Abstract
Background
Information available in the literature on clinically based and laboratory-based outcome measures of balance is limited. How much information is provided by clinically based outcome measures compared to laboratory-based measure in patients with total hip (THA) and knee arthroplasty (TKA) is not known.
Aim
The purpose of this study was to determine the relationship between selected clinically based outcome measures and laboratory-based force platform measure in patients following THA and TKA.
Methods
Patients who underwent THA (n = 26) and TKA (n = 28) were evaluated at about 5–7 weeks following surgery. Participants were assessed using four clinically based outcome measures – 1) the Berg Balance Scale (BBS), 2) the Timed Up and Go test (TUG), 3) the Activities-specific Balance Confidence Scale (ABC), and 4) the Western Ontario McMaster Universities Osteoarthritis Index-function subscale (WOMAC-function) – and one laboratory-based force plate measure (95% ellipse area).
Results
Moderate correlations were observed between the BBS and the 95% ellipse area of force plate (r = 0.46–0.51) for the two-legged stance, the anterior lean stance, and the posterior lean stance. Fair correlations were observed between TUG and the 95% ellipse area of force plate (r = 0.31–0.37) for all the three test conditions. Low correlations were observed for the ABC and the WOMAC-function with the 95% ellipse area of force plate (r = 0.11–0.25) for all the three test conditions.
Conclusion
The BBS demonstrated the greatest correlations with the 95% ellipse area of the force plate measure and should be preferred by physical therapists over the TUG, the ABC, and the WOMAC-function to assess balance in patients with THA and TKA.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Balance is critical for mobility and physical function in the elderly.Citation1,Citation2 Balance requires integration of information from somatosensory, visual, and vestibular systems and execution of appropriate musculoskeletal responses throughout the body, including the joints of the lower extremities.Citation3 Following orthopedic injury to the joints of the lower extremities, the sensory and motor processes are disrupted subsequently leading to balance problems.Citation4 Hip and knee osteoarthritis (OA) has been reported to significantly reduce standing balance in the elderly.Citation5 Although interventions such as total hip arthroplasty (THA) and total knee arthroplasty (TKA) for hip and knee OA, respectively, help to reduce joint pain and stiffness, and improve physical function, they may not necessarily improve patient’s balance. THA and TKA are costly surgeries with respect to actual financial costs for surgery and those incurred for patient care and rehabilitation during the recovery process. It is in the interest of the patient, health care professionals, and service providers that the outcome of THA and TKA is successful. Among many causes for unsuccessful surgery is injury to the replaced hip and knee joint as a result of fall. Impairment in balance is a major cause of falls. Patients with severe hip and knee OA, as well as those who had undergone THA and TKA, have been reported to have a higher incidence of falls compared to the general population.Citation6
A variety of approaches that include subjective and objective methods have been used to assess balance in the clinical and research areas. Clinically, several outcome measures have been used to assess balance in the elderly and in patients with THA and TKA. The Berg Balance Scale (BBS)Citation7 and the Timed Up and Go test (TUG)Citation8 which are clinician administered have been commonly used to assess balance in patients with THA and TKA. The Activities-specific Balance Confidence Scale (ABC)Citation9 and the Western Ontario McMaster Universities Osteoarthritis Index (WOMAC)Citation10 are self-reported outcome measures used to assess patient’s balance confidence and physical function, respectively. However, it is not known which outcome measure best reflects the ability to maintain balance in patients with THA and TKA. In validating outcome measures, they are usually compared with the gold standard which are typically the laboratory-based measures.
Force plate systems are laboratory-based systems that have made it possible to assess patients’ balance quantitatively. Force plate systems record vertical forces acting on a platform to determine parameters for balance using center of pressure (CoP).Citation3 Many force plate systems are available and commonly use three or four strain gauges.Citation11 Researchers have used different balance assessment protocols to assess balance on force plate systems including quiet standing,Citation12 perturbed standing,Citation12 balance during functional tasks,Citation13 and balance during eyes-open and eyes-closed conditions.Citation14 However, the force plate systems are very expensive, time-consuming, not readily accessible, and impractical to use in assessing patients’ balance on a day-to-day basis in clinical settings. Clinical outcome measures of balance, on the other hand, are cost-effective, easy to administer and score, readily available, and take relatively less time to administer and score. However, whether the clinical outcome measures provide comparable information as the force plate measure, in patients with THA and TKA, remains to be seen.
