Abstract
Background
The relationships between dietary fiber, whole grains, carbohydrate, glycemic index (GI), glycemic load (GL), and prostate cancer risk are unclear. We conducted a systematic review and meta-analysis to investigate these associations.
Methods
Relevant studies were identified by a search of PubMed database and EMBASE database up to April 2015. A random effects model was used to calculate the summary relative risks (RRs) and their corresponding 95% confidence intervals (CIs).
Results
Twenty-seven epidemiological studies (18 case–control studies and nine cohort studies) were included in the final analysis. The pooled RRs of prostate cancer were 0.94 (95% CI 0.85–1.05, P=0.285), 1.13 (95% CI 0.98–1.30, P=0.095), 0.96 (95% CI 0.81–1.14, P=0.672), 1.06 (95% CI 0.96–1.18, P=0.254), and 1.04 (95% CI 0.91–1.18, P=0.590) for dietary fiber, whole grains, carbohydrate, GI, and GL, respectively. There was no evidence of significant publication bias based on the Begg’s test and Egger’s test.
Conclusion
The findings of this meta-analysis indicate that, based on available information, dietary fiber, whole grains, carbohydrate, GI, and GL are not associated with the risk of prostate cancer.
Introduction
Prostate cancer has the second highest incidence of all cancers in men after lung cancer worldwide, and it was estimated that prostate cancer alone accounted for ~14% of all newly diagnosed cancers in the world.Citation1 Well-established risk factors for prostate cancer include age, race/ethnicity, and family history.Citation2 In addition, physical activity, body mass index, hormones, and diet have been suggested to be associated with prostate cancer risk.
In various epidemiological studies, including case–control and cohort studies, the potential relationship between dietary fiber, whole grains, carbohydrate, glycemic index (GI), glycemic load (GL), and prostate cancer risk has been investigated with inconsistent findings. For example, Walker et al,Citation3 Lewis et al,Citation4 and Deschasaux et alCitation5 reported an inverse association between fiber intake and prostate cancer risk. Augustin et alCitation6 and Hu et alCitation7 suggested a positive association between GI and prostate cancer risk. However, many other studies did not find such correlations.
To address the issues described earlier, we performed a systematic review and meta-analysis on dietary fiber, whole grains, carbohydrate, GI, GL, and risk of prostate cancer. Subgroup analyses were also carried out to identify possible variables or features moderating the results obtained.
Materials and methods
Search strategy
We searched PubMed database and EMBASE database up to April 2015 for all relevant studies with the following key words: fiber, fibre, grains, grain, carbohydrate, carbohydrates, GI, GL, glycaemic index, or glycaemic load combined with prostate cancer or prostate neoplasm. We also manually reviewed reference lists of retrieved articles and related reviews for additional pertinent studies. No language limitations were imposed.
Study selection
Studies included in this meta-analysis had to fulfill all the following criteria: 1) they had a cohort or case–control design; 2) the exposure of interest was dietary fiber, whole grains, carbohydrate, GI, or GL; 3) the outcome of interest was primary prostate cancer; and 4) studies provided the risk estimates with their 95% confidence intervals (CIs) or data to calculate them. If more than one publication from the same study population was available, the most recent and detailed study was included in this meta-analysis.
Quality assessment
The quality of included studies was evaluated by two authors with the Newcastle–Ottawa Scale (NOS) (http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp). NOS is a nine-star instrument designed to assess the selection of study population, study comparability, and ascertainment of either the exposure or the outcome of interest for case–control or cohort studies, respectively. The possible scores vary from 0 to 9. We used these scores to differentiate higher (7–9) from lower (0–6) quality studies.
Data extraction
The following data were extracted independently by two authors from each study: the first author’s last name, year of publication, study country, study design, sample size, age, types of exposure, the risk estimates with their corresponding 95% CIs, and matched or adjusted variables. From each study, we extracted the risk estimate that was most fully adjusted for potential confounders.
