Abstract
The number of children with hearing loss with additional disabilities receiving cochlear implantation has increased dramatically over the past decade. However, little is known about their auditory and speech and language development following implantation. The purpose of this review is to evaluate the effects of cochlear implantation on the most common genetic and developmental disorders in children with hearing loss. Benefits of cochlear implantation for children with autism spectrum disorder, developmental delay, CHARGE syndrome, cerebral palsy, learning disorders, Usher syndrome, Waardenburg syndrome, and attention deficit/hyperactivity disorder are reviewed. Our review indicates that children with hearing loss and additional disabilities benefit from cochlear implantation, especially when implanted early. Thus, early interventions seem as important for these children as for deaf children without additional disabilities. Comparisons of outcomes across these disabilities indicate that children with little to no cognitive impairment (eg, Waardenburg sydrome, attention deficit hyperactivity disorder) have better outcomes than those with greater deficits in intellectual functioning (eg, autism, CHARGE syndrome). In addition, parents of children with hearing loss and additional disabilities report higher levels of parenting stress and greater child behavior problems than those without comorbid diagnoses. However, these parents are as sensitive when interacting with their children as parents with typically developing children using cochlear implantation. Given these results, it is critical to evaluate these children’s developmental milestones to provide early implantation and intervention, appropriately counsel families regarding realistic expectations for the implant, and facilitate family adaptation.
Introduction
A cochlear implant (CI) stimulates the auditory nerve, bypassing the defective cochlea, and provides auditory information to the developing brain, thus improving oral language.Citation1,Citation2 They are currently approved for individuals with bilateral severe to profound sensorineural hearing loss. They are now widely used for children, with a growing body of evidence suggesting they are beneficial for speech and language development, as well as joint attention, symbolic play, and behavioral regulation.Citation3–Citation5 Initially, CIs were not recommended for children with hearing loss and additional disabilities.Citation6–Citation8 However, 30%–40% of children currently receiving CIs have a comorbid disorder, with mixed evidence of their potential benefits.Citation9
The purpose of this review is to evaluate the effects of CIs on the most common genetic and developmental disorders in this population and provide guidance on the needs for future research. There were no articles comparing normally hearing children with developmental or genetic disorders to CI users available to review. Notably, children with additional disabilities, but no hearing loss, are typically not referred to or evaluated by CI centers, and their trajectory of early intervention services is substantively different. We have organized this review based on the extent of developmental delays (DDs) associated with each disorder, from most severe (atypical) to least severe (typical). Each section provides a definition of the disorder, an estimate of its prevalence among the general population and in children with hearing loss, and a review of published outcomes.
Autism spectrum disorder
Autism spectrum disorder (ASD) is a developmental disability that causes significant social, communication and behavioral challenges. Severity is assessed on a continuum and includes children previously diagnosed with Pervasive Developmental and Asperger’s Disorder. ASD is characterized by impairment in social interactions, atypical communication, and restrictive, repetitive behaviors. Epidemiological studies found the prevalence of cognitive impairment in children with ASD to range between 50% and 70%.Citation10,Citation11 According to the Centers for Disease Control, one in 68 children are identified as having some form of ASD, and males have a greater likelihood of developing ASD than females (5:1; see ).Citation12 Comorbidity rates of hearing loss in children with ASD are high and increasing, with estimates of children having both ranging from 1% to 6%.Citation13 There is a disproportionate number of children with profound hearing loss who have a coexisting diagnosis of ASD (35.4%). In 2009–2010, the Annual Survey of Deaf and Hard of Hearing Children and Youth indicated that one in 59 children with hearing loss also receive services for ASD.Citation14
Table 1 Prevalence data for common comorbid disorders with hearing loss
In the largest, nationally representative study of young children receiving CIs (Childhood Development after Cochlear Implantation; CDaCI),Citation15 eight of 188 deaf children were diagnosed with an ASD.Citation16 Comparisons of receptive and expressive language skills and behavior problems before to 3 years after implantation indicated that those with an ASD had lower initial language scores but similar rates of externalizing behavior problems than those who were developing typically. Over time, children with ASD improved in both receptive and expressive language, but at half the rate of those who did not have a comorbid diagnosis. Increases in externalizing behaviors were also observed over the 3-year period in the ASD group compared with the non-ASD group. This is consistent with a more recent national study in Ireland.Citation17
Improvements in speech and language skills were also reported in a small descriptive study of children with ASD and hearing loss.Citation18 Four of the 14 children used verbal communication. In a retrospective chart review of six children aged 3–16 years with ASD and hearing loss, positive changes postimplantation were noted in responsiveness to sound, speech perception, interest in music, vocalizations, and eye contact.Citation19 Further, five of six parents would have recommended a CI for a family in a similar situation.
In sum, although few studies have been conducted comparing the outcomes of cochlear implantation in children with versus without ASD, the results are generally positive in terms of speech and language outcomes, and it seems critically important to provide this auditory stimulation. Given the challenge of “diagnostic overshadowing”, in which ASD may be overlooked in children with hearing loss, health care providers should closely monitor developmental milestones to identify those at increased risk for ASD or those who might benefit from a more in-depth assessment.
Developmental delay
In young children, DDs are characterized by a failure to reach expected developmental milestones, including motor and intellectual functioning.Citation20 This is a common diagnosis for children under the age of 5 years, for whom standardized testing is not possible. DDs occur frequently in children with hearing loss, who lack auditory input and communicative skills. Children with DD may have severe or more mild impairments as shown in ; however, we have reviewed studies of children with various levels of hearing loss and DD in the following text.
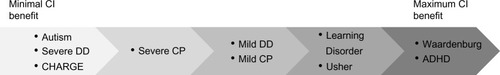
Figure 1 Various disabilities discussed in this paper placed on a continuum from minimal potential benefit to maximum potential benefit based on a review of the literature.
Children with DD experience impairments in adaptive functioning, such as communication, social skills, academic achievement, and independence. DD is usually caused by traumatic brain injury, genetic disorders (eg, CHARGE syndrome), viruses (cytomegalovirus), or abnormalities in the brain. DD has an overall prevalence of one in six children and approximately 15% of all those aged 3–17 years have one or more developmental disabilities.Citation21 Males are affected more often than females. Studies estimate that DDs occur in approximately 23%–34% of children receiving CIs.Citation22
Seven studies focusing on children with CIs and DD reported mixed evidence of improvements in auditory and speech and language outcomes. Results varied based on severity of impairment. Amirsalari et al compared 28 children with mild DD, based on gross motor functioning, with 234 children with CIs but without DD, before and 2 years after implantation.Citation23 Children in both groups demonstrated significant progress on the Categories of Auditory Perception and Speech Intelligibility Rating from pre to post implantation. No significant differences were found between the groups on the Categories of Auditory Perception or Speech Intelligibility Rating 2 years following implantation.
