Abstract
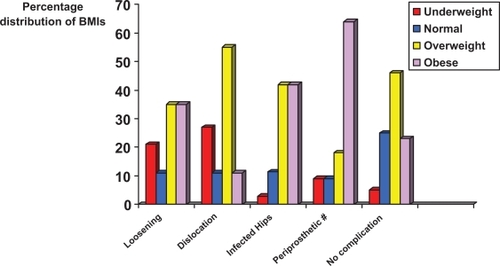
This work assessed the body mass characteristics of a cohort of community dwelling adults requiring surgery for complications related to primary hip arthroplasty, among other factors. The specific aim was to identify the extent to which high body mass prevailed in the cohort as a whole, to identify a role for subnormal body mass in the pathogenesis of post-operative complications following hip joint arthroplasty, and to identify whether different complication types could be differentiated on the basis of body mass profiles. The subjects were males and females drawn from a representative sample of 1,040 hip osteoarthritis patients between the ages of 30–89 years hospitalized for purposes of primary hip arthroplasty or complications related to prior replacement surgery. An analysis of their medical records showed: 1) Approximately 20% of the present cohort was constituted by patients with various complications related to prior arthroplasties, or to general deterioration of their condition; 2) The most common reasons for their re-hospitalization were aseptic prosthetic loosening followed by infection, prosthetic dislocations, prosthetic and periprosthetic fractures, and second surgeries on the opposite hip; 3) The presence of a high body mass index differentiated those presenting with aseptic prosthetic loosening, periprosthetic fractures, and those with infected hips (p < 0.007). Those with infection diagnoses were significantly heavier on average than those with no infection, regardless of diagnosis, and more cases with a dislocation history were underweight, rather than overweight (p < 0.05). It is concluded, a small but clinically relevant proportion of obese or underweight adults with hip osteoarthritis who undergo primary total hip replacement may experience complications at higher rates than cases with normal body weight, despite the generally successful outcomes experienced by the majority of hip arthroplasty patients.
Introduction
Aseptic loosening and periprosthetic osteolysis are the most common complications observed after total hip arthroplasty,Citation1 a surgical procedure that significantly improves the health and well-being of patients diagnosed as having painful disabling end-stage hip osteoarthritis.Citation2 Other problems that often require re-hospitalization after total hip replacement surgery are prosthetic infection, a major complication that can adversely affect the outcome of this surgical procedure.Citation3 Other reported problems include periprosthetic fracture, a failed arthroplasty, nonunion of an intertrochanteric fracture,Citation4 and prosthetic dislocation.Citation5 While mechanical factors due to the characteristics of the metal prostheses and fixation mechanisms used for this form of surgery can influence total hip arthroplasty outcomes differentially,Citation6 it is possible other factors explain why some hip arthroplasty cases are more vulnerable to complications than others. Some of these risk factors include, age, disease duration, and comorbid status. In addition, some evidence suggests body mass may influence prosthesis longevity, and/or the proclivity to dislocation, fracture, inactivity, and infection, which often necessitates surgical relocation, prosthetic removal, and reimplantation, differentially.Citation7 But there is less than universal consensus on this issue.
A further body of research shows that being overweight, as well as underweight, may be quite prevalent among adults of both genders undergoing total hip replacement,Citation8–Citation11 and that as shown in , there is both an increasing incidence of obesity in the population, and among patients undergoing primary Charnley hip replacement. Hence, given that total hip replacement surgery is the most common intervention for disabling hip osteoarthritis, but that dealing with complications post-operatively is extremely costly to the patient as well as the hospital and society as a whole, it seemed reasonable to investigate whether there is likely to be any possible post-operative risk to total hip replacement surgery related to body weight distribution, and if so, what are possible implications of this for those who perform and require total hip replacement.Citation12
Table 1 Table depicting study findings as regards the role of body mass in the context of hip joint osteoarthritis in general
Study aims
The first study aim was to examine whether patients with post-surgical complications are likely to constitute a sizeable proportion of patients with disabling hip joint osteoarthritis hospitalized at any point in time for hip joint surgery. A second aim was to examine the nature of these complications and their frequency of occurrence. A third aim was to examine if these complications would be likely to vary by age, numbers of prevailing comorbidities, and body mass among other factors. That is, the study sought to provide a better understanding of the potential influence of age, body mass and health status with respect to complications that can occur after total hip replacement, and their expected frequency of occurrence.
