Abstract
The pathogenesis of asthma and chronic obstructive pulmonary disease (COPD) has been claimed to be attributable to increased systemic and local oxidative stress. Detection of the oxidant burden and evaluation of their progression and phenotypes by oxidant biomarkers have proved challenging and difficult. A large number of asthmatics are cigarette smokers and smoke itself contains oxidants complicating further the use of oxidant biomarkers. One of the most widely used oxidant markers in asthma is exhaled nitric oxide (NO), which plays an important role in the pathogenesis of asthma and disease monitoring. Another oxidant marker that has been widely investigated in COPD is 8-isoprostane, but it is probably not capable of differentiating asthma from COPD, or even sensitive in the early assessment of these diseases. None of the current biomarkers have been shown to be better than exhaled NO in asthma. There is a need to identify new biomarkers for obstructive airway diseases, especially their differential diagnosis. A comprehensive evaluation of oxidant markers and their combinations will be presented in this review. In brief, it seems that additional analyses utilizing powerful tools such as genomics, metabolomics, lipidomics, and proteomics will be required to improve the specificity and sensitivity of the next generation of biomarkers.
Asthma and chronic obstructive pulmonary disease (COPD) are diseases with different physiological and anatomical features. However, a significant number of patients suffering from these diseases exhibit symptoms and signs which are associated with both conditions. Markers of the elevated oxidant burden have been detected in both of these disorders. This degree of overlap between asthma and COPD has proved to be especially important in smoking asthmatics, patients who have often been excluded from asthma trials and investigations. Oxidant markers are under intensive investigation as ways of assuring the early detection and monitoring of asthma and COPD, for the differentiation of the disease from the condition of “healthy smokers”, and also for the evaluation of the COPD phenotypes and their progression. This review will critically review potential markers that reflect oxidative stress in the airways of patients with asthma and COPD in exhaled air, exhaled breath condensate (EBC) and induced sputum. In addition, markers in bronchoalveolar lavage (BAL) will also be briefly surveyed, even though the technique, ie, fibreoptic bronchoscopy is an invasive technique used in the investigation of lung inflammation and the evaluation of the oxidant burden. In this review, we will also discuss the pros and cons of various noninvasive biological samples for assessing the oxidant burden in the airways, and then speculate on the possibilities of using the existing and new oxidant markers, their potential combinations, and make suggestions for future investigations.
Clinical and inflammatory features of asthma and COPD
According to the Global Initiative for Asthma Guidelines (CitationGINA 2002) asthma is defined as a chronic inflammatory disorder of the airways in which many cells and cellular elements play a role. The chronic inflammation evokes an associated increase in airway hyperresponsiveness that leads to recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night or in the early morning. These episodes are usually associated with widespread but variable airflow obstruction that is often reversible, either spontaneously or with treatment. In the Global Initiative for Chronic Obstructive Lung Disease Guidelines (CitationGOLD 2002; CitationRabe et al 2007), COPD is defined as a preventable and treatable disease state characterized by airflow limitation that is not fully reversible. COPD is also associated with emphysematous parenchymal destruction, variable loss of lung elastic recoil, and abnormalities in gas diffusion. The physiological findings in individual patients with either clinical asthma or COPD, when isolated from the context of their environmental and clinical histories, may not allow the physician to distinguish between the conditions (CitationBoulet et al 1998; CitationFabbri et al 2003). This inability to clearly differentiate these conditions can lead to frustration in both the clinic and research settings.
There are a large number of studies and reviews on the inflammatory profile in asthma and COPD (CitationKirby et al 1987; CitationWalters and Gardiner 1992; CitationKeatings and Barnes 1997; CitationChanez et al 1999; Citationvan Aalderen et al 1999; CitationGibson et al 1999; CitationJeffery 1999; CitationSaetta 1999; CitationNHLBI/WHO 2002; CitationLoh et al 2005; CitationTetley 2005). Airway inflammation is present in all forms of asthma, even in mild (CitationBattaglia et al 2005) and asymptomatic cases (CitationBousquet et al 2000; CitationMontuschi et al 2004) and it can be detected in both central and peripheral airways (CitationHamid et al 1997) in asthma. There is a strong association between fractional exhaled nitric oxide (FeNO) and skin prick test scores, total immunoglobulin E (IgE) (CitationHo et al 2000) and blood eosinophilia (CitationSilvestri et al 1999). In contrast, COPD is a disease characterized by airway inflammation with neutrophil predominance (CitationBosken et al 1992), and periods of acute exacerbations (CitationFletcher and Peto 1977) with further increased airway inflammation and worsening of lung function (CitationGompertz et al 2001). Cigarette smoking is the major risk factor for development of COPD, and smoking cessation is at present the only effective way to slow down the disease progression (CitationCulpitt and Rogers 2000; CitationScanlon et al 2000). COPD exacerbations are often triggered by viral or bacterial infections consisting not only of increased numbers of neutrophils, but also of eosinophils and activated macrophages in the airways (CitationRahman and MacNee 2000; CitationSaetta et al 2001). Neutrophil accumulation on the other hand is one typical feature that is seen in asthma exacerbation (CitationFahy et al 1995a; CitationKim et al 2000). There is overlap not only in the inflammatory profile but also in the oxidant markers, especially in acute asthma and COPD exacerbations. The present review focuses on oxidant markers, but the numbers of certain inflammatory cells and the levels of cytokines have also been found to be significantly correlated with oxidant markers in the airways of patients with asthma and COPD.
The differential diagnosis of asthma and COPD is especially difficult in smoking individuals. Cigarette smoke activates macrophages and polymorphonuclear leukocytes to produce more reactive oxygen species (ROS) and this, in turn, leads to the recruitment of leukocytes into the airways (CitationNiewoehner et al 1974; CitationHoidal and Niewoehner 1982). Since symptoms and lung function tests are indirect methods to assess the disease severity both in asthma and COPD, they may not reveal the extent of the underlying airway pathology. Smoking alone has multiple effects on the airways and there is a need to clearly differentiate the effects of smoking from the disease and its progression, a topic that has not been systematically evaluated.
Biomarker requirements in asthma and COPD differentiation
Oxidative stress has been claimed to be involved in the development of both asthma and COPD (CitationKharitonov and Barnes 2001b; CitationMontuschi et al 2004; CitationKinnula 2005a; CitationRahman and Adcock 2006). There is more than one phenotype in COPD and asthma and these phenotype subtypes have not been separately evaluated with respect to the profiles of the oxidative stress burden are influenced in the different phenotypes. Currently, there is plenty of research being conducted to develop noninvasive tools for disease detection and follow-up, eg, easy-to-use devices and sensitive and specific technologies. Only practical and readily reproducible, completely noninvasive techniques offer these possibilities. The biomarkers themselves must possess certain characteristics if they are to be of any use. In addition to sensitivity and specificity, a biomarker needs to be stable, with minimal diurnal or day-to-day variability, and it should be easy to access and analyse, and still be cost-effective. Furthermore, the biomarkers should be useful for early diagnostics, differential diagnosis, response to therapy, and for the evaluation of disease progression. It is unlikely that any single biomarker can ever possess all these characteristics. Instead, panels or various combinations of biomarkers are needed. These panels could consist of different components if they are used for either the differential diagnosis or for the assessment of disease severity and its progression.
Oxidative stress in the airways in asthma and COPD
ROS and reactive nitrogen species (RNS) are produced endogenously by several cell types including activated inflammatory and structural cells, the most potent generators of these species being eosinophils and neutrophils, ie, cells that are abundant both in asthma and COPD (CitationKinnula 2005b). The burden of ROS/RNS is further increased by exogenous factors, mostly by environmental agents and cigarette smoke. One puff of cigarette smoke contains billions of free radicals (CitationChurch and Pryor 1985). These ROS, present both in asthma and smoking-related airway diseases, have multiple effects including activation of proteases, mucus secretion, airway smooth muscle contraction, airway hyperresponsiveness, and transcription of many inflammatory genes (CitationKawikova et al 1996; CitationRahman and MacNee 1998; CitationParedi et al 2002; CitationWood et al 2003).