In contrast, Holt and Kirk reported on a group of 19 children with mild cognitive delays (mean age at implantation 37.7±14.6 years) and 50 without delays (mean age at implantation 28.8±13.2 years).Citation24 Measures of receptive and expressive language and sentence recognition, averaged across 2 years postimplantation, showed that children with mild cognitive delays scored significantly lower than their non-delayed peers. Hiraumi et al also found that eleven children with DD had lower speech perception skills than 24 non-delayed children 2 years after CI surgery.Citation22
Although the literature on auditory perception and speech intelligibility in children with mild delays is mixed, several studies have found that a greater degree of DD is associated with worse outcomes. Pyman et al retrospectively examined the speech perception outcomes for 75 pediatric CI users (mean age at implantation 3.2±1.2 years) to determine the effects of etiology of deafness.Citation25 Results showed that the presence of motor and/or cognitive delays was associated with slower high-level speech processing ability. Wiley et al similarly compared 14 children with DD (mean age at implantation 17 months) with 21 children without DD (mean age at implantation 16 months).Citation26 Children with DD were classified as either severely or mildly delayed. Results 1 year postimplantation showed that children with mild delay (ie, a developmental quotient of ≥80) made similar auditory skills improvement as those without DD. Children with more severe delay (ie, developmental quotient <80) were much slower in making these improvements. In a more recent study, children with DD (mean age at implantation 41.4 months) demonstrated gains in receptive language, self-care, and social functioning 1 year after implantation.Citation27
In addition, Edwards et al found that those with versus without DD (n=11 with DD; n=21 without DD) had significant delays in speech intelligibility and perception 1 and 2 years after surgery.Citation28 Post hoc analyses showed that children with severe DD had poor outcomes, but those with mild delays showed demonstrable progress. In general, retrospective chart reviews have indicated that children with DD demonstrate wide variability in speech and language outcomes following implantation.Citation26,Citation27,Citation29–Citation38
Overall, results were mixed, with children who had more severe DD lagging further behind than those with milder DD. Findings from individual studies were likely influenced by the inclusion and exclusion criteria for DD, how it was assessed, and which outcome measures were utilized. However, it is clear that children with DD do improve following cochlear implantation, although their rate of change may be slower than expected for typically developing deaf children.
CHARGE syndrome
CHARGE syndrome is a rare genetic pattern of birth defects, which occurs in about one in every 9–10,000 births worldwide (see ). It is an extremely complex syndrome, involving extensive medical and physical difficulties that vary across children. Infants with CHARGE syndrome are often born with severe birth defects, including coloboma (eg, visual defects causing vision loss), malformed cochlea, complex heart defects, and intellectual impairment.Citation39 Approximately 50% of children with CHARGE syndrome have typical intellectual functioning, 25% have moderate functioning, and 25% have very poor functioning.Citation40,Citation41 The incidence of severe to profound hearing loss ranges from 34% to 38%, with up to 75% of patients having some degree of hearing loss.Citation42,Citation43
In a study of eleven children with CHARGE syndrome implanted at 1–3.5 years of age and followed for 1–15 years, all showed varying degrees of auditory benefit. After cochlear implantation, most continued to show a mild hearing loss (eg, 30–45 dB). Note, however, improvements were found on a parent report measure of auditory skill development.Citation44 The majority of children were using manual communication and were enrolled in special education classrooms.
Two studies that each included six children with CHARGE syndrome, with a mean age at implantation of 4.9–5.9 years, measured speech perception and auditory performance.Citation42,Citation45 In both studies, children showed variable but improving performance depending on age and time since implantation. Children with CHARGE syndrome who had more severe intellectual disabilities showed poorer performance than the average. Five children with CHARGE syndrome, who had a mean age of 37 months at time of implantation, were followed for 1–4.5 years. Two used verbal communication, one began using oral language, and two did not develop any communicative skills.Citation43
Three case studies of children with CHARGE syndrome indicated that children showed benefits in terms of detection of sound, recognition, and identification of environmental sounds, and in some children, a demonstrable improvement in receptive language.Citation39,Citation46,Citation47 Although improvements in auditory perception have been documented in children with CHARGE postimplantation, their oral language skills appear to be limited. A comprehensive early intervention program is needed to follow up on the complex issues these children face.Citation16
Cerebral palsy
Cerebral palsy (CP) is a group of disorders that affects the development of movement, balance, and posture, and is the most common motor disability in childhood. “Cerebral” means having to do with the brain and “palsy” means weakness or problems using the muscles. CP is caused by abnormal brain development affecting control of children’s muscles.Citation48 Although all individuals with CP have problems with movement and posture, the severity of symptoms vary from person to person, ranging from mild difficulties with ambulation and fine motor control to use of assistive devices to walk and lifelong care. CP does not get worse over time, although symptoms often worsen over a person’s lifetime. It is frequently associated with other comorbidities, such as intellectual disability, seizures, problems with speech and hearing, and changes in the spine (eg, scoliosis). Cognitive impairment has been found in 2%–44% of children with CP; however, the prevalence increases when epilepsy is present.Citation49 Furthermore, among children with severe CP, approximately 97.7% have a profound mental impairment. The prevalence of CP is approximately one in 323 children in the USA, with 12%–25% experiencing some level of hearing loss (see ).Citation48–Citation50
In a small study comparing children with CIs and CP with those with CIs alone (n=8; age and sex-matched pairs), audiologic outcomes were mixed.Citation51 Within the CP group, four children performed similarly to their matched peers on measures of receptive and expressive language, speech perception, and social maturity. These children had less severe cognitive and motor impairment. The remaining four children in the CP group had a more severe degree of impairment and demonstrated slower rates of improvement in speech and auditory perception over time compared with the control group. Cruz et al also found that children with CP (n=4) develop language at a slower rate than CI children without additional disabilities.Citation16 The CP group also displayed higher rates of externalizing behaviors (eg, aggression) than typically developing children prior to implantation. However, externalizing behaviors decreased over time at a rate similar to that in the control group.