It was anticipated that by carefully examining the extent of this problem, and by identifying salient factors that might explain or place community dwelling elders at risk for complications after primary total hip replacement surgery, some insight into opportunities worthy of further study in the context of improving the clinical outcomes and reducing the costs of complications after primary total hip replacement surgery might be forthcoming. Based on an in-depth literature review, it was anticipated a sizeable volume of the present cases would be overweight, rather than underweight or of normal body weight, regardless of sub-group diagnosis. It was also anticipated that those hospitalized with complications from previous surgery would exhibit higher rates of subnormal body mass characteristics than those without complications, and that this could differ depending on the type of complication identified.
While various other risk factors for poor post-hip arthroplasty outcomes exist, body mass, an important proxy for health status was targeted given the prevailing support in the literature that this variable may be biomechanically and metabolically related to the development of complications post-hip arthroplasty. In particular, the impact of subnormal body mass indices as outlined in the literatureCitation9,Citation13 was specifically assessed because this variable is one which is potentially modifiable. Due to difficulties in conducting prospective studies in this area, a retrospective cross-sectional analysis was undertaken because of its descriptive value when exploring a phenomenon and formulating hypotheses.
Methods
All the available medical records charted over a 10 month period and drawn from a parent study of hip arthroplasty outcomes, but with no active patient involvement were examined to ensure the records were complete and patients had a diagnosis of osteoarthritis of one or both hips that required primary or secondary surgeries.
Study sample
The study cohort selected was a sample of 1,040 males and females between the ages of 23–89 years diagnosed as having definitive clinical and radiographic evidence of osteoarthritis of one or both hip joints. All were hospitalized for purposes of primary hip replacement (prosthetic) surgery or for complications related to prior prosthetic surgery or problems with one or both hips over a 10 month period in 2000.
Procedures
To obtain the desired information, data pertaining to the patient’s were extracted by the researcher from the charts in a systematic way. These data included measures of the patients’ body mass index (BMI), an indicator of fatness that represents the ratio of the subjects weight to the square of their height (w.h−2), as well as pertinent demographic variables, including age, gender, reason for hospital admission, baseline functional status, and comorbid status were noted. In addition subjects were categorized as presenting for primary surgery or with a complication related to prior surgery. If a complication was identified, the specific complication noted on the chart, including infection, periprosthetic fracture, dislocation, and the term ‘revision’, which referred to the aseptic loosening of an arthroplasty cup, stem or both, and duration since first surgery, was recorded. These data were entered onto an Excel (Microsoft Corp., Redmond, WA) spreadsheet and were transposed thereafter into SPSS (version 16.0; SPSS Inc., Chicago, IL) files. SPSS programming was then used to describe the sample and to analyze differences in the age and body mass distributions and related variables among the observed subgroups of hip osteoarthritis surgical candidates using chi-square tests, cross-tabulations, and analysis of variance, as indicated. An a priori significance level of 0.05 was adopted.
Results
Demographic and clinical characteristics
The subjects studied were predominantly Caucasians, mean age 65.4 ± 13.0 years and 60% were women. Approximately 20% or 200% cases were hospitalized for purposes of primary hip joint surgeries on the contralateral side or because they had experienced ipsilateral complications related to prior primary total hip replacement surgeries. As shown in depicting the six key reasons for re-hospitalization, the most common was some form of aseptic loosening of the initial prosthesis that required revision. also shows that in addition to the differing rates of complications that were observed, the mean age of patients experiencing these problems tended to vary and was highest for those hospitalized due to prosthetic and periprosthetic fractures and contralateral hip surgery.