Oxidants present in cigarette smoke stimulate alveolar macrophages to further produce ROS, such as superoxide radical (O2•−), hydroxyl radical (•OH), and hydrogen peroxide (H2O2), leading to release of a number of mediators, some of which attract neutrophils and other inflammatory cells into the lungs of COPD patients (CitationGOLD 2002). Activated inflammatory cells generate more ROS via the NADPH oxidase system. Similarly, increased levels of xanthine oxidase, found in cell free bronchoalveolar lavage (BAL) fluid and plasma from COPD patients, can elevate O2•− and lipid peroxide levels (CitationGOLD 2002). Thus, oxidants may be triggering factors for the inflammation seen in COPD. Asthma on the other hand, may be triggered by viral infections, air pollutants such as ozone and cigarette smoke, and other cellular mediators (CitationDworski 2000). These agents cause influx and activation of inflammatory cells (macrophages, neutrophils, eosinophils, lymphocytes, and mast cells) which subsequently evoke the generation of inflammatory mediators. All of these converge to produce ROS which in turn leads to an increased inflammatory response, producing asthma-like symptoms. Oxidative stress is associated with activation of cytokines/growth factors but in these same conditions activated inflammatory cells produce large amounts of ROS into the airways. Thereby it can be postulated that symptoms are not only linked to the airway inflammation but also to the oxidant burden in the airways both in asthma and COPD. ROS have been shown to be associated with the pathogenesis of asthma by evoking bronchial hyperreactivity as well as directly stimulating histamine release from mast cells and mucus secretion from airway epithelial cells (CitationDworski 2000). Thus, while oxidative stress due to smoking is a direct causative factor for COPD leading to a further elevation of oxidative stress, it is usually a secondary effect in asthma subsequent to a prior antigenic/allergic challenge of immune cells in the lungs.
Once oxidative stress reaches a critical level, it is difficult to demarcate between the two diseases asthma and COPD. However, site of affliction, the cells involved and the pattern of response by the lungs can help in differentiating these two diseases. In COPD, the major site of attack is the alveolar space. Inflammatory cells themselves become compartmentalized, for example, neutrophils are mainly located in the lumen of the airways and macrophages accumulate in the interstitium in COPD. COPD has been strongly associated with an accumulation of inflammatory mucous exudates in the lumen of the small airways (CitationSaetta et al 2001). In COPD, oxidant stress occurs in small airways, lung parenchyma, and the alveolar regions. In asthma, the larger airways are the major site of action, with the characteristic signs being reversible airflow obstruction, airway hyperresponsiveness/hyperreactivity, and chronic inflammation attributable to an influx of eosinophils and activation of inflammatory cells such as macrophages, neutrophils, lymphocytes, and mast cells. Airway smooth muscle contraction, increased airway reactivity and secretions, increased vascular permeability and increased generation of chemoattractants are the major features of an asthmatic response (CitationHamid et al 1997). Hence, compartmentation of different inflammatory cells in the lungs may help clarify the type of oxidative stress response in asthma and COPD.
Many oxidants (such as O2•− and •OH) are unstable and have very short half lives, and are therefore difficult to measure. Hydrogen peroxide (H2O2) is formed from superoxide (mainly by inflammatory cells including both eosinophils and neutrophils) and is directly involved in many reactions. NADPH oxidase is one of the key superoxide generating enzymes that is expressed both in phagocytic and nonphagocytic cells (CitationJones et al 2000). NADPH oxidases (NOXs) and dual oxidases (DUOXs) may function as potent ROS generators in inflammatory conditions of human airways, but little is known about their role in asthma or COPD. Myeloperoxidase (MPO) is abundantly present in neutrophils and catalyses the reaction of H2O2 with chloride forming hypochlorous acid (HOCl). Eosinophil peroxidase (EPO) catalyses the reaction of H2O2 with bromide within eosinophils forming hypobromous acid (HOBr), which is released during the respiratory burst (CitationWu et al 2000; Citationvan Dalen and Kettle 2001; CitationAldridge et al 2002). Endogenous NO is derived from L-arginine by at least three different isoforms of NOS (CitationNathan and Xie 1994). Two of these are expressed constitutively (NOS1, NOS3) while the inducible form of NOS (iNOS, NOS2) can be activated by inflammatory cytokines. Inducible NOS generates the majority of the NO encountered in inflammatory states since the enzyme is induced by cytokines and is expressed in inflammatory cells (like neutrophils) as well as in nonphagocytic cells (like alveolar/bronchial epithelial and endothelial cells) (CitationBarnes and Belvisi 1993). Once ROS are generated, they rapidly attack membrane lipids leading to the generation of lipid peroxidation products such as isoprostanoids, malondialdehyde, and 4-hydroxy-2-nonenal (4-HNE). These markers have been widely used in the assessment of oxidative stress in the lung (CitationKharitonov and Barnes 2001b; CitationParedi et al 2002), but a major limitation with most of these end products is their poor specificity and reproducibility in different diseases that are related to oxidative stress. Each of these markers will be discussed below in the context of their use in asthma and COPD diagnosis and differentiation.
The antioxidant machinery of the lung is complex, containing a variety of low molecular weight antioxidants, metal binding proteins, mucus glycoproteins, and several specific antioxidant enzymes (CitationKinnula et al 1995; CitationKinnula and Crapo 2003; CitationKinnula 2005a, Citation2005b). It is apparent that in oxidant-mediated airway diseases, ROS gradually overwhelm host antioxidant defenses, leading to the ultimate oxidant-mediated cell and tissue damage (CitationKinnula 2005b). Total antioxidant capacity of plasma is decreased in smokers and patients with asthma and COPD (CitationRahman et al 1996). It is interesting to note that the decrease in antioxidant capacity in smokers occurs transiently during smoking and resolves rapidly after smoking cessation. The depletion of total anti-oxidant capacity in smokers is associated with decreased levels of plasma antioxidants eg, ascorbic acid, vitamin E, β-carotene, and selenium (CitationRahman et al 1996). The depletion of antioxidants may thus be a reflection of ongoing oxidative stress due to underlying inflammation in these diseases. The thiol antioxidant glutathione (GSH) and its key biosynthesizing enzyme, glutamate cysteine ligase (GCL), are decreased in the airways, and in macrophages of smokers compared to nonsmokers (CitationHarju et al 2002a). However, very little is known about antioxidant enzymes/antioxidant biomarkers in asthma and COPD or their association with disease severity or progression. It is likely that there are no specific changes in the antioxidant systems during the early phases of airway diseases, instead their changes may reflect disease severity.
Noninvasive techniques to detect airway oxidative stress: Pros and cons
Exhaled air
Even though several methods have been developed to measure oxidant related damage/burden in cells, tissues, and body fluids, there has been great interest in the analysis of exhaled air since this is a totally noninvasive technique. Standardized measurements of fractional exhaled nitric oxide (FeNO) provide a noninvasive and reproducible means for monitoring asthma (CitationKharitonov et al 1997; CitationAnonymous 1999; CitationKharitonov 2004). A wide range of commercially available analyzers exist, which decreases the cost of individual measurements. Persistent generation of oxygen radicals in the body leads to the formation of other compounds, which can also be measured from the exhaled air; these include carbon monoxide (CO) which is formed by enzymatic degradation of heme aic degradation of heme aic degradation of heme aic degradation of heme aic degradation of heme aic degradation of heme and nonheme-related release (CitationKharitonov and Barnes 2001b) and hydrocarbons such as volatile organic compounds (VOC), which are nonspecific markers of lipid peroxidation (CitationKneepkens et al 1994). The activation of inflammatory cells, including macrophages, eosinophils, and neutrophils, results in increased production of O2•− and the subsequent formation of H2O2. H2O2 has been proposed to be a potential marker of oxidative stress in the lungs and this mediator has been evaluated in many investigations (CitationKharitonov 2004). In summary, exhaled air is one of the most promising ways for the assessment of oxidative stress; it has many advantages and the technology is now being developed so that there are portable devices at a relatively low cost. There exists, in addition, a good consensus on the significance of some oxidant markers (such as FeNO) that are detectable from the exhaled air.
Exhaled breath condensate
Exhaled breath condensate (EBC) is condensed from water but also contains droplets that carry solute from the lower respiratory tract. The collection of EBC by cooling exhaled air has several advantages compared to many other methods of sampling the airspaces. It is simple to conduct, noninvasive, and easily repeatable (CitationKharitonov and Barnes 2001b). It does not cause airway inflammation, nor does it have any significant influence on airway function (CitationBaraldi et al 2003c), making repeated sampling possible (CitationKharitonov and Barnes 2001b; CitationKharitonov and Barnes 2002). EBC collection is relatively inexpensive and does not include any appreciable discomfort or risk to the subject. Moreover, EBC collection is also suitable for children, because it is effort-independent. It can even be applied in mechanically ventilated patients. The collection of EBC has been described in detail (CitationRahman and Biswas 2004; CitationHorvath et al 2005). Many nonvolatile molecules (mediators, oxidation, and nitration products) can be measured in EBC, with 8-isoprostane being the most widely measured of the oxidant markers found in EBC (CitationKharitonov and Barnes 2001b). There is accumulating evidence suggesting that the abnormalities in biomarkers present in EBC may reflect the degree of asthma and COPD severity better than can be assessed by either spirometry or symptoms (CitationMontuschi et al 1999; CitationKharitonov and Barnes 2001b).
