Abstract
Vogt–Koyanagi–Harada syndrome is a cause of noninfectious panuveitis, leading to significant vision loss in many patients. It is an autoimmune disease occurring in genetically susceptible individuals and clinically presents as bilateral panuveitis with serous retinal detachments and hyperemic, swollen optic discs, which are associated with neurological and auditory manifestations. Early diagnosis and prompt and adequate treatment with immunosuppressive agents (corticosteroids and other immunosuppressive drugs) may halt disease progression and prevent recurrences and vision loss. This review summarizes the current knowledge on the variable clinical aspects of this disease, highlighting diagnostic and treatment strategies.
Introduction
Vogt–Koyanagi–Harada disease (VKHD) is a sight-threatening disease and a common cause of noninfectious panuveitis.Citation1,Citation2 It is described as a multisystemic, granulomatous inflammation related to T-cell-mediated autoimmune dysregulation, targeting melanocytic self-antigens. The tyrosinase family proteins and gp100 are common antigenic targets for VKHD.Citation1,Citation3–Citation5 The disease has a predilection for affecting melanocyte-containing tissues in the eye, the central nervous system (CNS), the inner ear and the skin, appears in genetically susceptible individuals and is related to HLA-DRB1*0405.Citation6–Citation8 Patients usually present with bilateral panuveitis preceded by a mild prodromal illness, associated with neurological and auditory features. However, it is common for patients to present with isolated ocular involvement during the early phases of the disease, with the choroid being the main site of ocular inflammation together with potential involvement of the iris and ciliary body. During the early acute phase of the disease, the inflammation is characterized by non-necrotizing diffuse granulomas, which persist following recurrences (chronic recurrent phase). As the disease progresses, it undergoes a chronic convalescent phase, which is characterized by a non-granulomatous inflammation, with later involvement of the choriocapillaris in the chronic recurrent phase.Citation9,Citation10 The disease has a variable clinical presentation, and clinical diagnosis is aided by the help of ophthalmic imaging such as fundus fluorescein angiography (FFA), indocyanine green angiography (ICG), and optical coherence tomography (OCT). Novel diagnostic techniques, which can demonstrate choroidal structure and precise retinal function, are now employed to assist in early diagnosis, leading to prompt treatment and monitoring of ongoing ocular inflammation.
Historical aspects and epidemiology
Ocular inflammation with poliosis was described in the first century AD by Ali-ibn-Isa.Citation11 In 1906, VogtCitation12 reported a case of a 16-year-old patient with iridocyclitis and poliosis. In 1929, Yoshizo Koyanagi described 16 cases with similar features, including six new cases.Citation13 In addition to the anterior uveitis and extraocular manifestations described by Vogt and Koyanagi, HaradaCitation14 described in 1926 a primarily posterior uveitis with exudative retinal detachments and pleocytosis of cerebrospinal fluid (CSF): an abnormal increase in the amount of lymphocytes and monocytes with normal glucose, as well as the prodromal phase of the disease and the integumentary signs. These findings were later noted by Babel, Bruno, and McPherson to represent a single, progressive syndrome, and the name was combined into VKHD syndrome.Citation15
VKHD has variable incidence; it appears to be more prevalent in people with Asian, Hispanic, Indian, Native American, or Mediterranean origin, accounting for 7%–22.4% of uveitis referrals.Citation16–Citation21 It is uncommon in Caucasians and people of Turkish descent, where it accounts for <3% of uveitis referrals.Citation22–Citation25 VKHD commonly affects young femalesCitation26–Citation28 between 20 and 50 years of age,Citation1 at a ratio of 2:1 in most large series.Citation29 However, pediatric cases,Citation30–Citation32 elderly onsetCitation33 and equal sex predilection have been reported in some studies.Citation34
Classification and clinical features
According to the revised diagnostic criteria proposed by the American Uveitis Society,Citation35 in its complete form, VKHD is defined as a non-traumatic bilateral panuveitis and is associated with integumentary, neurological/auditory signs. Probable (ocular) VKHD is characterized as matching ocular manifestations but in the absence of extraocular manifestations. Patients with the incomplete form of the disease usually present with bilateral ocular involvement with either integumentary features or neurologic/auditory manifestations.Citation35 In all forms of the disease, there should be no history of ocular surgery and no clinical or laboratory evidence suggestive of other ocular diseases.Citation35 It is important to recognize that although classically VKHD is a multisystemic disease, patients may fail to develop the complete or incomplete forms, and isolated ocular involvement has been reported in 45% of patients with acute VKHD and up to 58% of those presenting with chronic disease.Citation36
VKHD is a multiphasic disease that classically has four clinical phases or stages with variable clinical features in different ethnic groups: 1) prodromal; 2) acute; 3) chronic convalescent; and 4) chronic recurrent stage.
The prodromal phase, which may mimic a viral infection, generally precedes the ocular inflammation by a few days and lasts for 1–2 weeks. Patients typically complain of CNS and auditory symptoms including headaches, neck stiffness, photophobia, fever, orbital pain, scalp or skin sensitivity, and focal neurological deficits such as cranial nerve palsies.Citation1,Citation28 They may also have hearing loss, particularly for higher frequencies, dysacousia, vertigo, and tinnitus,Citation1,Citation37,Citation38 with less frequent auditory features observed in Hispanic patients.Citation39 CSF samples from lumbar punctures show pleocytosis in >80% of cases,Citation40,Citation41 and brain imaging studies can occasionally demonstrate focal parenchymal lesions.Citation42
In the eye, the acute phase of VKHD is characterized by a panuveitis or posterior uveitis with multifocal serous retinal detachments (SRDs). Vitreous inflammation is commonly noted with a low-grade non-granulomatous anterior uveitis seen in some patients.Citation10,Citation34,Citation41 The diffuse choroidal thickening seen on OCT scans during the acute phase of VKHD correlates with diffuse mononuclear inflammatory cellular infiltration of the uvea with sparing of the choriocapillarisCitation9 and the appearance of Dalen-Fuchs nodules on histopathological studies. The Dalen-Fuchs nodules are aggregates of lymphocytes and pigment-laden macrophages that appear mainly in the posterior pole between Bruch membrane and the retinal pigment epithelium (RPE).Citation9,Citation10 The inflammation lasts several weeks, and early treatment may prevent the later development of the chronic phases of the disease in up to a third of cases.Citation26,Citation43,Citation44 However, progression to the chronic convalescence phase occurs in 28%–62% of patients who present with acute VKHD, possibly due to more severe and rapid disease onset.Citation26,Citation45
The chronic convalescence phase usually develops 3–4 months after the onset of the disease and lasts from several weeks to years, during which time patients usually present with non-granulomatous panuveitis, poliosis of the eyebrows and eyelashes, vitiligo, and alopecia, as well as depigmentation of the choroid resulting in a bright-orange hue. The optic nerve remains pale, leading to the appearance of sunset glow fundus.Citation1,Citation2 This depigmentation of the integumentary system usually follows ocular and CNS involvement in VKHD and is more commonly seen in Japanese than in Hispanic patients.Citation1,Citation39 Despite early high-dose corticosteroid treatment, progression to the chronic recurrent phase may occur in up to 79% of the total cases who presented with acute VKHD.Citation44
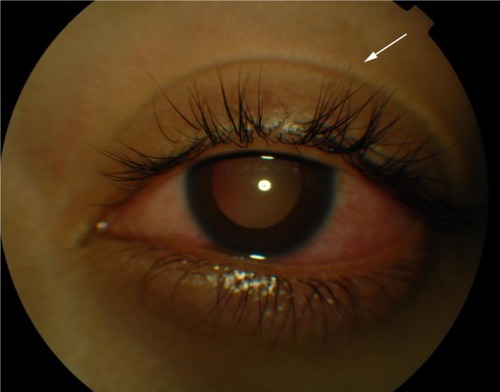
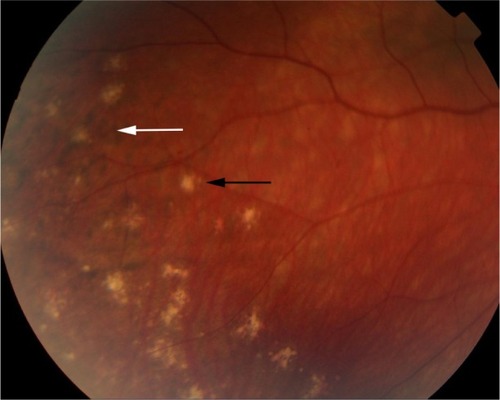
During the chronic recurrent phase, patients present with recurrent granulomatous anterior uveitis (), and choroidal thickening develops.Citation46–Citation48 Approximately 25% of VKHD patients develop posterior and anterior segment recurrences, mainly in cases of more aggressive disease with poor response to immunosuppressive treatment.Citation27 Anterior segment recurrences were found to be associated with choroidal inflammation and insufficient choroidal circulation demonstrated on ICG and OCT scans.Citation48,Citation49
Ocular findings in VKHD
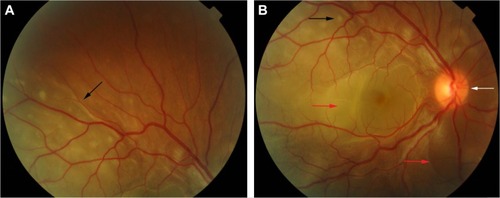
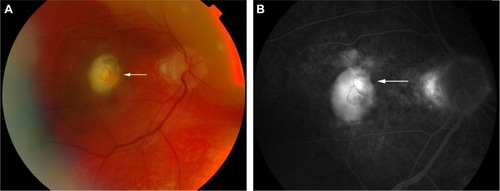
In the eye, orbital pain, photosensitivity and tearing have been reported during the prodromal phase of VKHD.Citation1 As the disease progresses to the acute phase, panuveitis manifests and patients commonly present with transient attacks of panuveitis or posterior uveitis with multifocal choroiditis lesions (), which progress to multifocal serous detachments and can coalesce into diffuse SRD (),Citation41,Citation50 resulting in reduced vision. SRD might initially be misdiagnosed as central serous chorioretinopathy (CSCR).Citation51 However, in the absence of ocular inflammation and other systemic features of VKHD, the presence of optic disc hyperemia and disc leakage on FFA support the diagnosis of VKHD rather than CSCR.Citation51
Figure 2 Color retinal photographs of a patient during the acute phase of VKHD.