Table 2 Table depicting global rates and major categories and related sub-categories and rates of occurrence among these major diagnostic groups plus the mean age of each major group as observed among 1040 hospitalized patients with primary or secondary total hip replacement diagnoses showing different types of complications and reasons for hospitalization, as well as subtle differences in mean ages across conditions
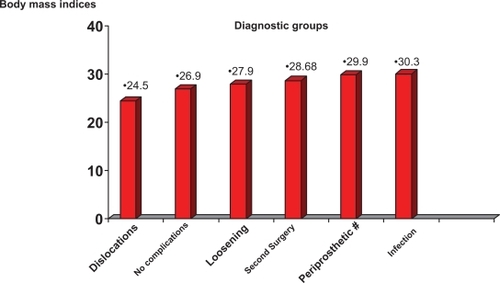
Body mass
In terms of body mass, and consistent with observations of several previously reported group characteristics, the hip osteoarthritis cases with no prior hospitalization history were predominantly overweight. Likewise, those with complications requiring re-hospitalization were generally overweight rather than of normal weight (60% vs 34%). Moreover, the mean BMIs of 29.8 ± 6.3 recorded for those with infection histories, regardless of diagnostic category, were significantly greater than the index of 26.7 ± 5.4 recorded for those with no infection (p = 0.001; equal variances assumed). As shown in , the mean BMI of those hospitalized for infections warranting removal or reimplantation procedures was higher than that of the other subgroups and those with no surgical complications (p = 0.004).
Figure 1 Body mass indices of hip osteoarthritis cases categorized by surgical requirements showing significant differences (p < 0.05) between those requiring reimplantation or removal and those requiring relocation due to dislocation.
The body mass indices defined as obese if this was greater or equal to 30 kg.m−1; overweight if body mass indices were 25–29 kg.m−1 or normal weight if less than 25 kg.m−1 showed that consistent with others, those who experienced infections were more likely to be overweight or obese than of normal weight (81% vs 18%). Those with periprosthetic fractures were also more likely to be overweight or obese than those requiring primary surgery or revision hip arthroplasty who were moderately overweight on average. No subject classified as being underweight was being hospitalized for an infection-related problem.
Conversely, a higher proportion of patients undergoing revisions for dislocation and/or prosthetic relocations were likely to be underweight (BMI < 20 kg.m−1) when compared to those hospitalized for second surgeries, prosthetic reimplantation, removal and periprosthetic fractures (p < 0.05) (see ). The body mass indices for the nine cases with primary dislocation histories ranged from 18–43. For the approximately half of the cases hospitalized with a dislocation history who had recurrent dislocation histories (N = 10), their body mass indices ranged from 19–33 suggesting that being excessively underweight or obese may place some hip arthroplasty cases at risk for persistent complications.
Comorbid conditions
In association with the aforementioned variations in body mass distributions within the observed sub-groups, patients hospitalized due to dislocated or infected prostheses, as well as for periprosthetic fractures, were more likely to have a higher prevalence of comorbid conditions than those who required revision surgery or primary hip osteoarthritis, but this was not statistically significant. Those with infected hips who had experienced complications within a range of two months to 11 years after initial surgery, had either none, one or more comorbid diseases. Those hospitalized with dislocated prostheses had had their first surgeries 1–3 years prior to their current hospitalization, while time to aseptic loosening or experiencing a periprosthetic fracture was generally longer than that of the median time to infection or dislocation and ranged from 15–25 years.
Pre- and post-surgical trends
In terms of their overall pre-surgical subjective pain experience as evaluated on a 4-point Likert scale where 1 = mild pain and 4 = severe pain, an unexpected finding was that overall pain was reported to be 25%–50% less intense in those with dislocation and periprosthetic fracture histories (mean = 2.0) compared to those with infections (mean = 3.2) and those with requiring revision surgery (mean = 4.00, p = 0.088).
In addition, compared to patients with secondary infections requiring removals who generally had a very limited ability to flex their hips when compared to the other major subgroups, the most mobile groups were those with primary or recurrent dislocations. The difference in flexion range of motion between those with infections of 68.6 ± 8.3 and those with dislocations of 98.1 ± 7.8 was significant (p = 0.012).
In terms of baseline presentation, pre-surgical walking capacity as indicated by maximum number of blocks a patient could complete also differentiated the subgroups and was more limited among the cases re-admitted with an infection diagnosis than those undergoing primary hip replacement (0.3 blocks versus 3.9 blocks, p = 0.002). On the third post-surgical day, the distance walked by patients was 50% lower among the group who underwent removals and replacements for infections than those undergoing surgery for the first time (p = 0.048). The patients with secondary infections and surgeries also stayed in hospital longer, and required rehabilitation more often than the other patients upon hospital discharge.