Statistical analysis
Considering that the absolute risk of prostate cancer is low, the odds ratio (OR) was assumed approximately the same as relative risk (RR), and the RR was used as the study outcome. Summary RR estimates with their corresponding 95% CIs for the highest versus the lowest level of fiber, whole grains, carbohydrate, GI, and GL were calculated with the DerSimonian and Laird random effect model,Citation8 which take into account both within-study and between-study variation. Subgroup analyses were performed by study design and geographic region. Heterogeneity between studies was assessed by Q statistic (significance level at P<0.10) and I2 (I2<25%, no heterogeneity; I2=25%–50%, low heterogeneity; I2=50%–75%, moderate heterogeneity; I2>75%, large or extreme heterogeneity).Citation9 A sensitivity analysis was carried out whereby each study was removed in turn and the combined estimate recalculated to determine the influence of each study. Publication bias was tested by Begg’s testCitation10 and Egger’s test.Citation11 A two-tailed P<0.05 was considered to be representative of a significant statistical publication bias. All the statistical analyses were conducted with STATA 12.0 (StataCorp LP, College Station, TX, USA).
Results
Study selection
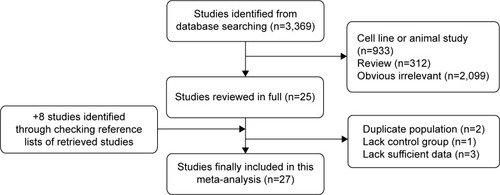
shows a flow diagram of the procedure used to identify potentially relevant studies. Searches of the electronic databases yielded 3,369 articles. After carefully reading the titles and abstracts, 3,344 studies that were obviously unrelated to our topic were excluded. Then, we reviewed the full text of the remaining 25 articles and six articles were excluded with the following reasons: duplicate population (n=2), lacking control group (n=1), and lacking sufficient data (n=3). Eight studies were identified through checking reference lists of retrieved studies. Finally, the present study included 27 epidemiological studies.Citation3–Citation7,Citation12–Citation33
Characteristics of the included studies
The main clinical features of these 27 eligible studies are summarized in . These studies were published between 1988 and 2015, including 18 case–control and nine cohort studies. Thirteen articles evaluated patients from North America, ten from Europe, two from Asia, one from Africa, and one from South America. The total number of prostate cancer patients was 39,352. Fiber was reported in 16 studies, whole grains reported in eight studies, carbohydrate reported in 13 studies, GI reported in six studies, and GL reported in five studies. Although the number of studies included in GI and GL was limited, the sample sizes were large with a total of 26,656 and 26,500 prostate cancer patients for GI and GL, respectively. In addition, these studies had high quality (mean NOS =6.8 and 7 for GI and GL, respectively) and adjusted major confounding.
Table 1 Main characteristics of the studies included in this meta-analysis
Quantitative synthesis
The pooled RRs of prostate cancer were 0.94 (95% CI 0.85–1.05, P=0.285), 1.13 (95% CI 0.98–1.30, P=0.095), 0.96 (95% CI 0.81–1.14, P=0.672), 1.06 (95% CI 0.96–1.18, P=0.254), and 1.04 (95% CI 0.91–1.18, P=0.590) for dietary fiber (), whole grains (), carbohydrate (), GI (), and GL (), respectively.
Figure 2 Summary RR of fiber intake and prostate cancer risk.
Abbreviations: RR, relative risk; CI, confidence interval.
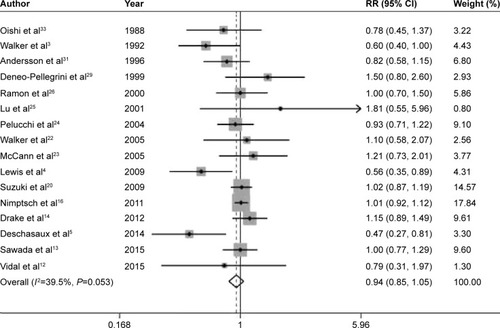
Figure 3 Summary RR of whole grains intake and prostate cancer risk.
Abbreviations: RR, relative risk; CI, confidence interval.
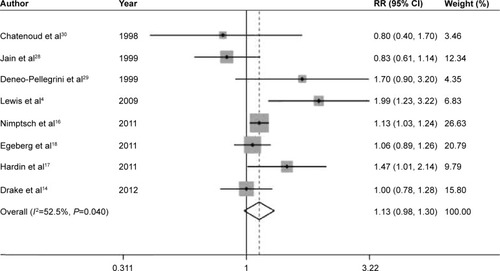
Figure 4 Summary RR of carbohydrate intake and prostate cancer risk.