Abbreviations: VKHD, Vogt–Koyanagi–Harada disease; SRDs, serous retinal detachments.
Although bilateral simultaneous involvement has been observed in the majority of patients, involvement of the second eye can take up to 2 weeks, with delayed involvement reported to occur up to 6 years after the first eye.Citation52 Sporadic cases of uniocular disease have also been reported with a follow-up time of 16 years;Citation32,Citation53,Citation54 therefore, uniocular presentation should not exclude the diagnosis or delay starting treatment.
Unilateral and bilateral optic disc hyperemia () without visual field loss is a frequent presentation in acute VKHDCitation55–Citation57 and is the most common finding in acute VKHD patients with no SRD at presentation.Citation58
Figure 3 Color retinal photographs of right (A) and left eye (B) showing swollen and hyperemic optic discs (white arrows), with choroidal folds disc (black arrows), in the acute phase of VKHD.
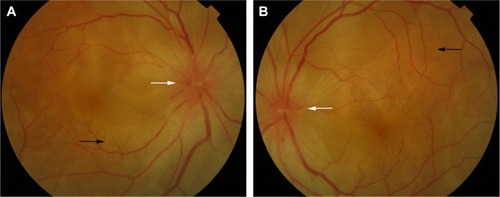
Optic disc involvement in acute VKHD is found to be more common in females and patients with a mean age of 55 years, who also have a greater likelihood of vision loss or progression to the chronic phases.Citation50 In addition to older age at presentation, optic disc swelling is found to correlate significantly with the morphology of the optic nerve (a smaller cup-to-disc ratio and a higher disc–macula distance to disc diameter).Citation57 Swollen optic discs may be the only presenting sign and should be differentiated from other conditions,Citation56 such as optic neuritis,Citation59 diabetic papillopathy,Citation58 central retinal vein occlusion, or anterior ischemic optic neuropathy (AION). Extensive optic disc swelling can itself lead to further optic nerve pathology, and patients can develop AION following the resolution of the optic disc swelling and SRD. This is thought to be due to an impaired posterior ciliary artery supply to the optic nerve, secondary to severe choroidal inflammation.Citation60–Citation62 Involvement of the optic nerve leading to fixed dilated pupils has also been observed in a 28-year-old patient with acute VKHD.Citation63
Choroidal folds are ripples in the RPE, Bruch membrane and the inner aspect of the choroid and have been described to accompany or precede the development of SRD in up to 71% of eyes with acute VKHD.Citation64 These folds () can be detected on fundus examination and are more easily identifiable on FFA, ICG, and OCT scans.Citation65–Citation67 Their reappearance on OCT is predictive of recurrence of SRD.Citation68 In studies examining VKHD patients, choroidal folds were noted in between 12% and 57% of cases. Their occurrence was related with poor visual acuity at presentation, as well as poor visual outcome,Citation65,Citation66,Citation69 disc swelling, and the development of choroidal thinning and sunset glow fundus later in the course of the disease.Citation69
Scleral involvement in patients in the acute phase of VKHD has been observed with case reports of patients presented with unilateral or bilateral posterior scleritis and choroidal thickening.Citation70 Extraocular features of VKHD with bilateral posterior scleritis, bilateral SRD, and optic disc swelling were also observed.Citation71
Rare presentations of acute VKHD include angle closure glaucoma, moderately elevated intraocular pressure (IOP) with variable degrees of intraocular inflammationCitation72–Citation74 or RPE tears that can be seen bilaterally without choroidal neovascularization (CNV) and are thought to be due to acute choroidal inflammation.Citation75 Vitreomacular traction (VMT) that rapidly progresses to full-thickness macular hole (MH) formation has also been noted to develop during acute VKHD,Citation76 possibly due to active inflammation.
In eyes that progress to the chronic convalescence stage, resolution of SRDs with the development of chorioretinal depigmentation results in an orange-red discoloration of the fundus giving the distinct sunset glow fundal appearance () and perilimbal vitiligo (Sugiura’s sign), which suggest ongoing uveal inflammation. Sunset glow fundus has been reported to develop as soon as 4 months after the initial presentation, despite treatment with high-dose immunosuppressive agents.Citation10,Citation45 Histological studies suggest that this is secondary to choroidal melanocyte loss from diffuse granulomatous choroiditis.Citation10,Citation77 The development of sunset glow fundus was found to be related to increased numbers of inflammatory cells in CSF samples and severe CNS involvement at presentation.Citation78
Figure 4 Color retinal photographs of right (A) and left eye (B) during the convalescent phase of VKHD, showing sunset glow fundus with pale optic discs (white arrows) and bright-orange choroids (black arrows). Note the peripapillary atrophy (gray arrow) and macular scaring (blue arrow) in (A).
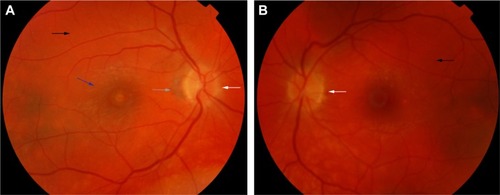
The convalescent phase is further characterized by the appearance of numerous small choroidal depigmented atrophic and hyperpigmented lesions in the retinal periphery ()Citation79 and peripapillary subretinal fibrosis lesions (), as well as the Dalen-Fuchs nodules that can be seen in all phases of the disease.Citation9,Citation10 Choroidal atrophy due to subfoveal loss of the choriocapillaris has been confirmed on spectral domain OCT (SD-OCT) scans and correlated with duration of the disease, lower visual acuity, and atrophy of overlying retina and RPE.Citation80
Figure 5 Color retinal photograph displaying sunset glow fundus with a numerous small choroidal depigmented atrophic lesions (black arrow) and hyperpigmented lesions (white arrow) in the retinal periphery during the convalescent phase of VKHD.
Other uncommon findings in this phase of the disease include progressive scleral changes and posterior scleritis possibly due to ongoing chronic choroidal inflammation,Citation81–Citation83 as well as VMT and epiretinal membranes (ERMs), possibly due to RPE migration later in the course of the disease.Citation84
The chronic recurrent phase is characterized by episodes of granulomatous anterior uveitis with mutton fat keratic precipitates, iris nodules, and posterior synechiae.Citation46 A prospective study that examined 70 eyes with acute VKHD and 92 eyes with recurrent disease, before and after treatment with immunosuppressive agents, showed a significantly higher anterior segment cell count and flare level in the eyes during the chronic recurrent phase, possibly reflecting a refractory inflammation with lasting breakdown of the blood–aqueous barrier.Citation85 Peripheral iris stromal and pigment epithelium depigmentation may develop due to ciliary body inflammation, associated with the severe lasting anterior uveitis.Citation86,Citation87 RPE clumping and disruption seen as multiple foci of hypopigmentation, in addition to sunset glow fundus and chorioretinal atrophy, are prominent findings on fundus examination. Though they do not appear to be active chorioretinal inflammation, OCT and ICG studies have demonstrated increased choroidal thickness during this stage, reflecting subclinical inflammation that may require additional immunosuppression.Citation47,Citation48
Imaging in VKHD
Imaging plays a major role in the diagnosis of VKHD, monitoring of the intraocular inflammation and response to treatment, as well as the development of complications.
Fundus fluorescein angiography
FFA is used to aid in the diagnosis, during follow up,Citation88,Citation89 and as a prognostic tool in VKHD.Citation90 (; color retinal photograph showing deep yellow lesions of variable size and multiple SRD). During the early venous phase of FFA, active inflammation in the acute phase leads to delayed choroidal perfusion in the posterior pole and retinal periphery, displayed as areas of hypofluorescent ().Citation91 Numerous hyperfluorescent pinpoint foci of leakage, which coincide with areas of choroiditis, are manifested at the level of RPE ().Citation91 This is accompanied by multilobular dye pooling in the subretinal space, each lobule surrounded by a dark rim () that is thought to be related to the formation of subretinal septa as demonstrated on previously published OCT scans.Citation88,Citation92,Citation93 Homogeneous staining on FFA is usually seen in areas of retinal detachment and optic disc leakage.Citation88,Citation90 A hot disc can be observed in up to 94.4% of patients with acute VKHD and 66.6% of those in the chronic convalescent phase ().Citation88 Numerous hyperfluorescent pinpoint foci of leakage at the level of RPE result in a classic “starry sky” appearance on the FFA that is highly suggestive of VKHD (). Hypofluorescent lines corresponding to choroidal folds are also seen.Citation65,Citation91 In a series of 95 patients with VKHD, 11 (12%) showed choroidal folds manifested as hypofluorescent bands radiating from the optic disc.Citation65 During the chronic phases of VKHD, FFA usually shows RPE window defects, spotted hyper- and hypofluorescence and blockage of choroidal fluorescence due to RPE migration.Citation1,Citation88 Complications such as CNV may also be seen on FFA ().Citation91
Figure 6 Color retinal and FFA photographs of a patient in the acute phase of VKHD showing (A) hyperemic optic disc with deep yellow lesions of variable size and multiple SRD, (B) early FFA showing delayed choroidal filling, (C) mid phase of FFA showing pinpoint hyperfluorescent leakage at the RPE level (D) with pooling of the dye in the subretinal space in the late phase of the angiogram.
