Abstract
Background
Communication with patients with fibromyalgia syndrome (FMS) is often considered difficult. The primary objective of this explorative study was to describe the communication preferences of FMS patients in comparison with other chronic diseases, and the secondary objective was to identify patient-related predictors of those communication preferences.
Methods
A total of 256 FMS patients were asked to fill out the KOPRA [(Kommunikationspraeferenzen), communication preferences of patients with chronic illness] questionnaire at the beginning of their rehabilitation, answering questions about their communication preferences. The KOPRA’s descriptive parameters were calculated and compared with other diagnosis groups. In order to include as many influencing factors as possible, data on patient-related sociodemographic, medical, pain impact and psychologic variables were gathered. A hierarchical regression analysis with four steps was performed to identify patient-related predictors of patients’ communication preferences.
Results
FMS patients consider an open and patient-centered communication style to be especially important. Emotionally supportive communication and communication about personal circumstances are important for FMS patients, but the preferences of individual patients vary widely. FMS patients reveal higher values in all the subdimensions of communication preferences compared with patients with low back pain or chronic ischemic heart disease. Only a few variables appear to predict patient communication preferences. The explained variance ranged from 3.1% to 9.7%. Psychologic variables have been identified as predictors in conjunction with all communication preferences.
Conclusion
Health care providers who communicate with FMS patients should employ an open and patient-centered communication style, and affective communication components should be adapted to accommodate each patient.
Introduction
Ever greater research efforts are being invested in examining patient–provider communication. Communication between patients and their health care providers is now considered the “royal pathway to patient-centered medicine”,Citation1 becoming a key component in health care of the chronically ill.
Patients with noninflammatory conditions such as fibromyalgia syndrome (FMS) pose a particular challenge for their health care providers. FMS is a chronic disease characterized by widespread musculoskeletal pain, disturbed sleep, reduced mental functioning and depressed mood.Citation2 Although recent progress has been made in improving the diagnostic criteria and treatment of FMS,Citation2 providers still encounter difficulties treating patients with this condition. For many patients with FMS it is very important to get a somatic diagnosis from their health care providers, but FMS often has no identified (somatic) cause.Citation3 In a study by Perrot et al,Citation4 over half of the health care providers queried (53%) admitted to having difficulties in diagnosing FMS. There are some possible reasons for this result, eg, the disease’s still unclear etiology and pathogenesis, and an often subjective diagnosis.Citation5 Given that there are few objectively-measurable criteria for FMS, health care providers must rely on patients’ subjective descriptions of their symptoms and their impacts. Many physicians characterize FMS patients as “interactionally difficult”.Citation6 Choy et al reported that 59% of the patients with FMS in their study admitted to having trouble discussing their symptoms with their health care providers.Citation7 Reasons for this may be the diffuse nature of FMS symptoms, and negative experiences with the health care system. Five years usually pass between the first experience of pain and first diagnosis.Citation7,Citation8 Encounters between FMS patients and health care providers are often associated with patients’ feelings of disappointment, dissatisfaction and rejection.Citation9 These perceptions may be triggered by divergent subjective illness beliefs on the part of health care providers and patients.Citation3 Dissatisfaction with one provider leads to more frequent contacts with other health care providers (called “doctor shopping”),Citation7 thus incurring a higher socioeconomic burden.Citation10
A deeper understanding of the nature of the communication between the patient and provider seems very much worth pursuing. Several studies have demonstrated that therapeutic decisions made in concert with patients (shared decision-making, or SDM)Citation11 can lead to a better relationship.Citation12 Further patients cite courtesy, respect and engagement as other important aspects of successful communication between them and their health care providers.Citation13 Researchers have also reported an association between effective communication on the one hand and patient satisfaction, adherence and various health outcomes on the other.Citation14–Citation16
One factor, determining whether a provider’s communication behavior is being assessed as either positive or negative, is the patient’s communication preference.Citation17 Patient–provider communication is influenced by each patient’s interindividual and intra-individual needs and preferences in relationship to the provider’s communication style. Each patient has slightly different expectations regarding conversations with his or her provider and the extent of participation in medical decision-making. The provider could adapt his or her communication behavior to the needs of FMS patients better by possessing a deeper understanding of their communication preferences. If the health care provider can fulfill the patient’s expectations and respect his or her preferences, this may affect patient satisfaction positively.Citation18 To the best of our knowledge, no study has examined the communication preferences of patients with FMS in detail so far.
