, CA). BCVA was measured at each visit with Snellen Chart and converted to the logarithm of the minimum angle of resolution (LogMAR) equivalent for the statistical analysis.
OCT imaging technique
All eyes were dilated before OCT examination. All OCT scans were centered on fovea by providing a central, internal fixation mark, and were performed by one experienced operator. The RTVue-100 had a 5 μm axial image resolution and imaging speed of 26,000 axial scans per second. On the RTVue-100, the MM5 (5 × 5 mm2 grid of eleven horizontal and eleven vertical lines with 668 A-scans each and an inner 3 × 3 mm2 grid of six horizontal and six vertical lines with 400 A-scans each) protocols were used, with all scans having signal strength of at least 40 (range, 40.4–79.4). Scans with low quality and blinks were not included and repeated. In all measurements, retinal thickness and volumetric analyses were performed in the circle with 1 mm diameter in the central macula (fovea), in the area between this circle and the surrounding circle with 3 mm diameter in four equal quadrants (parafoveal area; superior, inferior, temporal, and nasal), and in the remaining area beyond these quadrants and the surrounding circle with 5 mm diameter in four equal quadrants (perifoveal area; superior, inferior, temporal, and nasal).
Main outcome measures were BCVA at each follow-up appointment, macular thickness, and macular volume measured at the postoperative 3rd month.
Statistical analysis
NCSS (Number Cruncher Statistical System) 2007 and PASS 2008 statistical software (NCSS, Kaysville, UT) were used for statistical analysis. Student’s t-test was used to evaluate differences between groups. P value less than 0.05 was considered statistically significant. One-way analysis of variance test was used for comparison of the parameters between groups.
Results
The mean age of the patients was 67.30 ± 14.61 years (range, 19–89 years). There were nine female and eleven male patients. Among the eyes having undergone uncomplicated phacoemulsification, there were 12 right and eight left eyes. Among the eyes having undergone complicated phacoemulsification, there were eight right eyes and 12 left eyes. Average delay between two surgeries was 2.6 ± 0.98 months. Four patients had complicated surgery followed by an uneventful surgery, and 16 patients had uneventful surgeries followed by complicated surgeries.
There was no significant difference between the two groups in terms of preoperative BCVA (0.72 ± 0.25 and 0.65 ± 0.25, respectively). During postoperative follow-up, LogMAR BCVA of Group 1 was significantly better than Group 2 at all intervals (1st day, 1st week, 1st month, and 3rd month) (). On the postoperative 3rd month, mean LogMAR BCVA of Group 1 was significantly better than mean LogMAR BCVA of Group 2 (0.1 ± 0.08 versus 0.19 ± 0.16, respectively; P = 0.02).
Table 1 Comparison of preoperative and postoperative BCVA between Group 1 and Group 2
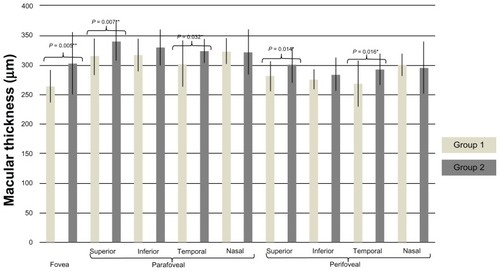
Comparison of macular thickness of Group 1 and Group 2 at the postoperative 3rd month showed that foveal macular thickness of Group 1 was significantly lower than Group 2 (264.48 ± 26.91 versus 303.95 ± 53.01; P = 0.005). Also, superior and temporal parafoveal measurements were significantly higher in Group 2 (315.16 ± 29.82 versus 340.35 ± 33.08, P = 0.007; and 302.74 ± 38.20 versus 323.30 ± 20.68, P = 0.032, respectively). Similarly, analysis of perifoveal macular thickness showed significant difference between the two groups in superior and temporal perifoveal regions (281.16 ± 25.45 versus 301.30 ± 30.38, P = 0.014; and 268.09 ± 39.05 versus 292.80 ± 26.33, P = 0.016, respectively). Analysis of macular thickness of both parafoveal and perifoveal inferior and nasal regions showed no statistically significant difference ().