Steven et al evaluated the speech recognition scores of 36 children with CP 2 years after implantation without a control group.Citation52 Results showed that children with mild cognitive disabilities displayed speech recognition scores that were significantly higher than those with severe impairments. Similarly, Bacciu et al reported on the auditory perception and speech intelligibility of five children with CP and CIs (mean age at implantation 91.6±9.7 years).Citation53 All five children demonstrated substantial improvements in auditory perception and speech intelligibility at least 1 year after device activation.
In conclusion, results were mixed, with children who had more severe CP developing language at a slower rate than those with milder CP. The findings across studies are similar to those for children with DD. It is evident that children with CP do improve following cochlear implantation, although expectations for development may need to be adjusted based on the degree of impairment. Furthermore, specific accommodations are often needed to assist the child with CP in wearing the implant device. A physical or occupational therapist should be consulted when making these adjustments.
Learning disorder
Learning disorder (LD), also known as “specific learning disorder” in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), is a neurodevelopmental disorder characterized by persistent difficulties learning core academic skills.Citation20 Key academic skills include reading single words accurately and fluently, reading comprehension, written expression and spelling, calculation, and mathematical reasoning. LD occurs due to an interaction of genetic, epigenetic, and environmental factors that affect the brain’s ability to perceive or process verbal or nonverbal information efficiently and accurately. In contrast to talking and walking, which are acquired developmental milestones that occur with maturation of the brain, academic skills must be explicitly taught and learned.Citation20 LDs disrupt the acquisition of learning skills, despite having an adequate opportunity to learn.
The prevalence of LDs across academic domains of reading, writing, and mathematics is 5%–15% among school-aged children (see ).Citation20 LDs are more common in males than females (estimates range from 2:1 to 3:1). Deafness has been linked to increased rates of academic difficulties, particularly the acquisition of reading skills.Citation54 The Annual Gallaudet Survey reported a national average of 7.2%.Citation14
Studies have shown a mixed pattern of outcomes. Isaacson et al matched five post-meningitic children with CIs and LDs (mean age at implantation 5.4 years) to non-LD peers (mean age at implantation 5.2 years).Citation55 In general, children with hearing loss and LDs made substantial improvements postimplantation; however, their progress was slower and less consistent in speech perception, speech-reading, and receptive vocabulary than the non-LD group over 30 months postimplantation. In contrast, Cruz et al compared seven children with LDs with 157 children without additional disabilities, and found no significant differences in the rate of language growth between groups pre to 36 months postimplantation.Citation16 However, the LD group had worse language scores prior to implantation. It is important to note that externalizing behavior problems decreased over 3 years postimplantation in this group. Positive outcomes from preimplantation to postimplantation were also reported in a sample of 20 children with CIs and LDs 1 year after implantation.Citation56 However, there was no typically developing deaf comparison group. Two case reports also reported improvements in speech intelligibility and auditory perception.Citation26,Citation57
Studies of children with hearing loss and LD, which documented later implantation (eg, after 10 years of age) have consistently reported worse language outcomes and furthermore their reliance on manual forms of communication.Citation58–Citation60 Both the severity of the learning disability and length of auditory deprivation are key factors in explaining the variability of these speech and language outcomes. In sum, these children should be implanted as early as possible and should receive early intervention and ongoing monitoring of their academic functioning.
Usher syndrome
Usher syndrome is an autosomal recessive, genetic disorder that affects both hearing and vision, with three clinical subtypes. It occurs in 3%–6% of children with congenital deafness and may account for 50% of the deaf-blind population (National Institute of Child Health and Human Development, 2008; see ).Citation61 In the typical population, Usher syndrome occurs in ten of every 100,000 people.Citation62 Usher syndrome type 1 is the most common and severe, characterized by profound hearing loss, vestibular dysfunction, and retinitis pigmentosa. Retinitis pigmentosa leads to degeneration of the rods of the retina causing impaired night vision, progressive narrowing of the visual field, and loss of peripheral vision. Type 2 is also common and is associated with moderate to severe hearing loss, retinitis pigmentosa, and normal vestibular function. Type 3 has a prelingual or post-lingual onset of progressive hearing loss, progressive loss of vestibular function, and occasionally, late onset of retinitis pigmentosa. Little is known about the prevalence of cognitive impairments in children with Usher syndrome. One study reported that 15% of their sample had some degree of intellectual impairment.Citation63 Another study found similar levels of cognitive performance when comparing children with Usher syndrome and CIs to children with hearing aids.Citation64
A multisite study of children receiving CIs from 1991 to 2010 identified 712 children; 26 (3.7%) of these children also had Usher syndrome type 1.Citation65 Mean time to follow-up was 7.8 (1–16) years. Speech perception outcomes for those with Usher syndrome indicated that 92% were able to achieve some level of open-set speech perception on age-appropriate tests and over half of these children were also oral communicators.
In a study at two CI centers, nine children with Usher syndrome type 1, implanted between age of 2 and 15 years, completed measures of speech perception and CI usage.Citation61 Outcomes were measured 1–2 years postimplantation. Six of nine children could discriminate speech sounds without lip reading, and three of nine scored well on an open-set word recognition task. Those who were implanted earlier, prior to the age of 3 years, performed significantly better than those implanted later. In a second study, of seven children with Usher syndrome type 1 and aged 7–16 years performed better on a working memory task (ie, sentence completion and recall) and nonword discrimination task than typically developing children with CIs.Citation64 No differences were found between these groups with regard to phonologic working memory.
In a study of 14 children and adults with Usher syndrome type 1, followed for 24–120 months, five of seven implanted before the age of 10 years improved significantly over time on a speech perception test.Citation66 Earlier implantation led to better performance. No relationship was found between gene mutation and audiologic outcomes. In a subsequent analysis of the same sample, children and adults with Usher syndrome using CIs reported better health-related quality of life scores on a hearing-specific questionnaire than those who were not implanted.Citation67 Overall, children with Usher syndrome type 1, which is the most severe form, performed similarly to typically developing children with CIs. Thus, early identification and implantation is recommended.