The extent to which communication preferences correlate with patient-related factors has not been unequivocally defined. Some researchers have investigated the relationship between sociodemographic, clinical, psychologic or other lifestyle variables, and patient preferences for participation (ie, an active versus a passive role).Citation19 The results show, that the probability of desiring an active role in the discussion falls significantly with increasing age and rises with increasing educational status. Sex and disease severity also influence preferences for participation. Patient-related factors only explain a minor proportion of the variance in patient preference.Citation20,Citation21 By identifying patient-related predictors, health care providers may better perceive initial indications of a patient’s communication preferences.
All these observations led us to our two explorative questions:
What communication preferences do FMS patients have, and how do they differ from patients with other chronic diseases?
Which patient-related factors predict the communication preferences of FMS patients?
Materials and methods
Sample and design
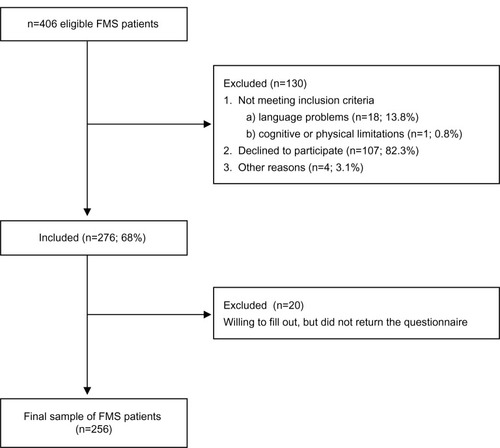
Our consecutive sample consisted of 256 patients whose primary diagnosis was fibromyalgia syndrome (International Classification of Diseases version 10: M79.7)Citation22 and who were undergoing treatment from August 2011 to July 2012 as inpatients in a German rehabilitation center (RehaKlinikum Bad Säckingen GmbH, Bad Säckingen). FMS had been diagnosed according to the 1990 American College of Rheumatology criteria.Citation23 All patients with FMS were asked to complete a questionnaire at the beginning of rehabilitation. Our patient questionnaire was given only to patients able and willing to fill out this questionnaire (informed consent). A total of n=406 eligible FMS patients were asked to participate. shows the participant flow in this study.
provides information (sociodemographic, medical, pain impact and psychologic variables) on the participants. Not surprisingly, significantly more women participated in the study than men. Population studies show that the female-to-male ratio for FMS varies between 2 – 21:1.Citation24 The study was approved by the Ethics Committee of the University of Freiburg (approval number 172/10).
Table 1 Respondent characteristics (n=256)
Instruments
We assessed sociodemographic, medical, pain impact, and psychologic variables using various patient self-report instruments. The sociodemographic variables we captured were age, sex, regular partner, highest level of education completed, employment and income. Medical variables were duration of illness and comorbidities measured using a rehabilitation-specific comorbidity score (KoMo-Score; 13 items).Citation25 The original KoMo-Score was expanded by four items. Those supplemental questions addressed the various comorbidities (and their severity) frequently associated with FMS. To assess pain impact, we used the German version of the Fibromyalgia Impact Questionnaire (FIQ), German Version (-G, 19 items). The FIQ-G is an assessment and evaluation instrument developed to measure FMS patient status, progress, and outcomes.Citation26 The psychologic variables we captured were Illness coherence ie, a belief that the illness “makes sense” (Illness Coherence scale [IPQ-COH] of the Revised Illness Perception Questionnaire, German version; five items),Citation27 depression and anxiety (both measured using the Hospital Anxiety and Depression scale [HADS], German version; 14 items),Citation28 self-efficacy expectancies concerning pain and other disease-related symptoms (Arthritis Self-Efficacy Short-Form scale [ASES], German version; eight items)Citation29 and pain acceptance (Chronic Pain Acceptance Questionnaire [CPAQ], German version; 20 items).Citation30 The CPAQ is an instrument to capture the acceptance in coping with chronic pain. For coping with pain we used a German questionnaire that addresses coping strategies (cognitive and behavioral coping) and psychologic strain through chronic pain (German Pain Coping Questionnaire [FESV], German version; 38 items).Citation31–Citation33