Therefore, the aim of the current study was to determine the relationship between selected clinically based outcome measures and laboratory-based force platform measure in patients following THA and TKA.
Methods
Study design
Participants in this study were a sample of convenience of consecutive patients referred to a large outpatient home physical therapy provider following either THA or TKA. Patients’ charts were reviewed to assess their eligibility for the study. Patients who met the eligibility criteria were advised of the study. Eligible participants were visited by their physical therapist at their home on the first or second day after discharge from the hospital, which was about 7–10 days following their THA or TKA. Participants were assessed by their physical therapist for their eligibility and to collect relevant medical information. After the first visit, participants were visited once or twice a week until 5 weeks to impart postsurgical physical therapy and to monitor their progress. Following completion of the 5-week home physical therapy program, participants were advised to come to the biomechanics laboratory at the School of Physical Therapy.
When participants arrived at the biomechanics laboratory, they were given considerable time to get comfortable with the surroundings in the laboratory, following which they were advised about the procedure of the study. Subsequently, participants were assessed on four clinical outcome measures. First, participants were assessed on two self-reported outcome measures (the WOMAC and the ABC), and then they were assessed on two clinician-administered outcome measures (the BBS and the TUG) in no particular order of administration. After assessments on these outcome measures, participants were then assessed on a laboratory-based outcome measure, the force plate. All participants were assessed on the clinical outcome measures as well as the laboratory-based outcome measure within a week (3–6 days) following the 5-week home physical therapy program. Ethics approval for the study was received from the University Research Ethics Board for Health Sciences Research Involving Human Subjects, University of Western Ontario, and all participants provided written consent prior to participation. One of the participants provided a written informed consent to have his picture taken on the laboratory-based outcome measure and the image published in the current study. This study is registered in ClinicalTrials.gov Protocol Registration System (ClinicalTrials.gov ID: NCT01555307; Protocol ID: R-06-461).
Participants and therapist
All participants had primary unilateral THA or TKA as a result of hip or knee joint OA and had been advised by their surgeon to weight-bear as tolerated following their surgery. Patients with revision THA or TKA, or those who had been advised by their surgeon to remain non-weight-bearing or partial weight-bearing on either the operated or nonoperated leg, were excluded. Patients with neurological conditions, such as hemiplegia, peripheral neuropathy, Parkinson’s disease, multiple sclerosis, and spinal cord compression, that might affect balance, and those who were considered unable to communicate or follow instructions were also excluded from the study.
Two physical therapists, who had 3–4 years of clinical experience as a physical therapist and who routinely provided physical therapy to patients who underwent THA and TKA, participated in the study. Assessments on the outcome measures were completed only by the primary investigator, who was one of the physical therapists.