EBC mirrors the composition of the extracellular lining fluid (ELF) but the major drawbacks are saliva contamination, sample dilution, and high individual variability. There exists a lack of evidence of the primary origin of the aerosol particles that carry the droplets from the lower respiratory tract (CitationVan Hoydonck et al 2004). Dilution of EBC can be corrected by measuring the level of urea and/or electrolytes derived from ELF. Other confounding factors include consumption of alcohol, diets with variable amounts of antioxidants, smoking, subclinical lung diseases which have not been clinically manifested, and differences in the collection of the samples and their storage. Significant salivary contamination can be excluded by measuring the amylase concentrations in samples (CitationKharitonov and Barnes 2001b), but uncertainty still exists with respect to the nasal contamination. Recommendations for EBC have been formulated by the European Respiratory Society/American Thoracic Society task force, but these recommendations also emphasized the difficulties encountered in the sampling and analysis of EBC (CitationHorvath et al 2005). To date the majority of the analyses conducted in EBC have involved spectrophotometry and enzyme immunoassays, as well as sophisticated analytical techniques such as gas chromatography/mass spectrometry (GC/MS) or high-performance liquid chromatography (HPLC). Spin trapping is one of the most direct methods available for the assessment of highly reactive free radicals/oxidants. These latter techniques require special expertise and as far as we are aware, they have not been used for assaying EBC in clinical settings. In summary, the collection of EBC is easy and it is therefore promising for the evaluation of oxidant markers. Major limitations in the EBC include the plethora of potential markers that cannot be reliably or easily analyzed in these highly diluted samples.
Induced sputum
Induced sputum represents a nearly noninvasive technique; the collection of induced sputum by hypertonic saline has been shown to be a safe (CitationVlachos-Mayer et al 2000; CitationWark et al 2001), effective, and relatively reproducible (CitationPizzichini et al 1996; CitationWard et al 1999; CitationFahy et al 2001; CitationSimpson et al 2005) method for investigating airway diseases in adults (CitationPizzichini et al 1998; CitationWark et al 2002; CitationWilson et al 2006) and children over 6 years of age (CitationTwaddell et al 1996; CitationNorzila et al 2000). Induced sputum samples provide information about both inflammatory mediators and the inflammatory cells present in the airways (CitationSimpson et al 2005) and they are believed to accurately mirror conditions at the site of oxidative damage (CitationKelly et al 1999).
However, there is some evidence that induced sputum is sampled predominantly from the large airways (CitationAlexis et al 2001) and may not reflect the peripheral airways. Sputum induction is often difficult to accomplish, involves some discomfort to the patient, induces an inflammatory response (CitationNightingale et al 1998), and may induce coughing and bronchoconstriction in patients with COPD (CitationRytila et al 2000; CitationTaube et al 2001) and in asthma (CitationSmith and Anderson 1990; CitationAntczak et al 2005), despite pretreatment with an inhaled beta2-agonist (CitationRytila et al 2000; CitationPaggiaro et al 2002). The processing of the sputum sample needs to be immediate and requires expertise and this significantly limits its use in routine clinical practice. Sampling cannot be repeated within a short period of time, and the technique itself may induce an inflammatory response, which may persist for 24 h (CitationNightingale et al 1998; CitationHolz et al 1998). Contamination of sputum samples by saliva may lead to reduced mediator concentrations, although differential cell counts remain relatively unchanged (CitationSimpson et al 2004). On the other hand, several markers are relatively similar in the induced sputum and BAL and the technique of collecting induced sputum is much less invasive than fibreoptic bronchoscopy (CitationFahy et al 1995b). Overall, induced sputum is a standardized method and recommendations for sputum induction have been formulated by a European Respiratory Society/American Thoracic Society task force (CitationDjukanovic et al 2002). Induced sputum and its processing do require expertise that may be available in specialized centers though its use in a primary care setting would be demanding.
Bronchoalveolar lavage (BAL)
Bronchoalveolar lavage has the advantage of sampling the distal airways and alveoli in the lung periphery (CitationKelly et al 1987). However, BAL is more invasive than the above-mentioned procedures and has also several other limitations. The invasiveness of BAL limits its clinical application in assessing airway inflammation in asthma and COPD. Generally, BAL has been performed safely on patients with stable COPD (CitationHattotuwa et al 2002). BAL is, however, risky to patients with moderate/severe lung disease, acute exacerbations of airway disease and also is unsuitable for children. It is also associated with sedation, impaired gas exchange and a risk of infections. Even though the BAL technique has also been standardized (CitationHaslam and Baughman 1999), BAL fluid of COPD patients is often inadequate and not representative of the situation in the bronchioles due to airway collapse and reduced fluid recovery (CitationBarnes et al 2006). Saline instillation into the lungs can lead to artefacts, ie, the dilution of the lavage may contribute to the variability of measurements. BAL cannot be recommended for the diagnosis or follow-up of the patients with asthma or COPD.
Exhaled markers of oxidant burden in asthma and COPD
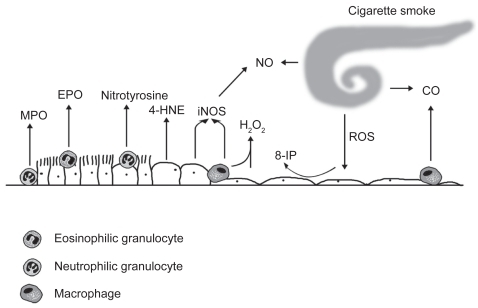
The markers of oxidant burden that have been generally measured from the human lung are shown in .
Figure 1 The markers of oxidative stress are derived from different cells and cell compartments in the alveolar or bronchiolar wall. Neutrophilic granulocytes express myeloperoxidase (MPO) and eosinophilic granulocytes are endowed with eosinophilic peroxidase (EPO). Inducible nitric oxide synthase (iNOS) is expressed in the inflamatory cells and bronchial epithelium. 4-hydroxy-2-nonenal (4-HNE) and 3-nitrotyrosine can be detected in a variety of cell types. Hydrogen peroxide (H2O2), nitric oxide (NO), carbon monoxide (CO), and 8-isoprostane (8-iso) represent widely investigated markers in the exhaled air/exhaled breath condensate.
Exhaled nitric oxide metabolites
Elevated FeNO levels have been widely documented in adults (CitationKharitonov et al 1994; CitationPersson et al 1994) and children (CitationLundberg et al 1996; CitationByrnes et al 1997; CitationNelson et al 1997) with asthma, even in mild and asymptomatic conditions (CitationAlving et al 1993; CitationKharitonov and Barnes 2001b). FeNO levels correlate with eosinophilic airway inflammation and predict a decline in asthma control when repeated as longitudinal measurements (CitationKharitonov and Barnes 2001a; CitationLiu and Thomas 2005; CitationSmith et al 2005). The changes in serial FeNO have a higher predictive value than single measurements (CitationJatakanon et al 2000; CitationLeuppi et al 2001; CitationKharitonov and Barnes 2001a). In addition, the level of FeNO is related to several markers of asthma control, such as asthma symptoms, dyspnea score, daily use of rescue medication, and reversibility of airflow obstruction (CitationSippel et al 2000). Elevated FeNO levels can be detected before one can determine any significant deterioration in airway hyperresponsiveness, elevation of sputum eosinophil levels or changes in lung function parameters (CitationKharitonov et al 1996b; CitationJatakanon et al 2000). The main site of origin of the increased levels of FeNO in asthma is the lower airways (CitationKharitonov et al 1996a). The measurement is highly reproducible both in healthy and asthmatic adults and children (CitationKharitonov et al 2003). Measurements of exhaled NO at different flows show that the increase in peripheral NO is often related to disease severity (CitationBrindicci et al 2005). Overall FeNO is one of the most widely used biomarkers in the diagnosis of asthma especially when the diagnosis is uncertain; recent results clearly highlight its benefits also in asthma management.
Exhaled NO is, however, somewhat nonspecific, for example the levels are increased in viral infections (CitationKharitonov and Barnes 2001b). On the other hand, FeNO levels are generally decreased in smokers (CitationMaziak et al 1998; CitationRytila et al 2006). There is also some disagreement on whether changes in serial FeNO are significant evidence of loss of asthma control or simply due to errors in measurements or the natural variability of airway inflammation over time (CitationKharitonov 2004). This suggests that FeNO may not always be related to asthma severity or airway inflammation (CitationKharitonov and Barnes 2000). Development of less expensive FeNO analyzers would be beneficial, since for now FeNO analyzers are available mostly in central/university hospitals. Despite these problems, FeNO measurements have remained as one of the most important parameters in evaluating, treating, and monitoring patients with asthma and airway disease with eosinophilic inflammation.