Abbreviations: RR, relative risk; CI, confidence interval.
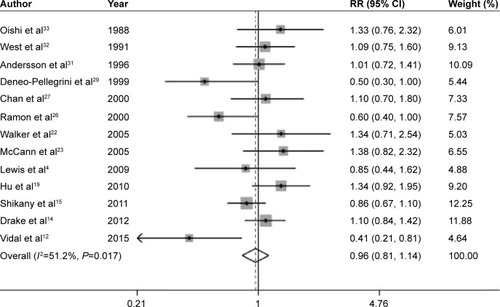
Figure 5 Summary RRs of GI (A), GL (B), and prostate cancer risk.
Abbreviations: RRs, relative risks; GI, glycemic index; GL, glycemic load; CI, confidence interval.
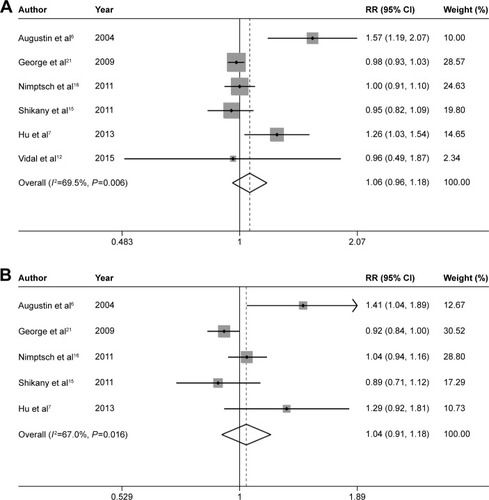
In the stratified analysis by study design and region, significant associations were observed for whole grains intake in cohort studies (RR =1.10, 95% CI 1.02–1.19, P=0.014), GI in case–control studies (RR =1.34, 95% CI 1.10–1.62, P=0.004), and GL in case–control studies (RR =1.36, 95% CI 1.08–1.70, P=0.008) (). For dietary fiber, we further conducted stratified analysis by the types of fiber. The pooled RRs of prostate cancer were 0.86 (95% CI 0.59–1.26, P=0.452), 0.93 (95% CI 0.83–1.04, P=0.213), 0.92 (95% CI 0.76–1.10, P=0.353), and 0.82 (95% CI 0.57–1.16, P=0.258) for vegetable fiber, fruit fiber, soluble fiber, and insoluble fiber, respectively.
Table 2 Pooled and subgroup analyses stratified by study design and area
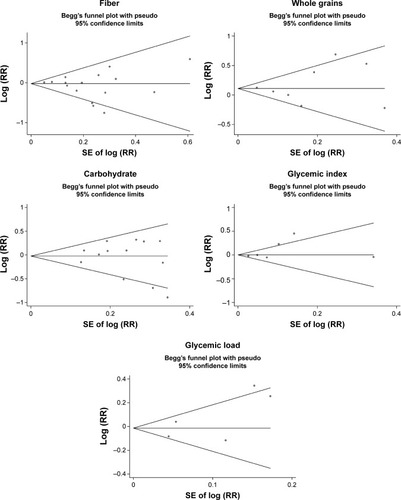
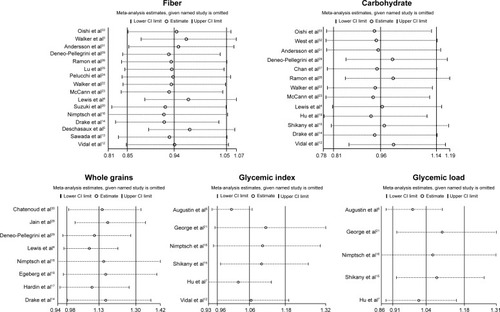
Low-to-moderate between-study heterogeneity was observed for dietary fiber (I2=39.5%), whole grains (I2=52.5%), carbohydrate (I2=51.2%), GI (I2=69.5%), and GL (I2=67.0%). There was no evidence of significant publication bias based on the Begg’s test and Egger’s test (fiber, PBegg =0.558, PEgger =0.545; whole grains, PBegg =1.000, PEgger =0.475; carbohydrate, PBegg =0.428, PEgger =0.598; GI, PBegg =0.260, PEgger =0.299; GL, PBegg =0.221, PEgger =0.247) (). Sensitivity analysis was carried out by removing each study sequentially. As shown in , for dietary fiber, carbohydrate, GI, and GL, all the pooled estimates were stable and not influenced by any included single study. However, for whole grains, the pooled estimate became statistically significant after removing the study by Jain et al.Citation28
Discussion
This systematic review of epidemiological studies evaluated the potential association between dietary fiber, whole grains, carbohydrate, GI, GL, and prostate cancer risk based on nine prospective and 18 case–control studies. Overall, the summary RRs indicated that there was no clear relationship between the above factors and prostate cancer incidence, although a few results of stratified analysis were statistically significant.