Gender
Overall, although more females were undergoing surgery for the first time than males, gender did not seem to be a factor placing patients at risk for revision. There were significantly more females with a diagnosis of dislocation and more males with a diagnosis of periprosthetic fracture and infection (p ≤ 0.05).
Discussion
Minimizing the disability and related burden experienced by older adults who are commonly at risk for or already suffering from hip joint osteoarthritis is of growing importance in an aging society. While hip joint replacement surgery is often very helpful in this respect, hip joint replacement surgery clearly remains subject to a variety of post-operative complications and variable implant survival rates that can impact desired health outcomes adversely. The present aim was to specifically examine rates of post-operative hip complications, the nature of these, and factors that may reduce the success rate of total hip replacement surgery in the context of an urban orthopedic center with an active and progressive hip replacement surgery program. The goal was to identify factors that might further improve a patient’s well-being and health in the course of undergoing total hip replacement surgeryCitation2 and to try to resolve some discrepant views about body mass and its potential influence on perioperative hip replacement complication rates.Citation14,Citation15
The approach taken was that this would be an exploratory study, and that if any trends in the observed data emerged, these could be useful for guiding future research. Although the sample was primarily one of convenience, and patients in this current analysis were mostly Caucasian men and women, it was believed they would be reasonably representative of the type of patient commonly receiving a hip replacement in the context of modern urban orthopedic hospital settings. Moreover, although the present data set may be skewed because some successful cases may not have been included in the analysis due to missing files and incomplete hospital records, and more patients with complications than is commonly found in the population may have been observed due to the nature of the hospital and its expertise, as outlined in , it does appear a fair proportion of patients with hip osteoarthritis who undergo hip replacement surgery can be expected to experience post-surgical complications, despite excellent overall results. This finding was also observed by Mahomed and colleaguesCitation16 for a United States Medicare population, and by Malchau and colleaugesCitation17 for a Swedish population, and while these complications vary, the trends presently observed were generally consistent with several current reports in the related literature and those reported in .
Table 3 Table depicting study findings as regards the role of body mass in the context of complications following total hip replacement surgery
However, because it is very challenging to follow controls who experience the same survival time but do not incur complications, and survival time does not appear to be the same for the different common post-operative complications observed, the reasons why post-surgical complications continue to prevail, why some forms of complication are more commonly observed than others and the specific risk factors involved remains unclear in the context of hip replacement surgery for disabling hip joint osteoarthritis. The present work thus focused specifically on ascertaining the extent to which complications following hip joint replacement surgery might prevail, the nature of these, and whether age, comorbid status and body mass might explain variations in the outcomes of such surgery. The extent to which these complications add to the burden of the disease was also a point of interest. While there is support for a correlation between obesity and post-hip surgery complications as outlined by Lübbeke and colleaguesCitation13 and Joshi and colleaguesCitation18 who showed linear wear was positively correlated with body weight, those presently analyzed, while somewhat overweight, were generally comparable in weight to those undergoing primary hip arthroplasty surgery as noted by McLaughlin and Lee,Citation19 and Haverkamp and colleagues.Citation15 Consistent with Effenberger and colleagues,Citation20 obesity did not seem to predominate among those requiring revision surgery, and their protracted survival times compared to those with infection diagnoses, suggested prosthetic ‘wear and tear’ rather than excess body weight alone explained this complication.
By contrast, those 24% of hip replacement patients with complications who were re-admitted with infection diagnoses generally had shorter arthroplasty survival rates than those requiring revision surgery, even though they should have had a generally equal chance of comparable prosthesis survival rates. They also had higher overweight and obesity rates than those requiring revision surgery with no infection history, suggesting mechanical wear and tear may be accelerated in those with excess body mass. Indeed, several cases with infection diagnoses were morbidly obese, and several had recurrent infection histories. They were also more likely to have one or more comorbid conditions, and to be more impaired than those with no infection history as discussed by Choong and colleaguesCitation21 and Dowsey and Choong.Citation22 Also noteworthy was that this group required a significantly increased length of hospital stay compared to the other hospitalized groups, which is consistent with MacWilliam and colleaguesCitation23 and Pulido and colleagues.Citation24 These observations also appear consistent with comparable findings of others outlined in , the significantly diminished functional outcomes these individuals may experience as outlined by Lübbeke and colleagues,Citation25 and the need to investigate and treat all potential determinants of this very disabling problem.
