Abstract
COVID-19 is a viral illness that can cause severe respiratory symptoms. COVID-19 has caused a worldwide pandemic that necessitated many countries to perform a national lockdown. In Jordan, a lockdown was imposed by the government. During the lockdown, the hospitals were only dealing with outpatient emergency cases, urgent referrals from primary or secondary health institutions, and inpatients whose medical conditions required keeping them admitted. Elective clinics and surgeries were canceled. At the King Abdullah University Hospital (KAUH), which is the only tertiary center in northern Jordan, we dealt with an unusual case of uncontrolled and advanced primary open angle glaucoma in a 38-year-old pregnant female patient. The patient was presented with an intraocular pressure (IOP) of 53 mmHg in the right eye and 40 mmHg in the left eye despite using dorzolamide and timolol eye drops twice daily. The angle was opened in gonioscopy. The decision was made to implant Ahmed glaucoma valves (AGV) in each eye in one session under general anesthesia which was performed successfully. At the last follow-up visit 4 years later, the IOP was maintained at 15 mmHg.
Novel coronavirus (COVID-19) is a new infectious disease that has caused a global pandemic. Due to the fast transmissibility of the disease from the infected person to others,Citation1 and the emergence of clusters and outbreaks between individuals,Citation2 many governments around the world-imposed lockdowns and/or social distancing in public areas.Citation3 Jordan was not an exception; a strict lockdown was imposed by the Jordanian government between March 18, 2020, and May 31, 2020, and between November 3, 2020, and January 3, 2021. Although the government loosened the lockdown at different intervals to allow people to get their important needs, most sectors were completely closed. Hospitals were allowed only to deal with emergency cases and urgent referrals from other health-care centers. King Abdullah University Hospital (KAUH) was assigned by the government to accommodate COVID-19 cases and other emergency cases. All elective clinic, procedure, and surgical appointments were canceled.
A 38-year-old-pregnant woman at 35 weeks of gestation presented to the emergency department during the second period of lockdown complaining of frontal headache and progressive decrease in the visual acuity in both eyes with more severe loss in the right eye. She was known to have primary open angle glaucoma, and she was on dorzolamide and timolol eye drops twice daily. Before pregnancy, she was on dorzolamide, timolol, and brimonidine twice a day, and latanoprost at bedtime. Upon examination, the best corrected visual acuity was 6/120 in the right eye and 6/9 in the left eye and was measured by Snellen chart. The intraocular pressure (IOP) was 53 mmHg in the right eye and 40 mmHg in the left eye and was measured by Goldmann applanation tonometry. The cornea was clear in both eyes, the anterior chamber was deep and quiet in both eyes, and the lens was clear in both eyes. The cup to disc ratio was around 0.9 in the right eye and 0.8 in the left one. The retina was flat in both eyes. Volk 4-mirrors gonio-lens showed wide pigmented angles in both eyes. The visual field was not performed preoperatively as the patient was presented urgently for the operating room while the outpatient clinics were closed due to COVID-19. The patient tested negative for COVID-19.
The diagnosis of primary open angle glaucoma (POAG) was established. According to the situation of advanced glaucomatous damage, pregnancy status, and COVID-19 lockdown difficulties, the decision of Ahmed glaucoma valve (AGV) implantation in one session under general anesthesia was reached. Before the surgery, IOP-lowering eye drops were given in cycles in order to decrease the IOP before the operation. The operation was performed under sterile conditions (). A partial thickness 6/0 traction suture was inserted in the peripheral cornea superiorly and the eye pulled inferio-nasally to expose the superior-temporal quadrant of the conjunctiva. Periotomy was done superior-temporally using Westcott scissors. Two conjunctival relaxing incisions of about 10 mm each were performed at the two ends of the periotomy. Blunt dissection of the conjunctiva and tenon’s capsule was performed of about 15–20 mm superior-temporally, and the sub-tenon’s space was checked to ensure there was enough space for the AGV plate. The model of AGV was FP7 (New World Medical, Rancho Cucamonga, CA, USA). The AGV was then opened and put in the field, and priming to separate the valve leaflets was performed; this was accomplished by injecting a balanced salt solution through the device tube until a jet of fluid existed from the valve outlet.
Figure 1 The steps in AGV surgery. (a) Tractional suture with conjunctival dissection. (b) Priming of the AGV. (c) Implantation and suturing of the plate. (d) Pericardial patch covering. (e) The tube in the anterior chamber.