In contrast to asthma, the FeNO levels in stable COPD do not differ significantly from controls (CitationKharitonov and Barnes 2001b; CitationRytila et al 2006). FeNO levels increase during COPD exacerbation (CitationMaziak et al 1998), most likely due to increased oxidative stress especially in cases with coexistent asthma and/or the presence of airway eosinophils (CitationPapi et al 2000). The elevated levels of FeNO in unstable COPD compared both with stable smokers or ex-smokers with COPD are attributable to the presence of eosinophils (CitationMaziak et al 1998). On the other hand, cigarette smoke decreases FeNO levels (CitationKharitonov et al 1995; CitationRobbins et al 1996) by down-regulating eNOS (CitationSu et al 1998) and consuming NO, making FeNO an unreliable marker for the diagnosis of asthma in smokers. FeNO has a minor role in evaluating COPD, but it may have importance in the differentiation of asthma, eosinophilic bronchitis, and COPD.
The reaction of NO and O2•− in the airways leads to the formation of peroxynitrite (ONOO) which reacts with tyrosine residues of proteins to form a stable product, nitrotyrosine. Nitrotyrosine can be detected in EBC, its levels are increased in asthma and decreased by corticosteroid treatment (CitationHanazawa et al 2000; CitationBaraldi et al 2006; CitationBodini et al 2006). However, even though both HPLC and GC/MS measurements are sensitive and detect similar nitrotyrosine levels in the EBC, they do not differentiate healthy controls from asthmatics, and therefore nitrotyrosine does not seem to be a selective marker for oxidative stress in asthma (CitationCelio et al 2006).
Nitric oxide can be trapped by thiol-containing biomolecules (such as GSH) to form S-nitrosothiols. The levels of these compounds are elevated in the EBC of smokers and in patients with asthma (CitationCorradi et al 2001) and the levels decline with corticosteroid treatment in asthma (CitationKharitonov et al 2002). Overall, the increase of the S-nitrosothiols in EBC is transitory, and probably not sensitive enough to help in the diagnostic assessment of airway diseases. Moreover, the levels of NO(x) in EBC appear to be too variable to be beneficial in clinical investigations (CitationFranklin et al 2006).
Volatile organic compounds
There are many volatile hydrocarbons, but only a few of them have been analyzed from exhaled air, with the most widely investigated being ethane. Elevated exhaled ethane levels have been detected in patients with mild steroid-naïve asthma compared with steroid-treated patients and normal subjects (CitationParedi et al 2000a). COPD patients display elevated exhaled ethane levels that correlate with the degree of airway obstruction (CitationParedi et al 2000b). Exhaled ethane, however, is increased by physical (CitationLeaf et al 1997) and mental stress and smoking (CitationHabib et al 1995), probably due to the high concentrations of hydrocarbons and direct oxidative damage. Cigarette smoke itself contains ethane, and a transient elevation of exhaled ethane has also been detected in healthy smokers (CitationHabib et al 1995). Another hydrocarbon of clinical interest is n-pentane and there are some correlations between breath pentane and serum biomarkers in smokers. Ethane is easier and faster to measure by GC/MS than the other hydrocarbons, but nonetheless these assays are difficult to conduct as the analyses require expertise, their measurement is expensive, and the biomarker itself is not specific for any particular airway disease. Moreover primary health care centers may not have access to a gas chromatograph or the necessary skills inherent in this technique. In brief, the measurement of ethane is demanding and difficult to transfer to clinical practice (CitationLarstad et al 2002; CitationBarnes et al 2006). Moreover, aldehydes can be detected both in EBC and induced sputum but their relative concentrations are different and do not correlate with each other (CitationCorradi et al 2004). There are a number of other VOCs in addition to ethane; whether their combination, ie, VOC “profiles” can be developed to be assayed by modern small gas chromatographic techniques would be an interesting area for future research. Recently, one technique, so called the electronic nose, in which expiratory vital capacity is collected and then smellprints are analyzed by linear discriminant analysis, has been found to be a promising method in differentiating exhaled breath of patients with asthma from controls even though it appears to be less accurate in distinguishing the severity of asthma (CitationDragonieri et al 2007).
Carbon monoxide
Carbon monoxide (CO) is derived from the degradation of heme by hemeoxygenase or nonheme-related release from xenobiotics and bacteria. Approximately 85% of CO is exhaled (CitationKharitonov and Barnes 2001b; CitationBarnes et al 2006). Many pathological conditions in addition to airway inflammation, can contribute to CO formation. One major limitation of exhaled CO in assessing oxidative stress in asthma or COPD is the marked effects of smoking on CO concentrations. The levels of exhaled CO are elevated in stable asthma and become reduced towards the normal values by administration of inhaled corticosteroids (CitationZayasu et al 1997; CitationHorvath et al 1998; CitationBarnes et al 2006). The effects of smoking make the assessment of exhaled CO in COPD difficult. Exhaled CO can be measured by electrochemical sensors, laser spectrophotometry, and by an infrared CO analysis as well as by gas chromatography, methods that are widely available in clinical laboratories. The analysis of CO is straightforward but the levels of CO are too variable to be significant in the clinical assessment of asthma and COPD, their diagnosis, or follow-up.
Hydrogen peroxide
Exhaled H2O2 has been detected in steroid-naïve asthmatics (CitationKharitonov and Barnes 2002), patients with stable COPD and during COPD exacerbation (CitationDekhuijzen et al 1996; CitationKharitonov 2004) being associated with the disease severity (CitationKostikas et al 2003). Macrophages from healthy smokers release more H2O2 than the cells from nonsmokers (CitationBaughman et al 1986; CitationNowak et al 1996; CitationGuatura et al 2000). Exhaled H2O2 concentrations are higher in smoking than nonsmoking asthmatic patients or controls, though there is extensive variability (CitationHorvath et al 2004). Acute smoking leads to a further elevation in exhaled H2O2 levels in asthmatic patients indicating that smoking causes an acute additional release of ROS in the airways (CitationHorvath et al 2004). Since H2O2 evaporates readily due to its highly unstable nature and its concentration decreases after a few days of storage at −70 °C, it needs to be assayed immediately (Citationvan Beurden et al 2002). One study claimed that EBC can be stored for up to 40 days without any loss of H2O2 concentration (Citationvan Beurden et al 2002). However, the variability of the H2O2 levels in airway fluids is high, generally the levels of H2O2 are low and the methods for H2O2 analysis are insensitive (CitationVan Hoydonck et al 2004). There are different techniques, all with their own limitations for H2O2 detection and therefore meaningful comparison of the results from various laboratories is difficult (CitationVan Hoydonck et al 2004). In summary, H2O2 is released from a number of cell types, it is relatively unstable, and its analysis is not sufficiently sensitive or specific to allow the diagnosis, differential diagnosis, or monitoring of asthma or COPD.
8-isoprostane
Oxidative damage to lipids leads to the production of isoprostanes, which are prostaglandin analogues produced primarily by free radical-induced peroxidation of arachidonic acid (CitationMorrow et al 1990). 8-isoprostaglandin F2α (8-isoprostane) is the best-characterized isomer, and is considered to be a reliable index reflecting the degree of oxidative stress in vivo. It is a stable metabolite and specific to lipid peroxidation (CitationJanssen 2001; CitationMorrow and Roberts 2002; CitationCracowski et al 2002). It has been proposed to represent an important tool for reliably exploring oxidative stress in lung diseases (CitationMontuschi et al 2004). Moreover, dietary fats do not have any significant effect on the 8-isoprostane concentration (CitationGopaul et al 2000). Although antioxidants scavenge ROS, it seems that they fail to reduce the rate of lipid peroxidation (CitationAnderson et al 1988; CitationHabib et al 1999) possibly due to the fact that lipid peroxidation is the result of a complicated metabolic pathway, where only the first step is initiated by free radicals (CitationMorrow et al 1990). Nevertheless several studies have indicated that 8-isoprostane may be an important mediator of oxidative stress and pulmonary oxygen toxicity (CitationJanssen 2001) and form part of a common pathway leading to airflow obstruction (CitationParedi et al 2002).