Waardenburg syndrome
Waardenburg syndrome (WS) is a group of genetic conditions that may cause hearing loss and changes in the pigmentation of the hair, skin, and eyes.Citation68 Children with WS often have extremely pale blue eyes or different colored eyes; in some cases, one eye may contain segments of two different colors. WS is also distinguished by a white forelock of hair or premature graying. There are five clinical subtypes of WS, each categorized by different physical characteristics. Types I and II are the most common and have similar features, with the exception of widely spaced eyes in those with type I. Limited evidence exists for a link between WS and cognitive impairment. One study reported delayed development or poor school performance in nine of 52 children with WS.Citation69 WS is caused by mutations in the EDN3, MITF, PAX3, SNAI2, and SIX10 genes and is inherited in an autosomal dominant pattern.
Estimates of prevalence are one in every 42,000 births, with equal sex representation.Citation70 Sensorineural hearing loss occurs in 35%–78% of children with type I WS and 55%–91% of children with type II WS.Citation71,Citation72 WS accounts for 2%–5% of all cases of congenital hearing loss.Citation73 Approximately one in five children with WS has a hearing loss that warrants some type of amplification (see ).Citation74 When evaluating a child with WS for implantation, extensive radiologic screening should be conducted. Several studies have described structural abnormalities of the inner ear that may affect the surgical procedure, such as vestibular aqueduct dilatations and semicircular malformations.Citation75–Citation77
A review of the literature revealed nine articles that specifically studied cochlear implantation in deaf children with WS (see ). Overall, the majority of studies found improved auditory performance and speech intelligibility. Three studies compared outcomes in implanted children with and without WS. Amirsalari et al compared six young deaf children with WS (mean age 26±15.8 months) and 75 deaf children without WS (mean age 54.5±14.8 months) 1 year following implantation.Citation78 Age at implantation was 2.2 years for the WS group; however, these data were not reported for the control group. All of the children with WS demonstrated significant improvement in auditory perception and speech intelligibility from preimplantation to postimplantation. However, the WS group had lower speech intelligibility than the control group. In contrast, no differences were found on auditory performance. Note that the WS group was 2 years younger than the control group and it is unclear whether chronological age was controlled for in the analyses. In a second comparison study, a small group of WS children (n=5; mean age at implantation 30.6±9.7 months) were compared with 261 non-syndromic children (mean age at implantation 36.7±18.6 months) and no differences were found between groups with regard to measures of auditory perception or speech performance.Citation79
Table 2 Studies in children with cochlear implantation and additional disabilities
In a sample of older children, Kontorinis et al compared outcomes in 25 deaf children with WS (mean age at implantation 5.9 years) with 50 children who had non-syndromic deafness (mean age at implantation not reported).Citation75 No significant differences were found between groups 8 years postimplantation on measures of auditory perception. However, the authors reported that four of 25 deaf children with WS showed little progress following implantation.
The remaining six studies reported implantation outcomes without a control group.Citation30,Citation73,Citation76,Citation77,Citation80–Citation82 All but one study found improvements in speech and language skills following implantation. Additionally, Broomfield et al compared outcomes across 38 children with different causes of syndromic deafness, 10 of whom had WS. Significant variation was found between and within syndromic groups. Retrospective reviews, which collapsed across disabilities, included children with WS, but did not analyze their outcome data separately.Citation32–Citation34,Citation57,Citation83
In sum, this review indicates that deaf children with WS who are implanted develop similar auditory perception and speech intelligibility skills as those with typical sensorineural hearing loss.
Attention deficit/hyperactivity disorder
Attention deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with daily functioning.Citation20 There are three primary classifications of ADHD predominantly inattentive presentation, which includes off-task behavior, lack of persistence, difficulty sustaining attention, and general disorganization; predominately hyperactive/impulsive presentation, which includes excessive motor activity, talkativeness, and impulsive behavior; and a combination of the above symptoms (inattentive and hyperactive behaviors). ADHD has a strong genetic component and is characterized by delayed development of the prefrontal cortex, which affects inhibition and self-regulation.Citation84 It is also associated with significant academic and social impairment.Citation20 Children with ADHD often experience cognitive difficulties, and perform poorly on tests of attention, executive functioning, memory, and processing speed.Citation20 Baker et al found that children with DD were three times as likely to have an ADHD diagnosis than typically developing children.Citation85
Population estimates indicate that ADHD occurs in approximately 5% of children and is more common in males than females (ratio 2:1; see ).Citation20 The Annual Survey of Deaf and Hard of Hearing Youth conducted by Gallaudet University reported similar prevalence rates of ADHD (3.4%–6.8%); however, several studies have reported higher rates of attention and impulsivity in children with hearing loss.Citation4,Citation14,Citation86
Outcomes of implantation in children with ADHD were reported in six studies that aggregated disabilities. The majority of these studies found that these children benefitted from implantation. Cruz et al compared 12 children with ADHD with 157 children without additional disabilities.Citation16 No significant differences were found in the rate of language growth preimplantation to 36 months postimplantation, suggesting children with ADHD develop language at a similar rate as typically developing children with CIs. Despite the improvements in language skills, these children evidenced increasing rates of externalizing behavior problems over time in comparison with children with CIs.
In general, retrospective chart reviews showed that children with ADHD improved significantly postimplantation, as measured by speech perception and communicative ability.Citation31,Citation56–Citation58 Similarly, case studies have also reported positive language outcomes for children with ADHD and hearing loss. Moreno-Torres et al described the language outcomes for a 9-year-old girl implanted at 18 months and diagnosed with ADHD-inattentive type at 3 years of age.Citation87 Results showed that some aspects of oral language (eg, acquisition of verbal morphemes) occurred within the typical timeframe of a CI user, but other domains were delayed, such as the number of lexical and grammatical errors, and mean length of utterance. In contrast, children with ADHD and comorbid learning or intellectual disabilities had worse performance across both retrospective reviews and case studies.Citation31,Citation60,Citation88
In conclusion, there is consistent evidence that children with ADHD and hearing loss benefit from cochlear implantation. Note, however, these children have difficulties with visual selective attention and externalizing behaviors, which may negatively impact the efficacy of cochlear implantation. Therefore, it may be important to assess these behaviors and incorporate parent training to target these issues.Citation4,Citation89 However, identification of ADHD in children is complex because attention difficulties are common at young ages and definitive diagnosis is often not made until the child enrolls in school.
