Abstract
Background
In Tanzania, where over a third of the society is impoverished, the burden of NCDs which account for about two-fifths of all disability-adjusted life years (DALYs) and one-third of premature deaths has doubled in the past two decades. However, notwithstanding a wider realization of the escalating burden of NCDs across Tanzania, the link between NCD awareness and lifestyle practices at the population level is not well characterized. We aimed to establish the gap between NCD knowledge and healthy behaviors.
Methods
This multi-regional community-based cross-sectional study was conducted in 5 regions of Tanzania between September 2022 and June 2023. A 22-item standardized tool evaluating various NCD risk behaviors was used in knowledge assessment and a cut-off of ≥70% was used to denote good knowledge. Bivariate analyses were performed to compare knowledge of NCD risk factors across various NCD risk subgroups. All tests were two tailed, and the significance was set at p<0.05.
Results
A total of 5121 individuals were consecutively enrolled. The mean age was 47.2 years and females comprised over three-fifths (60.8%) of the participants. With regard to behavioral NCD risks, physical inactivity, unhealthy diet, smoking and alcohol consumption were present in 79.0%, 70.2%, 2.1% and 17.6% of participants, respectively. Moreover, biological risk factors, ie, excess body weight, hypertension, and diabetes were present in 68.4%, 55.8% and 13.0% of participants, respectively. The mean knowledge score was 77.1% and 70.3% of participants demonstrated good knowledge of NCD risk factors. Except for smoking, individuals who showed awareness of various NCD risk factors were found to have significant rates of risky behaviors.
Conclusion
Despite sufficient NCD risk knowledge, incongruent lifestyle practices persist, highlighting a crucial concern. This suggests that awareness of NCDs and their risks may influence motivation for change but may not necessarily result in lifestyle modification.
Introduction
Despite remarkable medical breakthroughs in recent decades, non-communicable diseases (NCDs) which hinder socio-economic development besides posing significant threats to international health security remain a significant public health challenge across the globe.Citation1 Currently, three-quarters of the world’s deaths (85% of which transpire in low- and middle-income countries) are attributable to NCDs.Citation2,Citation3 In particular, the Sub-Saharan Africa (SSA) region which bear a disproportionate burden of the ever present communicable diseases has witnessed a 67% rise of NCDs in the past three decades (ie, more than any other region worldwide).Citation4 While barely 2% of the overall health development assistance has been dedicated to chronic diseases in the past two decades, NCDs continue to be one of the most underfunded threats of global health importance.Citation5–7 Consequently, the present global trends show that NCDs are assuming an alarming dimension and will inevitably eclipse the burden of communicable diseases to become the leading cause of morbidity and mortality in the foreseeable future.Citation8
In Tanzania, where over a third of the society is impoverished, the burden of NCDs which account for about two-fifths of all disability-adjusted life years (DALYs) as well as 34% and 31% of all deaths and premature deaths, respectively, has doubled in the past two decades.Citation9,Citation10 Similar to the rest of the developing world, the upsurge of NCDs outpaces population-level interventions (ie, inadequate efforts on prevention and control) in Tanzania. Moreover, in addressing effective prevention and treatment of NCDs, it is fundamental to explore the gaps in knowledge of risk factors and lifestyle practices in the general population. However, notwithstanding a wider realization of the escalating burden of NCDs across Tanzania, the link between NCD awareness and lifestyle practices at the population level is not well characterized.Citation11–13 In pursuit of a paradigm shift in the prevention of NCDs in Tanzania, this multiregional community-based study aspired to establish and bridge the gap between NCD knowledge and healthy behaviors.