Clinical outcome measures
Berg Balance Scale
The original 14-item BBS is a clinician-administered outcome measure that was originally designed to assess balance in the elderly and has been demonstrated to be valid, reliable, and responsive.Citation7 It includes 14 simple balance tasks, which are scored on a five-point ordinal scale (0, 1, 2, 3, and 4), with a maximum total score of 56. Higher scores on the BBS indicate better balance. All 14 performance tasks on the BBS focus on balance, and it has been previously used to assess balance in patients following hip fractureCitation15 and knee OA.Citation16
The Timed Up and Go test
The TUG is also administered by clinicians and is a test of functional mobility completed using a single chair and a 3 m walkway. It combines standing up from the chair, walking, turning around, and sitting down, and the performance is timed. The faster the time, the better is the subject’s physical function.Citation8 The test is simple, quick, requires no special equipment, and has been reported to be reliable, valid, and responsive for assessing functional mobility in an elderly population.Citation17,Citation18
The Activities-specific Balance Confidence Scale
The ABC is a self-reported outcome measure that was developed by Powell and Myers,Citation9 and was demonstrated to be valid, reliable, and responsive to assess the level of patient’s balance confidence in performing specific activities. The ABC has 16 items and is scored on a 0–100% response scale. An average of scores for all items is calculated as the patient’s total ABC score.Citation9 The ABC is simple and easy to understand, and takes 5–10 minutes to complete and score. The ABC has been used to assess balance confidence in patients with stroke,Citation19 and to assess fall-related self-efficacy in elderly patients after hip fracture.Citation20
Western Ontario McMaster Universities Osteoarthritis Index
The WOMAC is also a self-reported, disease-specific questionnaire used to assess patients having OA of the hip and/or knee, and has been demonstrated to be valid, reliable, and responsive.Citation10 It consists of 24 questions distributed among three subscales: 1) a pain subscale with five questions, 2) a stiffness subscale with two questions, and 3) a physical function subscale with 17 questions. The WOMAC allows patients to make their responses using five-point scales (0, 1, 2, 3, and 4) with the total possible score being 96. Higher scores on the WOMAC indicate greater pain and stiffness, and greater difficulty in performing selected functional activities.Citation10 While the WOMAC requests information from patients about their physical function rather than balance per se, it is very commonly used to assess patients with THA or TKA, and is widely popular among clinicians and patients.Citation21–Citation24 Although typically reported as a total score, the strong relationship between the pain and functional subscales of the WOMAC reported by Stratford et alCitation24 suggests the use of function subscale score of the WOMAC in place of the total score. Subsequently, the WOMAC-function subscale (WOMAC-function) scores were used in all analyses in this study.
Laboratory outcome measure
Force plate
Balance was assessed using an Advanced Mechanical Technology, Inc. (AMTI, Newton, MA, USA) stationary 51 cm × 46 cm steel force plate with implanted strain gauges, an amplifier, and a computer with Biosoft software (AMTI) which computed the CoP excursion in millimeters while the subject stood on the force plate. As the subject sways while standing on the force plate, the CoP excursion has trajectory in all directions (anterior–posterior and medial–lateral) of the sway which can be observed on the monitor of the computer. The Biosoft software computes an ellipse which covers 95% of the data points of the CoP excursions in square centimeters. The smaller the area of the 95% ellipse for a subject, the better is his/her balance.
Previous studies have utilized CoP amplitude, which is the total distance traveled in the medial–lateral and anterior–posterior directions to describe CoP patterns during balance assessments.Citation25,Citation26 For the purposes of the current study, the 95% ellipse area of the CoP amplitude in the medial–lateral and anterior–posterior directions was used as the CoP measure, and was calculated in square centimeters using the Bio-soft software. The rationale given by Thapa et alCitation14 for using an area measure to assess balance is that it represents the portion of the base of support utilized during standing conditions. The 95% ellipse area covers 95% of the data points of the CoP amplitude in the medial–lateral and anterior–posterior direction, which according to Lee and ParkCitation27 provides good information about balance in the anterior–posterior and medial–lateral directions, and is not biased by outliers. Swanenburg et alCitation28 have reported a good reliability of 95% ellipse area of the CoP using AMTI force plate to assess balance on two-legged stance in elderly patients.
Standing balance was assessed on the force plate equipment placed in the same biomechanics laboratory. Participants were comfortably dressed in shirt and pants and were barefoot during the tests. Before the balance tests began, participants were comfortably seated on a chair placed behind the force plate while the testing procedure was demonstrated and reviewed. Participants were encouraged to ask any questions related to the procedure and report any fatigue they experience during the testing. The participants were provided with suitable rest periods if required.
A walker was positioned immediately in front of the force plate for safety purposes. The participants were instructed to use the arms of the chair to stand up and then to use the walker to achieve balance before each test (). Once the participants obtained balance, they were asked to release the walker and stand in the test position for 10 seconds during the data capture interval. They were advised to use the walker in case they lost their balance. For safety reasons and to enhance the participant’s confidence, another physical therapist was present by the participant’s side to guard against any major loss of balance and potential fall. The 10-second data collection period began when the participants said “Now”, indicating that they believed they had established balance.