Most studies have used commercial EIA (enzyme immunoassay) kits to detect 8-isoprostane in EBC, this technique has a good correlation with GC/MS (CitationMontuschi et al 1999, Citation2000; CitationAntczak et al 2002; CitationKostikas et al 2003; CitationBiernacki et al 2003; CitationBaraldi et al 2003a; CitationVan Hoydonck et al 2004; CitationBattaglia et al 2005; CitationSimpson et al 2005), though there are also dissenting voices (CitationVan Hoydonck et al 2004; CitationRahman 2004; CitationBodini et al 2004; CitationSimpson et al 2005). Elevated EBC 8-isoprostane concentrations have been reported in children (CitationBaraldi et al 2003a, Citation2003b; CitationMondino et al 2004; CitationShahid et al 2005) and adults with asthma (CitationMontuschi et al 1999; CitationAntczak et al 2002; CitationBattaglia et al 2005) and COPD (CitationMontuschi et al 2000; CitationKostikas et al 2003; CitationBiernacki et al 2003; CitationKo et al 2006). The concentrations increase with asthma severity (CitationMontuschi et al 1999; CitationKharitonov and Barnes 2001b) and decline following resolution of acute asthma exacerbations, though they still remain higher than in healthy individuals (CitationBaraldi et al 2003a). EBC 8-isoprostane concentrations decline after allergen avoidance in children with allergic asthma (CitationBodini et al 2004), but are relatively resistant to inhaled corticosteroid therapy (CitationMontuschi et al 1999; CitationBaraldi et al 2003a, Citation2003b; CitationMondino et al 2004; CitationShahid et al 2005). The levels do not correlate with FeNO (CitationBaraldi et al 2003a) or lung function parameters in children with asthma (CitationBaraldi et al 2003b; CitationShahid et al 2005). The levels of 8-isoprostane are increased in EBC of COPD irrespective of smoking status and lung function impairment (CitationMontuschi et al 2000), increasing further during exacerbations of COPD, and declining after antibiotic treatment (CitationBiernacki et al 2003). Smoking seems to evoke an acute 50% increase in EBC 8-isoprostane levels within 15 minutes (CitationMontuschi et al 2000). The 8-isoprostane concentrations in EBC do not correlate with age, sex, or history of smoking in pack-years (CitationMontuschi et al 2000). No associations have been found between the levels of 8-isoprostane and dyspnea score, neutrophil count, or lung function parameters (CitationMontuschi et al 2000).
There are still major limitations in the detection of 8-isoprostane in the EBC, the concentrations are variable and often remain below the detection limit of the analysis (CitationVan Hoydonck et al 2004). These limitations may be partly related to the extensive dilution that occurs from water vapour during condensation and the low concentrations to be assayed that are near the detection limits of the EIA measurements (CitationEffros et al 2005). Other confounding factors include smoking, diurnal variation, age, alcohol consumption, caffeine and possibly also a diet rich in antioxidants. Several studies have also clearly revealed extensive variation in the levels of 8-isoprostane in nonsmokers and smokers suggesting that the commercial assay itself is variable. Based on the earlier and recent studies, it appears that EBC 8-isoprostane may not be very sensitive or specific biomarker of oxidative stress given the variability in its measurement. The actual significance of 8-isoprostane and its detection methods (eg, standardization) in the EBC still await clarification.
Markers of oxidative stress in induced sputum
Oxidant-generating enzymes
The most important oxidant-generating enzymes that have been assessed in induced sputum specimens include iNOS, EPO, and MPO (CitationKinnula 2005b). The main location of iNOS, which is the most efficient of the NO synthases in producing NO during inflammation, is the airway epithelium, but it has also been detected in inflammatory cells (CitationBarnes and Belvisi 1993). Although, the levels of iNOS have been found to be elevated in the induced sputum of asthmatics (CitationSugiura et al 2003), variable levels of iNOS have been reported in COPD patients (CitationIchinose et al 2000; CitationRytila et al 2006). EPO is elevated in asthma while MPO, which is expressed in neutrophils and monocytes (CitationKim et al 2001), is elevated in COPD with the levels being higher in COPD than in asthma (CitationMetso et al 2001). A rather similar elevation in the number of MPO-positive cells is seen in the induced sputum of chronic nonsymptomatic smokers and chronic symptomatic smokers with normal lung function, who are considered to be at risk of developing COPD (CitationRytila et al 2006). Sputum MPO concentrations have been reported to be extremely variable in several investigations with large standard deviations (CitationKim et al 2001). However, EPO and MPO may possess potential significance in differentiating asthma from COPD. MPO leads to the formation of HOCl and EPO to HOBr. These markers still seem to offer the greatest potential in the differentiation of asthma and COPD but both of them have been evaluated in only a few investigations. In one study, the best results when determining the most optimal fixation procedure to detect MPO and EPO in cytocentrifuged cell samples (induced sputum, BAL) were obtained using a commercial reagent Ortho PermeaFix (OPF; Ortho Clinical Diagnostics, Raritan, NJ) for flow cytometry (CitationMetso et al 2002a). EPO was found to be a useful marker for the identification of eosinophils in sputum and bronchoalveolar lavage since anti-EPO antibodies reacted only with eosinophils (CitationMetso et al 2002b).
3-nitrotyrosine
The reaction of NO and O2•− in the airways leads to the formation of peroxynitrite which reacts with tyrosine residues of proteins to form the stable product, nitrotyrosine (CitationIschiropoulos et al 1992). Nitrotyrosine can be formed not only by iNOS activation but also by MPO (CitationDavis et al 2001). Increased nitrotyrosine immunoreactivity has been reported in the lung biopsies of asthmatics (CitationSaleh et al 1998), in EBC from asthmatic adults (CitationHanazawa et al 2000) and children (CitationBaraldi et al 2006) as described above and it is associated with asthma exacerbation. Nitrotyrosine may play a major role in the pathogenesis of airway remodelling, (CitationKharitonov and Barnes 2001b) and it may contribute to airway obstruction and hyperresponsiveness and epithelial damage in asthma (CitationSaleh et al 1998). Abundant iNOS and nitrotyrosine positive sputum cells have also been seen in COPD patients compared to healthy smokers with a negative correlation to FEV1 (CitationIchinose et al 2000). However, the sputum samples of smokers without airway obstruction and also some samples of nonsmokers display increased levels of nitrotyrosine (CitationRytila et al 2006). It is likely that nitrotyrosine is not specific in differentiating between asthmatic and cigarette smoke-related airway disease.
8-isoprostane
Recent evidence suggests that sputum 8-isoprostane mirrors airway oxidative stress and is related to respiratory disease type pattern and activity (CitationWood et al 2005). The level of 8-isoprostane is higher in sputum than in EBC (CitationSimpson et al 2005). Sputum 8-isoprostane is higher in adults with stable asthma than in healthy subjects, increase further with disease severity and decrease significantly after treatment of acute asthma exacerbation, although there is a wide variability in the 8-isoprostane concentrations between and within the groups (CitationWood et al 2005). Moreover, a recent study could not detect any difference between sputum 8-isoprostane levels in mild asthmatics and healthy controls (CitationLouhelainen et al 2008). Sputum 8-isoprostane levels are elevated in COPD and cigarette smokers, but do not clearly differentiate healthy smokers from symptomatic smokers, ie, those who are at risk for developing COPD (CitationKinnula et al 2007). No longitudinal studies have been conducted with this marker, making it difficult to draw any final conclusions about its real significance. As described above, the major problems with this marker include the poor sensitivity, specificity and the fact that commercial EIA method and/or the impurities of the samples may contribute to its levels in sputum specimens.
4-hydroxy-2-nonenal
Aldehydes generated endogenously during lipid peroxidation may be involved in many pathophysiologic events associated with oxidative stress in cells and tissues (CitationGutteridge 1995). 4-HNE is a highly reactive and diffusible end-product of oxidative stress-induced lipid peroxidation that can attack targets far from the original site of free radical generation (CitationEsterbauer et al 1991). It is hypothesized that the degree of formation of 4-HNE in response to smoking may also contribute to the development of enhanced airspace inflammation in COPD (CitationRahman et al 2002). 4-HNE can be detected in lung biopsies of COPD patients (CitationRahman et al 2002), but recently it has also been detected in induced sputum samples of chronic smokers, irrespective of the lung function parameters or symptoms compared to nonsmokers (CitationRytila et al 2006). These results suggest that even though 4-HNE confirms that oxidative damage has occurred, it may not provide specific insight into the pathogenesis of the airway disease, and may not be a sensitive biomarker for assessing the disease severity.
Antioxidants and antioxidant enzymes
The oxidant/antioxidant equilibrium is disturbed in asthmatic and COPD patients not only due to the chronic inflammation, activation of inflammatory cells and/or oxidant producing enzymes but also due to changes in the antioxidant defense of the lung. It is believed that the major low molecular weight antioxidant of human airway secretions is GSH (CitationCantin et al 1987) but how well its levels are maintained in the ELF is still poorly understood. In addition to free GSH, a major proportion of GSH is bound to proteins and this fraction is difficult to measure. GSH has been investigated both in airway secretions and BAL but it has been shown to be neither sensitive nor specific for asthma or COPD.