Methods
Recruitment Process and Definition of Terms
This multi-regional community-based cross-sectional study was conducted in 5 regions (ie, Arusha, Dar es Salaam, Geita, Mtwara and Zanzibar) of Tanzania between September 2022 and June 2023. This is part of the countrywide ongoing NCD campaign by the Jakaya Kikwete Cardiac Institute (JKCI), and at the time of writing this manuscript, the aforementioned five regions were the ones that had been covered. The aforementioned screening program was announced in respective communities, utilized the respective regional hospitals premises and participants voluntarily came for the free NCD screening services. Participants (aged ≥18 years) were enrolled consecutively, and the total sample comprised 5121 individuals who voluntarily accessed the scheduled screening in their respective regions. As per the 2022 Tanzania Demographic and Health Survey and Malaria Indicator Survey (2022 TDHS-MIS) census; Arusha, Dar es Salaam, Geita, Mtwara and Zanzibar regions had a population of 2,356,255; 7,405,000; 2,977,608; 1,634,947; and 1,889,773 people, respectively.Citation14
Clinicodemographic and NCD risk profiles, key vitals (including blood pressure, blood sugar, height, and weight) and NCD risk knowledge were assessed using a structured questionnaire. Assessment of physical activity was self-reported and Physical Activity Vital Sign (PAVS) scale was utilized in estimating activity level.Citation15 Score of ≥150 min/week was used as a cut-off for physical activeness. With regard to weight, BMI < 18.5 kg/m2, 18.5–24.9 kg/m2, 25.0–29.9 kg/m2 and ≥30.0 kg/m2 were used to denote underweight, healthy weight, overweight and obesity, respectively.Citation16 Use of cigarette within a 6-month time frame was used to categorize participants as non-smoker, past smoker or current smoker. A weekly intake of an alcoholic beverage was used to label a participant as a drinker.
Participants using blood pressure lowering agents, systolic blood pressure (SBP) ≥140 mmHg or diastolic blood pressure (DBP) ≥90 mmHg were regarded as hypertensiveCitation17 Likewise, individuals on glucose-lowering agents, random blood glucose (RBG) ≥11.1 mmol/L or fasting blood glucose (FBG) ≥7 mmol/L were regarded as having diabetes.Citation18 A 22-item standardized tool evaluating various NCD risk behaviors was used in knowledge assessment and a cut-off of ≥70% was used to denote good knowledge.Citation19–21 Aside from screening, nutritional education pertaining to NCDs was given to all participants by a competent nutritionist. Following this, study subjects were given time to reflect on their dietary behaviors and eventually give a self-assessment of whether on average they have healthy or unhealthy eating habits. Moreover, one-on-one nutritional counseling was offered to eligible participants.
Statistical Analysis
STATA v11.0 software was employed in all statistical analyses. Continuous and categorical variables summaries are expressed as means (± SD) and percentages, respectively. Pearson Chi square test and Student’s t-test techniques were used for comparison of categorical and continuous variables, respectively. Bivariate analyses were performed to compare knowledge of NCD risk factors across various NCD risk subgroups. All tests were two tailed, and the significance was set at p<0.05.
Results
Sociodemographic Characteristics and NCD Risk Profile of Participants
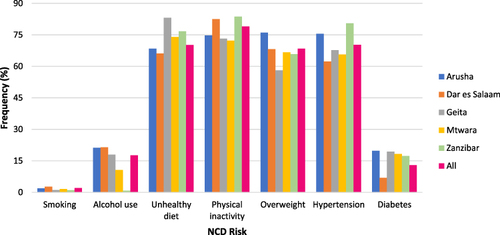
A total of 5121 individuals were consecutively enrolled in this multi-regional community-based screening. displays the sociodemographic and NCD risk profiles of the study participants. The mean age was 47.2 years and the age group 35–54 years constituted over two-fifths (43.3%) of the study population. Females comprised over three-fifths (60.8%) of the participants, over three-quarters (77.7%) were married, nearly two-fifths (39.2%) of participants had primary-level education or less, and over a quarter (26.9%) were either jobless or retired. Less than half (44.1%) of participants had health insurance and over a quarter (28.6%) had a positive family history of NCDs. With regard to behavioral NCD risks, physical inactivity, unhealthy diet, smoking and alcohol consumption were present in 79.0%, 70.2%, 2.1% and 17.6% of participants, respectively. Moreover, biological risk factors, ie, excess body weight, hypertension, and diabetes were recognized in 68.4%, 55.8% and 13.0% of participants, respectively. Among participants with hypertension and diabetes, 817 (28.6%) and 184 (27.5%), respectively, were newly diagnosed during this present screening. There was a slight variation in risk pattern across the 5 regions, .