We administered the KOPRA [(Kommunikationspraeferenzen), communication preferences of patients with chronic illness] questionnaire to measure the communication preferences of patients.Citation34 It possesses good psychometric properties and consists of 32 items categorized in four scales. “Patient participation and patient orientation” (PPO, 11 items) measures patient communication preferences with respect to the patient’s participation in treatment and consideration of their opinions and preferences. “Effective and open communication” (EOC, ten items) measures preferences with respect to effectively collecting, conveying, and sharing information and open communication about negative events. “Emotionally supportive communication” (ESC, six items) measures preferences regarding emotionally supportive communication. “Communication about personal circumstances” (CPC, five items) measures preferences regarding a personal communication style that also includes private aspects. The PPO and EOC scales tend to focus on instrumental aspects of communication, whereas the ESC and CPC scales address affective components of communication. The KOPRA questionnaire has been used in several patient samples (low back pain,Citation17 cancer,Citation35 chronic ischemic heart diseaseCitation36), but until now, not in FMS patients.
Statistical analysis
We applied Cronbach’s alpha to test the reliability of the four KOPRA scales for FMS patients. Cronbach’s alpha should exceed 0.70.Citation37
The parameters (mean and standard deviation) for KOPRA were calculated to answer the first question of our study. We also compared these with other diagnoses. Data for other diagnosis groups come from earlier studies done by the authors using the KOPRA questionnaire.Citation17,Citation35,Citation36 In addressing the prediction of communication preferences, we first calculated bivariate correlations between the predictors and KOPRA scales. Those predictors that correlated poorly with the KOPRA scales (P>0.20) were disregarded in subsequent analyses. Missing values in the remaining predictors were imputed using NORM software.Citation38 A hierarchical regression analysis with four steps was performed. In the first block we placed sociodemographic variables, in the second all medical variables, in the third pain-impact variables and in the fourth all psychologic variables. The backward method of variable selection was employed.Citation39 A separate model was specified for each of the KOPRA scales. To diagnose multicollinearity, the variance inflation factor was calculated. Values over 5 can be considered as an indication of multicollinearity.Citation40 Statistical analyses were performed using IBM Statistical Package for the Social Sciences version 20 software (IBM Corporation, Armonk, NY, USA).
Results
Communication preferences in patients with FMS
Cronbach’s alpha for the scale “Patient participation and patient orientation” reached 0.94, the “Effective and open communication” scale 0.94, the “Emotionally supportive communication” scale 0.88, and the “Communication about personal circumstances” scale 0.87. What becomes apparent is that all the scales (in FMS patients as well) are very reliable, and that the high values resemble those associated with other diagnoses.Citation17,Citation35,Citation36
illustrates the communication preferences of FMS patients. “Effective and open communication” is most important to patients with FMS, followed by “Patient-centered communication”. The mean values for both scales lie in the upper range (answer categories, “extremely important” and “very important”). “Emotionally supportive communication” scale items were rated by the patients as “important” (the mean). Least important to patients with FMS was a personal communication style on the part of the health care provider. The averages of the mean values in this scale lie between the answers “important” and “somewhat important”.
Table 2 Mean (M) and standard deviation (SD) of KOPRA items and scales
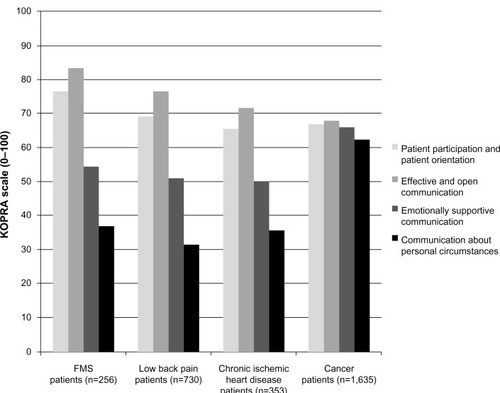
shows the means of the KOPRA scales for various diagnostic patient samples (FMS, low back pain, chronic ischemic heart disease and cancer). Means for FMS patients in the KOPRA reveal a distribution pattern similar to that found in the low back pain and chronic ischemic heart disease patient groups.Citation17,Citation36 Values for the FMS patients’ values are higher than the values of the other two groups in each of the KOPRA scales. Cancer patients show a different distribution pattern, as all their mean values range between M=62 and M=68. The four communication areas covered in the KOPRA questionnaire are similarly important to the cancer patients.Citation35
Predicting patients’ communication preferences
presents the hierarchical regression analysis results. All the variance inflation factor values fell below 1.10, so we can assume very minor multicollinearity among the predictors. Communication preferences’ explanation of variance was minor in all four models, lying between 3.1% and 9.7%.