The first line of defense enzymes against superoxide radicals involves superoxide dismutases (SOD) such as MnSOD and there are suggestions that MnSOD may become inactivated in the airways of asthma patients (CitationComhair et al 2005). Enzymes related to GSH synthesis/homeostasis such as glutathione peroxidases (GPx) play an important role in the antioxidant defense of human lung (CitationCantin et al 1987). Extracellular glutathione peroxidase (eGPx) has not been investigated in sputum specimens but it is increased in the BALF of asthma patients (CitationComhair et al 2001). Glutaredoxins (GRX) participate in GSH binding to proteins and thiol oxidation/reduction, reactions that regulate the active forms of many thiol containing enzymes. GRX-1 is mainly expressed by macrophages (CitationPeltoniemi et al 2004) and the levels are decreased in the sputum macrophages of COPD patients (CitationPeltoniemi et al 2006). Glutathione-S-transferase omega, which has many functional features in common with GRX, has been recently found to be expressed mainly in alveolar macrophages, and similar to GRX-1, its levels also decline in COPD (CitationHarju et al 2007). Catalase is expressed both in the inflammatory cells and alveolar epithelium, and it is inactivated at least in the murine model of asthma (CitationGhosh et al 2006). Heme oxygenase 1 (HO-1) is an enzyme induced by oxidant stress (stress-response protein) and cytokines. It is expressed mainly in alveolar macrophages of human lung and macrophages of induced sputum of steroid-naïve asthmatics show prominent but only transient HO-I immunoreactivity. This is not seen in asthmatics treated with corticosteroids (CitationHarju et al 2002b). The expression of HO-1 is increased also in the sputum macrophages of COPD patients compared to healthy nonsmokers, but there is no difference between COPD patients and healthy smokers (CitationMaestrelli et al 2001). Cigarette smoking increases especially the RNA expression of GSH-related enzymes in the bronchial brushings of healthy individuals (CitationHackett et al 2003), but the RNA levels of antioxidant enzymes in the bronchial epithelium have high variability in COPD depending on its severity (CitationPierrou et al 2007). Even though the above mentioned findings have not been confirmed in sputum, the results are interesting; they suggest that combined profiles of antioxidant and detoxification enzymes and their posttranslational modifications (such as oxidation, thiolation, S-nitrosylation) may be promising indicators of the severity of oxidative stress in human airways.
Matrix metalloproteinases
Matrix metalloproteinases (MMPs) are a large family of proteolytic enzymes (over 30 MMPs have been characterized) that degrade the components of the extracellular matrix (CitationOhbayashi 2002). These enzymes are involved in the pulmonary remodelling processes that underpin both asthma and COPD (CitationParks and Shapiro 2001; CitationKelly and Jarjour 2003). Oxidative stress, mainly cigarette smoke associated oxidants, may be one of the major factors contributing to MMP activation. MMPs can be readily detected in sputum specimens. There are significant differences in the MMP profiles in COPD and asthma. In COPD, elevated levels of MMP–1, –8, and –9 compared with asthmatics, nonsmokers, and non-symptomatic cigarette smokers have been reported, and these changes may also reflect the different pathogenesis of these diseases (CitationCulpitt et al 2005). In the future, MMPs may be considered as additional biomarkers in COPD and/or asthma development. These markers also hold potential in evaluating COPD phenotypes, since the emphysematous type of COPD would be predicted to exhibit a different profile of MMPs than the disease where there is airway predominance.
Oxidant markers in bronchoalveolar lavage
The total BAL cell profile and also the cell count differ in asthma and COPD. The number of inflammatory cells, especially neutrophils, are higher in COPD patients suffering exacerbations compared with stable COPD patients or healthy controls (CitationDrost et al 2005). BAL fluid has been widely used for the assessment of inflammatory cytokines such as interleukin-8 (IL-8) and tumor necrosis factor alpha (TNFα) in asthma and COPD (CitationAaron et al 2001; CitationDrost et al 2005). The most widely investigated marker of oxidant/antioxidant balance in BAL fluid is GSH, the levels of which are increased in smokers and patients with stable COPD compared to the nonsmokers, but reduced during exacerbations as compared to the levels found in stable COPD (CitationDrost et al 2005). On the other hand, older smokers with a long-term smoking history exhibit elevated oxidized glutathione (GSSG) and protein carbonyls in their BAL fluid even in the absence of any lung disease, indicating that lung antioxidant defences have become overwhelmed the prolonged exposure to the noxious substances present in cigarette smoke (CitationNagai et al 2006). 8-isoprostane and some other oxidant markers have been compared between EBC and BAL, but clinical disease markers of inflammation and oxidative stress in EBC and BAL do not correlate with each other (CitationJackson et al 2007). Thus, even though some markers in BAL fluid may seem to offer promise in the assessment of inflammation, BAL is too invasive and not sensitive enough to be of use in the assessment of oxidative stress/airway inflammation in clinical practice.
Pitfalls in measuring ROS in smoking asthmatics
One problem in assessing the importance of oxidant-related biomarkers, for example FeNO and 8-isoprostane, is that smoking per se has significant effects on the levels of these markers, and this phenomenon is especially important in asthma. The prevalence of active cigarette smoking among asthmatics is as common as it is in the general population, for example in Finland as many as 30% of asthmatics are smokers (CitationHaahtela et al 2006). There is limited data on the airway pathology of smoking asthmatics, since these patients are frequently excluded from experimental studies. Asthma and cigarette smoking potentiate the effects of each other, leading to impaired asthma control, more severe symptoms (CitationAlthuis et al 1999), increased need for rescue medication (CitationGallefoss and Bakke 2003), accelerated deterioration of lung function (CitationLange et al 1998) and reduced short-term therapeutic response to corticosteroids (CitationChaudhuri et al 2003). Smoking may also modify the typical asthmatic inflammation profile, which complicates the differential diagnosis from COPD. It also appears that there are features of both accelerated and suppressed inflammatory responses in smokers with asthma. The number of eosinophils in sputum are decreased (CitationChalmers et al 2001), perhaps due to the exogenous NO in cigarette smoke increasing apoptosis of activated eosinophils (CitationAssreuy et al 1993) whereas the number of neutrophils is elevated (CitationChalmers et al 2001). Many asthmatic smokers have mixed features of typical asthmatic and smoke-related airway inflammation and pathology. Results from clinical studies suggest that smokers with asthma may be resistant to therapeutic effects of the corticosteroids (CitationChalmers et al 2001; CitationChaudhuri et al 2003). There is also evidence that the time of initiation of smoking may influence the asthma phenotype: atopy-associated asthma has been shown to develop before smoking initiation (CitationRaherison et al 2003). It has been claimed that the remodeling of airways might be more severe in asthmatic smokers (CitationCarroll et al 2000). Several markers of oxidative/nitrosative stress are increased even in “healthy” smokers, but we are not aware of any studies where the oxidant markers have been compared between healthy smokers and smoking asthmatics. It is apparent that the sensitivity of FeNO to detect a worsening of asthmatic inflammation in smokers is poor, since smoking on its own decreases FeNO levels significantly.
Disease progression, COPD phenotypes, and oxidative stress
The evaluation of oxidative stress in disease progression is especially complex in COPD. The symptoms do not closely reflect spirometric changes and the symptoms may predict exacerbation only in some individuals (CitationSeemungal et al 2000). COPD exacerbations in turn are important events in terms of disease progression, morbidity, and mortality. Many patients with COPD never recover completely from the exacerbation. The lung pathology is especially complex in COPD as the disease contains many phenotypes displaying a wide variety of airway and emphysematous changes. However, all phenotypes are treated similarly, because there are no specific biomarkers for the differentiation of the disease subtypes or their progression. At present, no biomarker in clinical practice is able to differentiate small airway inflammation and fibrosis from alveolar destruction even though these changes are the main pathophysiologic events in COPD (CitationBarnes et al 2006). Special efforts should be directed towards finding reliable biomarkers that would differentiate the phenotypes of COPD in addition to identifying markers that can be used in the assessment of disease progression. Though outside the scope of this review, which concentrates on local airway biomarkers, a number of biomarkers in the circulating blood/plasma and in the skeletal muscle are under intensive investigation as ways of monitoring the progression of COPD (CitationAldonyte et al 2004; CitationGosker et al 2005; CitationHurst et al 2006; CitationJones and Agusti 2006).
Several studies have highlighted the usefulness of 8-isoprostane in the evaluation of oxidative stress in COPD and during COPD exacerbations. This agent is known to exert biological activity such as evoking the contraction of human bronchial smooth muscle in vitro (CitationParedi et al 2002), and being able to elicit airway hyperresponsiveness (CitationHeld and Uhlig 2000) and evoke airway obstruction and plasma exudation (CitationOkazawa et al 1997), evidence that it may be involved in the pathophysiology and progression of COPD. Many cross-sectional studies have shown that 8-isoprostane levels correlate with lung function parameters, but these findings have not been confirmed in longitudinal investigations. As far as we are aware there are no studies to explain how elevated 8-isoprostane levels are associated with COPD phenotypes, respond to treatment in COPD, or whether 8-isoprostane can be used in the follow-up of these patients.
