Abstract
Background
Adhering to weight loss interventions is difficult for many people. The majority of those who are overweight or obese and attempt to lose weight are simply not successful. The objectives of this study were 1) to quantify overall adherence rates for various weight loss interventions and 2) to provide pooled estimates for factors associated with improved adherence to weight loss interventions.
Methods
We performed a systematic literature review and meta-analysis of all studies published between January 2004 and August 2015 that reviewed weight loss intervention adherence.
Results
After applying inclusion and exclusion criteria and checking the methodological quality, 27 studies were included in the meta-analysis. The overall adherence rate was 60.5% (95% confidence interval [CI] 53.6–67.2). The following three main variables were found to impact adherence: 1) supervised attendance programs had higher adherence rates than those with no supervision (rate ratio [RR] 1.65; 95% CI 1.54–1.77); 2) interventions that offered social support had higher adherence than those without social support (RR 1.29; 95% CI 1.24–1.34); and 3) dietary intervention alone had higher adherence than exercise programs alone (RR 1.27; 95% CI 1.19–1.35).
Conclusion
A substantial proportion of people do not adhere to weight loss interventions. Programs supervising attendance, offering social support, and focusing on dietary modification have better adherence than interventions not supervising attendance, not offering social support, and focusing exclusively on exercise.
Introduction
Obesity is a common chronic condition that increases the risk of numerous health problems, including cardiovascular diseases, diabetes, cancer, and mental health issues.Citation1 Substantial weight loss is not required to start to see health benefits. For example, a 5% reduction in body weight is enough to improve health outcomes.Citation1 According to data from the 1998 National Health Interview Survey, 50% of obese men and 58% of obese women in the US are actively trying to lose weight.Citation2 Regrettably, despite the efforts of a large portion of the population, the prevalence of obesity has remained high.Citation3
It is especially difficult to lose weight among those suffering from obesity, as it is a complex condition created by diverse genetic, environmental, cultural, and socioeconomic pathways. For example, a recent study concluded that the chances of returning to a normal weight for someone who is already obese are extremely low: one in 210 chances for men and one in 124 chances for women.Citation4 According to the National Health Interview Study mentioned earlier, the most commonly reported weight loss methods are as follows: 1) calorie restriction alone, 2) eating less fat, and 3) exercising more.Citation2
All of that said, moderate weight loss for health reasons is possible, even among those who are obese. For example, a study of 4,034 obese adults in the US found that 40% lost >5% of their body weight in the past year and 20% lost >10%.Citation5 However, participants need to adhere to evidence-based weight loss methods to lose weight and maintain weight loss in the long term. A meta-analysis of 18 randomized controlled trials (RCTs) found that diet and exercise programs combined were clearly superior to diet programs alone or exercise programs alone.Citation6 A meta-analysis of 29 studies looking at long-term (5 years) weight loss maintenance among those who participated in structured weight loss programs, found that the average individual maintained at least 3 kg of weight loss and at least a 3% reduction of initial body weight. The authors found that those who lost more weight prior to starting the programs were more likely to keep weight off and those who exercised more were able to better maintain their weight loss than those who did not.Citation7
Adhering to healthy weight loss behaviors is required for weight loss initially and in the long term. If participants are unable to adhere to weight loss strategies, they will not lose weight. Problems with attrition and nonadherence exist for intervention programs that are often evaluated in the short term. For example, a meta-analysis of 80 studies on weight loss interventions with a control group found a mean attrition rate of 31%.Citation8 In a meta-analysis of 45 RCTs of nonsurgical weight loss interventions in obese adults, it was found that 28.4% of participants dropped out of the study prior to the maintenance phase and that many of these dropouts were due to not meeting adherence criteria or weight loss criteria during the study phase.Citation9
An important part of advancing weight loss interventions is to understand how to improve adherence to weight loss behaviors. In any health behavior, nonadherence is a problem. The World Health Organization has identified nonadherence as a problem, “of striking magnitude”.Citation10 Behavior change is complex, and even in life-threatening situations, it is difficult for people to adhere to medical advice. For example, a report from Statistics Canada found that among smokers with new diagnoses of chronic diseases: 75% of patients with a recent diagnosis of heart disease, 78% of those with a new cancer diagnosis, 74% of those with stroke, and 96% of those with respiratory disease did not quit smoking.Citation11 Concerning weight-related health risks, more optimistic results have been reported about behavioral changes. For example, a study of 600 participants with a new diagnosis of type II diabetes found that only 20 people were able to change all their cardiovascular disease risk behaviors within 1 year, but many were able to decrease their Body Mass Index (BMI) and decrease their total daily calorie intake.Citation12
In regard to weight loss interventions among those with obesity, there have been no meta-analyses investigating factors that improve adherence rates. The objective of this review and meta-analysis was to quantify adherence rates for various weight loss intervention types and to provide pooled estimates for factors associated with improved adherence to weight loss interventions.