Family influences on CI outcomes
The studies reviewed above focused almost exclusively on auditory and speech and language outcomes, ignoring the larger family system in which these children develop.Citation90 In the CDaCI study, the largest longitudinal study of young children receiving CIs, two key parental factors were examined that affect outcomes, ie, parenting stress and maternal sensitivity (MS). The CDaCI study enrolled 188 deaf children of hearing parents prior to implantation and 97 age-matched normally hearing children, with assessments every 6 months over 3 years.Citation15 The average age of the deaf children prior to implantation was 26.7 months and in the hearing comparison group was 27.5 months. All of the deaf children had severe to profound hearing loss and parents committed to educating their children in spoken English.
Parenting stress
We measured both general and context-specific parenting stress using the Parenting Stress Index and the Family Stress Scale.Citation89,Citation91,Citation92 At baseline, prior to implantation, we found that parents of deaf children reported similar levels of general stress but higher levels of deaf-specific stress. Highest ranked stressors for parents of children with hearing loss were communication, finances, and educational concerns. In contrast, parents of hearing children ranked finances, disciplines, and safety as their top three stressors.Citation89 Hearing status was significantly related to parenting stress by way of language delays and externalizing child behavior problems.
Levels of parenting stress may be even higher when raising a child who is deaf with an additional disability. To test this hypothesis, we compared parents of typically and atypically developing deaf children on both of these measures. Prior to implantation, these two subgroups did not differ in levels of generic or context-specific stress [Parenting Stress Index (t(145) =−0.40, P>0.05; Family Stress Scale t(158) =−0.30, P>0.05]. At the assessment 36 months after cochlear implantation, significant differences in parenting stress were found between these subgroups on both measures, with parents of children having additional disabilities reporting higher levels of stress [Parenting Stress Index, t(132) =−3.1, P<0.05, r=0.35; Family Stress Scale, t(157) =−3.1, P<0.05, r=0.31].
Maternal sensitivity
In addition, we videotaped parent–child interactions in both the deaf and hearing groups in the CDaCI study every year for 4 years to evaluate levels of MS. This construct is well-validated and has been used in several large national studies such as the National Institute of Child Health and Human Development Early Childcare Study.Citation93,Citation94 MS was scored by rating videotapes of structured and unstructured parent–child interactions on the following dimensions: sensitivity/responsivity, respect for child autonomy, positive regard, and hostility (reverse-coded). At baseline, parents of deaf children were less sensitive on the MS composite than parents of hearing children and this difference was observed across the 4 years postimplantation.Citation95 Further, after accounting for early hearing experience and child and family demographics, MS predicted growth in oral language over 4 years, and the magnitude of this effect was similar to that observed for age at implantation. Specifically, children of parents with higher MS had only a 1.3-year language delay 4 years post-CI compared with a 2.7-year delay in children of parents with low MS.
An examination of MS in the typically and atypically developing children revealed no significant differences at baseline [t(183)= 0.8, P>0.05] or 3 years after implantation [t(172)=1.1, P>0.05]. Thus, despite the challenges of managing a child with a CI who has other disabilities, these parents were equally sensitive when interacting with their children. Given that MS plays a strong role in the development of oral language, the family resilience evidenced by these parents argues strongly for the importance of early implantation.
Conclusion
Our review indicates that children with hearing loss and additional disabilities benefit from cochlear implantation, and similar to typically developing deaf children, earlier implantation is better.Citation96 The majority of articles have focused on auditory performance and speech and language development. Overall, these studies showed that children’s speech intelligibility and auditory perception improved following implantation, despite a slower rate of growth. A few studies also reported positive outcomes for self-care, social functioning, and quality of life. In the CDaCI study, we found that parents of children with deafness and additional disabilities reported higher levels of parenting stress and child behavior problems than those without comorbid diagnoses. On the positive side, these parents were as sensitive when interacting with their children. This suggests that early interventions to reduce family stress and foster positive parent–child interactions are needed.
Comparisons of outcomes across these disabilities indicated that children with little to no cognitive impairment (eg, WS, ADHD) had better outcomes than those with greater deficits in intellectual functioning (eg, autism, CHARGE syndrome). We have illustrated these outcomes by disability and potential benefit in . Given these results, it is critical to evaluate these children’s developmental milestones to provide early implantation and intervention, appropriately counsel families regarding expectations for the implant, and facilitate family adaptation.Citation16,Citation97
Prior research in this area has been plagued by a number of methodologic limitations, which have limited our understanding of the potential benefits of implantation for this population. These studies have relied on case reports, retrospective chart reviews, and prospective investigations with small samples. Future studies with limited samples should report effect sizes, given that they are likely underpowered to find statistically significant effects. There is also a need for multisite, collaborative studies that utilize the same outcome measures and evaluate larger numbers of children with hearing loss and additional disabilities. In addition, a broader array of outcomes should be examined to identify potential benefits of implantation, such as improved attention, behavioral regulation, social functioning, school performance, and health-related quality of life.Citation4,Citation98,Citation99
In conclusion, we strongly advocate for early cochlear implantation in children with hearing loss and additional disabilities. CI centers should make accommodations in their protocols for evaluation, CI programming, and rehabilitation services for these children and their families. These services are best provided by multidisciplinary teams, which include social workers and psychologists who can assist with both assessment and the intervention process.
Disclosure
The authors report no conflicts of interest in this work.