Table 3 Results of hierarchical regression analysis
A more pronounced communication preference is only predicted by the CPAQ score on the “Patient participation and patient orientation” scale. Acceptance of chronic pain in FMS patients was negatively associated with the preference for a patient-centered style of communication.
We identified two predictors for the “Effective and open communication” scale. The preference for effective and open communication is stronger the less accepting patients are of chronic pain and the less often they implement relaxation techniques (FESV). Sociodemographic, medical or pain impact variables (blocks 1–3) did not prove to predict communication preferences in either the PPO or EOC scale.
More pronounced “Anger” (FESV) was associated with more pronounced communication preferences on the ESC scale. Moreover, having an elementary school certificate was also associated with a more pronounced preference on the “Emotionally supportive communication” scale. We identified the same two predictors to be relevant in the “Communication about personal circumstances” scale.
Discussion
Communication preferences in patients with FMS
In this study, we observed that FMS patients prefer an effective, open and patient-centered style of communication (EOC and PPO scales) with their health care providers. They also prefer an emotionally supportive communication style on the part of their provider(s) (ESC scale). On the other hand, FMS patients are less likely to prefer a very personal communication style (CPC scale). It is important to note that the standard deviation in the ESC and CPC scale is much higher compared with the other two. We can deduce that the preference for a communication style, that patients perceive as being particularly emotionally supportive, or that pays special attention to the patient’s personal situation, varies widely from individual to individual. Keeping this in mind, the health care provider should take special care to adapt his or her behavior to the patient’s individual communication preferences.Citation41
We assume that our results reflect the great need for information that patients with FMS perceive. These patients prefer to be thoroughly informed about their illness and its symptoms by their health care providers, as well as about potential therapeutic alternatives. Therefore it is essential that health care providers are well-informed about FMS and its therapy. In March 2011, a new guideline (S-3-Leitlinie)Citation42 was set up by the Working Group of the Scientific Medical Societies (Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften AWMF, 2011) in Germany, containing information about FMS. These guidelines assist in the definition, classification, diagnosis, and prognosis of the condition, provide various treatment approaches and reports on their efficacy beyond the American College of Rheumatology criteria from 1990Citation23 and 2010.Citation2
Patients consider open communication about the pros and cons associated with a therapy as important. A fundamental assumption for shared decision-making between a patient and his or her physician is an effective patient-centered communication of information about a disease and its therapy.Citation12 Many methods have been developed in recent years that improve the quality of the decisions made within a given treatment situation.Citation43 Those proven successful are methods describing interventions or the provision of educational information materials for patients and their health care providers.Citation13 To make a decision together within a dyadic consultation, health care providers and patients must possess certain skills.Citation44
Health care providers should take communication preferences of patients with FMS into account and try to create an open communicative atmosphere that enables active engagement in a consultation.Citation45 Thus, time must be set aside at the start of patient–provider communication to “capture” the patient’s individual communication preferences.Citation19 With a deeper understanding of the communication preferences of patients with FMS, health care providers can better adapt their communication behavior to these patients’ individual needs. The challenge for the health care provider is to find the time within his or her institution’s organizational and economic framework to engage in such patient–provider communication. One of the examinations addressing this topic reported that patient-centered communication is associated with less diagnostic testing expenditure.Citation46 Paying greater attention to patients’ preferences can also lead to better health outcomes via several routes. Adherence on the behavioral level and on the psychologic level, a sense of autonomy and satisfaction with decisions can be influenced by respecting patients’ preferences.Citation47
When we compare the FMS patients’ KOPRA questionnaire results with those of other diagnostic groups, it is apparent that all the FMS patients’ KOPRA scale values lie above the means of those for patients with low back pain or chronic ischemic heart disease.Citation17,Citation35 The distribution pattern of their communication preferences does not differ, but the strength of their preferences is greater than that expressed in the other diagnoses. This result is not surprising when we remember that patients in chronic pain place particular importance on sensing an acceptance and understanding of their pain during communication.Citation48 That the means in the instrumental (PPO and EOC scales) and affective dimension (ESC and CPC scales) are higher in the FMS patients highlights this group’s special position among patients suffering from chronic pain.