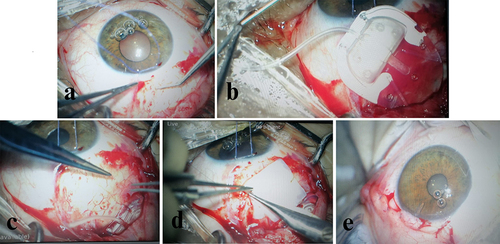
The plate was sutured to the sclera in the superior-temporal quadrant approximately 10 mm posterior to the limbus using 10/0 nylon sutures. Paracentesis was done using an MVR blade, and viscoelastic material was injected in the anterior chamber. The tube of the AGV was cut to the appropriate length with the bevel up, and a 23-gauge needle was used to make a tunnel starting 2 mm posterior to the limbus to the anterior chamber, with a careful insertion through the angle and parallel to the iris plane to ensure a good positioning of tube. The tube was then inserted through the tunnel and its position and length was carefully checked. Three 10/0 nylon sutures were used to stabilize the tube over the sclera. A pericardium patch (New World Medical, CA, USA) was cut to the appropriate size and used to cover the tube and sutured to the sclera using 10/0 nylon sutures. The conjunctiva was then hydrated and pulled carefully to the limbus, it was sutured to the limbus using interrupted 8/0 vicryl sutures, and the conjunctival relaxing incisions were sutured using continuous 8/0 vicryl sutures. The paracentesis was closed using stromal hydration with balanced salt solution. No antimetabolites were utilized. On the next day, the IOP was 10 mmHg in the right eye and 8 mmHg in the left eye. The patient was discharged on prednisolone acetate and moxifloxacin eye drops. The patient presented three months postoperatively after an uneventful 39-week pregnancy (gestational age at delivery was 39 weeks). The IOP was 22 mmHg in both eyes with Tenon’s cyst which suggests early encapsulation. The visual acuity was the same and stable preoperatively and postoperatively. She commenced on timolol and dorzolamide eye drops twice a day. One week later, the IOP was maintained at 12 mmHg in the right eye and 10 mmHg in the left one with the use of timolol and dorzolamide eye drops. At the last follow-up visit 4 years later, the visual acuity was 6/120 in the right eye and 6/9 in the left eye. The IOP was 15 mmHg in both eyes and maintained on a combination of timolol and dorzolamide eye drops twice a day. The cup to disc ratio was 0.9 in the right eye and 0.8 in the left eye. The valve plates were mildly encysted with tip of the valves located in the anterior chamber.
The COVID-19 pandemic represented a challenge to the health systems in most countries. Hospitals were overwhelmed with COVID-19 cases and patients’ accessibility to regular health services was limited. This limitation has negatively affected many patients with chronic health issues including those with chronic eye diseases.
KAUH is the only tertiary center in the north of Jordan and is one of the two university hospitals in the whole country. It was one of the hospitals designated by the Jordanian government to receive and manage COVID-19 cases. All elective clinic, procedure, and surgical appointments were canceled. Ophthalmology clinics were open only for emergency cases.Citation4 Patients with eye complaints were able to get in touch with the on-call ophthalmologists who used their judgment to determine the urgency of the problem and to decide whether the patient needed to come to the ophthalmology emergency room. Since the ocular surface has been shown to be a possible route for COVID-19 transmission,Citation5,Citation6 ophthalmologists were instructed to follow clinical guidelines to face the pandemic and protect themselves and their patients from COVID-19 infection. These guidelines were based on recommendations from the American Academy of Ophthalmology (AAO)Citation7 and the International Council of Ophthalmology (ICO),Citation8 and on different published papers that discussed protocols and effective measures to prevent COVID-19 transmission.Citation9–11 These recommendations included the use of protective goggles, face shields, slit lamp breath shields, disposable gloves, thorough hand washing with soap and water, and disinfection of examination rooms and slit lamps after each examination. In addition, general protective measures were strictly implemented inside the hospital such as the use of a face mask, social distancing, and body temperature measurement for every single patient.
Glaucoma is a chronic eye disease that requires regular follow-up in ophthalmology clinics, and it was part of the chronic eye diseases that were negatively impacted by the COVID-19 pandemic.Citation12 This was due to the limited access to the health care facilities during the pandemic-associated lockdowns, and due to patients’ preference to stay home because of their intrinsic fears to visit clinics and hospitals during the pandemic to avoid contacting people infected with COVID-19. Besides the COVID-19 lockdown, pregnancy represented another challenge in our patient.