References
- ParmentSLymnCGlassRCochlear implantsJAMA20042912398741758
- SvirskyMARobbinsAMKirkKIPisoniDBMiyamotoRTLanguage development in profoundly deaf children with cochlear implantsPsychol Sci200011215315811273423
- NiparkoJKTobeyEAThalDJSpoken language development in children following cochlear implantationJAMA2010303151498150620407059
- BarkerDHQuittnerALFinkNEEisenbergLSTobeyEANiparkoJKPredicting behavior problems in deaf and hearing children: the influences of language, attention, and parent-child communicationDev Psychopathol200921237339219338689
- CejasIBarkerDHQuittnerALNiparkoJKDevelopment of joint engagement in young deaf and hearing children: effects of chronological age and language skillsJ Speech Lang Hear Res20145751831184124845423
- BerlinerKIEisenbergLSMethods and issues in the cochlear implantation of children: an overviewEar Hear1985636S13S3839477
- BlackFONorthernJLBrimacombeJASelection of children for cochlear implantationMecklenbergDJSeminars in Hearing7Thieme Medical PublishersNew York, NY, USA1986
- TiberNA psychological evaluation of cochlear implants in childrenEar Hear19856348S51S3839475
- JohnsonKWileySCochlear implantation in children with multiple disabilitiesEisenbergLSClinical Management of Children with Cochlear ImplantsSan Diego, CA, USAPlural Publishing Inc.2009
- ChakrabartiSFombonneEPervasive developmental disorders in preschool childrenJAMA2001285243093309911427137
- CharmanTPicklesASimonoffEChandlerSLoucasTBairdGIQ in children with autism spectrum disorders: data from the Special Needs and Autism ProjectPsychol Med2011410361962721272389
- Centers for Disease ControlAutism Spectrum Disorder2014 Available from: http://www.cdc.gov/ncbddd/autism/facts.htmlAccessed Janurary 25, 2015
- Autism and Developmental Disabilities Monitoring Network Surveillance Year 2008 Principal InvestigatorsCenters for Disease Control and PreventionPrevalence of autism spectrum disorders: Autism and Developmental Disabilities Monitoring Network, 14 Sites, United States, 2008MMWR Surveill Summ2012613119
- Gallaudet Research Institute2011–12 Regional and National Summary2012 Available from: http://www.gallaudet.edu/rsia/research_support/demographics.htmlAccessed Janurary 30, 2015
- FinkNEWangNYVisayaJChildhood development after cochlear implantation (CDaCI) study: design and baseline characteristicsCochear Implants Int20078292116
- CruzIVicariaIWangN-YNiparkoJQuittnerALTeam CILanguage and behavioral outcomes in children with developmental disabilities using cochlear implantsOtol Neurotol201233575122699986
- RobertsonJChildren with cochlear implants and autism – challenges and outcomes: the experience of the National Cochlear Implant Programme, IrelandCochear Implants Int201314Suppl 3S11S14
- Meinzen-DerrJWileySBishopSManning-CourtneyPChooDIMurrayDAutism spectrum disorders in 24 children who are deaf or hard of hearingInt J Pediatr Otorhinolaryngol201478111211824290951
- DonaldsonAIHeavnerKSZwolanTAMeasuring progress in children with autism spectrum disorder who have cochlear implantsArch Otolaryngol20041305666671
- American Psychiatric AssociationDiagnostic and Statistical Manual of Mental Disorders Fifth EditionWashington, DC, USAAmerican Psychiatric Association2013
- BoyleCABouletSSchieveLATrends in the prevalence of developmental disabilities in US children, 1997–2008Pediatrics201112761034104221606152
- HiraumiHYamamotoNTatsunoriSShinu YamaguchiJIThe effect of pre-operative developmental delays on the speech perception of children with CIsAuris Nasus Larynx201340323522727355
- AmirsalariSYousefiJRadfarSCochlear implant outcomes in children with motor developmental delayInt J Pediatr Otorhinolaryngol201276110010322100224
- HoltRFKirkKISpeech and language development in cognitively delayed children with cochlear implantsEar Hear200526213214815809541
- PymanBBlameyPLacyPClarkGDowellRThe development of speech perception in children using cochlear implants: effects of etiologic factors and delayed milestonesOtol Neurotol20002115761
- WileySMeinzen-DerrJChooDAuditory skills development among children with developmental delays and cochlear implantsAnn Otol Rhinol20081171071171818998496
- WakilNFitzpatrickEMOldsJSchrammDWhittinghamJLong-term outcome after cochlear implantation in children with additional developmental disabilitiesInt J Audiol201453958759424825367
- EdwardsLCFrostRWithamFDevelopmental delay and outcomes in paediatric cochlear implantation: implications for candidacyInt J Pediatr Otorhinolaryngol20067091593160016814874
- BeerJHarrisMSKronenbergerWGHoltRFPisoniDBAuditory skills, language development, and adaptive behavior of children with cochlear implants and additional disabilitiesInt J Audiol201251649149822509948
- BroomfieldSJBruceIAHendersonLRamsdenRTGreenKMCochlear implantation in children with syndromic deafnessInt J Pediatr Otorhinolaryngol20137781312131623773333
- BerrettiniSForliFGenoveseECochlear implantation in deaf children with associated disabilities: challenges and outcomesInt J Audiol200847419920818389416
- CupplesLChingTYCroweKOutcomes of 3-year-old children with hearing loss and different types of additional disabilitiesJ Deaf Stud Deaf Educ2014191203924150488
- DettmanSJFiketHDowellRCSpeech perception results for children using cochlear implants who have additional special needsVolta Rev20041044361392
- FilipoRBoscoEManciniPBallantyneDCochlear implants in special cases: deafness in the presence of disabilities and/or associated problemsActa Otolaryngol Suppl20045527480
- FukudaSFukushimaKMaedaYLanguage development of a multiply handicapped child after cochlear implantationInt J Pediatr Otorhinolaryngol200367662763312745156
- LeeY-MKimL-SJeongS-WKimJ-SChungS-HPerformance of children with mental retardation after cochlear implantation: speech perception, speech intelligibility, and language developmentActa Otolaryngol2010130892493420105112
- NikolopoulosTPArchboldSMWeverCCLloydHSpeech production in deaf implanted children with additional disabilities and comparison with age-equivalent implanted children without such disordersInt J Pediatr Otorhinolaryngol200872121823182818922585
- YangH-MLinC-YChenY-JWuJ-LThe auditory performance in children using cochlear implants: effects of mental functionInt J Pediatr Otorhinolaryngol20046891185118815302150