Figure 1 Comparison of macular thickness between Group 1 and Group 2 at the postoperative 3rd month.
Foveal volume was also significantly higher in Group 1 (2.128 ± 0.35 versus 1.968 ± 0.16; P = 0.032) ().
Table 2 Evaluation of the foveal macular volume in Group 1 and Group 2
In the follow-up period, CME was not diagnosed at any eye in Group 1. In Group 2, two eyes (10%) were diagnosed with clinically significant CME on the 1st month visit. Eyes were treated with a regime of additional ketorolac tromethamine 0.4% (Acular LS; Allergan Inc, Irvine, CA) eye drops four times a day with continuation of prednisolone acetate four times a day. In one eye, CME resolved within 4 weeks. In the other eyes, CME resolved after 20 weeks.
Discussion
In this study, OCT was utilized for quantitative evaluation of macula following complicated and uneventful cataract surgery. It was found that, at the postoperative 3rd month, macular thickness was significantly higher after cataract surgeries with posterior capsular tear.
Most common factors proposed to cause postoperative CME include increased prostaglandin production due to surgical trauma and mechanical tractions by vitreoretinal adhesions.Citation1,Citation2,Citation4 Therefore, it was no surprise that complicated surgeries with relatively longer surgical time (surgical trauma presumably), longer exposure to microscope light, and vitreous traction had repercussions on macular thickness.
However, to the best of the authors’ knowledge, there is no study evaluating macular thickness after complicated cataract surgery using a quantitative method such as OCT. Besides, this study also allowed a comparison to be made with fellow eyes which underwent uneventful surgeries.
In this current series, the incidence of CME was 10% after complicated surgeries, while none of the eyes with uneventful cataract surgery developed CME. Studies with a higher number of patients evaluating cataract surgeries complicated by posterior capsular tear report 6.8%,Citation7 8.7%,Citation8 and 10%Citation9 incidences of CME. Several studies reported varying incidences of postoperative CME.Citation1–Citation5,Citation10 Definition of CME and the diagnostic method to evaluate it (with angiography or OCT) were main variables which caused the reported variability of incidences.
Also, some studies included eyes which were more prone to developing CME or directly focused on evaluating patients such as diabetics.Citation11–Citation13 In this present study, patients with diagnosis of diabetes mellitus or history of uveitis were excluded. These eyes were presumed to be more susceptible to surgical trauma because of earlier history of disrupted blood–aqueous and/or blood–retina barrier. Thus, the reason no cases of CME were encountered following uneventful cataract surgeries may be attributed to the exclusion criteria.
Evaluation of CME by using OCT as a measuring tool has led many authors to investigate macular thickness quantitatively. Macular thickness was found to increase even following uneventful cataract surgeries when compared with preoperative values. Biro et al reported significant increase of the foveal and perifoveal thickness at 1 week, 1 month, and 2 months after uneventful cataract surgery.Citation14 In another study by Cagini et al, an asymptomatic increase in macular thickness and volume at 12 weeks was reported to be observed with respect to preoperative values.Citation15 On the other hand, Nicholas et al reported a significant correlation between foveal minimum thickness and BCVA 6 weeks following routine cataract surgery.Citation1 In a similar study, von Jagow et al reported significant increase in foveal thickness but no correlation with visual acuity and concluded that this increase may depend both on anatomical changes and measurement technique following change of media opacity.Citation6 Interestingly, one of the weaknesses of this present study was absence of preoperative OCT images due to significant cataracts which prevented good quality OCT scans. Thus, the study did not compare the change of macular thickness before and after cataract surgery. However, taking fellow eyes as control group provided a good comparative control group.
In terms of visual rehabilitation, BCVA was found to be better after uneventful cataract surgeries than complicated ones during the follow-up period. In earlier visits, worse visual outcomes after complicated surgeries were expected due to collateral damage to anterior structures: corneal edema, flare, or ocular surface disorder.