The safety of different groups of anti-glaucoma eye drops in pregnancy has been studied before, and all groups of anti-glaucoma drops were put in category C except alpha agonists which were put in category B based on the FDA classification of the drugs’ safety during pregnancy.Citation13 So, no topical antiglaucoma agents have strong evidence of safety to the fetus based on the human studies.Citation14,Citation15 In addition, there is theoretical evidence of an increase in uterine tone with the use of prostaglandin which can limit its use in the third trimester to avoid the possible risk of premature delivery. However, it was found the dosage used to stimulate abortion is 400 cm3 of the ocular formulation of the latanoprost.Citation16 The relatively negligible small dose of the eye drops to the human body could have negligible effect on the fetus. However, it is recommended to council pregnant women about the importance of nasolacrimal occlusion, eyelid closure, or blotting the excess drops away during drops administration, and punctual plugging on using topical antiglaucoma medications.Citation17 This can significantly decrease the systemic absorption of these medications.
In general, there is a general level of uncertainty among ophthalmologists regarding the use of different antiglaucoma medications in pregnant women.Citation18 This could explain why our patient was only on two antiglaucoma eye drops despite her advanced glaucoma status. It is important to notify that most pregnant women with glaucoma generally remain stable during pregnancy although a small percentage (about 10%) have increased IOP or progression of the disease.Citation19 A retrospective case series from Harvard Medical School reviewed pregnant women with pre-existing glaucoma and reported that 57% eyes had stable IOPs and visual fields during pregnancy, 18% eyes had increased IOP despite stable visual fields, and 18% of eyes experienced progressive visual field loss with stable or elevated IOPs.Citation20
There are specific risks and considerations of glaucoma surgery in pregnant patients, including timing of surgery, position of the patient during surgery, risks of local and general anesthesia, and intraoperative and postoperative medications.Citation21 Although trabeculectomy is the classical primary surgery for virgin eyes with POAG, and tube implants have historically been reserved for refractory glaucoma at high risk of failure with standard filtering surgery, the decision was based on the fact that postoperative interventions and surgical complications that require frequent follow-up visits after trabeculectomy are more common than after AGV implant.Citation21 In addition, trabeculectomy may be at relatively higher risk of failure because of young age, physiological changes during pregnancy, and contraindicated antimetabolite usage which is considered as group X.Citation22 Razeghinejad et al described a case series for three pregnant women who underwent surgical procedures for glaucoma. The first case described underwent trabeculectomy without antimetabolites in both eyes because of uncontrolled intraocular pressure during the second and third trimesters. The second patient had an Ahmed valve implantation in both eyes during the second and third trimesters because of uncontrolled IOP with topical medications and no response to selective laser trabeculoplasty. The third case had a Baerveldt valve implantation under general anesthesia in the second trimester.Citation22
This advanced glaucoma status, high IOP, pregnancy situation, and COVID-19 lockdown necessitated urgent surgical intervention for both eyes. Although we rarely perform bilateral glaucoma surgery in one session, a decision was made to perform bilateral glaucoma surgery under general anesthesia in one session.
In conclusion, although trabeculectomy is the classical primary surgery for virgin eyes with POAG, and tube implants have historically been reserved for refractory glaucoma at high risk of failure with standard filtering surgery, the decision was based on the fact that postoperative interventions and surgical complications that require frequent follow-up visits after trabeculectomy are more common than after AGV implant. This case represents the challenge of deciding AGV implantation to be operated in pregnant women when the situation necessitates minimal follow visits in a period of very restrictive lockdown.
Data Sharing Statement
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.
Ethics Approval
The Institutional Review Board approval is not required.
Consent for Publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Disclosure
The authors declare that they have no competing interests.
Additional information
Funding
References
- European Centre for Disease Prevention and Control (ECDC). Transmission of COVID-19. Available from: https://www.ecdc.europa.eu/en/infectious-disease-topics/z-disease-list/covid-19/facts/transmission-covid-19. Accessed September 22, 2020.