Table 1 Sociodemographic Characteristics and NCD Risk Profile of Study Participants (N = 5121)
Knowledge of NCD Risk Factors
summarizes respondents’ responses on NCD knowledge questions. The mean NCD knowledge score was 77.1% with a range between 31.8% and 100%. Overall, individuals in each of the 5 regions demonstrated an averagely good knowledge ranging from 74.6% in Dar es Salaam to 83.7% in Arusha. A total of 3600 (70.3%) participants demonstrated good knowledge, 1387 (27.1%) displayed moderate knowledge, and 134 (2.6%) had low knowledge of NCD risk factors. About 30.1% of Individuals were not aware that NCDs are the leading cause of global mortality, while 22.6% believed that NCDs are not preventable. Additionally, 66.1% of participants thought that one may know if they have NCDs based on symptoms alone, whereas 54.0% had a perception that NCDs are curable upon completion of prescribed dosage. Smoking was recognized as an NCD risk by 73.0%, physical inactivity by 93.6%, excessive alcohol drinking by 92.0%, and high-salt diet by 80.5% of participants. Moreover, excess body weight, high blood pressure and diabetes were acknowledged as risks by 91.9%, 91.3%, and 78.3% of participants respectively.
Table 2 Participants’ Responses to the NCD Knowledge Questionnaire by Region (N = 5121)
displays knowledge of NCD risk factors across various NCD risk subgroups. Physically active participants displayed superior NCD knowledge compared to their underactive counterparts, ie, 76.5% vs 68.6%, p<0.001. On the other hand, participants with unhealthy eating habits exhibited similar NCD knowledge to the healthy eating individuals, ie, 70.1% vs 70.7%, p = 0.6. Likewise, alcohol drinking participants showed similar knowledge to their non-drinking counterparts, ie, 69.1% vs 70.6%, p = 0.4. With regard to tobacco use, smokers displayed inferior NCD knowledge to non-smokers, ie, 50.9% vs 70.7%, p<0.001. Interestingly, overweight, hypertensive and participants with diabetes displayed significantly higher NCD knowledge compared to their healthy weight, normotensive and normoglycemic counterparts, respectively, ie, 72.5% vs 65.1%, 76.8% vs 62.1%, 80.1% vs 68.8%; all p<0.001.
Table 3 NCD Knowledge Across Various NCD Risk Subgroups (N=5121)
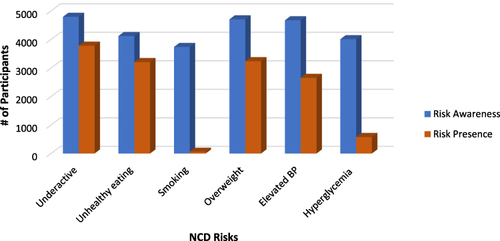
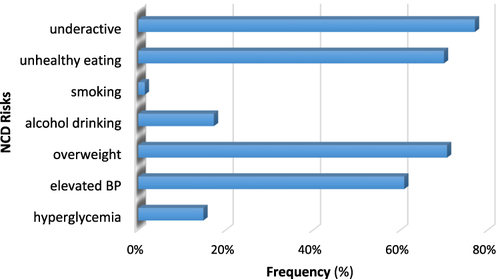
Association Between NCD Knowledge and Lifestyle
displays the pattern of NCD risks awareness versus existence of such risks in our study group. Overall, of the individuals that demonstrated awareness to physical inactivity as a risk, 78.9% were underactive; 77.8% of those aware that unhealthy eating is a risk had bad eating habits; 1.7% of participants with awareness of smoking as a risk were current smokers; 69.3% of study subjects with awareness of overweight as a risk had excess body weight; and 14.4% of those aware of hyperglycemia as a risk were categorized as diabetic in this study. shows the pattern of NCD risk factors among participants with good NCD knowledge. Although smoking (1.5%), diabetes (14.9%) and alcohol drinking (17.3%) were present in relatively lesser frequencies, other risk factors including hypertension (60.9%), unhealthy eating (70.0%), overweight (70.7%) and physical inactivity (77.1%) were observed in a striking proportion of knowledgeable participants.