The balance testing comprised three test conditions performed with the participant’s eyes open. The three test conditions were 1) two-legged stance, 2) two-legged anterior lean stance, and 3) two-legged posterior lean stance. Testing started with the two-legged standing position with evenly distributed weight, followed by the anterior and posterior lean standing positions. For the anterior and posterior lean stance, participants were instructed to lean anteriorly and posteriorly as far as they could comfortably and maintain the position. Two repetitions of each test were completed, with a 10-second rest interval between repetitions during which the patient remained standing and used the walker for support, as needed. Demonstration of the balance tests on the force plate was provided to the participants by the primary investigator prior to balance testing. No trial training was given to the participants to avoid any learning effect.
Statistical analysis
Descriptive statistics were used to characterize participants with THA and TKA on the clinical measures and the force plate measure. Student’s t-tests were used to compare participants who underwent THA with those who underwent TKA on the BBS, the TUG, the ABC, and the WOMAC-function clinical measures. Student’s t-tests were also used to compare participants with THA to those with TKA on the 95% ellipse area of the force plate for the three test conditions (two-legged stance, anterior lean stance, and posterior lean stance). An average of scores of the two repetitions for each test condition was used as the final score of 95% ellipse area for that condition.
Pearson’s correlation coefficients were used to compare scores on the BBS, the ABC, the TUG, and the WOMAC-function with those on the 95% ellipse area of the force plate for all the three test conditions. Also, Pearson’s correlation coefficients were used to compare scores among the clinical measures. Correlations were also performed separately for participants with THA and those with TKA between the clinical measures and the 95% ellipse area of the force plate for the three test conditions.
Correlation coefficients were assessed using the criteria provided by Portney and Watkins.Citation29 Correlation coefficients in the range of 0.00–0.25 indicated little or no relationship, 0.25–0.50 indicated a fair-to-moderate relationship, 0.50–0.75 indicated a moderate-to-good relationship, and above 0.75 indicated a good-to-excellent relationship. All statistical tests were completed using STATISTICA,Citation30 and the level of statistical significance was set at p < 0.05.
Sample size estimation
Based on the hypothesized prediction of a significant and moderate correlation (r ≥ 0.40) between the BBS and the 95% ellipse area of the force plate, with a power of 0.80 at a significance level of 0.05 (two-tailed), 47 participants were required to participate in this study.Citation31 Participants with THA and those with TKA were pooled together to achieve the required sample size for the study.
Results
A total of 63 participants participated in the study, of which 30 participants had THA and 33 participants had TKA. Thirty-five percent of the participants were males, and 65% females. Fifty-four participants completed the four clinical outcome measures (the BBS, the TUG, the ABC, and the WOMAC-function), and 50 participants completed the laboratory-based force plate outcome measure (95% ellipse area). Of the 54 participants who completed the clinical outcome measures, four patients were not tested on the force plate due to technical problems with the equipment. Demographic information of participants is presented in . No statistically significant differences were observed in age, height, and body mass between participants who had THA and those who had TKA (p > 0.05).
Table 1 Descriptive information of the participants
Scores on clinical outcome measures are presented in . No statistically significant differences were observed between participants who had THA and those who had TKA on the BBS, the TUG, the ABC, and the WOMAC-function (p > 0.05). Data on all clinical outcome measures were found to be normally distributed (). Also, no statistically significant differences were observed between participants who had THA and those who had TKA on the 95% ellipse area for the three force plate test conditions – the two-legged stance, the anterior lean stance, and the posterior lean stance (p > 0.05, ). Data on the force plate for all test conditions were found to be normally distributed ().
Figure 2 Histogram of scores on the clinical outcome measures, Berg Balance Scale (BBS), Timed Up and Go test (TUG), Activities-specific Balance Confidence Scale (ABC), and Western Ontario and McMaster Universities Osteoarthritis Index function subscale (WOMAC-function) by the type of surgery, total hip arthroplasty (THA), and total knee arthroplasty (TKA).