- Desjardins MR, Hohl A, Delmelle EM. Rapid surveillance of COVID-19 in the United States using a prospective space-time scan statistic: detecting and evaluating emerging clusters. Appl Geogr. 2020;118:102202. doi:10.1016/j.apgeog.2020.102202
- Wilder-Smith A, Bar-Yam Y, Fisher D. Lockdown to contain COVID-19 is a window of opportunity to prevent the second wave. J Travel Med. 2020;27(5):taaa091. doi:10.1093/jtm/taaa091
- Al-Dwairi R, Rwashdeh H, Otoom M. The influence of COVID-19 lockdown in Jordan on patients with diabetic retinopathy: a Case-Control Study. Ther Clin Risk Manag. 2021;17:1011–1022. doi:10.2147/TCRM.S316265
- Napoli PE, Nioi M, d’Aloja E, Fossarello M. The ocular surface and the Coronavirus disease 2019: does a dual ‘Ocular route’ exist? J Clin Med. 2020;9(5):1269. doi:10.3390/jcm9051269
- Wang YH, Zhao LM, Liu ZY, Li XM. Perioperative management by WeChat under the haze of COVID-19. Int J Ophthalmol. 2020;13(7):1161–1163. doi:10.18240/ijo.2020.07.22
- American Academy of Ophthalmology. Important coronavirus updates for ophthalmologists. Available from: https://www.aao.org/headline/alert-important-coronavirus-context.37. Accessed September 22, 2020.
- International Council of Ophthalmology. ICO global COVID-19 resource center. Available from: http://www.icoph.org/news/news_detail/602/ICO-Global-COVID-19-Resource-Center.html. Accessed September 22, 2020.
- Pei X, Jiao X, Lu D, Qi D, Huang S, Li Z. How to face COVID-19 in ophthalmology practice. Med Hypothesis Discov Innov Ophthalmol. 2020;9(3):164–171. doi:10.51329/mehdiophthal1406
- Reda AM, Ahmed WM. Standard precaution measurements during ophthalmology practice in the pandemic stage of COVID-19. Int J Ophthalmol. 2020;13(7):1017–1022. doi:10.18240/ijo.2020.07.01
- Soleimani M, Mehrpour M, Mohammad-Rabei H. Ophthalmic practice during COVID-19 pandemic. Int J Ophthalmol. 2021;14(5):639–642. doi:10.18240/ijo.2021.05.01
- Yadav M, Tanwar M. Impact of COVID-19 on glaucoma management: a review. Front Ophthalmol. 2022. doi:10.3389/fopht.2022.1003653
- Teratology Society Public Affairs Committee. FDA classification of drugs for teratogenic risk. Teratology. 1994;49(6):446–447. doi:10.1002/tera.1420490603
- Razeghinejad MR, Tania Tai TY, Fudemberg SJ, Katz LJ. Pregnancy and glaucoma. Surv Ophthalmol. 2011;56(4):324–335. doi:10.1016/j.survophthal.2010.11.008
- Mehran NA, Sinha S, Razeghinejad R. New glaucoma medications: latanoprostene bunod, netarsudil, and fixed combination netarsudil-latanoprost. Eye. 2020;34(1):72–88. doi:10.1038/s41433-019-0671-0
- Netland P. Glaucoma Medical Therapy: Principles and Management. New York: Oxford University Press; 2008:31–155.
- Razeghinejad MR, Nowroozzadeh MH. Anti-glaucoma medication exposure in pregnancy: an observational study and literature review. Clin Exp Optom. 2010;93(6):458–465. doi:10.1111/j.1444-0938.2010.00526.x
- Vaideanu D, Fraser S. Glaucoma management in pregnancy: a questionnaire survey. Eye. 2007;21(3):341–343. doi:10.1038/sj.eye.6702193
- Mendez-Hernandez C, Garcia-Feijoo J, Saenz-Frances F, et al. Topical intraocular pressure therapy effects on pregnancy. Clin Ophthalmol. 2012;6:1629–1632. doi:10.2147/OPTH.S36712
- Brauner SC, Chen TC, Hutchinson BT, Chang MA, Pasquale LR, Grosskreutz CL. The course of glaucoma during pregnancy: a retrospective case series. Arch Ophthalmol. 2006;124(8):1089–1094. doi:10.1001/archopht.124.8.1089
- Gedde SJ, Schiffman JC, Feuer WJ, Herndon LW, Brandt JD, Budenz DL. Treatment outcomes in the tube versus trabeculectomy study after one year of follow-up. Am J Ophthalmol. 2007;143(1):9–22. doi:10.1016/j.ajo.2006.07.020
- Razeghinejad MR, Masoumpour M, Eghbal MH, Myers JS, Moster MR. Glaucoma surgery in pregnancy: a case series and literature review. Iran J Med Sci. 2016;41(5):437–445.