Methods
A systematic literature review was performed, accessing the following databases: Medline, PubMed, ProQuest, CINAHL, Cochrane Central, Global Health, ISI Web of Knowledge, ProQuest, SCOPUS, and EMBASE. Search dates ranged from January 2004 to August 2015.
Subject search descriptors included terms listed in . Search terms included relevant weight loss or reduction interventions and adherence or behavior modification (Supplementary material). Adherence was defined as completion of the weight loss program or, in certain cases, was assessed by the level of consistency with the weight loss intervention of interest. Reference sections of each article were reviewed for additional articles. Unpublished articles were not included in our search.
The following inclusion criteria were used in the search:
Article should clearly describe adherence to a weight loss program, and the said program should be neither pharmacological nor surgical.
Article should have quantifiable data describing the effect size (ie, some absolute or relative measure of program adherence).
Article should describe a study that is prospective in nature (ie, an RCT, a quasiexperimental, or a cohort study).
Article should be publicly available.
Article should be published in the English language.
The search strategies excluded opinion articles, letters to the editor, case reports, and case studies.
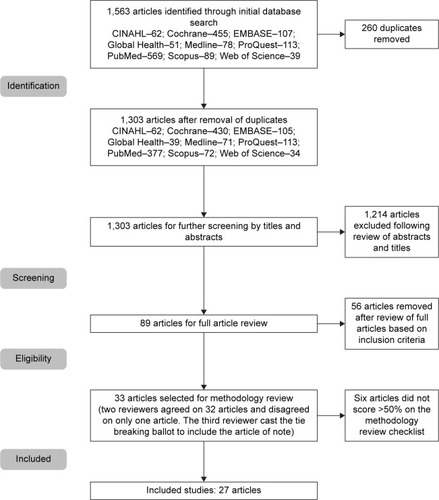
Titles were initially reviewed for relevance and to remove duplication. The articles that remained were then subjected to full abstract review in order to apply inclusion and exclusion criteria. Finally, the remaining articles were subjected to full review and methodological quality evaluation by a panel of two reviewers (CN and ML). Unanimous agreement was sought; however, when there was disagreement, a tie breaker was used with a third author (JM).
We used methodological quality checklists for experimental and quasiexperimental designs from Greenhalgh et al.Citation13 These checklists are a validated modification of the Cochrane Effective Practice and Organization of Care checklist and contain ten questions covering six areas of methodological rigor (eleven questions for quasiexperimental designs). The lists made provisions for assessing bias with the different study designs. A score of six was required in order to be accepted for review (ie, a score >50%).Citation14,Citation15 The checklists are presented in and .
Table 1 Methodology checklist for experimental designs
Table 2 Quasiexperimental designs
A computer program that utilized a random effects model, taken from Fleiss,Citation16 was built to take interstudy heterogeneity into account. The statistical basis and its assumptions have been previously described in detail elsewhere.Citation17–Citation19 At least four articles were required for statistical pooling.
Results
Systematic review
The initial search generated 1,563 articles of which 260 articles were duplicates and removed, leaving 1,303 articles to screen abstracts. After the initial screening, 89 articles were included in the full review with 56 articles removed based on the inclusion/exclusion criteria. The remaining 33 articles were then subjected to full methodological review by two reviewers. There was disagreement on only one article that was included based on tie-breaking vote from a third reviewer. In total, six of the articles did not meet methodological requirements, leaving 27 articles for meta-analysis. depicts the search process. Studies included in the analysis and their detailed results are presented in .Citation20–Citation46
Table 3 Included studies in meta-analysis
Operationalizing adherence
Intervention adherence ranged significantly from 10%Citation20 to 99.5%.Citation29 Adherence was operationalized in 13 studies, where threshold rates were given to determine adherence to particular intervention behaviors.Citation20,Citation22–Citation24,Citation29–Citation32,Citation34,Citation35,Citation37,Citation38,Citation43
Study design
Twenty of the articles were RCTs with 5,576 participants (ranging from 34 to 2,503). The remaining seven articles were observational intervention studies with 1,227 participants (ranging from 29 to 481), for a total of 6,803 participants included in the overall analysis. Among RCTs, the mean adherence was 63.1%, while the mean adherence for the observational intervention studies was 59.6%.