In the pooled analysis, low-to-moderate between-study heterogeneity was observed, I2 ranging from 39.5% for dietary fiber to 69.5% for GI. Significant heterogeneity may be attributed to the study population, study design, sample size, method of exposure measurement, and adjustment for confounders. The presence of heterogeneity somewhat limited the interpretation of the results.
Up to now, the only fully established risk factors of prostate cancer are age, African–American ethnicity, and family history of prostate cancer.Citation2 No lifestyle factors (eg, diet and exercise) have been conclusively confirmed as prostate cancer risk or protective factors, although many have been considered with supporting evidence. For example, physical activity in both occupational and recreational time has been associated with a decreased risk of prostate cancer.Citation34 Another recent meta-analysis of cohort studies has indicated that high intakes of dairy products and dairy calcium may increase total prostate cancer risk.Citation35 Conversely, consumption of dietary carrotCitation36 and cruciferous vegetablesCitation37 might be inversely associated with prostate cancer risk.
As for dietary fiber, whole grains, and carbohydrate, several clinical and animal studies have indicated that they may play a role in prostate cancer development. Landberg et alCitation38 reported that whole grains and bran from rye led to significantly lower plasma prostate specific antigen. Bylund et alCitation39 suggested that factors in rye bran could inhibit prostate cancer growth. Mavropoulos et alCitation40 and Freedland et alCitation41 indicated that increased carbohydrate consumption may promote tumor growth and inhibit apoptosis of prostate cancer cells. However, our meta-analysis, based on all available epidemiologic studies, indicated no statistically significant relationships between dietary fiber, whole grains, carbohydrate, and prostate cancer risk.
Emerging studies also have evaluated the relationship between dietary fiber, whole grains, carbohydrate, GI, GL, and various types of other human diseases. Aune et alCitation42 reported that there was an inverse association between dietary fiber intake and breast cancer risk. Yang et alCitation43 suggested that fiber intake was associated with a reduced risk of all-cause mortality. Consumption of whole grains has been reported to be inversely associated with the risk of colorectal cancerCitation44 and type 2 diabetes.Citation45 GI and GL have been suggested to be related with the risk of breast cancerCitation46 and digestive tract neoplasms.Citation47 Therefore, dietary fiber, whole grains, carbohydrate, GI, and GL may only play a role in specific diseases.
Our study has several strengths. This meta-analysis included a large number of studies and more than 39,000 cases, which enhanced the statistical power. All included studies ascertained outcomes according to histologic findings. A recent meta-analysis reported that there was no clear association between carbohydrate intake and the risk of prostate cancer,Citation48 which was in accordance with our study. However, we evaluated as many as five factors, including dietary fiber, whole grains, carbohydrate, GI, and GL.
Some limitations of this meta-analysis should be acknowledged. First, measurement errors in the assessment of exposure may bias the overall effect estimates. Second, residual confounding (ie, uncontrolled confounding) are always a concern in observational studies. Third, as discussed earlier, significant heterogeneity was observed among several analyses. Fourth, sensitivity analysis indicated that the summary estimate for whole grains was not stable and influenced by a single study. Finally, publication bias could not be ruled out as small studies with null results tend not to be reported.
Conclusion
Overall, the findings of this meta-analysis indicate that, based on available information, dietary fiber, whole grains, carbohydrate, GI, and GL are not associated with the risk of prostate cancer. To provide a more definitive conclusion, further prospective cohort studies with larger sample size, better exposure assessment, and longer follow-up are warranted in this area.