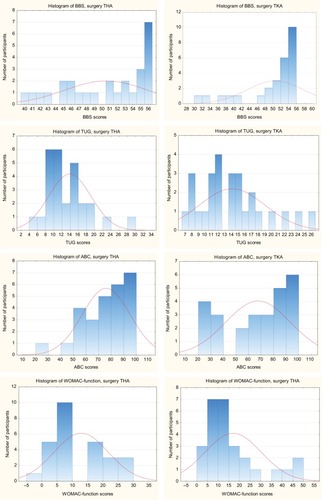
Figure 3 Histogram of scores on the force plate for the different test conditions by the type of surgery, total hip arthroplasty (THA) and total knee arthroplasty (TKA).
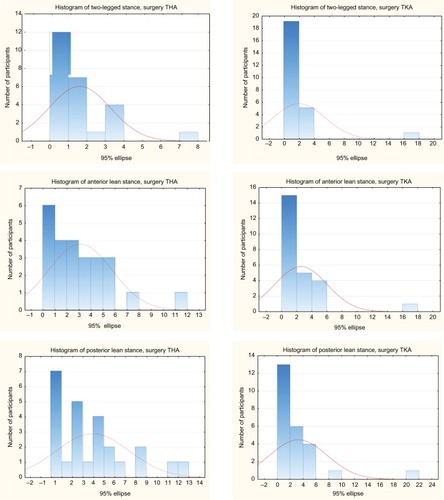
Table 2 Means and SDs for the scores on clinical outcome measures
Table 3 Values for 95% ellipse area force plate for the three test conditions
Moderate correlations were observed between the BBS and the 95% ellipse area for all the three force plate test conditions (r = 0.46–0.51, ). The scatter plot in shows that the participants who scored near maximum on the BBS had the 95% ellipse area of the force plate varied within a considerably small part of the total range observed in the study sample. Fair correlations were observed between the TUG and the 95% ellipse area (r = 0.31–0.37), again for all the three force plate test conditions. However, low correlations were observed for the ABC and the WOMAC-function with the 95% ellipse area of the force plate (r = 0.11–0.25) on the three test conditions. Correlations performed separately for participants with THA and those with TKA also demonstrated a similar pattern of relationships between the clinical measures and the 95% ellipse area of the force plate as that observed for the pooled total participants.
Figure 4 Scores on the Berg Balance Scale plotted against 95% ellipse area of the force plate. Regression line shown as illustration (r = −0.51).
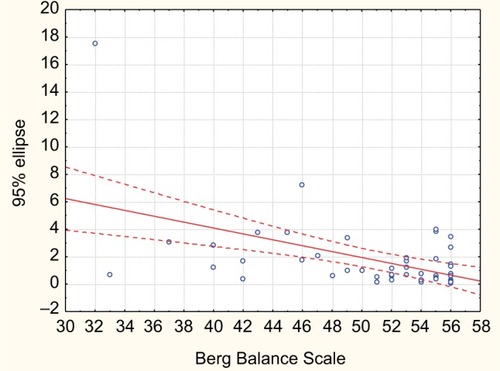
Table 4 Correlations between the clinical outcome measures and the 95% ellipse area of the force plate for the three test conditions (p < 0.05)
Correlations among the four clinical measures are presented in . The BBS and the TUG demonstrated a good relationship (r = −0.75). While the ABC demonstrated a good relationship with the TUG (r = −0.73), the relationship with the BBS was moderate (r = 0.60). The WOMAC-function demonstrated only moderate relationships with the BBS, the TUG, and the ABC (r = 0.66–0.70).
Table 5 Correlations among the four clinical measures (p < 0.05)
Discussion
The current study explored relationships of the clinical outcome measures the BBS, the TUG, the ABC, and the WOMAC-function with the laboratory-based force plate measure (95% ellipse area). The authors used concurrent validity, a measure of criterion-related validity, by comparing the clinical measures of balance with a force plate measure that has been established as standard for assessment of balance.Citation29 Moderate correlations of the BBS with the 95% ellipse area of the force plate suggest that the BBS provides information about the ability to maintain balance and supports its validity in assessing balance in patients with THA and TKA. The BBS was the only measure among the four outcome measures in the current study that demonstrated the strongest relationship with the 95% ellipse area of the force plate.
The BBS has been previously compared with other different force plate measures of balance but not the 95% ellipse area, and in different sample populations but not in patients with THA and TKA.