Study length of time and adherence
The duration of nine of the studies was 12 months, with a sample size of 3,831 participants.Citation20,Citation21,Citation31,Citation33,Citation37,Citation38,Citation40,Citation44,Citation46 The duration of 13 studies was <12 months with a sample size of 1,631 participants,Citation22,Citation23,Citation25,Citation27–Citation30,Citation32,Citation35,Citation36,Citation39,Citation41,Citation42 and the duration of five studies was ≥18 months with a sample size of 1,341 participantsCitation24,Citation26,Citation34,Citation43,Citation45 (no articles had study durations between 12 months and 18 months). Interventions lasting <12 months had a mean adherence rate of 69.9%, while those lasting ≥12 months had a mean adherence rate of 53.0%.
Factors that affect adherence
Only ten of the 27 studies discussed factors that affected adherence.Citation23,Citation27,Citation28,Citation30,Citation34–Citation37,Citation40,Citation45 One studyCitation23 found associations between higher adherence and older age, higher income, and higher education. Older age was also associated with better adherence in two other studies,Citation30,Citation40 and increasing education levels were associated with higher adherence in two other studies.Citation35,Citation40 Social support contracts increased adherence rates in two studiesCitation27,Citation35 and six studies in total, including a social support aspect to the intervention.Citation27,Citation32,Citation35,Citation36,Citation41,Citation43
Six studies discussed factors associated with lower adherence.Citation23,Citation28,Citation30,Citation34,Citation35,Citation37 These included lower socioeconomic status (education and income),Citation23,Citation35 higher weight,Citation28,Citation30 poor health,Citation28 dissatisfaction with the program or weight loss results,Citation34,Citation37 smoking status,Citation34 and depressed mood.Citation35
Subgroup analysis
Subgroup analysis is presented in . Interventions with a duration of <12 months had higher adherence rates than interventions lasting ≥12 months (RR 1.32; 95% CI 1.28–1.36). Those interventions that included social support improved adherence rates by 29% compared to those interventions that did not include social support (95% CI 1.24–1.34).
Table 4 Adherence rate and rate ratio for multifactor subgroup analysis across baseline body mass index, study duration, incentive, social support, age, study design, and intervention type
Self-monitoring programs had the lowest adherence rate (41.5%), and supervised interventions had the highest adherence rate (68.6%). When attendance was monitored (supervised) by a researcher or intervention leader, participants were more adherent compared to programs that used self-monitoring interventions (RR 1.65; 95% CI 1.54–1.77), diet interventions, or physical activity interventions without supervision or attendance tracking. Participants were more adherent to diet interventions alone than exercise interventions alone (RR 1.27; 95% CI 1.19–1.35) or self-monitoring interventions (RR 1.54; 95% CI 1.43–1.65).
Interpretation
It is not possible to lose weight without actually adhering to weight loss protocols, such as exercise and dietary interventions. In weight loss interventions, nonadherence rates are usually high. In this article, we have included studies with interventions using methods, such as education, self-monitoring (electronic or nonelectronic), group-based or individual exercise or diet interventions, peer support, and lifestyle interventions, which included both diet and exercise. For many studies, adherence rates were low; as low as 10% in a 12-month study.Citation20 Different intervention strategies reported various adherence rates within different study designs. We performed a pooled subgroup analysis to determine intervention characteristics that increase the likelihood of participant adherence.