Acknowledgments
This study was supported from Public Welfare General Project of Huzhou Science and Technology Agency (2012YSB25).
Disclosure
The authors report no conflicts of interest in this work.
References
- JemalABrayFCenterMMFerlayJWardEFormanDGlobal cancer statisticsCA Cancer J Clin2011612699021296855
- BloomJRStewartSLOakley GirvanIBanksPJChangSFamily history, perceived risk, and prostate cancer screening among African American menCancer Epidemiol Biomarkers Prev200615112167217317119042
- WalkerARWalkerBFTsotetsiNGSebitsoCSiwediDWalkerAJCase-control study of prostate cancer in black patients in Soweto, South AfricaBr J Cancer19926534384411558801
- LewisJESoler-VilaHClarkPEKrestyLAAllenGOHuJJIntake of plant foods and associated nutrients in prostate cancer riskNutr Cancer200961221622419235037
- DeschasauxMPouchieuCHisMHercbergSLatino-MartelPTouvierMDietary total and insoluble fiber intakes are inversely associated with prostate cancer riskJ Nutr2014144450451024553693
- AugustinLSGaleoneCDal MasoLGlycemic index, glycemic load and risk of prostate cancerInt J Cancer2004112344645015382070
- HuJLa VecchiaCAugustinLSCanadian Cancer Registries Epidemiology Research GroupGlycemic index, glycemic load and cancer riskAnn Oncol201324124525122831983
- DerSimonianRLairdNMeta-analysis in clinical trialsControl Clin Trials1986731771883802833
- HigginsJPThompsonSGQuantifying heterogeneity in a meta-analysisStat Med200221111539155812111919
- BeggCBMazumdarMOperating characteristics of a rank correlation test for publication biasBiometrics1994504108811017786990
- EggerMDavey SmithGSchneiderMMinderCBias in meta-analysis detected by a simple, graphical testBMJ199731571096296349310563
- VidalACWilliamsCDAllottEHCarbohydrate intake, glycemic index and prostate cancer riskProstate201575443043925417840
- SawadaNIwasakiMYamajiTJapan Public Health Center–based Prospective Study GroupFiber intake and risk of subsequent prostate cancer in Japanese menAm J Clin Nutr2015101111812525527755
- DrakeISonestedtEGullbergBDietary intakes of carbohydrates in relation to prostate cancer risk: a prospective study in the Malmo Diet and Cancer cohortAm J Clin Nutr20129661409141823134882
- ShikanyJMFloodAPKitaharaCMDietary carbohydrate, glycemic index, glycemic load, and risk of prostate cancer in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial (PLCO) cohortCancer Causes Control2011227995100221553078
- NimptschKKenfieldSJensenMKDietary glycemic index, glycemic load, insulin index, fiber and whole-grain intake in relation to risk of prostate cancerCancer Causes Control2011221516121069447
- HardinJChengIWitteJSImpact of consumption of vegetable, fruit, grain, and high glycemic index foods on aggressive prostate cancer riskNutr Cancer201163686087221774611
- EgebergROlsenAChristensenJIntake of whole-grain products and risk of prostate cancer among men in the Danish Diet, Cancer and Health cohort studyCancer Causes Control20112281133113921656162
- HuJLa VecchiaCGibbonsLNegriEMeryLNutrients and risk of prostate cancerNutr Cancer201062671071820661818
- SuzukiRAllenNEKeyTJA prospective analysis of the association between dietary fiber intake and prostate cancer risk in EPICInt J Cancer2009124124524918814263
- GeorgeSMMayneSTLeitzmannMFDietary glycemic index, glycemic load, and risk of cancer: a prospective cohort studyAm J Epidemiol2009169446247219095757
- WalkerMAronsonKJKingWDietary patterns and risk of prostate cancer in Ontario, CanadaInt J Cancer2005116459259815825170
- McCannSEAmbrosoneCBMoysichKBIntakes of selected nutrients, foods, and phytochemicals and prostate cancer risk in western New YorkNutr Cancer2005531334116351504
- PelucchiCTalaminiRGaleoneCFibre intake and prostate cancer riskInt J Cancer2004109227828014750181