In addition, one of limitations of this study was that making a flawless comparison was quite difficult because when cataract surgeries got complicated, applying a standard protocol was naturally impossible. However, the authos believe that this study was internally valid because all posterior capsular ruptures were managed using similar techniques (eg, anterior vitrectomy, foldable three-piece intraocular lens implantation to posterior chamber) and eyes which needed extra manipulations (eg, corneal suturing of main incisions, staining of vitreous with triamcinolone) were not included in the study. Furthermore, on the 3-month visit, all anterior chambers were found to be uniform, with some subtle differences of corneal thickness and iris atrophies of varying degrees.
To the best of the authors’ knowledge, there has been no study comparing macular thickness after complicated cataract surgery. Significantly higher rates of foveal, parafoveal, and perifoveal thicknesses were found in eyes which had complicated cataract surgery compared with fellow eyes which underwent uneventful cataract surgery. The authors believe that comparative studies with long-term follow-up would be beneficial.
Disclosure
The authors report no conflicts of interest in this work.
References
- NicholasSRileyAPatelHNeveldsonBPurdieGWellsAPCorrelations between optical coherence tomography measurement of macular thickness and visual acuity after cataract extractionClin Experiment Ophthalmol2006342124129 quiz 19416626425
- MentesJErakgunTAfrashiFKerciGIncidence of cystoid macular edema after uncomplicated phacoemulsificationOphthalmologica2003217640841214573973
- GulkilikGKocaboraSTaskapiliMEnginGCystoid macular edema after phacoemulsification: risk factors and effect on visual acuityCan J Ophthalmol200641669970317224950
- UrsellPGSpaltonDJWhitcupSMNussenblattRBCystoid macular edema after phacoemulsification: relationship to blood-aqueous barrier damage and visual acuityJ Cataract Refract Surg199925111492149710569164
- VukicevicMGinTAl-QureshiSPrevalence of optical coherence tomography-diagnosed post-operative cystoid macular oedema in patients following uncomplicated phacoemulsification cataract surgeryClin Experiment Ophthalmol201240328228721718410
- von JagowBOhrloffCKohnenTMacular thickness after uneventful cataract surgery determined by optical coherence tomographyGraefes Arch Clin Exp Ophthalmol2007245121765177117619896
- OnalSGozumNGucukogluAVisual results and complications of posterior chamber intraocular lens implantation after capsular tear during phacoemulsificationOphthalmic Surg Lasers Imaging200435321922415185790
- KonstantopoulosAYadegarfarGMadhusudhanaKPrognostic factors that determine visual outcome following cataract surgery complicated by vitreous lossEur J Ophthalmol200919224725319253242
- BlomquistPHRugwaniRMVisual outcomes after vitreous loss during cataract surgery performed by residentsJ Cataract Refract Surg200228584785211978467
- PerenteIUtineCAOzturkerCEvaluation of macular changes after uncomplicated phacoemulsification surgery by optical coherence tomographyCurr Eye Res200732324124717453944
- BiroZBallaZOCT measurements on the foveal and perifoveal retinal thickness on diabetic patients after phacoemulsification and IOL implantationEye (Lond)201024463964719590521
- KimSJEquiRBresslerNMAnalysis of macular edema after cataract surgery in patients with diabetes using optical coherence tomographyOphthalmology2007114588188917275910
- KimSJBelairMLBresslerNMA method of reporting macular edema after cataract surgery using optical coherence tomographyRetina200828687087618536605
- BiroZBallaZKovacsBChange of foveal and perifoveal thickness measured by OCT after phacoemulsification and IOL implantationEye (Lond)200822181216751754
- CaginiCFioreTIaccheriBPiccinelliFRicciMAFruttiniDMacular thickness measured by optical coherence tomography in a healthy population before and after uncomplicated cataract phacoemulsification surgeryCurr Eye Res200934121036104119958122