High adherence rates were observed for interventions that incorporated aspects of social support. Social support is an important determinant in overall health. The Public Health Agency of Canada has listed social support as the second most important determinant of health,Citation47 and the results from a number of studies indicate that those with social supports in place even have a reduced risk of premature mortality.Citation48–Citation50
Social support in the studies reviewed in this article ranged from group sessions to peer coaches to social support contracts to “buddy” programs. In the existing literature, multiple studies have indicated that social support (whether through family, friends, peers, or providers) is important for successful behavioral change. For example, one study found that those who received guided support for weight loss were 37% more likely to maintain weight loss than those who participated in self-directed strategies.Citation51
Participation in weight loss interventions that allow friends or family to participate may have important implications for weight loss and weight loss maintenance. A previous study compared a weight loss intervention in which participants attended alone, with three friends, or with family members and found that at 6-month follow-up, those who attended with family or friends were more likely to maintain weight loss after program completion than those who attended alone.Citation52 Social support contracts also allow ongoing support outside of the program. These contracts can help maintain a stronger commitment to a weight loss plan and have been shown to also improve rates of weight loss when compared to those who try to lose weight on their own.Citation53 As such, it is important to incorporate aspects of social support into weight loss interventions and to provide social support when participants have none. Utilizing existing social networks may be one way to do this, while using existing technology to deliver social support via the web or smartphones is another. These social tools may also act as a motivational tool for participants to remain engaged in the weight loss intervention.Citation54
Our analysis also determined that programs supervising and monitoring attendance improved adherence rates by 65% compared to self-monitoring programs and had the highest adherence rates overall. Monitoring attendance likely improves adherence rates since participants are more accountable for their behaviors. Supervision has been found to increase physical activity intervention adherence in other conditions. For example, a mixed methodology study on adherence to a physical activity program in patients with chronic obstructive pulmonary disorder found that participants felt that they would not be able to maintain the behaviors if not for the group dynamic of the classes and the required reporting to the physiotherapist.Citation55
Supervised programs also allow participants to access health-care provider knowledge and feedback. Working without guidance can be discouraging and, at times, dangerous. Increasing knowledge transfer through access to an expert supervisor may help improve self-efficacy.Citation56 Furthermore, a good relationship between supervisors and participants can increase adherence to additional health advice.Citation56
Better adherence was also seen when comparing randomized with nonrandomized studies. This result has been observed in other health intervention studies, including a meta-analysis on adherence to statin therapy, where 90% of patients in RCTs were adherent to statin therapy, while only 49% were adherent in observational studies.Citation57 This may be attributed in large part to the structured and specific nature of the inclusion and exclusion criteria used in RCTs. As such, participants in RCTs tend to be “less sick, younger, better educated, and of higher socioeconomic status”.Citation58 It has been estimated that the average RCT excludes 90% of patients.Citation59 There are other key differences in RCTs when compared to observational studies that could improve adherence, including differences in patient populations, different intervention intensities or therapeutic regimens, control of confounding factors, potentially more rigorous follow-up, among others.Citation60 Additionally, due to the funding structure of RCTs and their need to evaluate efficacy instead of real-world effectiveness, these studies tend to be more heavily supervised. As such, the finding that randomized trials have higher adherence than observational studies is likely due to supervised programming and the recruitment of more “ideal” participants. For those offering clinical weight loss interventions, it is important to have participants engage in activities in which they are held accountable for their attendance or adherence to a group, a care provider, or a social support individual.
We also found better adherence to dietary interventions alone than exercise interventions alone. This could be due to a number of reasons. First, in cases where diet adherence was captured via self-report, poor recall or false information could be a possibility.Citation61 Second, it may be due in part to participants seeing more weight loss from restrictive diets than from exercise interventions, which is supported by the literature.Citation6,Citation62 However, it has been previously stated that dietary and exercise programming needs to be combined in order to be most effective.Citation6,Citation62 Physical activity is important to overall health and overall weight loss maintenanceCitation63 and should be encouraged as a part of a weight loss intervention along with dietary change.
Financial incentives for weight loss programs are discussed throughout the literature, and four studies were included in our analysis.Citation23,Citation32,Citation38,Citation39 However, when comparing interventions that utilized financial incentives with those studies that did not, there were no significant differences in adherence rates. Among the studies using financial incentives, the participant pool was among the smallest in our analysis.
Future research
Weight loss intervention studies targeting obese individuals should take into account and measure factors that predict adherence. Few studies were found in this systematic review that had acceptable methodological rigor. Given the high prevalence of obesity and the importance of adherence in order to lose weight and maintain weight loss, this is an important area to continue to study.