Another less commonly observed patient subgroup, namely those with diagnoses of periprosthetic fractures also tended to be overweight or obese rather than of normal weight. While patient demographics, a variety of clinical characteristics and surgical procedures may underpin this specific post-operative problem, it is unclear why periprosthetic fractures, while uncommon after hip arthroplasy, are increasing in number and severity.Citation26 These disturbances, which are serious and costly, may involve stress fractures of the pubis or medial wall, significant bone loss secondary to osteolysis and subsequent loss of column integrity, or complete pelvic discontinuity.Citation27 They may occur due to trauma or without significant trauma as outlined by Katzer and colleagues.Citation26 They may also occur as a result of bone weakening and loosening of the prosthesis stemCitation18 and the use of small hip replacement components in patients with a high body mass.Citation28 It is possible too, there may be some age-related factor, along with trauma that raises the risk for this complication, as this subgroup was significantly older than the others, and the patients’ charts revealed all had recent fall-related histories and a majority were overweight.
Dislocations, which occurred in about 10% of the cases with complications, and in varying time frames from initial surgery were also potentially influenced by body mass and its impact on the distribution of joint load as outlined in and . In addition to influencing joint loading, surgery may also be more problematic in either the overweight or extremely underweight candidate because of its impact on the long-term healing process, even though a short-term study has suggested no impact of body mass on early outcome or hospital length of stay.Citation29 Many candidates who are extremely overweight or underweight are also likely to be in poor health in general due to the presence of one or more comorbid conditions and/or the presence of past hip fractures, congenital joint problems, or trauma and may be more prone to developing problems related to implant failure and dislocation as a result. Patients who experience high dislocation rates may also include those who do not even sense there is any problem until they can no longer function because they do not perceive this situation in terms of pain, as was presently observed and thus early detection is unlikely.Citation30
Figure 3 Possible role of obesity in mediating complications post-hip replacement surgery among hip osteoarthritis patients.
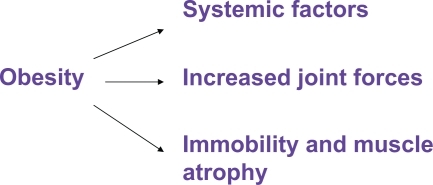
Figure 4 Possible role of low body mass in mediating complications post-hip replacement surgery among hip osteoarthritis patients.
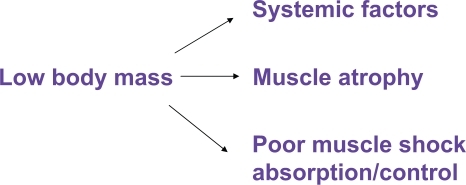
In summary, while patients differ in their pre-surgical functional abilities, age at admission and morphology, and not all are susceptible to complications after hip replacement surgery, the immense costs of complications to the individual and hospital when they occur demands more be done to understand and prevent or reduce these. In light of the present observations, the 1994 observations by Woolf and colleaguesCitation31 and that being obese may impact the success of hip replacement surgery in a negative wayCitation14,Citation32 especially in younger patients with unrestricted mobility,Citation33 it seems this is one factor worthy of further exploration. Moreover, a growing literature indicates that being overweight may be associated with the need for total hip replacement.Citation9,Citation10,Citation34 Other patients undergoing this form of surgery, such as those with a prior hip fracture injury, are a group often found to be frail and underweight, and these features may explain why a moderate percentage of these cases are likely to experience aseptic loosening, and/or infection, periprosthetic fractures and especially dislocations.Citation35