Cancer patients are an exception.Citation34 They score much higher on the affective dimension of communication than other diagnostic groups. Facing a life-threatening disease, cancer patients experience their illness by showing a strong tendency to feel negative emotions like fear, sadness, and anxietyCitation49 and thus usually sense a much greater need for emotional support.Citation50 We also have to take into account that the illness experienced by cancer patients might vary depending on their types of cancer.
Predicting patients’ communication preferences
Our results are similar to those obtained in other studies identifying patient-related predictors of patient communication preferences.Citation20,Citation21 Few patient-related factors predict the communication preferences of FMS patients. The explanation of variance is quite small with a maximum of 9.7%.
McKinstryCitation51 reported an association between a patient’s social class and a stronger preference for a shared condition when consulting with the health care provider. We observed that the only sociodemographic variable with predictive power was the patient’s level of education (in terms of an emotionally supportive communication style and communication about personal circumstances). Less well educated patients with FMS tend to prefer a communication style that is more strongly oriented toward their affective needs.
In contrast with other studies, ie, those that reveal ageCitation21 as a relevant factor in the context of patient preferences, we found in our study that psychologic factors played a stronger role as predictors of communication preferences. There is little published research on the relationship between psychologic factors and communication preferences.Citation52 In our study we found that dysfunctional coping with pain (low acceptance of pain, poor implementation of relaxation and increased anger) in FMS patients tended to be associated with a stronger preference for all of the health care providers’ communication behaviors thus far examined.
Acceptance is the cognitive attitude necessary for perception and coping with pain.Citation53 Further, it influences the patient’s participation in life and activities.Citation54 Lower levels of acceptance correlate with a higher level of distress and poorer physical and social functioning.Citation55 We discovered in our study that a more pronounced preference for the instrumental dimension of communication (PPO and EOC scale of the KOPRA questionnaire) was predicted by a rather low acceptance of pain. Patients with FMS must deal with the problem that symptoms of their disease are often invisible to othersCitation56 and that there are still difficulties in diagnosing FMS.Citation4 Yet, a requirement for acceptance of a disease is that it has been diagnosed by one’s physician. Feelings of being misunderstood, rejected, or ignoredCitation9 can cause the patient to sense a higher level of distress, thus counteracting the process of acceptance.Citation53
Patients who score lower on the scale “Relaxation” (FESV) prefer an effective and open communication style from their health care providers. The “Relaxation” scale reflect the extent to which patients implement methods to relax physically.Citation31 One potential reason for this observation is that FMS patients who are insecure about applying behavioral management strategies have a stronger need for information.
FMS is often accompanied by negative emotions such as anger, stress, fear and depression.Citation57 Anger – as an affective dimension from the FESV’s psychologic strain through chronic pain – functioned as a predictor for an emotional and personal communication style (ESC and CPC scales) in our study. Other working groups have demonstrated that the intensity of anger and the general tendency to suppress it predict a stronger perception of pain in the daily life of female FMS patients.Citation58,Citation59 The desire to be able to speak about emotions and personal relationships with a provider on the part of patients who are under great emotional strain should be examined and could be treated as a specific topic.
Limitations
One of the strengths of this study is that we employed a psychometrically well tested questionnaire already administered in samples with other chronic diseases. We thus have produced a differentiated description of the communication preferences of FMS patients and have compared these with patients suffering from other chronic illnesses. We also considered a large number of patient-related predictors from four areas (sociodemographic, medical, pain impact and psychologic) to predict communication preferences.