Several markers of oxidant burden have been suggested to associate both with the pathogenesis and disease progression of asthma (CitationBarnes 1990) and COPD (CitationRepine et al 1997). Considering the complexity of oxidative stress and the inflammatory cascade and the interaction between these two processes, it is, however, unlikely that measurement of any single molecule in the EBC, sputum, or in biological fluids would be able to provide adequate information about disease progression. Potential current markers that could possibly be used for the assessment of the disease severity or progression include the combination of several markers such as EBC VOC profiles with small detectors, FeNO, sputum oxidant markers, specific MMPs, and selected antioxidant enzymes.
Antioxidant therapies and disease progression
Since it seems likely that asthma and COPD are associated with an elevated oxidant burden, these diseases might be treated with exogenous antioxidants or related strategies. It is likely that vitamins taken orally do not reach the critically damaged areas of the lung, which has its own highly specific antioxidant systems. Several attempts have been made to improve GSH homeostasis by treatment with inhaled and oral GSH, since the level of GSH is much higher in the epithelial lining fluid than in any other organ or circulating blood, and decreased by oxidative stress. However, GSH is poorly absorbed through membranes and inhaled GSH itself has been shown to cause bronchoconstriction (CitationRahman and MacNee 1999). N-acetyl-L-cysteine (NAC) may improve GSH balance but this compound is known to also possess GSH-independent pro-oxidant effects at the cellular level. NAC has been tested and administered by inhalation, orally and intravenously (CitationRahman and MacNee 1999). Oral NAC has been shown to decrease the risk for COPD re-hospitalisations (CitationGerrits et al 2003) and to decrease H2O2 levels in the exhaled air in COPD (CitationKasielski and Nowak 2001), but the results of the multicenter BRONCUS-trial revealed no major effects on lung function values or COPD exacerbations (CitationDekhuijzen 2004; CitationDecramer et al 2005). A recent systematic review on NAC indicated that the use of NAC could significantly reduce the odds of exacerbation in patients with COPD (CitationSutherland et al 2006) and therefore could possibly have effects on disease progression. Whether the new antioxidant mimetics that are under development will have benefits in asthma or COPD will be an interesting area of future investigation.
Perspective/conclusions
The assessment of noninvasive biomarkers in asthma and COPD is an area of intensive investigation. Noninvasive specimens that reflect oxidative stress in the airways include exhaled air, EBC, and induced sputum. Induced sputum is a widely used technique and there are many advantages in using induced sputum both in asthma and COPD. One practical problem with induced sputum, however, is the fact that it is not totally noninvasive and sample processing requires expertise. Nonetheless, induced sputum is promising especially for the analysis of markers with different roles in the pathogenesis of asthma and COPD. One example is the differentiation of the subphenotypes (either airway or emphysema predominance) of COPD by combining the existent knowledge of oxidant markers in the sputum specimens and expanding the methodology to new technologies including proteomics (sputome).
Exhaled air and EBC are totally noninvasive and therefore most interesting for the clinical evaluation of airway diseases, their differential diagnosis and progression. FeNO has been the most widely used of the various markers and has been shown to have clinical significance in asthma, its differential diagnosis and monitoring (). Further emphasis should be directed in the development of small, easy-to-handle, portable devices for the investigation of the exhaled gas profiles (such as VOCs) and their role especially in COPD. Real time analysis of volatile organic molecules by infrared laser spectroscopy enables online measurement of oxidative markers (CitationMurtz et al 1999) and these techniques offer the potential for real time monitoring of EBC also in asthma and COPD. Metabolomic analysis (quantitative measurement of the dynamic multiparametric metabolic response of living systems to pathophysiological stimuli or genetic modification) (CitationNicholson et al 1999) can provide new biochemical profiles for the assessment of low molecular weight metabolites in EBC. These methods include nuclear magnetic resonance (NMR) and allow simultaneous detection of hundreds of low molecular weight species within a single fluid sample. These NMR “fingerprints” may further improve the characterization of the specific features in asthma and COPD and their differentiation (CitationCarraro et al 2007). Lipidomics has been evaluated in vitro and in the developing lung (CitationPostle et al 2006; CitationBernhard et al 2007), but its value in asthma and COPD remains to be confirmed in the future.
Table 1 The principal noninvasive methods in assessing airway inflammation and oxidative stress from patients with known or suspected obstructive pulmonary disease. The list includes some markers that already are in clinical use as well as several markers in experimental use
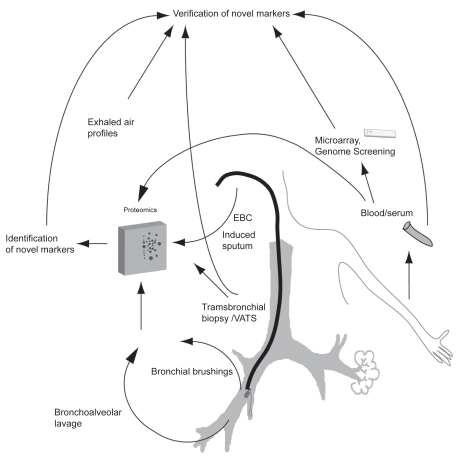
Many investigations have used sophisticated techniques such as microarray or proteomics which generate enormous amounts of information that is difficult to interpret even by the investigators. It is clearly challenging to extrapolate these results from a specific cell type (for example bronchial epithelial cells obtained by bronchial brushing) or from total lung homogenate to a noninvasive specimen such as exhaled air or sputum. It is likely that proteomics offers multiple advantages compared to the gene expression studies since proteins and not genes ultimately determine cellular function (CitationRaj et al 2007). Proteomic studies have also revealed a total of nearly 200 human proteins from the induced sputum specimens (sputome) (CitationNicholas et al 2006; CitationCasado et al 2007) and these profiles may differ in various airway diseases and phenotypes (CitationCasado et al 2007). Recent studies have also discovered panels/clusters of oxidant/antioxidant enzymes that may be utilized for the assessment of disease severity. Overproduction of ROS can also cause oxidative modifications of several important antioxidant/defense enzymes, which may be associated with alterations in enzyme conformation and thus they can function as markers of the degree of oxidative stress present in the airways. These changes that currently can be analyzed by 2DE electrophoresis and MS but in the future new potent nongel-based proteomic methods may represent the next generation of more specific biomarkers both for asthma and COPD. In view of the overlapping patterns of the profiles of various oxidant biomarkers in asthma and COPD, the utilization of very sophisticated techniques in their assessment is important. Since cigarette smoking is inevitably related to COPD and since smoking only partly overlaps with the pathophysiology of asthma, new tools might offer an easier and cost-effective way for early diagnosis and differentiation of asthma and COPD. The future directions in the search for potential markers of oxidant burden are summarized in and .
Table 2 Potential noninvasive oxidant biomarkers for the assessment of asthma, COPD, their differential diagnosis and phenotypes by combining the existent knowledge and future technologies
Figure 2 Future strategies for the discovery of new biomarkers in asthma and COPD, their diagnosis, differential diagnosis and assessment of the COPD phenotypes. The methods include microarray and proteomics combined with novel technologies. In these studies, protein expression has multiple advantages compared to gene expression, since proteins and not genes finally determine cellular function. Methods such as metabolomics (analysis of low molecular weight molecules from exhaled breath condensate), lipodomics and sputome (proteomics from induced sputum) have been evaluated and are ready for clinical prospective studies in asthma and COPD. Microarray/proteomics obtained from lung tissue, bronchial brushings and/or bronchoalveolar lavage have been conducted in asthma and/or COPD, and their extrapolation to noninvasive samples is being investigated in many laboratories.
Acknowledgments
This review and our studies closely related to this issue have been supported by the EVO funding of Helsinki University Hospital, Finnish Antituberculosis Association Foundation, the Ahokas Foundation, the Finnish medical foundation, and the Yrjo Jahnsson Foundation. The authors report no conflicts of interest in this work.