Frykberg et alCitation32 reported correlations similar to that observed in the current study between the BBS subgroup score of items that involved maintaining a position and the force plate measure in patients who had stroke (r = −0.50, p < 0.05), and they used the mean velocity of CoP displacement as a force plate measure. Although the mean velocity of CoP displacement has been identified as a consistent and stable force plate measure,Citation12,Citation33 Frykberg et alCitation32 reported a disproportionably low mean velocity of CoP displacement in participants even with considerably good balance with a maximum score on the BBS. However, in the current study, as illustrated in , the 95% ellipse area of the force plate could be quite small in participants with considerable balance ability as demonstrated by their maximum scores on the BBS.
Sabchuk et alCitation34 have also reported fair-to-moderate correlations between the BBS and the force plate measure in young and elderly healthy individuals (r = −0.37 to −0.51, p < 0.05) using CoP displacement as a force plate measure, and under different test conditions such as eyes-open and eyes-closed conditions. Berg et alCitation12 reported fair correlations between the BBS and the force plate measure during platform-induced sway (r = −0.38, p < 0.05), and moderate correlations when the platform was stationary (r = −0.55, p < 0.05) using CoP amplitude and speed as force plate measure, but the participants in the study were healthy elderly individuals. Based on the results of the current study, the authors support the use of the BBS by clinicians for assessment of balance in patients with THA and TKA.
The TUG demonstrated fair correlations with the 95% ellipse area of the force plate. Previous research by Sabchuk et alCitation34 that compared the TUG with CoP displacement measure of force plate also reported fair-to-moderate correlations (r = 0.32–0.47, p < 0.05) in young and elderly volunteers.
While the TUG demonstrated good correlations with the BBS in the current study, Sabchuk et alCitation34 reported moderate correlations (r = −0.57, r < 0.05) between the TUG and the BBS. All participants in the current study were elderly, while one half of the participants in the study by Sabchuk et alCitation34 were young and the other half elderly. Consistent with the results of the current study, Hatch et alCitation35 reported good correlations between the TUG and the BBS (r = 0.81, p < 0.01) in community-dwelling elderly individuals. The results of the current study suggest that if the BBS is not available, the TUG may also be used to assess balance in patients with THA and TKA and can provide comparable information as that of the force plate measure and the BBS.
The ABC demonstrated low correlations with the 95% ellipse area of the force plate in the current study and moderate correlations with the BBS. Previous work by Lajoie et alCitation36 has also reported low correlations (r = −0.17, p < 0.05) for the anteroposterior sway of the force plate measure and moderate correlations (r = −0.37, p < 0.05) for the lateral sway of the force plate measure with the ABC in elderly participants. The same authors also reported moderate correlations between the ABC and the BBS (r = 0.67, p < 0.05)Citation36 similar to the results observed in the current study. On the other hand, the ABC demonstrated good correlations with the TUG in the current study. Hatch et al,Citation35 however, reported moderate correlations between the ABC and the TUG (r = 0.69, p < 0.05) and good correlations (r = 0.75, p < 0.05) between the ABC and the BBS, but the participants in the study were healthy community-dwelling elderly individuals. The result of the current study suggests that the ABC may not provide accurate information on balance in patients with THA and TKA. The ABC is a self-reported measure that may provide information on patients’ confidence about their balance but may not provide information about patients’ balance per se.
The WOMAC-function correlated the least with the 95% ellipse area among the four clinical measures used in the current study, and the correlations were low. In addition, the WOMAC-function correlated moderately with the BBS, the TUG, and the ABC. The WOMAC-function, like the ABC, is also a self-reported measure developed to assess pain, stiffness, and physical function in patients with THA and TKA, and not necessarily balance. Low correlations were expected between the WOMAC-function and the 95% ellipse area of the force plate. The authors were trying to explore the ability of the WOMAC to provide any information on balance in addition to function as it is very widely used by clinicians to assess patients with THA and TKA. Although very popular among clinicians to assess patients with THA and TKA, the WOMAC has not been studied for its relationship with outcome measures of balance in the past. Results of the current study suggest that the WOMAC-function does not provide any information on balance in patients with THA and TKA, and does not support its use to assess balance in these patients.