Study limitations
Due to the variability between studies, the pooling of data, while helpful in increasing the sample size, does introduce a level of uncertainty, with regard to the study conclusion due to possible sampling errors or unmeasured covariates. Also, there were only ten studies in which the authors set out to measure factors that predict adherence to weight loss programs. Therefore, it is possible that the remaining studies may not have given proper consideration to potential con-founders for adherence or made the necessary adjustment as needed.
Conclusion
It is unlikely that there is a single solution to reverse the rising prevalence of obesity observed globally. A comprehensive approach is needed to address this complex issue. Supervising weight loss programs and adding social supports help improve adherence to weight loss programs. It is expected that with better adherence, overweight or obese persons can lose more weight and help keep it off in the long term. Evaluating the views of participants and adherence rates to weight loss programs is critical as it can offer insight, expand our current knowledge, and provide evidence in support of designing and implementing more effective interventions.
Supplementary materials
Search terms
Weight loss programs
Weight loss intervention
Weight loss regimen
Weight loss plan
Weight reduction programs
Weight reduction intervention
Weight reduction regimen
Weight reduction plan
Adherence
Behavior modification
Search strategy
(((((((((Weight loss programs) OR weight loss intervention) OR weight loss regimen) OR weight loss plan) OR weight reduction programs) OR weight reduction intervention) OR weight reduction regimen) OR weight reduction plan)) AND ((adherence) OR “behavior modification”).
Databases searched
Medline
PubMed
Cochrane Library
CINAHL
Global Health
ISI Web of Knowledge
ProQuest
SCOPUS
EMBASE
Inclusion criteria
Article should be in English language.
Article should have a prospective design.
Article should have quantifiable data describing the effect size.
Article should describe participation in a supervised weight loss program that is neither pharmacologic nor surgical and assess adherence to the said program.
Article is publicly available.
Disclosure
The authors report no conflicts of interest in this work.
References
- National Institutes of HealthClinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence ReportBethesda, MDNational Institutes of Health1998 NIH Publication No. 98-4083
- KrugerJGaluskDASerdulaMKJonesDAAttempting to lose weight: specific practices among U.S. adultsAm J Prev Med200426540240615165656
- OgdenCLCarrollMDKitBKFlegalKMPrevalence of childhood and adult obesity in the United States, 2011–2012JAMA2014311880681424570244
- FildesACharltonJRudisillCLittlejohnsTGullifordMCPrevostATProbability of an obese person attaining normal body weight: cohort study using electronic health recordsAm J Pub Health20151059e54e5926180980
- NicklasJMHuskeyKDavisRBWeeCCSuccessful weight loss among obese U.S. adultsAm J Prev Med201242548148522516488
- WuTGaoXChenMvan DamRMLong-term effectiveness of diet-plus-exercise interventions vs diet-only interventions for weight loss: a meta-analysisObes Rev200910331332319175510
- AndersonJWKonzECFrederichRCWoodCLLong-term weight-loss maintenance: a meta-analysis of US studiesAm J Clin Nutr200174557958411684524
- FranzMJvan WormerJJCrainALWeight-loss outcomes: systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-upJ Am Diet Assoc2007107101755176717904936
- DombrowskiSUKnittleKAvenellAAraujo-SoaresVSniehottaFFLong-term maintenance of weight loss with non-surgical interventions in obese adults: systematic review and meta-analyses of randomised controlled trialsBMJ2014348g264625134100
- World Health Organization [webpage on the Internet]Adherence to Long-Term Therapies. Evidence for ActionGenevaWorld Health Organization2003 Available from: http://whqlibdoc.who.int/publications/2003/9241545992.pdfAccessed April 22, 2016
- Statistics Canada [webpage on the Internet]Health Behaviour Changes After Diagnosis of Chronic Illness Among Canadians Aged 50 or Olde; 2012) Available from: http://www.statcan.gc.ca/pub/82-003-x/2012004/article/11740-eng.pdfAccessed April 22, 2016
- LongGHCooperAJMWarehamNJGriffinSJSimmonsRKHealthy behavior change and cardiovascular outcomes in newly diagnosed Type 2 diabetic patients: a cohort analysis of the ADDITION-Cambridge studyDiabetes Care20143761712172024658389