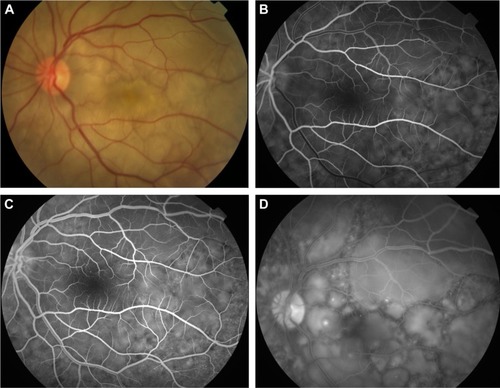
Figure 7 Color retinal photograph of the right eye showing swollen and hyperemic optic discs (A) and FFA showing hot disc (B) (white arrows), in the acute phase of VKHD.
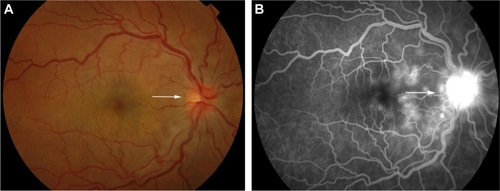
Figure 8 FFA photograph of a patient in the acute phase of VKHD showing optic disc leakage and numerous hyperfluorescent pinpoint foci of leakage at the level of RPE leading to the classic “starry sky” appearance.
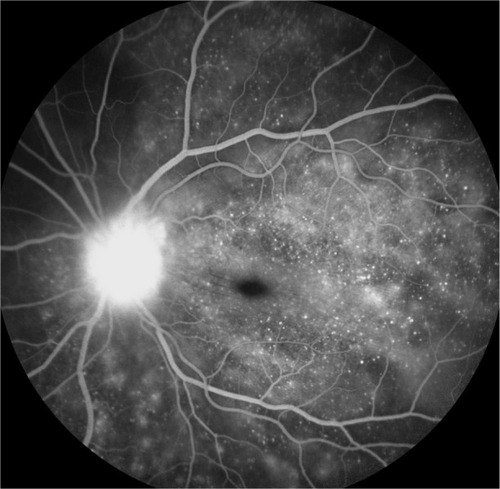
Figure 9 Color retinal (A) and FFA (B) photographs of a VKHD patient with macular CNV (white arrows).
FFA is also found to have a prognostic value in acute VKHD, where the absence of early pinpoint peripapillary hyperfluorescence on pretreatment FFA is a poor prognostic factor for developing chronic VKHD, and its presence is observed in up to 85% of eyes that resolved.Citation90
Indocyanine green angiography
ICG is well established as a sensitive method to delineate the choroidal circulation and visualize the choroid.Citation94 In VKHD, it is used to confirm the presence of choroidal inflammation, monitor choroidal activity and response to therapy.Citation95,Citation96 However, it is an invasive and time-consuming imaging method, in which it is difficult to distinguish stromal scarring rather than active choroiditis,Citation97 and pretreatment ICG findings have been shown to have limited prognostic value for the development of chronic VKHD.Citation90
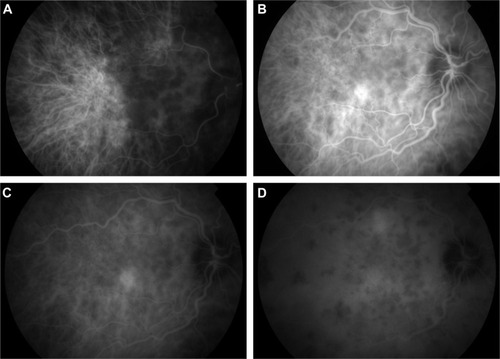
The main ICG features in acute VKHD are: 1) a patchy hypofluorescence pattern at the posterior pole and retinal periphery during the early angiographic phase due to choroidal inflammatory vasculopathy and delayed choroidal perfusion (); 2) large choroidal stromal vessel hyperfluorescence in the early phase (); 3) diffusely leaking fuzzy choroidal vessels possibly due to vasculitis (); 4) hypofluorescent dark dots during the intermediate phase of angiography (), representing partial or full-thickness choroidal scaring and granulomas observed in all eyes in a series of 36 patients with acute VKHD.Citation98 These dark spots are noted to regress with treatment at 2 months follow-upCitation96 and even to completely resolve in some patients;Citation95 5) diffuse choroidal hyperfluorescence in the late phase (22–28 minutes) ().Citation96 Unlike in healthy eyes, where the optic disc remains hypofluorescent, VKHD eyes exhibit optic disc hyperfluorescence indicating severe papillitis and corresponding to the “hot disc” appearance on FFA, which resolves following treatment.Citation95,Citation98 Hypofluorescent patches in areas of exudative retinal detachments have been described during the early phases of the angiogram.Citation98 Choroidal folds are also seen in the late phase of the ICG as long hyperfluorescent lines radiating from the optic disc.Citation91 Patients with chronic VKHD usually display similar but less severe ICG findings to those seen in the acute phase, which are fuzzy vessels, late diffuse choroidal hyperfluorescence, and hypofluorescent lesions corresponding to areas of chorioretinal atrophy.Citation99 Evidence of active ongoing choroidal inflammation can be detected even in the absence of manifest clinical inflammation. Signs of choroidal inflammation were found in ICG scans of 72.5% (31 of 51 eyes) of patients with chronic VKHD, regardless of their clinical appearance and duration of treatment, as clinically active disease was observed in only 41.2% (21 of 51 eyes) of those eyes.Citation99
Figure 10 ICG photographs of the right eye of a patient in the acute phase of VKHD showing (A) patchy hypofluorescence during the early angiographic phase, (B) large choroidal stromal vessel hyperfluorescence with fuzzy choroidal vessels in the early phase, (C) hypofluorescent dark dots during the intermediate phase of angiography, and (D) diffuse choroidal hyperfluorescence in the late phase.
B-scan ultrasonography
Ultrasound (US) is a non-contact diagnostic imaging technique that uses high-frequency acoustic (sound) waves to provide a dynamic view of ocular structures. It has been found to be useful in diagnosing different stages of VKHD, particularly in cases with severe media opacities and a poor fundal view. Diffuse low-to-medium reflective choroidal thickening and SRD are evident during acute VKHD, especially when the SRD is too extensive.Citation89 Swollen ciliary body with shallow anterior chamber, vitreous condensations, and scleral or episcleral thickening have also been seen on US in the acute stage.Citation100–Citation102 Subretinal fibrosis in chronic VKHD was described on US in 64.8% of the eyes with chronic VKHD as dome shaped, heterogeneous lesion; however, no other clinical signs of the chronic disease were detected on the US.Citation103 Therefore, it is relatively unreliable in detecting subclinical recurrences and minor changes in choroidal thickness due to its limited resolution in comparison to OCT.Citation104
Fundus autofluorescence (FAF)
FAF is a noninvasive efficient imaging technique that provides valuable information on the RPE and outer retinal layers.Citation105
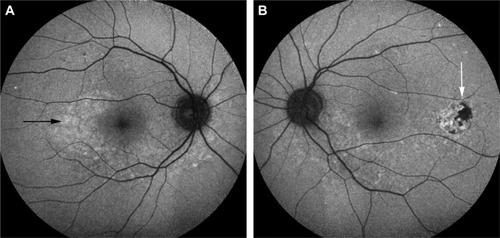
Metabolic and functional activity of the RPE can be detected in different stages of VKHD using the short wavelength light (blue) FAF that has been used to detect lipofuscin abnormalities and the near-infrared light FAF that has been used for melanin and melanin compound abnormalities.Citation106 Different patterns of FAF have been demonstrated in different phases of VKHD, which supports the role of the RPE in the disease and allows repeated close monitoring of disease progression. In the acute phase, FAF demonstrates mild and uniform hyperautofluorescence in the macula and areas of hypoautofluorescence, corresponding to the areas of SRD.Citation106,Citation107 Resolution of the SRD with treatment after 1 month is associated with the appearance of placoid areas of hyperautofluorescence in the macula and peripapillary regions. These FAF changes are more evident on the near-infrared FAF and typically resolve after 6 months of treatment.Citation106 In the chronic phase of VKHD, areas of hypoautofluorescence (), hyperautofluorescence (), and lattice-like pattern in the peripheral fundus are observed.Citation108 Areas of hypoautofluorescence on FAF corresponded with peripapillary atrophy and RPE loss, while increased autofluorescence matches areas of RPE proliferation on SD-OCT in chronic VKHD.Citation109
Figure 11 Short wavelength light (blue) FAF photographs of eyes of a patient with chronic VKHD.
Abbreviations: FAF, fundus autofluorescence; VKHD, Vogt–Koyanagi–Harada disease; RPE, retinal pigment epithelium.