However, our study also has a few weaknesses that should be mentioned. Our data were exclusively recruited at the beginning of treatment in one inpatient rehabilitation center in Germany. Patient preferences can change in response to the health care provider’s communication, due to changes in one’s condition, or because of certain consequences of treatment.Citation47 We did not investigate these aspects of patient preferences in this study, but we do intend to consider them in future studies. Another problem is that we do not have any information on the characteristics of our relatively large group of nonresponders (32%). Our sample size of male participants was very small (n=22). In future studies it might be interesting to consider more about sex specific differences in patients’ communication preferences.
Conclusion
Patients with FMS prefer open and patient-centered communication with their health care providers. This finding illustrates that health care providers dealing with FMS patients face a particular challenge. For one, FMS patients prefer patient-centered exchanges of information about their disease, while current medical knowledge about the precise causes of FMS is quite limited.
Emotionally supportive communication or communication about personal circumstances is less important to patients with FMS. Whether a given patient requires a more emotional communication style or prefers to talk about personal issues is up to the health care provider to determine, because the preferences for these modes of behavior vary widely. A better understanding of the individual communication preferences of patients with FMS should facilitate the provider in adapting his/her communication behavior more closely to patients’ needs.
We addressed various patient-centered factors in this study when seeking predictors for patients’ communication preferences. We noted few factors associated with communication preferences. Knowledge about the factors we considered to be relevant (education status, psychologic variables) may help health care providers to identify and apply one of the communication styles that their patient prefers. Because the association between the predictors and preferences was not too high, the influencing factors can only give us initial hints or show tendencies, which would then need to be verified in consultation with individual patients. The psychologic variables associated with higher expectations from communication were also revealed to be predictors for psychologic distress in FMS.Citation60 Patients with FMS thus present their health care providers with a double challenge.
Acknowledgments
We wish to thank the cooperating rehabilitation center (RehaKlinikum Bad Säckingen GmbH; Bad Säckingen, Germany) for their support with data collection.
The article processing charge was funded by the open access publication fund of the Albert Ludwigs University of Freiburg.
Disclosure
The authors report no conflicts of interest in this work.
References
- BensingJBridging the gap. The separate worlds of evidence-based medicine and patient-centered medicinePatient Educ Couns200039172511013544
- WolfeFClauwDFitzcharlesMAThe American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severityArthritis Care Res201062600610
- HaugliLStrandEFinestAHow do patients with rheumatic disease experience their relationship with their doctors? A qualitative study of experiences of stress and support in the doctor-patient relationshipPatient Educ Couns20045216917415132522
- PerrotSChoyEPeterselDGinovkerAKramerESurvey of physician experiences and perceptions about the diagnosis and treatment of fibromyalgiaBMC Health Serv Res20121235623051101
- BieberCMuellerKGBlumenstielKEichWPartizipative Entscheidungsfindung als Maßnahme zur Verbesserung der Arzt-Patienten-Interaktion mit Fibromyalgie-Patienten [Shared decision making improves the physician-patient interaction with fibromyalgia patients]Z Med Psychol2006155360 German
- AsbringPNarvanenALIdeal versus reality: physicians perspectives on patients with chronic fatigue syndrome (CFS) and fibromyalgiaSoc Sci Med20035771172012821018
- ChoyEPerrotSLeonTA patient survey of the impact of fibromyalgia and the journey to diagnosisBMC Health Serv Res20101010220420681