- SouthwellKEBirdPAMurrayDCochlear implantation in children with CHARGE syndromeCochear Implants Int2010113170183
- BlakeKDHartshorneTSLawandCDailorANThelinJWCranial nerve manifestations in CHARGE syndromeAm J Med Genet20081465585592
- RaqbiFLe BihanCDureauPLyonnetSAbadieVEarly prognostic factors for intellectual outcome in CHARGE syndromeDev Med Child Neurol200345748348812828403
- BauerPWWippoldFJIIGoldinJLuskRPCochlear implantation in children with CHARGE associationArch Otolaryngol2002128910131017
- RicciGTrabalziniFFaralliMD’AscanioLCristiCMoliniECochlear implantation in children with” CHARGE syndrome”: surgical options and outcomesEur Arch Otorhinolaryngol2014271348949323525650
- LansonBGGreenJERolandJTLalwaniAKWaltzmanSBCochlear implantation in children with CHARGE syndrome: therapeutic decisions and outcomesLaryngoscope200711771260126617507827
- AhnJHLeeK-SOutcomes of cochlear implantation in children with CHARGE syndromeActa Otolaryngol2013133111148115324125186
- AuDKHuiYTsangAWWeiWIENT management of a child with CHARGE associationAsian J Surg200427214114315140668
- MacArdleBBaileyCPhelpsPBradleyJBrownTWheelerACochlear implants in children with craniofacial syndromes: assessment and outcomesInt J Audiol200241634735612353607
- Centers for Disease ControlCerebral palsy2015 Available from: http://www.cdc.gov/ncbddd/cp/facts.htmlAccessed Jan 2015
- OddingERoebroeckMEStamHJThe epidemiology of cerebral palsy: incidence, impairments and risk factorsDisabil Rehabil200628418319116467053
- AshwalSRussmanBBlascoPPractice parameter: diagnostic assessment of the child with cerebral palsy. Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology SocietyNeurology200462685186315037681
- ByunHMoonIJKimEYPerformance after timely cochlear implantation in prelingually deaf children with cerebral palsyInt J Pediatr Otorhinolaryngol20137761013101823639338
- StevenRAGreenKMBroomfieldSJHendersonLARamsdenRTBruceIACochlear implantation in children with cerebral palsyInt J Pediatr Otorhinolaryngol201175111427143021893352
- BacciuAPasanisiEVincentiVCochlear implantation in children with cerebral palsy. A preliminary reportInt J Pediatr Otorhinolaryngol200973571772119201488
- MarscharkMRhotenCFabichMEffects of cochlear implants on children’s reading and academic achievementJ Deaf Stud Deaf Educ200712326928217526867
- IsaacsonJEHasenstabMSWohlDLWilliamsGHLearning disability in children with postmeningitic cochlear implantsArch Otolaryngol19961229929936
- DaneshiAHassanzadehSCochlear implantation in prelingually deaf persons with additional disabilityJ Laryngol Otol20071210763563817147840
- WaltzmanSBScalchunesVCohenNLPerformance of multiply handicapped children using cochlear implantsOtol Neurotol2000213329335
- WileySChooDMeinzen-DerrJHilbertLGreinwaldJGJB2 mutations and additional disabilities in a pediatric cochlear implant populationInt J Pediatr Otorhinolaryngol200670349350016154643
- WileySJahnkeMMeinzen-DerrJChooDPerceived qualitative benefits of cochlear implants in children with multi-handicapsInt J Pediatr Otorhinolaryngol200569679179815885331
- HamzaviJBaumgartnerWDEgelierlerBFranzPSchenkBGstoettnerWFollow up of cochlear implanted handicapped childrenInt J Pediatr Otorhinolaryngol200056316917411137590
- LiuXZAngeliSIRajputKCochlear implantation in individuals with Usher type 1 syndromeInt J Pediatr Otorhinolaryngol200872684184718395802
- SadeghiMKimberlingWTranebjoergLMöllerCThe prevalence of Usher syndrome in Sweden: a nationwide epidemiological and clinical surveyAudiol Med200424220228
- DammeyerJChildren with Usher syndrome: mental and behavioral disordersBehav Brain Funct201281690819088
- HenricsonCWassMLidestamBMöllerCLyxellBCognitive skills in children with Usher syndrome type 1 and cochlear implantsInt J Pediatr Otorhinolaryngol201276101449145722795738
- JatanaKRThomasDWeberLMetsMBSilvermanJBYoungNMUsher syndrome: characteristics and outcomes of pediatric cochlear implant recipientsOtol Neurotol201334348448923442567
- PenningsRJDamenGWSnikAFHoefslootLCremersCWMylanusEAAudiologic performance and benefit of cochlear implantation in Usher syndrome type ILaryngoscope2006116571772216652077
- DamenGWPenningsRJSnikAFMylanusEAQuality of life and cochlear implantation in Usher syndrome type ILaryngoscope2006116572372816652078
- National Institute of HealthWaardenburg syndrome2015 Available from: http://ghr.nlm.nih.gov/condition/waardenburg-syndromeAccessed Janurary 29, 2015
- De SaxeMKrombergJJenkinsTWaardenburg syndrome in South Africa. Part I. An evaluation of the clinical findings in 11 familiesS Afr Med J19846672562616463802
- ReadAPNewtonVEWaardenburg syndromeJ Med Genet19973486566659279758
- LiuXZNewtonVEReadAPWaardenburg syndrome type II: phenotypic findings and diagnostic criteriaAm J Med Genet1995551951007702105
- OysuCBasererNTinazMAudiometric manifestations of Waardenburg’s syndromeEar Nose Throat J200079970470911011489
- CullenRDZdanskiCRoushPCochlear implants in Waardenburg syndromeLaryngoscope200611671273127516826074
- KobleJMaking connections between genes and diseases Available from: http://www.cdc.gov/excite/ScienceAmbassador/ambassador_pgm/lessonplans_genetics.htmAccessed April 11, 2015
- KontorinisGLenarzTGiourgasADurisinMLesinski-SchiedatAOutcomes and special considerations of cochlear implantation in Waardenburg syndromeOtol Neurotol201132695195521512421
- PauHGibsonWPCochlear implantations in children with Waardenburg syndrome: an electrophysiological and psychophysical reviewCochear Implants Int200674202206
- SugiiAIwakiTTakahashiYCochlear implant in a young child with Waardenburg syndromeAdv Otorhinolaryngol2004200057215219
- AmirsalariSAjallouyeanMSaburiAAbedMGhazaviYCochlear implantation outcomes in children with Waardenburg syndromeEur Arch Otorhinolaryngol2012269102179218322159916
- de Sousa AndradeSMMonteiroARMartinsJHCochlear implant rehabilitation outcomes in Waardenburg syndrome childrenInt J Pediatr Otorhinolaryngol20127691375137822784507
- DaneshiAHassanzadehSFarhadiMCochlear implantation in children with Waardenburg syndromeJ Laryngol Otol20051190971972316156914