Optical coherence tomography
Recent advances in OCT imaging allows visualization of the choroid and choriocapillaris by providing cross-sectional images of the choroid.Citation110 It is a noninvasive method, which is used to measure choroidal thickness for frequent, quantitative assessment of disease activity and response to treatment in different phases of VKHD. The presence of SRDs is seen on OCT scans as areas of subretinal fluid.Citation92,Citation93 This is usually associated with formation of fibrinous subretinal septa dividing the subretinal space into several compartments.Citation92 Intraretinal edema, RPE undulation, choroidal folds, and choroidal hyperreflective dots can also be seen on the OCT scan in acute VKHD.Citation67,Citation111,Citation112 Following resolution of the inflammation, with corticosteroid treatment, these signs resolve ().Citation113 Damage to the ellipsoid zone, persistent choroidal folds, and RPE undulation have been correlated with poor visual prognosis.Citation69,Citation93,Citation114 OCT can be used to differentiate VKHD from other similar conditions, such as CSCR. In a retrospective study that compared the SD-OCT features of acute VKHD and acute CSCR, SRD was found to be present in both diseases, while RPE folds, fluctuations (rising and falling) of the internal limiting membrane (ILM) and fibrinous subretinal septa were only present in VKHD (). The CSCR cases were found to have significantly more pigment epithelial detachments and bulges of the RPE.Citation115 High-penetration OCT (HP-OCT) using a light source with a long wavelength (1,060 nm) may be superior to SD-OCT in visualizing structures beneath the RPE.Citation116 HP-OCT is used to study 42 eyes of 21 patients with acute VKHD, of whom 24 eyes of 13 patients (57.1%) developed choroidal folds at presentation.Citation69 The presence of these folds significantly correlated with older age, presence of disc swelling, increased choroidal thickness, and the development of sunset glow fundus at 6 months follow-up.Citation69
Figure 12 OCT scan of the macula of a patient in the acute phase of VKHD before and after starting corticosteroid treatment.
Abbreviations: OCT, optical coherence tomography; VKHD, Vogt–Koyanagi–Harada disease; SRD, serous retinal detachment; ILM, internal limiting membrane.
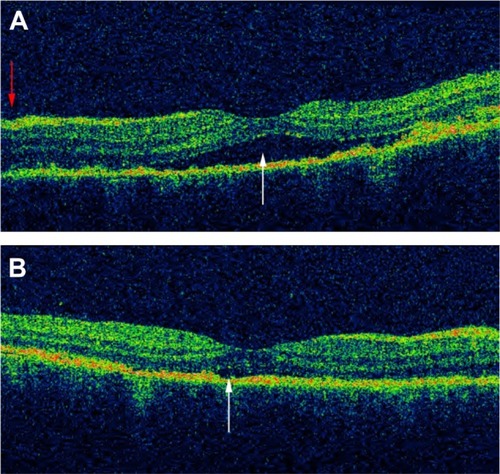
Enhanced depth imaging (EDI)-OCT demonstrates that patients with the acute phase of VKHD have a marked increase in the average subfoveal choroidal thickness, possibly due to inflammatory infiltration and exudation, which reverses following systemic corticosteroid therapy and resolution of the inflammation.Citation104,Citation117 Choroidal thickness continues to be abnormally increased during the chronic recurrent phase.Citation118 An increase in choroidal thickness of >100 μm during corticosteroid tapering, even in the presence of apparently good clinical control, has been defined as rebound choroidal thickening suggesting recurrent subclinical inflammation.Citation117 While this can be accompanied by other ocular signs, such as anterior chamber cells and/or optic disc hyperfluorescence on FFA and/or dark dots on ICG,Citation119 it can also precede them.Citation47 Rebound choroidal thickening on EDI-OCT was the only sign of ocular inflammation in a 71-year-old patient who presented 6 months after his initial diagnosis with headache, tinnitus, and bilateral sensorineural hearing loss.Citation120 Conversely, in chronic VKHD, sunglow fundus correlates with choroidal thinning on EDI-OCT scans.Citation121 The mean subfoveal choroidal thickness is significantly reduced in patients with severe depigmentation of the fundus, in comparison to patients with no-or-mild fundus depigmentation or healthy controls.Citation122 Subfoveal choroidal thinning and focal loss of the choriocapillaris, with preservation of medium (Sattler’s layer) and large choroidal vessels (Haller’s layer), have also been observed on SD-OCT scans of 26 eyes of 13 consecutive patients during the convalescent stage of the disease.Citation80
Ancillary tests
Electroretinography
Full-field electroretinography (ERG), which reflects the total electrophysiological activity of the entire retina, and the multifocal ERG, which represents the simultaneous electrical response of photoreceptors and the inner retina from different regions, are used to evaluate visual function in patients with VKHD.Citation123,Citation124 Extensive chorioretinal atrophy in chronic VKHD is associated with abnormal ERG recordings, possibly due to inflammatory retinal changes. A marked diffuse reduction in the amplitude of both scotopic and photopic phases of full-field ERG is correlated with severe fundus depigmentation and fibrosis in those patients.Citation123 Reduction in multifocal ERG is correlated with reduced vision before treatment in chronic VKHD and shows good recovery with immunosuppressive therapy, reflecting improvement in the visual function.Citation124 Improvement in the N1 and P1 waves of multifocal ERG is observed after treatment in a prospective study that involved 22 eyes with VKHD, which suggests that ERG may be a useful tool to monitor peripheral retinal disease activity and response to treatment.Citation125
Microperimetry
Microperimetry, which determines differential light sensitivity at a certain retinal area, is used to assess the effect of VKHD on the retina and determine response to treatment. It provides a quantitative measurement of the visual function of a specific part of the retina and correlates that to OCT structural changes in that area. In patients with chronic VKHD, macular sensitivity on microperimetry and functional changes (best corrected visual acuity) match RPE thickening and other structural retinal changes on OCT scans. This could help in monitoring disease activity by assessing the visual function in those patients.Citation126 Chronic recurrent disease with sunset glow fundus is associated with worse retinal sensitivity and poor visual outcome.Citation127
Differential diagnosis of VKHD
The differential diagnosis of VKHD includes many other causes of panuveitis and posterior scleritis. Sympathetic ophthalmia (SO) has a similar clinical and histopathological appearance to VKHD, with swollen hyperemic optic discs and SRDs, and is in differential diagnosis of VKHD. However, bilateral granulomatous panuveitis in eyes with SO follow previous penetrating trauma or surgery to one eye.Citation128,Citation129
Posterior scleritis may present with SRD, optic disc swelling and choroidal or retinal folds and may be a presenting feature of VKHD. However, in cases of posterior scleritis, pain is a common feature classically radiating to the forehead or face and waking the patient up during the night. In addition, posterior scleritis is usually unilateral presenting often with reduced vision and ocular pain. Scleral and choroidal thickening, fluid in the Tenon’s capsule, and optic nerve head with the resulting “T sign” appearance are characteristic features on US.Citation70,Citation71,Citation83
CSCR is an idiopathic condition that commonly affects healthy middle-aged men and is characterized by the development of SRDs, and patients may present with headaches that might be mistaken for the prodromal stage of VKHD. However, in CSCR, visual acuity remains good, patients do not complain of ocular pain and there is no evidence of granulomatous ocular inflammation or a hot optic disc on FFA.Citation51,Citation130 Infectious choroiditis caused by syphilis,Citation131 tuberculosis,Citation132 and Bartonella henselae infectionCitation133,Citation134 should also been considered in the differential diagnosis of VKHD. Cat scratch disease caused by B. henselae can present with headache, tinnitus, panuveitis, optic disc swelling, and diffuse choroidal thickening mimicking VKHD. However, in cat scratch disease, the CSF is usually normal with raised antibody titers against B. henselae in the serum.Citation134
Other less frequent causes of panuveitis include intraocular lymphoma that can present with neurological features and/or panuveitis masquerade appearance with thickened choroid and multifocal yellowish subretinal lesions.Citation135 The rare occurrence of idiopathic uveal effusion syndrome is another differential that presents with scleral thickening, subacute onset of exudative detachments of choroid and retina but with no intraocular inflammation.Citation136 Finally, ocular sarcoidosis can present as a granulomatous anterior uveitis or panuveitis with choroidal and optic disc granulomas, segmental phlebitis, and SRDs.Citation137 Pulmonary findings, as well as elevated serum angiotensin-converting enzyme levels, will help differentiate the two conditions.