- MuellerAHartmannMEichWInanspruchnahme medizinischer Versorgungsleistungen. Untersuchung bei Patienten mit Fibromyalgiesyndrom (FMS) [Health care utilization in patients with fibromyalgia syndrome (FMS)]Schmerz2000147783 German12800043
- WernerAMalterudKIt is hard work behaving as a credible patient: encounters between women with chronic pain and their doctorsSoc Sci Med2003571409141912927471
- AnnemansLLe LayKTaiebCSocietal and patient burden of fibromyalgia syndromePharmacoeconomics20092754755919663526
- SepuchaAMullyAExtending decision support: preparation and implementationPatient Educ Couns20035026927112900098
- BieberCMuellerKGBlumenstielKA shared decision-making communication training program for physicians treating fibromyalgia patients: effects of randomized controlled trialJ Psychosom Res200864132018157994
- ThorneSEHarrisSRMahoneyKConAMcGuinnessLThe context of health care communication in chronic illnessPatient Educ Couns20045429930615324981
- WilliamsSWeinmanJDaleJDoctor-patient communication and patient satisfaction. A reviewFam Pract199815140192
- BeckRSDaughtridgeRSloanePDPhysician-patient communication in the primary care office: a systematic reviewJ Am Board Fam Pract200215253811841136
- GriffinSJKinmonthALVeltmanMWMGillardSGrantJStewardMEffect on health-related outcomes of interventions to alter the interaction between patients and practitioners: a systematic review of trialsAnn Fam Med2004259560815576546
- FarinEGrammLSchmidtETaking into account patient`s communication preferences: instrument development and results in chronic back pain patientsPatient Educ Couns201286414821570795
- SerberERCronanTAWalenHRPredictors of patient satisfaction and health care costs for patients with fibromyalgiaPsychol Health200318771787
- AroraNKMcHorneyCPatient preferences for medical decision making: who really wants to participate?Med Care20003833534110718358
- GarfieldSSmithFFrancisSAChalmersCCan patient`s preferences for involvement in decision-making regarding the use of medicines be predicted?Patient Educ Couns20076636136717331691
- CoulterAEllinsJPatient-focused Interventions: A Review of the Evidence (Report)London, UKPicker Institute Europe and Health Foundation2006
- World Health Organization (WHO)The ICD-10 Classification of Mental and Behavioural DisordersGenevaWHO1992
- WolfeFSmytheHAYunusMBThe American College of Rheumatology criteria for the classification of fibromyalgia. Report of the Multicenter Criteria CommitteeArthritis Rheum1990331601722306288
- GranJTThe epidemiology of chronic generalized musculoskeletal painBest Pract Res Clin Rheumatol20031754756112849711
- GlattackerMMeixnerKFarinEJäckelWHEntwicklung eines rehabilitationsspezifischen Komorbiditätsscores und Prüfung der methodischen Gütekriterien [Development and psychometric testing of a rehabilitation specific comorbidity score]Phys Med Rehab Kuror200717260270 German
- OffenbaecherMWaltzMSchoepsPValidation of a German version of the Fibromyalgia Impact Questionnaire (FIQ-G)J Rheumatol2000271984198810955342
- Moss-MorrisRWeinmanJPetrieKJHorneRCameronLDBuickDThe Revised Illness Perception Questionnaire (IPQ-R)Psychol Health200217116
- HerrmannCBussUSnaithRPHADS-D – Hospital Anxiety and Depression Scale, Deutsche Version: Ein Fragebogen zur Erfassung von Angst und Depressivität in der somatischen MedizinBernHans Huber1995 German
- MüllerAHartmannMMüllerKValidation of the arthritis self-efficacy short-form scale in German fibromyalgia patientsEur J Pain2003716317112600798
- NilgesPKösterBSchmidtCOSchmerzakzeptanz – Konzept und Überprüfung einer deutschen Fassung des Chronic Pain Acceptance Questionnaire [Pain acceptance – concept and validation of a German version of the Chronic Pain Acceptance Questionnaire]Schmerz2007215767 German17111168
- GeissnerEFESV Fragebogen zur Erfassung der Schmerzverarbeitung (Manual)GöttingenHogrefe2001 German
- ScascighiniLLitschiMWaltiMSprottHEffect of an interdisciplinary outpatient pain management program (IOPP) for chronic pain patients with and without migration background: A prospective, observational clinical studyPain Med20111270671621463468