- LuQYHungJCHeberDInverse associations between plasma lycopene and other carotenoids and prostate cancerCancer Epidemiol Biomarkers Prev200110774975611440960
- RamonJMBouRRomeaSDietary fat intake and prostate cancer risk: a case-control study in SpainCancer Causes Control200011867968511065004
- ChanJMPietinenPVirtanenMDiet and prostate cancer risk in a cohort of smokers, with a specific focus on calcium and phosphorus (Finland)Cancer Causes Control200011985986711075876
- JainMGHislopGTHoweGRGhadirianPPlant foods, antioxidants, and prostate cancer risk: findings from case-control studies in CanadaNutr Cancer199934217318410578485
- Deneo-PellegriniHDe StefaniERoncoAMendilaharsuMFoods, nutrients and prostate cancer: a case-control study in UruguayBr J Cancer1999803–459159710408871
- ChatenoudLTavaniALa VecchiaCWhole grain food intake and cancer riskInt J Cancer199877124289639389
- AnderssonSOWolkABergströmREnergy, nutrient intake and prostate cancer risk: a population-based case-control study in SwedenInt J Cancer19966867167228980172
- WestDWSlatteryMLRobisonLMFrenchTKMahoneyAWAdult dietary intake and prostate cancer risk in Utah: a case-control study with special emphasis on aggressive tumorsCancer Causes Control19912285941873441
- OishiKOkadaKYoshidaOA case-control study of prostatic cancer with reference to dietary habitsProstate19881221791903368406
- LiuYHuFLiDDoes physical activity reduce the risk of prostate cancer? A systematic review and meta-analysisEur Urol20116051029104421802197
- AuneDNavarro RosenblattDAChanDSDairy products, calcium, and prostate cancer risk: a systematic review and meta-analysis of cohort studiesAm J Clin Nutr201510118711725527754
- XuXChengYLiSDietary carrot consumption and the risk of prostate cancerEur J Nutr20145381615162324519559
- LiuBMaoQCaoMXieLCruciferous vegetables intake and risk of prostate cancer: a meta-analysisInt J Urol201219213414122121852
- LandbergRAnderssonSOZhangJXRye whole grain and bran intake compared with refined wheat decreases urinary C-peptide, plasma insulin, and prostate specific antigen in men with prostate cancerJ Nutr2010140122180218620980650
- BylundAZhangJXBerghARye bran and soy protein delay growth and increase apoptosis of human LNCaP prostate adenocarcinoma in nude miceProstate200042430431410679760
- MavropoulosJCBuschemeyerWC3rdTewariAKThe effects of varying dietary carbohydrate and fat content on survival in a murine LNCaP prostate cancer xenograft modelCancer Prev Res (Phila)20092655756519470786
- FreedlandSJMavropoulosJWangACarbohydrate restriction, prostate cancer growth, and the insulin-like growth factor axisProstate2008681111917999389
- AuneDChanDSGreenwoodDCDietary fiber and breast cancer risk: a systematic review and meta-analysis of prospective studiesAnn Oncol20122361394140222234738
- YangYZhaoLGWuQJMaXXiangYBAssociation between dietary fiber and lower risk of all-cause mortality: a meta-analysis of cohort studiesAm J Epidemiol20151812839125552267
- HaasPMachadoMJAntonAASilvaASde FranciscoAEffectiveness of whole grain consumption in the prevention of colorectal cancer: meta-analysis of cohort studiesInt J Food Sci Nutr200960suppl 611319306224
- de MunterJSHuFBSpiegelmanDFranzMvan DamRMWhole grain, bran, and germ intake and risk of type 2 diabetes: a prospective cohort study and systematic reviewPLoS Med200748e26117760498
- DongJYQinLQDietary glycemic index, glycemic load, and risk of breast cancer: meta-analysis of prospective cohort studiesBreast Cancer Res Treat2011126228729421221764
- MulhollandHGMurrayLJCardwellCRCantwellMMGlycemic index, glycemic load, and risk of digestive tract neoplasms: a systematic review and meta-analysisAm J Clin Nutr200989256857619088152
- ZhaiLChengSZhangDDietary carbohydrate and prostate cancer risk: a meta-analysisNutr Cancer201567459460225875159