Treatment
The goal of treatment in VKHD is to suppress active ocular inflammation, prevent disease relapse and avoid sight-threatening complications. As such, early diagnosis and rapid commencement of treatment are important in preserving vision in these young patients. Multiple therapeutic regimens are used combining both systemic immunosuppression agents together with locally administered corticosteroids and anti-vascular endothelial growth factor drugs (anti-VEGF).Citation138–Citation142 Because VKHD can involve multiple organs, the mainstay of treatment is based on high-dose systemic corticosteroids,Citation43 administered either orally or intravenously.Citation143 Oral prednisone at a dose of 1–2 mg/kg/day started early in the course of the disease followed by slow tapering to avoid recurrences is the generally accepted regimen,Citation144,Citation145 while pulse intravenous corticosteroid therapy of 1 g/day of methylprednisolone for 3–5 days followed by oral prednisolone is usually reserved for cases with severe inflammation.Citation43 Slow tapering of the corticosteroid dose, with frequent follow-up examinations, is warranted in order to avoid recurrence of posterior segment inflammation.Citation144 Aiming to reach a dose of <7.5 mg/day over several months and keeping patients on long-term treatment may reduce the risk of relapses, but nonetheless, these occur even when inflammatory control is achieved at high doses.Citation27,Citation44 Treatment at these low, safe doses with no evident ocular inflammation should be maintained for several years before cessation of therapy is considered. Topical corticosteroids and cycloplegic agents are effective in controlling the anterior segment inflammation.Citation34 The addition of second-line immunosuppressive agents including mycophenolate mofetil, methotrexate, cyclosporine, or azathioprine are usually considered in patients who are not controlled with corticosteroids alone or cannot be tapered to a safe low dose for the extended period of time they require to control their inflammation.Citation146–Citation148 Use of these agents has been found to shorten the duration of the acute stage and to reduce the risk of progression to the chronic stages and development of sight-threatening complications.Citation138,Citation149,Citation150 Their addition early in the disease has been found to be associated with a better visual outcome in comparison to corticosteroids alone or if their addition is delayed.Citation138,Citation151
While intravitreal and posterior subtenon triamcinolone acetonide injections have been found to be effective in short-term control of inflammation during the acute phase of VKHD,Citation139,Citation140 intravenous infusion of anti-tumor necrosis factor α agents (adalimumab and infliximab) and rituximab, which is an anti-CD20 monoclonal antibody, has been used in refractory cases and found to be effective in long-term disease control.Citation152–Citation154
Intravitreal injections of anti-VEGF have been used successfully for the treatment of CNVs,Citation155 and combined treatment of triamcinolone acetate and anti-VEGF has also been tried to treat recurrent CNVs.Citation156 Persistent SRDs involving the fovea in four patients with bilateral VKHD were successfully resolved using intravitreal injections of anti-VEGF.Citation142
Complications associated with VKHD
Although the inflammation can be controlled by corticosteroids and other immunosuppressive agents, some patients may still have a poor visual outcome due to development of other sight-threatening complications such as glaucoma, cataract (which can be treated), CNV, and subretinal fibrosis (). These complications tend to occur during the chronic stage of the disease and are associated with a poor visual outcome,Citation1,Citation2 especially if there is delayed presentation.Citation86
Table 1 Complications associated with VKHD
Glaucoma is the most common complication of VKHD with an incidence of up to 45%.Citation157–Citation159 Secondary glaucoma has been attributed to a combination of ciliary body inflammation, pupillary block, formation of anterior synechiae leading to trabecular meshwork obstruction and uveal effusion.Citation159,Citation160 In one study, glaucoma occurred in up to 38% of VKHD patients with the majority requiring surgical intervention to control their IOP.Citation159 A lower incidence of 15.8% has been reported by another group, in whom IOP was controlled mainly by medical treatment. The authors propose that aggressive use of steroid-sparing immunosuppressive agents to control the inflammatory process in their cohort, as well as the effectiveness of the currently available topical anti-glaucoma medication, prevented the need for glaucoma surgery.Citation160
Cataract is the second most common complication of VKHD,Citation157,Citation158,Citation161 with an incidence of up to 42%.Citation2,Citation34 Prolonged steroid treatment and recurrent ocular inflammation are the main risk factors for its development.Citation1,Citation30 Cataract surgery is usually recommended only when the inflammation is quiescent for at least 3 months and should be performed with preoperative steroid cover for up to 2 weeks.Citation162,Citation163 Other less common complications that might be responsible for visual loss in patients with VKHD include peripapillary and macular CNVs,Citation164 which develop in up to 14.7%,Citation165 and subretinal fibrosis.Citation2,Citation30,Citation34 Subretinal fibrosis can occur in up to 40% of VKHD patientsCitation165 and may lead to substantial visual impairment when the fovea is involved.Citation166 Unlike other ocular inflammatory conditions, CME appears to be a relatively rare complication of VKHD.Citation160,Citation167 Other uncommon complications () includes posterior synechiae,Citation158 rhegmatogenous retinal detachment and ERMCitation160 and MH formation,Citation84 band keratopathy,Citation168 and pseudotumoral RPE proliferation.Citation169,Citation170 The high number of complications together with delayed treatment and poor visual acuity at presentation especially in older patients is found to be associated with poor prognosis.Citation2,Citation171
Conclusion
VKHD is a multisystemic autoimmune disease affecting mainly middle-aged patients; it has four distinct phases that may not present in sequential order and detection of subclinical inflammation is still a challenge. Therefore, in order to avoid delayed treatment and development of sight-threatening complications that tend to occur mostly in patients with long-standing ocular inflammation, it is important to recognize the variable clinical presentations of the disease. Utilizing ocular imaging for diagnosis and repeat use of noninvasive modalities, such as OCT to monitor disease activity, can promote early treatment and prevent the development of ocular complications. Early aggressive treatment with systemic corticosteroids during the acute stage is highly recommended. The use of immunosuppressive agents has reduced the risk of developing ocular complications; however, a considerable number of patients still progress to the chronic stages, suffer recurrences and progress to visual loss, probably due to undetectable and undertreated subclinical inflammation. Further prospective studies using sensitive imaging methods are needed to help clarify the role of ongoing choroidal inflammation and RPE activity on the clinical course of the disease and its effect on retinal function and visual outcome.
Disclosure
The authors report no conflicts of interest in this work.
References
- MoorthyRSInomataHRaoNAVogt–Koyanagi–Harada syndromeSurv Ophthalmol19953942652927725227
- ReadRWRechodouniAButaniNComplications and prognostic factors in Vogt–Koyanagi–Harada diseaseAm J Ophthalmol2001131559960611336934
- NoroseKYanoAMelanoma specific Th1 cytotoxic T lymphocyte lines in Vogt–Koyanagi–Harada diseaseBr J Ophthalmol19968011100210088976730
- YamakiKGochoKHayakawaKKondoISakuragiSTyrosinase family proteins are antigens specific to Vogt–Koyanagi–Harada diseaseJ Immunol2000165127323732911120868
- SugitaSTakaseHTaguchiCOcular infiltrating CD4+ T cells from patients with Vogt–Koyanagi–Harada disease recognize human melanocyte antigensInvest Ophthalmol Vis Sci20064762547255416723469
- ShindoYInokoHYamamotoTOhnoSHLA-DRB1 typing of Vogt–Koyanagi–Harada’s disease by PCR-RFLP and the strong association with DRB1*0405 and DRB1*0410Br J Ophthalmol19947832232267908535
- ShiTLvWZhangLChenJChenHAssociation of HLA-DR4/HLA-DRB1*04 with Vogt–Koyanagi–Harada disease: a systematic review and meta-analysisSci Rep20144688725382027
- DamicoFMCunha-NetoEGoldbergACT-cell recognition and cytokine profile induced by melanocyte epitopes in patients with HLA-DRB1*0405-positive and -negative Vogt–Koyanagi–Harada uveitisInvest Ophthalmol Vis Sci20054672465247115980237