In the current study, no differences were observed between patients with THA and those with TKA on all the outcome measures, and data on patients with THA and TKA were pooled together for the purpose of the study. Previous studies have also reported no differences in functional outcomes between patients who had undergone THA and those who had undergone TKA at 5–7 weeksCitation37 and at 6 monthsCitation38,Citation39 postsurgery.
In conclusion, the current study provided information suggesting that the BBS is preferable for assessing balance in patients with THA and TKA over the TUG and the ABC. The ABC and the WOMAC-function may not provide any information on the balance ability of these patients and may not be used to assess balance. Moderate relationship was observed between the BBS and the 95% ellipse area of the force plate. Fair relationship was observed between the TUG and the 95% ellipse area, and good relationship between the TUG and the BBS. The relationship of the ABC and the WOMAC-function with the 95% ellipse area of the force plate was weak.
This study presented some limitations. Participants in the study were a sample of convenience referred to home-based community physical therapy within a limited geographical area. Although participants were provided with adequate rest periods, influence of participants’ fatigue on their performance on outcome measures, especially during the later stages of the study procedure, cannot be ruled out. The clinical and force plate measures were administered to patients simultaneously one after the other, and how much learning effect occurred in participants as the assessment progressed is unclear.
Acknowledgments
The authors would like to thank all the participants who took part in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
- BrouwerBMusselmanKCulhamEPhysical function and health status among seniors with and without a fear of fallingGerontology200450313514115114034
- ChoBLScarpaceDAlexanderNBTests of stepping as indicators of mobility, balance, and fall risk in balance-impaired older adultsJ Am Geriatr Soc20045271168117315209657
- RiemannBLGuskiewiczKMSheildsEWRelationship between clinical and forceplate measures of postural stabilityJ Sport Rehabil1999827182
- FridénTZätterströmRLindstrandAMoritzUA stabilometric technique for evaluation of lower limb instabilitiesAm J Sports Med19891711181222929827
- WegenerLKisnerCNicholsDStatic and dynamic balance responses in persons with bilateral knee osteoarthritisJ Orthop Sports Phys Ther199725113188979171
- MitchellSYMcCaskieAWFrancisRMPeastonRTBirrellFNLingardEAP69 falls in patients with hip and knee osteoarthritis: the impact of joint replacement surgeryJ Bone Joint Surg (Br)200890Suppl B38518310766
- BergKWood-DauphineSWilliamJIGaytonDMeasuring balance in the elderly: preliminary development of an instrumentPhysiother Can1989416304311
- PodsiadloDRichardsonSThe timed “Up & Go”: a test of basic functional mobility for frail elderly personsJ Am Geriatr Soc19913921421481991946
- PowellLEMyersAMThe Activities-specific Balance Confidence (ABC) ScaleJ Gerontol A Biol Sci Med Sci199550A1M28M347814786
- BellamyNBuchananWWGoldsmithHCampbellJStittLValidation study of WOMAC: a health status instrument for measuring clinically-important patient-relevant outcomes following total hip or knee arthroplasty in osteoarthritisJ Orthop Rheumat1988195108
- BauerCGrögerIRupprechtRGassmannKGIntrasession reliability of force platform parameters in community-dwelling older adultsArch Phys Med Rehabil200889101977198218929026
- BergKOMakiBEWilliamsJIHollidayPJWood-DauphineeSLClinical and laboratory measures of postural balance in an elderly populationArch Phys Med Rehabil19927311107310801444775
- KarstGMVenemaDMRoehrsTGTylerAECenter of pressure measures during standing tasks in minimally impaired persons with multiple sclerosisJ Neural Phys Ther2005294170180
- ThapaPBGideonPBrockmanKGFoughtRLRayWAClinical and biomechanical measures of balance as fall predictors in ambulatory nursing home residentsJ Gerontol A Biol Sci Med Sci1996515M239M2468808996