Thus even though this present research is limited in that it was done largely retrospectively with only a limited follow up period, cases were not strictly matched on the time of the hip replacement, and the information presented was dependent on accuracy of the chart records and measurement approaches, the possibility that body mass, a modifiable factor may be a predictor of some common deleterious post-hip replacement surgical outcomes such as infections, periprosthetic fractures and dislocations, should not be ignored. As well, it is possible there are age and gender-specific differences in risk for some complications and these warrant further study. As well, even though revision surgery at the hip may not be driven by weight factors per se,Citation19 obesity was also found by Lübbeke and colleaguesCitation13 to be strongly associated with unfavorable outcomes after revision, and more research to see if weight control and careful radiological and clinical follow-up will reduce the prevalence of these complicationsCitation36,Citation37 may be fruitful. There may also be a decreased need for total hip replacement or the possibility of delaying this till later on in life through dietary and exercise intervention and/or better recovery after surgery,Citation38 and this avenue warrants further study.Citation39
Conclusion
Complications that occur after surgical replacement of a hip joint for painful disabling osteoarthritis are costly and potentially preventable conditions. While the literature on this topic remains equivocal, it is possible that common complications such as infections, periprosthetic fractures and dislocations are more likely to arise in patients who are excessively over or underweight. Other factors that need to be examined in well-designed case control studies include the potential role of age, gender, comorbid disease profile, trauma and extent of prevailing joint pain, among other factors. Given that primary hip osteoarthritis cases are growing in number and these patients are more than likely to be overweight than of normal weight, concerted efforts to examine the relative risks of failure after total hip replacement where body mass is clearly too high, or too low, seems highly advisable. In addition to well designed case control studies of hip prosthesis cases who do and do not experience complications, prospective studies to tease out the predictive validity of some of the aforementioned risk factors and to examine if it is possible to improve upon current outcomes and reduce costs associated with end-stage hip osteoarthritis may be especially fruitful.
Disclosure
The author reports no conflicts of interest in this work.
References
- AnissianHLIn vitro evaluation of hip prostheses Doctoral Thesis. Karolinska Institute2001
- MarchLMCrossMJLapsleyHOutcomes after hip or knee replacement surgery for osteoarthritis. A prospective cohort study comparing patients’ quality of life before and after surgery with age-related normsMed J Aust199917123523810495753
- SegalAKraussESInfected total hip arthroplasty after intravesical bacillus Calmette-Guérin therapyJ Arthroplasty200722575976217689788
- ParviziJTarityTDSlenkerNProximal femoral replacement in patients with non-neoplastic conditionsJ Bone Joint Surg Am20078951036104317473141
- BerendKRLombardiAVJrMalloryTHAdamsJBRussellJHGrosethKLThe long-term outcome of 755 consecutive constrained acetabular components in total hip arthroplasty examining the successes and failuresJ Arthroplasty2005Suppl 39310216214009
- IkemaMOyamaMKitaAFunayamaKPoor results of the cementless total hip arthroplasty with a nonporous coated acetabular component: AcSys Shearer CupJ Orthop Sci20071246647017909932
- YoungNLCheahDWaddellJPWrightJGPatient characteristics that affect the outcome of total hip arthroplasty: a reviewCJS19984188195
- JacobsenSSonne-HolmSIncreased body mass index is a predisposition for treatment by total hip replacementInt Orthop20052922923415856229
- FlugsrudGBNorslettenLEspehaugBHavelinLIMeyerHERisk factors for total hip replacement due to primary osteoarthritis: a cohort study in 50,034 personsArthritis Rheum20024667568211920403
- HarmsSLarsonRSahmounAEBealJRObesity increases the likelihood of total joint replacement surgery among younger adultsInt Orthop200731232616688455
- AlfonsoDTHowellRDCaceresGKozlowskiPDi CesarePETotal hip arthroplasty in the underweightJ Arthroplasty200823795695918534502
- WroblewskiBMSineyPDFlemingPAIncreasing patients’ body mass. Are the criteria for testing stemmed femoral components in total hip arthroplasty still valid?Proc Inst Mech Eng [H]20072218959961
- LübbekeAKatzJNPernegerTVHoffmeyerPPrimary and revision hip arthroplasty: 5-year outcomes and influence of age and comorbidityJ Rheumatol20073439440017143967