- RaoNAPathology of Vogt–Koyanagi–Harada diseaseInt Ophthalmol2007272–3818517435969
- OellersPJaffeGJProiaADClinical-pathological correlation of Vogt–Koyanagi–Harada diseaseJAMA Ophthalmol2016713
- PattisonEMUveomeningoencephalitic syndrome (Vogt–Koyanagi–Harada)Arch Neurol19651219720514237777
- VogtAFrühzeitiges Ergrauen der Zilien und Bemerkungen über den sogenannten plötzlichen Eintritt dieser Veränderung [Early graying of cilia and remarks about the so-called sudden occurrence of these change]Klin Monatsbl Augenheilkd190644228242 German
- KoyanagiYDAlopecia und Poliosis bei schwerer Uveitis nicht traumatischen Ursprungs [Dysacusis, alopecia and poliosis in severe uveitis without traumatic origin]Klin Monatsbl Augenheilkd192982194211 German
- HaradaEClinical study of nonsuppurative choroiditis: a report of acute diffuse choroiditisActa Soc Opthalmol Jpn192630356378
- HerbortCPMochizukiMVogt–Koyanagi–Harada disease: inquiry into the genesis of a disease name in the historical context of Switzerland and JapanInt Ophthalmol2007272–3677917468832
- YangPZhangZZhouHClinical patterns and characteristics of uveitis in a tertiary center for uveitis in ChinaCurr Eye Res2005301194394816282128
- OhguroNSonodaKHTakeuchiMMatsumuraMMochizukiMThe 2009 prospective multi-center epidemiologic survey of uveitis in JapanJpn J Ophthalmol201256543243522752308
- Silpa-ArchaSNoonpradejSAmphornphruetAPattern of uveitis in a referral ophthalmology center in the central district of ThailandOcul Immunol Inflamm201419 Epub 2014 Aug 11
- Al DhahriHAl RubaieKHemachandranSPatterns of uveitis in a University-Based Tertiary Referral Center in Riyadh, Saudi ArabiaOcul Immunol Inflamm201419 Epub 2014 Jul 24
- LibermanPGauroFBergerOUrzuaCACauses of uveitis in a tertiary center in Chile: a cross-sectional retrospective reviewOcul Immunol Inflamm201417 Epub 2014 Dec 1
- NussenblattRBClinical studies of Vogt–Koyanagi–Harada’s disease at the National Eye Institute, NIH, USAJpn J Ophthalmol19883233303333230719
- PerkinsESFolkJUveitis in London and IowaOphthalmologica19841891–236406472804
- SmitRLBaarsmaGSde VriesJClassification of 750 consecutive uveitis patients in the Rotterdam Eye HospitalInt Ophthalmol199317271768407119
- CiminoLAldigeriRSalvaraniCThe causes of uveitis in a referral centre of Northern ItalyInt Ophthalmol201030552152920229320
- Tugal-TutkunIOzyazganYAkovaYAThe spectrum of Vogt–Koyanagi–Harada disease in Turkey: VKH in TurkeyInt Ophthalmol2007272–311712316957877
- CheeSPJapABacsalKSpectrum of Vogt–Koyanagi–Harada disease in SingaporeInt Ophthalmol2007272–313714217103022
- IwahashiCOkunoKHashidaNNakaiKOhguroNNishidaKIncidence and clinical features of recurrent Vogt–Koyanagi–Harada disease in Japanese individualsJpn J Ophthalmol201559315716325808016
- RaoNAGuptaADustinLFrequency of distinguishing clinical features in Vogt–Koyanagi–Harada diseaseOphthalmology20101173591599599.e120036008
- WangYChanCCGender differences in Vogt–Koyanagi–Harada disease and sympathetic ophthalmiaJ Ophthalmol2014201415780324734166
- Abu El-AsrarAMAl-KharashiASAldibhiHAl-FraykhHKangaveDVogt–Koyanagi–Harada disease in childrenEye20082291124113117479116
- MartinTDRathinamSRCunninghamETJrPrevalence, clinical characteristics, and causes of vision loss in children with Vogt–Koyanagi–Harada disease in South IndiaRetina20103071113112120168275
- ForsterDJGreenRLRaoNAUnilateral manifestation of the Vogt–Koyanagi–Harada syndrome in a 7-year-old childAm J Ophthalmol199111133803822000916
- YamamotoYFukushimaANishinoKKouraYKomatsuTUenoHVogt–Koyanagi–Harada disease with onset in elderly patients aged 68 to 89 yearsJpn J Ophthalmol2007511606317295144
- YangPRenYLiBFangWMengQKijlstraAClinical characteristics of Vogt–Koyanagi–Harada syndrome in Chinese patientsOphthalmology2007114360661417123618
- ReadRWHollandGNRaoNARevised diagnostic criteria for Vogt–Koyanagi–Harada disease: report of an international committee on nomenclatureAm J Ophthalmol2001131564765211336942
- RaoNASukavatcharinSTsaiJHVogt–Koyanagi–Harada disease diagnostic criteriaInt Ophthalmol2007272–319519917384920
- MoritaSNakamaruYObaraNMasuyaMFukudaSCharacteristics and prognosis of hearing loss associated with Vogt–Koyanagi–Harada diseaseAudiol Neurootol2014191495624335059
- GaudreauPMoyJLindsayFAn unusual cause of vertigo, tinnitus, and hyperacusis: Vogt–Koyanagi–Harada syndromeEar Nose Throat J20129112E7E9
- SukavatcharinSTsaiJHRaoNAVogt–Koyanagi–Harada disease in Hispanic patientsInt Ophthalmol2007272–314314817380271
- TsaiJHSukavatcharinSRaoNAUtility of lumbar puncture in diagnosis of Vogt–Koyanagi–Harada diseaseInt Ophthalmol2007272–318919417340216
- BenizJForsterDJLeanJSSmithRERaoNAVariations in clinical features of the Vogt–Koyanagi–Harada syndromeRetina19911132752801961985
- HanHJKimHYParkJHLeeEJKim doGShinDIMagnetic resonance imaging of pachymeningeal enhancement in Vogt–Koyanagi–Harada diseaseNeurol Sci201031678578820198496
- RaoNATreatment of Vogt–Koyanagi–Harada disease by corticosteroids and immunosuppressive agentsOcul Immunol Inflamm2006142717216597535
- SakataVMda SilvaFTHirataCEHigh rate of clinical recurrence in patients with Vogt–Koyanagi–Harada disease treated with early high-dose corticosteroidsGraefes Arch Clin Exp Ophthalmol2015253578579025592477
- KeinoHGotoHUsuiMSunset glow fundus in Vogt–Koyanagi–Harada disease with or without chronic ocular inflammationGraefes Arch Clin Exp Ophthalmol20022401087888212397437
- TaylorSLightmanSRecurrent anterior uveitis in patients with Vogt–Koyanagi–Harada syndromeArch Ophthalmol2004122692292315197072
- TagawaYNambaKMizuuchiKChoroidal thickening prior to anterior recurrence in patients with Vogt–Koyanagi–Harada diseaseBr J Ophthalmol2016100447347726261230
- BacsalKWenDSCheeSPConcomitant choroidal inflammation during anterior segment recurrence in Vogt–Koyanagi–Harada diseaseAm J Ophthalmol2008145348048618191100
- TakemotoYNambaKMizuuchiKChoroidal circulation impairment during the anterior recurrence of Vogt–Koyanagi–Harada disease confirmed with indocyanine green angiography and laser speckle flowgraphyActa Ophthalmol2016 Epub 2016 Apr 15
- OkunukiYTsubotaKKezukaTGotoHDifferences in the clinical features of two types of Vogt–Koyanagi–Harada disease: serous retinal detachment and optic disc swellingJpn J Ophthalmol201559210310825465197
- ShinWBKimMKLeeCSLeeSCKimHComparison of the Clinical Manifestations between Acute Vogt–Koyanagi–Harada Disease and Acute Bilateral Central Serous ChorioretinopathyKorean J Ophthalmol201529638939526635455
- RoeRHRathinamSRWongRWMcDonaldHRJumperJMCunninghamETJrDelayed fellow eye involvement in patients with Vogt–Koyanagi–Harada diseaseBr J Ophthalmol200993570170219395635
- NevesACardosoAAlmeidaMCamposJCamposACastro SousaJPUnilateral Vogt–Koyanagi–Harada Disease: a Clinical Case ReportCase Rep Ophthalmol20156336136526600790
- UsuiYGotoHSakaiJTakeuchiMUsuiMRaoNAPresumed Vogt–Koyanagi–Harada disease with unilateral ocular involvement: report of three casesGraefes Arch Clin Exp Ophthalmol200924781127113219308440
- OhnoSMinakawaRMatsudaHClinical studies of Vogt–Koyanagi–Harada’s diseaseJpn J Ophthalmol19883233343433230720
- YangHKParkKHKimJSHwangJMBilateral disc edema in a patient with Vogt–Koyanagi–Harada diseaseCan J Ophthalmol2014492e54e5624767242
- NakaoKAbematsuNMizushimaYSakamotoTOptic disc swelling in Vogt–Koyanagi–Harada diseaseInvest Ophthalmol Vis Sci20125341917192222408010
- AttiaSKhochtaliSKahlounRClinical and multimodal imaging characteristics of acute Vogt–Koyanagi–Harada disease unassociated with clinically evident exudative retinal detachmentInt Ophthalmol2016361374425939987
- RajendramREvansMKhuranaRNTsaiJHRaoNAVogt–Koyanagi–Harada disease presenting as optic neuritisInt Ophthalmol2007272–321722017437062
- NakaoKMizushimaYAbematsuNGohNSakamotoTAnterior ischemic optic neuropathy associated with Vogt–Koyanagi–Harada diseaseGraefes Arch Clin Exp Ophthalmol2009247101417142519568763
- AbematsuNShimonaganoYNakaoKSakamotoTShimizuKHirashimaSA case of anterior ischemic optic neuropathy associated with Vogt–Koyanagi–Harada diseaseNippon Ganka Gakkai Zasshi20061108601606 Japanese16972652
- YokoyamaAOhtaKKojimaHYoshimuraNVogt–Koyanagi–Harada disease masquerading anterior ischaemic optic neuropathyBr J Ophthalmol1999831123
- NarangSSoodSMalikAProbable Vogt–Koyanagi–Harada’s syndrome associated with tonic pupilsNepal J Ophthalmol20102215415621505533
- KatoYYamamotoYTabuchiHFukushimaARetinal pigment epithelium folds as a diagnostic finding of Vogt–Koyanagi–Harada diseaseJpn J Ophthalmol2013571909423149670
- WuWWenFHuangSLuoGWuDChoroidal folds in Vogt–Koyanagi–Harada diseaseAm J Ophthalmol2007143590090117452188
- ZhaoCZhangMWenXDongFHanBDuHChoroidal folds in acute Vogt–Koyanagi–Harada diseaseOcul Immunol Inflamm200917428228819657984
- GuptaVGuptaAGuptaPSharmaASpectral-domain cirrus optical coherence tomography of choroidal striations seen in the acute stage of Vogt–Koyanagi–Harada diseaseAm J Ophthalmol20091471148153.e14218834577