Discussion
The soaring NCD epidemic in SSA has surpassed the global average, continues to entrench poverty and remains a formidable threat to accomplishment of the developmental goals.Citation22 Moreover, the NCD burden adds substantial pressure to already overstrained healthcare systems in SSA and the rest of the developing world. Over two-fifths of NCD-related deaths occur prematurely, with four-fifths of these transpiring in the developing world.Citation23 Formulation and implementation of effective behavior change interventions are fundamental if the global quest to reduce premature mortality from NCDs by a quarter 2025 and achieve a 30% reduction in sustainable development goal (SDG) by 2030 is to be attained.Citation24 Inevitably, the escalating NCD epidemic requires both strengthening and adaptation of health systems across the globe; however, the developing world in general and SSA in particular is lagging behind with population-level interventions for NCD prevention.Citation25
Despite its complexity and pervasiveness, over two-fifths of the variations in health among persons is attributable to lifestyle practices.Citation26 As healthy lifestyles influence both disease prevention and health promotion, individuals with poor lifestyle practices display superior all-cause mortality, which rises with an increase in the number of unhealthy behaviors. For instance, nonsmokers, physically active and healthy eating individuals have a 56%, 47% and 26% reduction in all-cause mortality, respectively, compared to their counterparts who do not engage in the aforementioned behaviors.Citation27 Moreover, for participants who engage in the aforementioned behaviors, the risk of death is significantly reduced across all major NCDs.Citation27 Participants from this study displayed concerning rates of risky behaviors, particularly unhealthy diet and physical inactivity, which resonates with the observed high rates of excess body weight. Indeed, unhealthy diet and physical inactivity are the major NCD drivers with decisive roles in the epidemic.Citation28–30 In unison with our present findings, a couple of other studies in a Tanzanian setting revealed somewhat similar rates of modifiable behavioral risks.Citation11–13,Citation31 Nonetheless, regardless of the enormous challenges facing its implementation and sustainability, maintaining a healthy lifestyle is undeniably the most efficient and cost-effective strategy in the battle against NCDs.
To curb the NCD menace, a holistic approach from global to individual level is pivotal. As lifestyle modification entails both behavioral and cognitive adjustments, the gap in knowledge of NCD risk factors at the population level is realized as an important barrier to both its prevention and management. We observed quite impressive rates of NCD knowledge in this study. These findings are fairly similar to those from our earlier study conducted among caregivers of cardiovascular disease (CVD) patients,Citation12 however, other studies from Tanzania have revealed significantly lower knowledge rates (ie, 25.4% and 35.4%).Citation31,Citation32 Likewise, other African studies have revealed significantly lower knowledge rates, ranging from 6.7% in Rwanda to 33.9% in Ethiopia.Citation33–35 The good public knowledge observed in this present multiregional study is potentially a result of scaling up of NCD advocacy activities along with other NCD initiatives by the Tanzanian Ministry of Health (MoH). In congruence with the Global Week for Action on NCDs, the MoH Tanzania initiated the National NCD week since 2019 whose aim is to promote NCD prevention through creating awareness, health promotion, community engagement, screening services and sharing best practices regarding NCDs in a scientific platform.Citation36,Citation37 Considering such commendable efforts yet a rather wide knowledge variation across existing studies in Tanzania, it is clear that region-specific tailored efforts to improve awareness are required.
A notable finding from this study is the observation that knowledge had no correlation with lifestyle practices. Contrary to our expectations, participants with good knowledge displayed alarming rates of modifiable risk factors, particularly unhealthy diets, physical inactivity and excess body weight. Congruently, such pattern of behavioral risks in a subset of knowledgeable individuals is observed in numerous studies across the globe. For instance, although between 71.1% and 80% of study participants from Tanzania, United Arab Emirates, Ghana, Malaysia, and Nigeria displayed good NCD knowledge; physical inactivity, unhealthy eating and overweight rates ranged between 75.2%-90.1%, 79.7%-82.2% and 66.8%-78%, respectively.Citation12,Citation38–41 As disease prevention is based on the execution of effective national healthcare policies, the dearth of NCD policies or their slow and uneven implementation among African states (Tanzania inclusive) remains a barrier in the fight against NCDs and is a potential contributor to the high frequency of risky behaviors irrespective of improved awareness. For instance, at 47% and 16% implementation rates, tobacco and physical activity policies are the highest and least implemented, respectively, in Africa.Citation42 Furthermore, with respect to East Africa, just 5.5% and 9.0% of dietary and physical activity policies, respectively, are implemented.Citation42 In view of the above, it remains a colossal challenge translating and integrating NCD policy strategies into daily operations in Africa and thus for their successful implementation; improved harmonization, sustainable funding, and robust monitoring strategies are indispensable.