- GreenhalghTRobertGBatePDiffusion of Innovations in Health Service Organizations: A Systematic Literature ReviewMalden, MABlackwell Publishing Ltd2005
- LemstraMAlsabbaghMWProportion and risk indicators of nonadherence to antihypertensive therapy: a meta-analysisPatient Prefer Adherence2014821121824611002
- AlsabbaghWLemstraMEurichD webpage on the InternetSocioeconomic Status and Non Adherence to Anti-Hypertensive Drugs: A Systematic Review and Meta-AnalysisValue in Health2014 Available from: http://www.ispor.org/publications/value/articlesin-press.aspAccessed April 22, 2016
- FleissJLThe statistical basis of meta-analysisStat Methods Med Res1993221211458261254
- LemstraMBennettNNeudorfCA meta-analysis of school based marijuana and alcohol prevention programs in targeting adolescents aged 10–15 years oldAddict Res Theory20101818496
- LemstraMBennettNNeudorfCA systematic review of drug and alcohol use by socioeconomic status in adolescents aged 10–15 yearsCan J Pub Health200899317217718615935
- LemstraMNeudorfCD’ArcyCKunstAWarrenLBennettNA systematic review of depressed mood and anxiety by socioeconomic status in adolescents aged 10–15 yearsCan J Pub Health200899212512918457287
- AcharyaSElciOSereikaSAdherence to a behavioral weight loss treatment program enhances weight loss and improvements in biomarkersPatient Prefer Adherence2009315116019936157
- AnnunziatoRTimkoCCrerandCA randomized trial examining differential meal replacement adherence in a weight loss maintenance program after one-year follow-upEat Behav200910317618319665101
- ArdJKumanyikaSStevensVEffect of group racial composition on weight loss in African AmericansObesity200816230631018239637
- AustinJSmithJGianiniLCampos-MeladyMAttitudinal familism predicts weight management adherence in Mexican American womenJ Behav Med201336325926922487966
- BartfieldJStevensVJeromeGBehavioral transitions and weight change patterns within the PREMIER TrialObesity20111981609161521455122
- BefortCNollenNEllerbeckESullivanDThomasJAhluwaliaJMotivational interviewing fails to improve outcomes of a behavioral weight loss program for obese African American women: a pilot randomized trialJ Behav Med200831536737718587639
- BurkeLStynMGlanzKSMART trial: a randomized clinical trial of self-monitoring in behavioral weight management-design and baseline findingsContemp Clin Trials200930654055119665588
- CarsonTEddingsKKrukowskiRLoveSHarvey-BerinoJWestDExamining social influence on participation and outcomes among a network of behavioral weight-loss intervention enrolleesJ Obes2013201318
- CarterMBurleyVNykjaerCCadeJAdherence to a smart-phone application for weight loss compared to website and paper diary: pilot randomized controlled trialJ Med Internet Res2013154e3223587561
- ChurchTMartinCThompsonAEarnestCMikusCBlairSChanges in weight, waist circumference and compensatory responses with different doses of exercise among sedentary, overweight postmenopausal womenPLoS One200942e451519223984
- ColleyRHillsAO’Moore-SullivanTHickmanIPrinsJByrneNVariability in adherence to an unsupervised exercise prescription in obese womenInt J Obes Relat Metab Disord2008325837844
- DasSSaltzmanEGilhoolyCLow or moderate dietary energy restriction for long-term weight loss: what works best?Obesity200917112019202419390525
- DuttonGPhillipsJKukkamallaMCherringtonASaffordMPilot study evaluating the feasibility and initial outcomes of a primary care weight loss intervention with peer coachesDiabetes Educ201541336136825740817
- DuttonGNackersLDubyakPA randomized trial comparing weight loss treatment delivered in large versus small groupsInt J Behav Nutr Phys Act201411112325249056
- GreenbergIStampferMSchwarzfuchsDShaiIDIRECT GroupAdherence and success in long-term weight loss diets: the dietary intervention randomized controlled trial (DIRECT)J Am Coll Nutr200928215916819828901
- LemstraMRogersMThe importance of community consultation and social support in adhering to an obesity reduction program: results from the Healthy Weights InitiativePatient Preference and Adherence2015991473148026508843
- McAndrewLNapolitanoMPogachLThe impact of self-monitoring of blood glucose on a behavioral weight loss intervention for patients with Type 2 diabetesDiabetes Educ201239339740522735195