- Sadr AzodiOSAdamiJLindstromDErikssonKOWladisABelloccoRHigh body mass index is associated with increased risk of implant dislocation following primary total hip replacement: 2,106 patients followed for up to 8 yearsActa Orthop20087914114718283586
- HaverkampDde ManFHde JongPTvan StralenRAMartiRKIs the long-term outcome of cemented THA jeopardized by patient’s being overweight?Clin Orthop Relat Res20084661162116818288553
- MahomedNNBarrettJAKatzJNRates and outcomes of primary and revision total hip replacement in the United States medicare populationJ Bone Joint Surg Am200385273212533568
- MalchauHHebertsPEislerTGarellickGSodermanPThe Swedish Total Hip Replacement RegisterJ Bone Joint Surg Am200284Suppl 222012479335
- JoshiAIlchmannTMarkovicLSocket wear in bilateral simultaneous total hip arthroplastyJ Arthroplasty20011611712011172281
- McLaughlinJRLeeKRThe outcome of total hip replacement in obese and non-obese patients at 10- to 18-yearsJ Bone Joint Surg Br2006881286129217012415
- EffenbergerHRamsauerTDornUImhofMFactors influencing the revision rate of Zweymueller acetabular cupInt Orthop20042815515815054674
- ChoongPFMDowseyMMCarrDDaffyJStanleyPRisk factors associated with acute hip prosthetic joint infections and outcome of treatment with a rifampin-based regimenActa Orthopaedica20077875576518236181
- DowseyMMChoongPFMObesity is a major risk factor for prosthetic infection after primary hip arthroplastyClin Orthop Relat Res200846615315818196388
- MacWilliamCHYoodMUVernerJJMcCarthyBDWardREPatient-related risk factors that predict poor outcome after total hip replacementHealth Serv Res199636236388943994
- PulidoLGhanemEJoshiAPurtillJJParviziJPeriprosthetic joint infectionClin Orthop Relat Res20084661710171518421542
- LübbekeAMoonsKGMGaravagliaGHoffmeyerPOutcomes of obese and nonobese patients undergoing revision total hip arthroplastyArthritis Rheum20085973874518438918
- KatzerAInceAWodtkeJLoehrJFComponent exchange in treatment of periprosthetic femoral fracturesJ Arthroplasty20062157257916781412
- HelfetDLAliAPeriprosthetic fractures of the acetabulumInstr Course Lect200453939815116603
- HarviePHaroonMHendersonNEl-GuindiMFracture of the hydroxyapatite-ceramic-coated JRI-Furlong femoral component: body mass index and implications for selection of the implantJ Bone Joint Surg Br20078974274517613497
- KesslerSKäferWOverweight and obesity: two predictors for worse early outcome in total hip replacement?Obesity2007152840284518070776
- RoderCEggliSAebiMBusatoAThe validity of clinical examination in the diagnosis of loosening of components in total hip arthroplastyJ Bone Joint Surg B2003853744
- WoolfVJCharnleyGJGoddardNJWeight changes after total hip arthroplastyJ Arthroplasty199493893917964770
- KimYMorshedSJosephTBozicKRiesMDClinical impact of obesity on stability following revision total hip arthroplastyClin. Orthop Rel Res2006453142146
- MüngerPRöderCAckermann-LiebrichUBusatoAPatient-related risk factors leading to aseptic stem loosening in total hip arthroplasty: a case-control study of 5, 035 patientsActa Orthop20067756757416929432
- KarlsonEMandlLGideonASanghaOLiangMHGrodsteinFTotal hip replacement due to osteoarthritis: the importance of age, obesity, and other modifiable factorsAm J Med2003114939812586227
- MeekRMDAllanDBMcPhillipsKerrLHowieCREpidemiology of dislocation after total hip arthroplastyClin Orthop Rel Res2006447918
- BusatoARoderCHerrenSEggliSInfluence of high BMI on functional outcome after total hip arthroplastyObesity Surgery20081859560018369684
- NambaRSPaxtonLFithianDCStoneMLObesity and perioperative morbidity in total hip and total knee arthroplasty patientsJ Arthroplasty200520465016214002
- NaylorJMHarmerARHeardRCSevere other joint disease and obesity independently influence recovery after joint replacement surgery: an observational studyAustral J Physiother2008545764
- FelsonDTChaissonCEUnderstanding the relationship between body weight and osteoarthritisBaillieres Clin Rheumatol19971146716819429730
- ChangulaniMKalairajahYPeelTFieldREThe relationship between obesity and the age at which hip and knee replacement is undertakenJ Bone Joint Surg (Br)200890B36036318310761
- JärvholmBLewoldSMalchauHVingårdEAge, bodyweight, smoking habits and the risk of severe osteoarthritis in the hip and knee in menEur J Epidemiol20052053754216121763