We acknowledge several strengths including (i) a sizeable sample for a robust estimation and description of burden and pattern of risky behaviors, (ii) utilization of competent personnel as well as utilization of standardized tools for assessment of behavior and knowledge of NCDs. However, we faced the following limitations: (i) due to the study design and sampling method used, generalizability of findings and causality exploration are not conceivable. Nevertheless, these findings raise considerable public health concerns as well as providing grounds for conducting further research on a larger scale for a more reliable estimation of NCD risks and lifestyle practices. Lastly, owing to the self-report nature of some variables (ie, smoking, alcohol use, physical inactivity and eating habits), our findings could potentially be prone to reverse causation, response bias, participation bias and recall bias.
Conclusion
Notwithstanding the adequate NCD risk knowledge observed in this study, lifestyle practices were incongruent and remain a major concern. This implies that awareness of NCDs and their attributable risks may affect the motivation for lifestyle change but does not necessarily lead to lifestyle modification. As strengthening of community’s primary prevention interventions and improving responsiveness of health care systems to NCD prevention remain a priority in the fight against NCDs, efforts to devise strategies to ensure that NCD risk knowledge and lifestyle practices are at par is fundamental. Successful implemented lifestyle modification programs in community settings have enormous potential to improve lifestyle practices, particularly physical activity and eating behaviors. Furthermore, as unhealthy eating and physical inactivity were the leading modifiable behavioral risks, it is high time that NCD policies are integrated particularly into urban planning by restricting unhealthy food environment and developing activity-friendly milieu. Moreover, considering the highly convincing marketing strategies by the burgeoning fast food and beverage industries, incentivization of healthy behaviors could potentially be a viable stimulant to behavior change. Lastly, owing to their cost-effective and prompt attribute, mobile phones which are potential tools in improving healthcare delivery and promoting healthy behaviors will be rewarding in this setting.Citation43
Abbreviations
BMI, body mass index; BP, blood pressure; CVD, cardiovascular disease; DALYs, disability-adjusted life years; DBP, diastolic blood pressure; DSM, Dar es Salaam; ECHO, echocardiography; FBG, fasting blood glucose; JKCI, Jakaya Kikwete Cardiac Institute; MoH, Ministry of Health; NCDs, non-communicable diseases; PAVS, physical activity vital sign; SSA, sub-Saharan Africa; SBP, systolic blood pressure; SD, standard deviation; TDHS-MIS, Tanzania Demographic and Health Survey and Malaria Indicator Survey; ZnZ, Zanzibar.
Ethics Approval and Consent to Participate
The study protocol was submitted to and approved by the Ethical Committee, of the Jakaya Kikwete Cardiac Institute. Written informed consent was obtained from all study participants. This research was conducted in accordance with the Declaration of Helsinki.
Disclosure
The authors have no conflict of interest to declare in this work.
Acknowledgment
We are thankful to all study participants for their cooperation during this multi-regional community-based screening.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- Lago-Peñas S, Rivera B, Cantarero D, et al. The impact of socioeconomic position on non-communicable diseases: what do we know about it? Perspect Public Health. 2021;141(3):158–176. doi:10.1177/1757913920914952
- Abajobir AA, Abbafati C, Abbas KM, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–1210. doi:10.1016/S0140-6736(17)32152-9
- Bollyky TJ, Templin T, Cohen M, Dieleman JL. Lower-income countries that face the most rapid shift in noncommunicable disease burden are also the least prepared. Health Aff. 2017;36(11):1866–1875. doi:10.1377/hlthaff.2017.0708
- Gouda HN, Charlson F, Sorsdahl K, et al. Burden of non-communicable diseases in sub-Saharan Africa, 1990–2017: results from the Global Burden of Disease Study 2017. Lancet Glob Health. 2019;7(10):e1375–e1387. doi:10.1016/S2214-109X(19)30374-2
- Allen LN. Financing national non-communicable disease responses. Glob Health Action. 2017;10(1):1326687. doi:10.1080/16549716.2017.1326687
- Collins TE, Nugent R, Webb D, et al. Time to align: development cooperation for the prevention and control of non-communicable diseases. BMJ. 2019;366:l4499. doi:10.1136/bmj.l4499
- Institute for Health Metrics and Evaluation (IHME) Financing global health 2018: countries and programs in transition. IHME; 2019. Available from: http://www.healthdata.org/sites/default/files/files/policy_report/FGH/2019/FGH_2018_full-report.pdf. Accessed May 7, 2024.
- Noncommunicable diseases. World Health Organization Regional Office of Africa. Available from: https://www.afro.who.int/health-topics/noncommunicable-diseases. Accessed October 22, 2023.