- MeffertCGerdesNProgram adherence and efectiveness of a commercial nutrition program: the metabolic balance studyJ Nutr Metab2010201018
- ShapiroJKoroTDoranNText4Diet: a randomized controlled study using text messaging for weight loss behaviorsPrev Med201255541241722944150
- SteinbergDLevineEAskewSFoleyPBennettGDaily text messaging for weight control among racial and ethnic minority women: randomized controlled pilot studyJ Med Internet Res20131511e24424246427
- SteinbergDLevineELaneIAdherence to self-monitoring via interactive voice response technology in an ehealth intervention targeting weight gain prevention among Black women: randomized controlled trialJ Med Internet Res2014164e11424780934
- TheimKSintonMGoldschmidtAAdherence to behavioral targets and treatment attendance during a pediatric weight control trialObesity201321239439723532993
- TravierNFonseca-NunesAJavierreCEffect of a diet and physical activity intervention on body weight and nutritional patterns in overweight and obese breast cancer survivorsMed Oncol201431178324310809
- Turner-McGrievyGBarnardNScialliAA two-year randomized weight loss trial comparing a vegan diet to a more moderate low-fat dietObesity20071592276228117890496
- UnickJBeaversDJakicicJEffectiveness of lifestyle interventions for individuals with severe obesity and Type 2 diabetes: results from the Look AHEAD trialDiabetes Care201134102152215721836103
- van GoolCPenninxBKempenGDeterminants of high and low attendance to diet and exercise interventions among overweight and obese older adultsContemp Clin Trials200627322723716387555
- WangJSereikaSChasensEREwingLJMatthewsJTBurkeLEEffect of adherence to self-monitoring of diet and physical activity on weight loss in a technology-supported behavioral interventionPatient Prefer Adherence2012622122622536058
- Public Health Agency of Canada [webpage on the Internet]What Makes Canadians Healthy or Unhealthy? Available from: http://www.phac-aspc.gc.ca/ph-sp/determinants/determinants-eng/phpAccessed December 7, 2015
- Ben-ShlomoYSmithGDShipleyMMarmotMGMagnitude and causes of mortality differences between married and unmarried menJ Epidemiol Community Health19934732002058350032
- Holt-LunstadJSmithTBLaytonJBSocial relationships and mortality risk: a meta-analytic reviewPLoS Med201077e100031620668659
- BeasleyJMNewcombPATrentham-DietzASocial networks and survival after breast cancer diagnosisJ Cancer Surviv20104437238020652435
- BrantleyPJStewartDWMyersVHPsychosocial predictors of weight regain in the weight loss maintenance trialJ Behav Med20143761155116824722826
- WingRRJefferyRWBenefits of recruiting participants with friends and increasing social support for weight loss and maintenanceJ Consult Clin Psychol199967113213810028217
- HarrisMBBrunerCGA comparison of a self-control and a contract procedure for weight controlBehav Res Ther1971943473545149586
- Aguilar-MartinezASole-SedenoJMMancebo-MorenoGMedinaFXCarreras-ColladoRSaigi-RubioFUse of mobile phones as a tool for weight loss: a systematic reviewJ Telemed Telecare201420633934924875928
- O’SheaSDTaylorNFParatzJD…But watch out for the weather: factors affecting adherence to progressive resistance exercise for persons with COPDJ Cardiopulm Rehabil Prev200727316617417558200
- AversDWhartonMImproving exercise adherence: instructional strategiesTop Geriatr Rehabil199166273
- LemstraMBlackburnDCrawleyFFungFProportion and risk indicators of non-adherence to statin therapy: a meta-analysisCan J Cardiol201228557458022884278
- HannanELRandomized clinical trials and observational studies: guidelines for assessing respective strengths and limitationsJACC20081321121719463302
- SorensenJTLashTLRothmanKJBeyond randomized controlled trials: a critical comparison of trials with nonrandomized studiesHepatology20064451075108217058242
- TingHHSjojaniaKGMontoriVMBradleyEHQuality improvement – science and actionCirculation2009119141962197419364989
- DhurandharNVSchoellerDBrownAWEnergy balance measurement: when something is not better than nothingInt J Obes201439711091113
- MillWCKocejaDMHamiltonEJA meta-analysis of the past 25 years of weight loss research using diet, exercise, or diet plus exercise interventionInt J Obes19972110941947
- KrugerJBlanckHMGillespieCDietary and physical activity behaviors among adults successful at weight loss maintenanceInt J Behav Nutr Phys Act20063172616854220