- DekaRCSikkaKChaturvedyGCochlear implantation in Waardenburg syndrome: the Indian scenarioActa Otolaryngol2010130101097110020443755
- MigirovLHenkinYHildesheimerMMuchnikCKronenbergJCochlear implantation in Waardenburg’s syndromeActa Otolaryngol2005125771371716012032
- RajputKBrownTBamiouD-EAetiology of hearing loss and other related factors versus language outcome after cochlear implantation in childrenInt J Pediatr Otorhinolaryngol200367549750412697351
- BeauchaineTPHinshawSPPangKLComorbidity of attention deficit/hyperactivity disorder and early-onset conduct disorder: biological, environmental, and developmental mechanismsClin Psychol2010174327336
- BakerBLNeeceCLFenningRMCrnicKABlacherJMental disorders in five-year-old children with or without developmental delay: focus on ADHDJ Clin Child Adolesc Psychol201039449250520589561
- DyeMWHauserPCBavelierDVisual attention in deaf children and adultsMarscharkMHauserPCDeaf Cognition: Foundations and OutcomesOxford University PressNew York, NY, USA2008
- Moreno-TorresITorresSSantanaRLexical and grammatical development in a child with cochlear implant and attention deficit: a case studyClin Linguist Phon201024970672120645855
- PundirMNagarkarANPandaNKIntervention strategies in children with cochlear implants having attention deficit hyperactivity disorderInt J Pediatr Otorhinolaryngol200771698598817391776
- QuittnerALBarkerDHCruzIParenting stress among parents of deaf and hearing children: associations with language delays and behavior problemsParent Sci Pract201010213615520607098
- QuittnerALCejasIBarkerDHHoffmanMFEffects of cochlear implants on young, deaf children’s development: longitudinal analysis of behavioral regulation, attention and parenting in a national sampleKirwinSHCochlear Implants: Technological Advances, Psychological/Social Impacts and Long-Term Effectiveness1Hauppauge, NY, USANova Science2014
- AbidinRRParenting Stress Index (PSI)Charlottesville, VA, USAPediatric Psychology Press1990
- QuittnerALSteckJTRouillerRLCochlear implants in children: a study of parental stress and adjustmentOtol Neurotol199112Suppl95104
- No authors listedChild care and mother-child interaction in the first 3 years of life. National Institute of Child Health and Development Early Child Care Research NetworkDev Psychol19993561399141310563730
- No authors listedThe relation of child care to cognitive and language development. National Institute of Child Health Human Development Early Child Care Research NetworkChild Dev200071496098011016559
- QuittnerALCruzIBarkerDHEffects of maternal sensitivity and cognitive and linguistic stimulation on cochlear implant users’ language development over four yearsJ Pediatr20131622343348.e34322985723
- GeersAENicholasJGSedeyALLanguage skills of children with early cochlear implantationEar Hear200324146S58S12612480
- CruzIQuittnerALMarkerCDesJardinJLIdentification of effective strategies to promote language in deaf children with cochlear implantsChild Dev201384254355923002910
- QuittnerALBarkerDHSnellCImprovements in visual attention in deaf infants and toddlers after cochlear implantationAudiol Med200754242249
- MeseroleRLCarsonCMRileyAWAssessment of health-related quality of life 6 years after childhood cochlear implantationQual Life Res201423271973123975382
- RosenhallUNordinVSandströmMAhlsenGGillbergCAutism and hearing lossJ Autism Dev Disord1999295349357
- RoperLArnoldPMonteiroBCo-occurrence of autism and deafness diagnostic considerationsAutism20037324525314516058
- IssekutzKAGrahamJMPrasadCSmithIMBlakeKDAn epidemiological analysis of CHARGE syndrome: preliminary results from a Canadian studyAm J Med Genet20051333309317
- JohnstonMVHagbergHSex and the pathogenesis of cerebral palsyDev Med Child Neurol2007491747817209983
- National Institute on Deafness and Other Communication DisordersUsher syndrome2008 Available from: http://www.nidcd.nih.gov/health/hearing/pages/usher.aspx/Accessed March 23, 2015
- National Eye InstituteWhat is Usher syndrome2015 Available from: http://www.ushersyndrome.nih.gov/whatis/fulltext.htmlAccessed March 23, 2015
- HaymanCDFranckKHCochlear implant candidacy in children with autismSemin Hear2005264217225
- BeersANMcBoyleMKakandeEDar SantosRCKozakFKAutism and peripheral hearing loss: A systematic reviewInt J Pediatr Otorhinolaryngol20147819610124300947
- FitzpatrickEMLambertLWhittinghamJLeblancEExamination of characteristics and management of children with hearing loss and autism spectrum disordersInt J Audiol201453957758624832530
- EzeNOfoEJiangDO’ConnorAFSystematic review of cochlear implantation in children with developmental disabilityOtol Neurotol20133481385139324005167
- Meinzen-DerrJWileySGretherSChooDILanguage performance in children with cochlear implants and additional disabilitiesLaryngoscope2010120240541319950380
- MacArdleBBaileyCPhelpsPBradleyJBrownTWheelerACochlear implants in children with craniofacial syndromes: Assessment and outcomesInt J Audiol200241634735612353607
- BuchmanCACopelandBJYuKKBrownCJCarrascoVNPillsburyHCCochlear implantation in children with congenital inner ear malformationsLaryngoscope2004114230931614755210
- CardosoCCMenesesMSdSilvaIMdCAlvesAMVSCochlear implants in children diagnosed with CHARGE syndromeArch Otorhinolaryngol2013174424428
- IsaacsonJEHasenstabMSWohlDLWilliamsGHLearning disability in children with postmeningitic cochlear implantsArch Otolaryngol Head Neck Surg199612299299368797555
- HinderlinkJBrokxJMensLVan den BroekPResults from four cochlear implant patients with Usher’s syndromeAnn Otol Rhinol Laryngol19941032852938154770
- JenisonVWCochlear implantation of two siblings with Usher syndrome – case studiesSeminars in Hearing1995163240245
- BirmanCSElliottEJGibsonWPPediatric cochlear implants: Additional disabilities prevalence, risk factors, and effect on language outcomesOtol Neurotol20123381347135222975903
- WileySMeinzen-DerrJGretherSChooDIHughesMLLongitudinal functional performance among children with cochlear implants and disabilities: a prospective study using the pediatric evaluation of disability inventoryInt J Pediatr Otorhinolaryngol201276569369722381362
- JaneschikSTeschendorfMBagusHArweiler-HarbeckDInfluence of etiologic factors on speech perception of cochlear-implanted childrenCochear Implants Int2013144190199