- The Tanzania NCDI Poverty Commission Tanzania non-Communicable Diseases and Injuries Poverty Commission: Findings and Recommendations; 2020. Available from: https://www.ncdipoverty.org/national-commission-reports. Accessed October 22, 2023.
- The United Republic of Tanzania, Ministry of Health and Social Welfare. National noncommunicable diseases strategy, July 2008–June 2018; 2008.
- Pallangyo P, Komba M, Mkojera ZS, et al. Non-communicable disease risk factors among caregivers of patients attending a tertiary cardiovascular hospital in Tanzania. Int J Gen Med. 2022;15:4685–4696. doi:10.2147/IJGM.S364392
- Pallangyo P, Misidai N, Komba M, et al. Knowledge of cardiovascular risk factors among caretakers of outpatients attending a tertiary cardiovascular center in Tanzania: a cross-sectional survey. BMC Cardiovasc Disord. 2020;20(1):364. doi:10.1186/s12872-020-01648-1
- Pallangyo P, Mkojera ZS, Hemed NR, et al. Obesity epidemic in urban Tanzania: a public health calamity in an already overwhelmed and fragmented health system. BMC Endocr Disord. 2020;20(1):147. doi:10.1186/s12902-020-00631-3
- Ministry of Health (MoH) [Tanzania Mainland], Ministry of Health (MoH) [Zanzibar], National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS), and ICF. Tanzania Demographic and Health Survey and Malaria Indicator Survey 2022 Final Report. Dodoma, Tanzania, and Rockville, Maryland, USA: MoH, NBS, OCGS, and ICF; 2022. Available from: https://www.dhsprogram.com/pubs/pdf/FR382/FR382.pdf. Accessed May 7, 2024.
- Strath SJ, Kaminsky LA, Ainsworth BE, et al. Guide to the assessment of physical activity: clinical and research applications. A scientific statement from the American Heart Association. Circulation. 2013;128(20):2259–2279. doi:10.1161/01.cir.0000435708.67487.da
- Centers for Disease Control and Prevention. Division of nutrition, physical activity, and obesity. About Adult BMI. Available from: http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/. Accessed May 7, 2024.
- Chobanian AV, Bakris GL, Black HR. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206–1252. doi:10.1161/01.HYP.0000107251.49515.c2
- American Diabetes Association. Classification and diagnosis of diabetes. Sec. 2. In Standards of Medical Care in Diabetes—2015. Diabetes Care. 2015;38(Suppl. 1):S8–S16.
- Burger A, Pretorius R, Fourie Carla MT, et al. The relationship between cardiovascular risk factors and knowledge of cardiovascular disease in African men in the north-West Province. Health SA. 2016;21(1):364–371. doi:10.1016/j.hsag.2016.07.003
- Amadi CE, Lawal FO, Mbakwem AC, et al. Knowledge of cardiovascular disease risk factors and practice of primary prevention of cardiovascular disease by Community Pharmacists in Nigeria: a cross-sectional study. Int J Clin Pharm. 2018;40(6):1587–1595. doi:10.1007/s11096-018-0744-3
- Boateng D, Wekesah F, Browne JL, et al. Knowledge and awareness of and perception towards cardiovascular disease risk in sub-Saharan Africa: a systematic review. PLoS One. 2017;12(12):e0189264. doi:10.1371/journal.pone.0189264
- Mudie K, Jin MM, Tan, et al. Non-communicable diseases in sub-Saharan Africa: a scoping review of large cohort studies. J Glob Health. 2019;9(2):020409. doi:10.7189/jogh.09.020409
- Hadian M, Mozafari MR, Mazaheri E, Jabbari A. Challenges of the health system in preventing non-communicable diseases; systematized review. Int J Prev Med. 2021;12:71. doi:10.4103/ijpvm.IJPVM_487_20
- Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020. Geneva: World Health Organization; 2013. Available from: http://apps.who.int/iris/bitstream/10665/148114/9789241564854_eng.pdf. Accessed January 15, 2024.
- Juma K, Juma PA, Shumba C, Otieno P, Asiki G. Non-communicable diseases and urbanization in African Cities: a narrative review. In: Public Health in Developing Countries—Challenges and Opportunities. IntechOpen; 2020:1–274.