- KulmalaJSihvonenSKallinenMAlenMKivirantaISipiläSBalance confidence and functional balance in relation to falls in older persons with hip fracture historyJ Geriatr Phys Ther200730311412018171495
- SunSFHsuCWHwangCWHyaluronate improves pain, physical function and balance in the geriatric osteoarthritic knee: a 6-month follow-up study using clinical testsOsteoarthritis Cartilage200614769670116520067
- BergerLKleinCCommandeurMEvaluation of the immediate and midterm effects of mobilization in hot spa water on static and dynamic balance in elderly subjectsAnn Readapt Med Phys2008512849518191267
- BouillonLESklenkaDKDriverACComparison of training between 2 cycle ergometers on dynamic balance for middle-aged womenJ Sport Rehabil200918231632619561372
- BotnerEMMillerWCEngJJMeasurement properties of the Activities-specific Balance Confidence Scale among individuals with strokeDisabil Rehabil200527415616315824045
- PetrellaRJPayneMMyersAOverendTChesworthBPhysical function and fear of falling after hip fracture rehabilitation in the elderlyAm J Phys Med Rehabil200079215416010744190
- MoffetHColletJPShapiroSHParadisGMarquisFRoyLEffectiveness of intensive rehabilitation on functional ability and quality of life after first total knee arthroplasty: a single-blind randomized controlled trialArch Phys Med Rehabil200485454655615083429
- KramerJFSpeechleyMBourneRRorabeckCVazMComparison of clinic and home-based rehabilitation programs after total knee arthroplastyClin Orthop Relat Res2003410225234
- SashikaHMatsubaYWatanabeYHome program of physical therapy: effect on disabilities of patients with total hip arthroplastyArch Phys Med Rehabil19967732732778600871
- StratfordPWDograMWoodhouseLKennedyDMSpadoniGFValidating self-report measures of pain and function in patients undergoing hip and knee arthroplastyPhysiother Can200961418919420808479
- GiemzaCOstrowskaBMatczak-GiemzaMThe effect of physiotherapy training programme on postural stability in men with hip osteoarthritisAging Male2007102677017558970
- ArokoskiJPLeinonenVArokoskiMHAaltoHValtonenHPostural control in male patients with hip osteoarthritisGait Posture2006231455016311194
- LeeGParkAEDevelopment of a more robust tool for postural stability analysis of laparoscopic surgeonsSurg Endosc20082241087109218030522
- SwanenburgJde BruinEDFaveroKUebelhartDMulderTThe reliability of postural balance measures in single and dual tasking in elderly fallers and non-fallersBMC Musculoskelet Disord2008916219068125
- PortneyLGWatkinsMPFoundations of Clinical Research2nd edUpper Saddle River, NJPrentice-Hall Inc2000
- StatSoft IncSTATISTICA 7.0Tulsa, OKStatSoft Inc.2000
- HulleySBCummingsSRBrownerWSGradyDHearstNNewmanTBDesigning Clinical Research2nd edPhiladelphia, PALippincott Williams & Wilkins2001
- FrykbergGELindmarkBLanshammarHBorgJCorrelation between clinical assessment and force plate measurement of postural control after strokeJ Rehabil Med200739644845317624478
- StevensonTJGarlandSJStanding balance during internally produced perturbations in subjects with hemiplegia: validation of the balance scaleArch Phys Med Rehabil19967776566628669991
- SabchukRACBentoPCBRodackiALFComparison between field balance tests and force platformRev Bras Med Esporte2012186404408
- HatchJGill-BodyKMPortneyLGDeterminants of balance confidence in community-dwelling elderly peoplePhys Ther200383121072107914640866
- LajoieYGirardAGuayMComparison of the reaction time, the Berg Scale and the ABC in non-fallers and fallersArch Gerontol Geriatr200235321522514764360
- JogiPOverendTJSpauldingSJZecevicAKramerJFEffectiveness of balance exercises in the acute post-operative phase following total hip and knee arthroplasty: a randomized clinical trialSAGE Open Med20153205031211557076926770765
- JonesCAVoaklanderDCJohnstonDWSuarez-AlmazonMEThe effect of age on pain, function and quality of life after total hip and knee arthroplastyArch Intern Med2001161345446011176772
- MahomedNNLiangMHCookEFThe importance of patient expectations in predicting functional outcomes after total joint arthroplastyJ Rheumatol20022961273127912064846