- VerraMLAngstFLehmannSAeschlimannATranslation, cross-cultural adaptation, reliability, and validity of the German version of the Coping Strategies Questionnaire (CSQ-D)J Pain2006732733616632322
- FarinEGrammLKosiolDDevelopment of a questionnaire to assess communication preferences of patients with chronic illnessPatient Educ Couns201182818820219317
- FarinEBaumannWKommunikationspräferenzen onkologischer Patienten [Communication preferences of oncology patients]Das Gesundheitswesen In press German
- FarinEGrammLSchmidtEThe congruence of patient communication preferences and physician communication behavior in cardiac patientsJ Cardiopulm Rehabil201131349357
- NunnallyJCBernsteinIRAPsychometric Theory3rd edNew YorkMcGraw-Hill1994
- SchaferJLNORM: multiple imputation of incomplete multivariate data under a normal model, version 2.03, software for Windows 95/98/NT Available from http://sites.stat.psu.edu/~jls/misoftwa.htmlAccessed August 20, 2013
- MantelNWhy stepwise procedures in variable selectionTechnometrics197012621625
- MenardSWApplied Logistic Regression Analysis2nd edThousand Oaks, CASage2002
- FarinENaglMThe patient-physician relationship in patients with breast cancer: descriptive results and influence on quality of life after rehabilitationQual Life Res20132228329422419450
- SepuchaKMulleyAGJrA perspective on the patient`s role in treatment decisionsMed Care Res Rev2009665374
- EichWHäuserWArnoldBFibromyalgia syndrome: Definition, classification, clinical diagnosis and prognosisSchmerz20122610.1007/s00482-012-1169-x
- TowleAGodolphinWFramework for teaching and learning informed shared decision makingBMJ199931976677110488010
- TarimanJDBerryDLCochraneBDoorenbosAScheppKPreferred and actual roles during health care decision making in persons with cancer: a systematic reviewAnn Oncol2010211145115119940010
- EpsteinRMFranksPShieldsCGMeldrumSCMillerKNCampbellTLPatient-centered communication and diagnostic testingAnn Fam Med2005341542116189057
- StreetRLJrElwynGEpsteinRMPatient preferences and outcomes: an ecological perspectiveExpert Rev Pharmacoecon Outcomes Res20121216718022458618
- MatthiasMSBairMJThe patient-provider relationship in chronic pain management: Where do we go from here?Pain Med2010111747174921134115
- KenniferSLAlexanderSCPollakKINegative emotions in cancer care: Do oncologist` responses depend on severity and type of emotion?Patient Educ Couns200976515619041211
- HackTFDegnerLFParkerPAThe communication goals and needs of cancer patients: a reviewPsychooncology20051483184516200519
- McKinstryBDo patients wish to be involved in decision making in the consultation?Brit Med J200032186787111021866
- HashimotoHFukuharaSThe influence of locus of control on preferences for information and decision makingPatient Educ Couns20045523624015530760
- LaChapelleDLLavoieSBoudreauAThe meaning and process of pain acceptance. Perceptions of women living with arthritis and fibromyalgiaPain Res Manag200813320121018592056
- VianeICrombezGEcclestonCAcceptance of pain is an independent predictor of mental well-being in patients with chronic pain: empirical evidence and reappraisalPain2003106657214581112
- RoderoBCasanuevaBLucianoJVGiliMSerrano-BlancoACarcìa-CampayoJRelationship between behavorial coping strategies and acceptance in patients with fibromyalgia syndrome: Elucidating targets of interventionsBMC Musculoskel Dis201112143
- SimJMaddenSCreating meaning in fibromyalgia syndromeSoc Sci Med2006632962297316949713
- ToussaintLOvervold-RonningenMVincentAImplications of forgiveness enhancement in patients with fibromyalgia and chronic fatigue syndromeJ Health Care Chaplain20101612313920658426
- Van MiddendorpHLumleyMAMoerbeekMJacobsJWGBijlsmaJWJGeenenREffects of anger and anger regulation styles on pain in daily life of women with fibromyalgia: A diary studyEur J Pain20101417618219375966
- BurnsJWArousal of negative emotions and symptom-specific reactivity in chronic low back pain patientsEmotion2006630931916768562
- Van KoulilSVan LankveldWKraaimaatFWVan RielPLCMEversAWMRisk factors for longer term psychological distress in well-functioning fibromyalgia patients: A prospective study into prognostic factorsPatient Educ Couns20108012612919744816
- ZigmondASSnaithRPThe Hospital Anxiety and Depression ScaleActa Psychiatr Scand1983673613706880820