- Satcher D, Higginbotham EJ. The public health approach to eliminating disparities in health. Am J Public Health. 2008;98(9 Suppl):S8–S11. doi:10.2105/AJPH.98.Supplement_1.S8
- Ford E, Bergmann M, Boeing H, et al. Healthy lifestyle behaviors and all-cause mortality among adults in the United States. Prev Med. 2012;55(1):23–27. doi:10.1016/j.ypmed.2012.04.016
- Afshin A, Sur PJ, Fay KA; GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;393(10184):1958–1972. doi:10.1016/S0140-6736(19)30041-8
- Al-Jawaldeh A, Abbass MMS. Unhealthy dietary habits and obesity: the major risk factors beyond non-communicable diseases in the Eastern Mediterranean Region. Front Nutr. 2022;9:817808. doi:10.3389/fnut.2022.817808
- Cerf ME. Healthy lifestyles and noncommunicable diseases: nutrition, the life-course, and health promotion. Lifestyle Med. 2021;2(2):e31. doi:10.1002/lim2.31
- Gibore NS, Munyogwa MJ, Ng’weshemi SK, Gesase AP. Prevalence and knowledge of modifiable cardiovascular diseases risk factors among vulnerable population in Central Tanzania. BMC Cardiovasc Disord. 2023;23(1):373. doi:10.1186/s12872-023-03408-3
- Muhihi AJ, Anaeli A, Mpembeni RNM, et al. Public knowledge of risk factors and warning signs for cardiovascular disease among young and middle-aged adults in rural Tanzania. BMC Public Health. 2020;20(1). doi:10.1186/s12889-020-09956-z
- Biraguma J, Mutimura E, Frantz JM. Knowledge about modifiable risk factors for non-communicable diseases adults living with HIV in Rwanda. Afr Health Sci. 2019;19(4):3181–3189. doi:10.4314/ahs.v19i4.41
- Akintunde AA, Akintunde T, Opadijo OG. Knowledge of heart disease risk factors among workers in a Nigerian University: a call for concern. Niger Med J. 2015;56(2):91–95. doi:10.4103/0300-1652.150688
- Legesse E, Nigussie T, Girma D, et al. Level of adequate knowledge of non-communicable diseases and associated factors among adult residents of North Shewa Zone, Oromia Region, Ethiopia: a Mixed-Method Approach. Front Public Health. 2022;10:892108. doi:10.3389/fpubh.2022.892108
- Ndumwa HP, Amani DE, Ngowi JE, et al. Mitigating the rising burden of non-communicable diseases through locally generated evidence-lessons from Tanzania. Ann Glob Health. 2023;89(1):77. doi:10.5334/aogh.4111
- Njiro BJ, Ngowi JE, Ndumwa HP, et al. Non-communicable diseases week: best practices in addressing the NCDs Burden from Tanzania. Ann Glob Health. 2023;89(1):89. doi:10.5334/aogh.4116
- Kazim MN, AbouMoussa TH, Al-Hammadi FA, et al. Population awareness of cardiovascular disease risk factors and health care seeking behavior in the UAE. Am J Prev Cardiol. 2021;8:100255. doi:10.1016/j.ajpc.2021.100255
- Sanuade OA, Kushitor MK, Awuah RB, et al. Lay knowledge of cardiovascular disease and risk factors in three communities in Accra, Ghana: a cross-sectional survey. BMJ Open. 2021;11(12):e049451. doi:10.1136/bmjopen-2021-049451
- Ithnin M, Nor NAUM, Nordin NJ, et al. Knowledge, attitude, and practice on Non-Communicable Diseases (NCDs) among the adult population in the urban area of Negeri Sembilan. Malaysia Int J Res Pharm Sci. 2023;9(SPL 2):88–94.
- Ricketts-Odebode OO, Ladi-Akinyemi TW, Kanma-Okafor OJ. Knowledge and exposure to non-communicable disease risk factors amongst undergraduates in the University of Lagos. Niger J Health Sci. 2022;22(1):1–10. doi:10.4103/njhs.njhs_3_22
- Kassa MD, Grace JM. Noncommunicable diseases prevention policies and their implementation in Africa: a systematic review. Public Health Rev. 2022;42:1604310. doi:10.3389/phrs.2021.1604310
- Müller AM, Alley S, Schoeppe S, et al. The effectiveness of e-& mHealth interventions to promote physical activity and healthy diets in developing countries: a systematic review. Int J Behav Nutr Phys Act. 2016;13(1):109. doi:10.1186/s12966-016-0434-2