- TanigawaMOchiaiHTsukaharaYOchiaiYYamanakaHChoroidal folds in acute-stage Vogt–Koyanagi–Harada disease patients with relatively short axial lengthCase Rep Ophthalmol201231384522615700
- TsuboiKNakaiKIwahashiCGomiFIkunoYNishidaKAnalysis of choroidal folds in acute Vogt–Koyanagi–Harada disease using high-penetration optical coherence tomographyGraefes Arch Clin Exp Ophthalmol2015253695996425663475
- KoudaNSasakiHHaradaSYamadaYTakahashiNSasakiKEarly manifestation of Vogt–Koyanagi–Harada disease as unilateral posterior scleritisJpn J Ophthalmol200246559059312457922
- WatanabeKKatoTHayasakaSConcurrent bilateral posterior scleritis and Vogt–Koyanagi–Harada disease in a patient with positive rheumatoid factorOphthalmologica199721153163199286810
- RathinamSRNamperumalsamyPNozikRACunninghamETJrAngle closure glaucoma as a presenting sign of Vogt–Koyanagi–Harada syndromeBr J Ophthalmol1997817608609
- YaoJChenYShaoTLingZWangWQianSBilateral acute angle closure glaucoma as a presentation of Vogt–Koyanagi–Harada syndrome in four Chinese patients: a small case seriesOcul Immunol Inflamm201321428629123718571
- YangPLiuXZhouHGuoWZhouCKijlstraAVogt–Koyanagi–Harada disease presenting as acute angle closure glaucoma at onsetClin Experiment Ophthalmol201139763964722452682
- Mili-BoussenILetaiefIDridiHOuertaniABilateral retinal pigment epithelium tears in acute Vogt–Koyanagi–Harada diseaseRetin Cases Brief Rep20137435035425383819
- MizunoMFujinamiKWatanabeKAkiyamaKMacular hole associated with Vogt–Koyanagi–Harada Disease at the Acute Uveitic StageCase Rep Ophthalmol20156332833226483677
- InomataHSakamotoTImmunohistochemical studies of Vogt–Koyanagi–Harada disease with sunset sky fundusCurr Eye Res19909suppl35401974489
- KeinoHGotoHMoriHIwasakiTUsuiMAssociation between severity of inflammation in CNS and development of sunset glow fundus in Vogt–Koyanagi–Harada diseaseAm J Ophthalmol200614161140114216765691
- InomataHRaoNADepigmented atrophic lesions in sunset glow fundi of Vogt–Koyanagi–Harada diseaseAm J Ophthalmol2001131560761411336935
- NazariHHaririAHuZOuyangYSaddaSRaoNAChoroidal atrophy and loss of choriocapillaris in convalescent stage of Vogt–Koyanagi–Harada disease: in vivo documentationJ Ophthalmic Inflamm Infect20144924655594
- HaradaYBhatPMunkMRGoldsteinDAChanges in Scleral Architecture in Chronic Vogt–Koyanagi–Harada diseaseOcul Immunol Inflamm201518 Epub 2015 Dec 8
- MoonSYYoonWTParkSPRecurrent unilateral Vogt–Koyanagi–Harada disease with posterior scleritisKorean J Ophthalmol2015295352354
- SambhavKMajumderPDBiswasJNecrotizing scleritis in a case of Vogt–Koyanagi–Harada diseaseOman J Ophthalmol20158321626903739
- KobayashiIInoueMOkadaAAKeinoHWakabayashiTHirakataAVitreous surgery for macular hole in patients with Vogt–Koyanagi–Harada diseaseClin Experiment Ophthalmol200836986186419278482
- FangWZhouHYangPHuangXWangLKijlstraALongitudinal quantification of aqueous flare and cells in Vogt–Koyanagi–Harada diseaseBr J Ophthalmol200892218218517965105
- AttiaSZaoualiSBettaiebAYahiaSBKhairallahMPeripheral iris depigmentation and ocular hypotony: result of the natural course of non-treated Vogt–Koyanagi–Harada (VKH) diseaseInt Ophthalmol2007272–322122217318319
- SuhlerEBBuggageRRNussenblattRBNeumannRSymmetric peripheral iris depigmentation in Vogt–Koyanagi–Harada syndromeArch Ophthalmol200212081104110512149073
- Arellanes-GarciaLHernandez-BarriosMFromow-GuerraJCervantes-FanningPFluorescein fundus angiographic findings in Vogt–Koyanagi–Harada syndromeInt Ophthalmol2007272–315516117253110
- JapACheeSPImaging in the diagnosis and management of Vogt–Koyanagi–Harada diseaseInt Ophthalmol Clin201252416317222954938
- CheeSPJapACheungCMThe prognostic value of angiography in Vogt–Koyanagi–Harada diseaseAm J Ophthalmol2010150688889320933219
- FardeauCTranTHGharbiBCassouxNBodaghiBLeHoangPRetinal fluorescein and indocyanine green angiography and optical coherence tomography in successive stages of Vogt–Koyanagi–Harada diseaseInt Ophthalmol2007272–316317217273903
- YamaguchiYOtaniTKishiSTomographic features of serous retinal detachment with multilobular dye pooling in acute Vogt–Koyanagi–Harada diseaseAm J Ophthalmol2007144226026517533104
- IshiharaKHangaiMKitaMYoshimuraNAcute Vogt–Koyanagi–Harada disease in enhanced spectral-domain optical coherence tomographyOphthalmology200911691799180719643489
- YannuzziLASlakterJSSorensonJAGuyerDROrlockDADigital indocyanine green videoangiography and choroidal neovascularization. 1992Retina201232suppl 1191
- HerbortCPMantovaniABouchenakiNIndocyanine green angiography in Vogt–Koyanagi–Harada disease: angiographic signs and utility in patient follow-upInt Ophthalmol2007272–317318217457515
- BouchenakiNHerbortCPThe contribution of indocyanine green angiography to the appraisal and management of Vogt–Koyanagi–Harada diseaseOphthalmology20011081546411150265
- KnechtPBMantovaniAHerbortCPIndocyanine green angiography-guided management of Vogt–Koyanagi–Harada disease: differentiation between choroidal scars and active lesionsInt Ophthalmol201333557157723277207
- AbouammohMAGuptaVHemachandranSHerbortCPAbu El-AsrarAMIndocyanine green angiographic findings in initial-onset acute Vogt–Koyanagi–Harada diseaseActa Ophthalmol201694657357826823203
- da SilvaFTHirataCESakataVMIndocyanine green angiography findings in patients with long-standing Vogt–Koyanagi–Harada disease: a cross-sectional studyBMC Ophthalmol2012124022889440
- ForsterDJCanoMRGreenRLRaoNAEchographic features of the Vogt–Koyanagi–Harada syndromeArch Ophthalmol199010810142114262222275
- KishiANao-iNSawadaAUltrasound biomicroscopic findings of acute angle-closure glaucoma in Vogt–Koyanagi–Harada syndromeAm J Ophthalmol199612257357378909219
- WadaSKohnoTYanagiharaNUltrasound biomicroscopic study of ciliary body changes in the post-treatment phase of Vogt–Koyanagi–Harada diseaseBr J Ophthalmol200286121374137912446369
- Mayorquín-RuizMCheja-KalbRConcha-del RíoLArellanes-GarcíaLMoragrega-AdameEEchographic findings in the late stages of Vogt–Koyanagi–Harada disease in Mexican populationRev Bras Oftalmol2014736348350
- MarukoIIidaTSuganoYSubfoveal choroidal thickness after treatment of Vogt–Koyanagi–Harada diseaseRetina201131351051720948460
- Schmitz-ValckenbergSHolzFGBirdACSpaideRFFundus auto-fluorescence imaging: review and perspectivesRetina200828338540918327131
- KoizumiHMaruyamaKKinoshitaSBlue light and near-infrared fundus autofluorescence in acute Vogt–Koyanagi–Harada diseaseBr J Ophthalmol201094111499150519965835
- AyataADogruSSenolMGUnalMErsanliDBilgeAHAuto-fluorescence findings in Vogt–Koyanagi–Harada diseaseEur J Ophthalmol20091961094109719882556
- HeussenFMVasconcelos-SantosDVPappuruRRWalshACRaoNASaddaSRUltra-wide-field green-light (532-nm) autofluorescence imaging in chronic Vogt–Koyanagi–Harada diseaseOphthalmic Surg Lasers Imaging201142427227721553702
- Vasconcelos-SantosDVSohnEHSaddaSRaoNARetinal pigment epithelial changes in chronic Vogt–Koyanagi–Harada disease: fundus autofluorescence and spectral domain-optical coherence tomography findingsRetina2010301334120010321
- MrejenSSpaideRFOptical coherence tomography: imaging of the choroid and beyondSurv Ophthalmol201358538742923916620
- FongAHLiKKWongDChoroidal evaluation using enhanced depth imaging spectral-domain optical coherence tomography in Vogt-Koyanagi-Harada diseaseRetina201131350250921336069
- ZhaoCZhangMFDongFTSpectral domain optical coherence tomography of Vogt–Koyanagi–Harada disease: novel findings and new insights into the pathogenesisChin Med Sci J2012271293422734211
- YamanakaEOhguroNYamamotoSNakagawaYImotoYTanoYEvaluation of pulse corticosteroid therapy for Vogt–Koyanagi–Harada disease assessed by optical coherence tomographyAm J Ophthalmol2002134345445612208266
- HosodaYUjiAHangaiMMorookaSNishijimaKYoshimuraNRelationship between retinal lesions and inward choroidal bulging in Vogt–Koyanagi–Harada diseaseAm J Ophthalmol201415751056106324491415
- LinDChenWZhangGComparison of the optical coherence tomographic characters between acute Vogt–Koyanagi–Harada disease and acute central serous chorioretinopathyBMC Ophthalmol2014148724974016
- NakaiKGomiFIkunoYChoroidal observations in Vogt–Koyanagi–Harada disease using high-penetration optical coherence tomographyGraefes Arch Clin Exp Ophthalmol201225071089109522240936
- NakayamaMKeinoHOkadaAAEnhanced depth imaging optical coherence tomography of the choroid in Vogt–Koyanagi–Harada diseaseRetina201232102061206923095726
- HashizumeKImamuraYFujiwaraTMachidaSIshidaMKurosakaDChoroidal thickness in eyes with posterior recurrence of Vogt–Koyanagi–Harada disease after high-dose steroid therapyActa Ophthalmol2014926e490e49124588838
- SakataVMda SilvaFTHirataCETakahashiWYCostaRAYamamotoJHChoroidal bulging in patients with Vogt–Koyanagi–Harada disease in the non-acute uveitic stageJ Ophthalmic Inflamm Infect201441624548697
- IshibazawaAKinouchiRMinamiYKatadaAYoshidaARecurrent Vogt–Koyanagi–Harada disease with sensorineural hearing loss and choroidal thickeningInt Ophthalmol201434367968424022645
- da SilvaFTSakataVMNakashimaAEnhanced depth imaging optical coherence tomography in long-standing Vogt–Koyanagi–Harada diseaseBr J Ophthalmol2013971707423099292
- TakahashiHTakaseHIshizukaAChoroidal thickness in convalescent Vogt–Koyanagi–Harada diseaseRetina201434477578023979311
- da SilvaFTHirataCEOlivalvesEOyamadaMKYamamotoJHFundus-based and electroretinographic strategies for stratification of late-stage Vogt–Koyanagi–Harada disease patientsAm J Ophthalmol20091486939945.e93319781687
- CheeSPLuuCDChengCLLimWKJapAVisual function in Vogt–Koyanagi–Harada patientsGraefes Arch Clin Exp Ophthalmol2005243878579015761760
- YangPFangWWangLWenFWuWKijlstraAStudy of macular function by multifocal electroretinography in patients with Vogt–Koyanagi–Harada syndromeAm J Ophthalmol2008146576777118672226
- ZhouMJiangCGuRSunZHuynhNChangQCorrelation between retinal changes and visual function in late-stage Vogt–Koyanagi–Harada disease: an Optical Coherence Tomography StudyJ Ophthalmol2015201591648526301103
- AbuEl-AsrarAMMudhaiyanTAAlNajashiAAChronic recurrent Vogt–Koyanagi–Harada disease and development of ‘sunset glow fundus’ predict worse retinal sensitivityOcul Immunol Inflamm2016111 Epub 2016 Mar 22
- GotoHRaoNASympathetic ophthalmia and Vogt–Koyanagi–Harada syndromeInt Ophthalmol Clin19903042792852228475
- RaoNAMarakGESympathetic ophthalmia simulating Vogt–Koyanagi–Harada’s disease: a clinico-pathologic study of four casesJpn J Ophthalmol19832735065116656012
- KomukuYIwahashiCYanoSTanakaCNakagawaTGomiFEn face optical coherence tomography imaging of the choroid in a case with central serous chorioretinopathy during the course of Vogt–Koyanagi–Harada Disease: a case reportCase Rep Ophthalmol20156348849426955354
- KimLAKhuranaRNParikhJGRaoNAMelanin-laden macrophages in the CSF to diagnose Vogt–Koyanagi–Harada simulating ocular syphilisOcul Immunol Inflamm2008161596118379946
- GuptaVGuptaARaoNAIntraocular tuberculosis – an updateSurv Ophthalmol200752656158718029267
- JaumouilleSMortemousqueBNeurorétinite avec oedème maculaire stellaire et oedème papillaire : infection à Bartonella henselae (maladie des griffes du chat) [Neuroretinitis with stellate macular edema and papilledema: Bartonella henselae infection (cat-scratch disease)]Journal francais d’ophtalmologie2016391127128 French
- KhuranaRNAlbiniTGreenRLRaoNALimJIBartonella henselae infection presenting as a unilateral panuveitis simulating Vogt–Koyanagi–Harada syndromeAm J Ophthalmol200413861063106515629311
- SagooMSMehtaHSwampillaiAJPrimary intraocular lymphomaSurv Ophthalmol201459550351624560125
- ElagouzMStanescu-SegallDJacksonTLUveal effusion syndromeSurv Ophthalmol201055213414520159229
- HerbortCPRaoNAMochizukiMMembers of Scientific Committee of First International Workshop on Ocular SInternational criteria for the diagnosis of ocular sarcoidosis: results of the first International Workshop on Ocular Sarcoidosis (IWOS)Ocul Immunol Inflamm200917316016919585358
- ParedesIAhmedMFosterCSImmunomodulatory therapy for Vogt–Koyanagi–Harada patients as first-line therapyOcul Immunol Inflamm2006142879016597537
- AndradeREMuccioliCFarahMENussenblattRBBelfortRJrIntravitreal triamcinolone in the treatment of serous retinal detachment in Vogt–Koyanagi–Harada syndromeAm J Ophthalmol2004137357257415013890
- HosodaYHayashiHKuriyamaSPosterior subtenon triamcinolone acetonide injection as a primary treatment in eyes with acute Vogt–Koyanagi–Harada diseaseBr J Ophthalmol20159991211121425792626
- LatronicoMERiganteDCasoFBilateral dexamethasone intravitreal implant in a young patient with Vogt–Koyanagi–Harada disease and refractory uveitisClin Rheumatol20153461145114824763751
- ReibaldiMRussoAAvitabileTTreatment of persistent serous retinal detachment in Vogt–Koyanagi–Harada syndrome with intravitreal bevacizumab during the systemic steroid treatmentRetina201434349049623903795
- ReadRWYuFAccorintiMEvaluation of the effect on outcomes of the route of administration of corticosteroids in acute Vogt–Koyanagi–Harada diseaseAm J Ophthalmol2006142111912416815259
- LaiTYChanRPChanCKLamDSEffects of the duration of initial oral corticosteroid treatment on the recurrence of inflammation in Vogt–Koyanagi–Harada diseaseEye200923354354818369377
- ErreraMHFardeauCCohenDEffect of the duration of immunomodulatory therapy on the clinical features of recurrent episodes in Vogt–Koyanagi–Harada diseaseActa Ophthalmol2011894e357e36621251241
- JabsDANussenblattRBRosenbaumJTStandardization of Uveitis Nomenclature Working GStandardization of uveitis nomenclature for reporting clinical data. Results of the First International WorkshopAm J Ophthalmol2005140350951616196117
- Tomkins-NetzerOTalatLBarALong-term clinical outcome and causes of vision loss in patients with uveitisOphthalmology2014121122387239225178807
- Tomkins-NetzerOTalatLIsmetovaFSamyALightmanSImmunomodulatory therapy in uveitisDev Ophthalmol20165526527526501368
- Abu El-AsrarAMAl TamimiMHemachandranSAl-MezaineHSAl-MuammarAKangaveDPrognostic factors for clinical outcomes in patients with Vogt–Koyanagi–Harada disease treated with high-dose corticosteroidsActa Ophthalmol2013916e486e49323575246
- Abu El-AsrarAMHemachandranSAl-MezaineHSKangaveDAl-MuammarAMThe outcomes of mycophenolate mofetil therapy combined with systemic corticosteroids in acute uveitis associated with Vogt–Koyanagi–Harada diseaseActa Ophthalmol2012908e603e60822971163
- UrzuaCAVelasquezVSabatPEarlier immunomodulatory treatment is associated with better visual outcomes in a subset of patients with Vogt–Koyanagi–Harada diseaseActa Ophthalmol2015936e475e48025565265
- JeroudiAAngeles-HanSTYehSEfficacy of adalimumab for pediatric Vogt–Koyanagi–Harada syndromeOphthalmic Surg Lasers Imaging Retina201445433233425037015
- ZmudaMTievKPKnoeriJHéronESuccessful use of infliximab therapy in sight-threatening corticosteroid-resistant Vogt–Koyanagi–Harada diseaseOcul Immunol Inflamm201321431031623617262
- Dolz-MarcoRGallego-PinazoRDiaz-LlopisMRituximab in refractory Vogt–Koyanagi–Harada diseaseJ Ophthalmic Inflamm Infect20111417718021744181
- WuLEvansTSaraviaMSchlaenACoutoCIntravitreal bevacizumab for choroidal neovascularization secondary to Vogt–Koyanagi–Harada syndromeJpn J Ophthalmol2009531576019184312
- PaiSAHebriSPLootahAMManagement of recurrent inflammatory choroidal neovascular membrane secondary to Vogt–Koyanagi–Harada syndrome, using combined intravitreal injection of bevacizumab and triamcinolone acetateIndian J Ophthalmol201260655155223202396
- RubsamenPEGassJDVogt–Koyanagi–Harada syndrome. Clinical course, therapy, and long-term visual outcomeArch Ophthalmol199110956826872025171
- ArevaloJFLasaveAFGuptaVClinical outcomes of patients with Vogt–Koyanagi–Harada disease over 12 years at a tertiary centerOcul Immunol Inflamm20152319
- ForsterDJRaoNAHillRANguyenQHBaerveldtGIncidence and management of glaucoma in Vogt–Koyanagi–Harada syndromeOphthalmology199310056136188098519
- PandeyABalekudaruSVenkatramaniDVGeorgeAELingamVBiswasJIncidence and management of glaucoma in Vogt Koyanagi Harada diseaseJ Glaucoma201625867468026967258
- BykhovskayaIThorneJEKempenJHDunnJPJabsDAVogt–Koyanagi–Harada disease: clinical outcomesAm J Ophthalmol2005140467467816226518
- MeacockWRSpaltonDJBenderLSteroid prophylaxis in eyes with uveitis undergoing phacoemulsificationBr J Ophthalmol20048891122112415317700
- QuekDTJapACheeSPRisk factors for poor visual outcome following cataract surgery in Vogt–Koyanagi–Harada diseaseBr J Ophthalmol201195111542154621349937
- MoorthyRSChongLPSmithRERaoNASubretinal neovascular membranes in Vogt–Koyanagi–Harada syndromeAm J Ophthalmol199311621641708352300
- LertsumitkulSWhitcupSMNussenblattRBChanCCSubretinal fibrosis and choroidal neovascularization in Vogt–Koyanagi–Harada syndromeGraefes Arch Clin Exp Ophthalmol1999237121039104510654175
- KuoICRechdouniARaoNAJohnstonRHMargolisTPCunninghamETJrSubretinal fibrosis in patients with Vogt–Koyanagi–Harada diseaseOphthalmology200010791721172810964836
- RutzenAROrtega-LarroceaGFrambachDARaoNAMacular edema in chronic Vogt–Koyanagi–Harada syndromeRetina19951564754798747440
- YangPSunMBand-shaped keratopathy in Chinese patients with Vogt–Koyanagi–Harada syndromeCornea201130121336134021934492
- KhairallahMRaoNABen YahiaSZaoualiSAttiaSPseudotumoral retinal pigment epithelium proliferation in a patient with Vogt–Koyanagi–Harada diseaseArch Ophthalmol200612491366136716966643
- YepezJBMuratiFPetittoMArevaloJFPseudotumoral and multiple retinal pigment epithelium proliferation in Vogt–Koyanagi–Harada diseaseCase Rep Ophthalmol Med2015201515383126509089
- CheeSPJapABacsalKPrognostic factors of Vogt–Koyanagi–Harada disease in SingaporeAm J Ophthalmol20091471154161.e15118834575