References
- AaronSDAngelJBLunauM2001Granulocyte inflammatory markers and airway infection during acute exacerbation of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med1633495511179105
- AldonyteRErikssonSPiitulainenE2004Analysis of systemic biomarkers in COPD patientsCOPD11556417136983
- AldridgeREChanTvan DalenCJ2002Eosinophil peroxidase produces hypobromous acid in the airways of stable asthmaticsFree Radic Biol Med338475612208372
- AlexisNEHuSCZemanK2001Induced sputum derives from the central airways: confirmation using a radiolabeled aerosol bolus delivery techniqueAm J Respir Crit Care Med16419647011734453
- AlthuisMDSextonMPrybylskiD1999Cigarette smoking and asthma symptom severity among adult asthmaticsJ Asthma362576410350222
- AlvingKWeitzbergELundbergJM1993Increased amount of nitric oxide in exhaled air of asthmaticsEur Respir J61368707507065
- AndersonRTheronAJRasGJ1988Ascorbic acid neutralizes reactive oxidants released by hyperactive phagocytes from cigarette smokersLung166149593132577
- Anonymous1999Recommendations for standardized procedures for the online and offline measurement of exhaled lower respiratory nitric oxide and nasal in adults and childrenAm J Respir Crit Care Med16021041710588636
- AntczakAKharitonovSAMontuschiP2005Inflammatory response to sputum induction measured by exhaled markersRespiration72594915988171
- AntczakAMontuschiPKharitonovS2002Increased exhaled cysteinyl-leukotrienes and 8-isoprostane in aspirin-induced asthmaAm J Respir Crit Care Med166301612153961
- AssreuyJCunhaFQLiewFY1993Feedback inhibition of nitric oxide synthase activity by nitric oxideBr J Pharmacol10883377682140
- BaraldiECarraroSAlinoviR2003aCysteinyl leukotrienes and 8-isoprostane in exhaled breath condensate of children with asthma exacerbationsThorax58505912775861
- BaraldiEGhiroLPiovanV2003bIncreased exhaled 8-isoprostane in childhood asthmaChest124253112853498
- BaraldiEGhiroLPiovanV2003cSafety and success of exhaled breath condensate collection in asthmaArch Dis Child883586012651772
- BaraldiEGiordanoGPasqualeMF20063-Nitrotyrosine, a marker of nitrosative stress, is increased in breath condensate of allergic asthmatic childrenAllergy6190616364162
- BarnesPJ1990Reactive oxygen species and airway inflammationFree Radic Biol Med9235432272532
- BarnesPJBelvisiMG1993Nitric oxide and lung diseaseThorax481034437903007
- BarnesPJChowdhuryBKharitonovSA2006Pulmonary biomarkers in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med17461416556692
- BattagliaSdenHHTimmersMC2005Small airways function and molecular markers in exhaled air in mild asthmaThorax606394416061704
- BaughmanRPCorserBCStrohoferS1986Spontaneous hydrogen peroxide release from alveolar macrophages of some cigarette smokersJ Lab Clin Med10723373005452
- BernhardWSchmiedlAKosterG2007Developmental changes in rat surfactant lipidomics in the context of species variabilityPediatr Pulmonol4279480417659602
- BiernackiWAKharitonovSABarnesPJ2003Increased leukotriene B4 and 8-isoprostane in exhaled breath condensate of patients with exacerbations of COPDThorax58294812668789
- BodiniAPeroniDVicentiniL2004Exhaled breath condensate eicosanoids and sputum eosinophils in asthmatic children: a pilot studyPediatr Allergy Immunol15263114998379
- BodiniAPeroniDGZardiniF2006Flunisolide decreases exhaled nitric oxide and nitrotyrosine levels in asthmatic childrenMediators Inflamm20063191917047290
- BoskenCHHardsJGatterK1992Characterization of the inflammatory reaction in the peripheral airways of cigarette smokers using immunocytochemistryAm Rev Respir Dis14591171554220
- BouletLPTurcotteHHudonC1998Clinical, physiological and radiological features of asthma with incomplete reversibility of airflow obstruction compared with those of COPDCan Respir J527079753528
- BousquetJJefferyPKBusseWW2000Asthma. From bronchoconstriction to airways inflammation and remodelingAm J Respir Crit Care Med16117204510806180
- BrindicciCItoKRestaO2005Exhaled nitric oxide from lung periphery is increased in COPDEur Respir J2652915994389
- ByrnesCADinarevicSShinebourneEA1997Exhaled nitric oxide measurements in normal and asthmatic childrenPediatr Pulmonol24312189407563
- CantinAMNorthSLHubbardRC1987Normal alveolar epithelial lining fluid contains high levels of glutathioneJ Appl Physiol6315273040659
- CarraroSRezziSRenieroF2007Metabolomics applied to exhaled breath condensate in childhood asthmaAm J Respir Crit Care Med1759869017303796
- CarrollNGPerrySKarkhanisA2000The airway longitudinal elastic fiber network and mucosal folding in patients with asthmaAm J Respir Crit Care Med161244810619827
- CasadoBIadarolaPPannellLK2007Protein expression in sputum of smokers and chronic obstructive pulmonary disease patients: a pilot study by CapLC-ESI-Q-TOFJ Proteome Res646152317973440
- CelioSTroxlerHDurkaSS2006Free 3-nitrotyrosine in exhaled breath condensates of children fails as a marker for oxidative stress in stable cystic fibrosis and asthmaNitric Oxide152263216931075
- ChalmersGWMacLeodKJThomsonL2001Smoking and airway inflammation in patients with mild asthmaChest12019172211742922
- ChanezPVignolaAMVicP1999Comparison between nasal and bronchial inflammation in asthmatic and control subjectsAm J Respir Crit Care Med159588959927377
- ChaudhuriRLivingstonEMcMahonAD2003Cigarette smoking impairs the therapeutic response to oral corticosteroids in chronic asthmaAm J Respir Crit Care Med16813081112893649
- ChurchDFPryorWA1985Free-radical chemistry of cigarette smoke and its toxicological implicationsEnviron Health Perspect64111263007083
- ComhairSABhathenaPRFarverC2001Extracellular glutathione peroxidase induction in asthmatic lungs: evidence for redox regulation of expression in human airway epithelial cellsFASEB J1570811149894
- ComhairSAXuWGhoshS2005Superoxide dismutase inactivation in pathophysiology of asthmatic airway remodeling and reactivityAm J Pathol1666637415743779
- CorradiMMontuschiPDonnellyLE2001Increased nitrosothiols in exhaled breath condensate in inflammatory airway diseasesAm J Respir Crit Care Med163854811282756
- CorradiMPignattiPManiniP2004Comparison between exhaled and sputum oxidative stress biomarkers in chronic airway inflammationEur Respir J241011715572547
- CracowskiJLDurandTBessardG2002Isoprostanes as a biomarker of lipid peroxidation in humans: physiology, pharmacology and clinical implicationsTrends Pharmacol Sci23360612377577
- CulpittSVRogersDF2000Evaluation of current pharmacotherapy of chronic obstructive pulmonary diseaseExpert Opin Pharmacother110072011249492
- CulpittSVRogersDFTravesSL2005Sputum matrix metalloproteases: comparison between chronic obstructive pulmonary disease and asthmaRespir Med997031015878486
- DavisKLMartinETurkoIV2001Novel effects of nitric oxideAnnu Rev Pharmacol Toxicol412033611264456
- DecramerMRuttenvanMMDekhuijzenPN2005Effects of N-acetylcysteine on outcomes in chronic obstructive pulmonary disease (Bronchitis Randomized on NAC Cost-Utility Study, BRONCUS): a randomised placebo-controlled trialLancet36515526015866309
- DekhuijzenPN2004Antioxidant properties of N-acetylcysteine: their relevance in relation to chronic obstructive pulmonary diseaseEur Respir J236293615083766
- DekhuijzenPNAbenKKDekkerI1996Increased exhalation of hydrogen peroxide in patients with stable and unstable chronic obstructive pulmonary diseaseAm J Respir Crit Care Med15481368810624
- DjukanovicRSterkPJFahyJV2002Standardised methodology of sputum induction and processingEur Respir J Suppl371s55s12361359
- DragonieriSSchotRMertensBJ2007An electronic nose in the discrimination of patients with asthma and controlsJ Allergy Clin Immunol1208566217658592
- DrostEMSkwarskiKMSauledaJ2005Oxidative stress and airway inflammation in severe exacerbations of COPDThorax6029330015790984
- DworskiR2000Oxidant stress in asthmaThorax55Suppl 2S51S5310992559
- EffrosRMSuJCasaburiR2005Utility of exhaled breath condensates in chronic obstructive pulmonary disease: a critical reviewCurr Opin Pulm Med11135915699785
- EsterbauerHSchaurRJZollnerH1991Chemistry and biochemistry of 4-hydroxynonenal, malonaldehyde and related aldehydesFree Radic Biol Med11811281937131
- FabbriLMRomagnoliMCorbettaL2003Differences in airway inflammation in patients with fixed airflow obstruction due to asthma or chronic obstructive pulmonary diseaseAm J Respir Crit Care Med1674182412426229
- FahyJVBousheyHALazarusSC2001Safety and reproducibility of sputum induction in asthmatic subjects in a multicenter studyAm J Respir Crit Care Med1631470511371420
- FahyJVKimKWLiuJ1995aProminent neutrophilic inflammation in sputum from subjects with asthma exacerbationJ Allergy Clin Immunol95843527722165
- FahyJVWongHLiuJ1995bComparison of samples collected by sputum induction and bronchoscopy from asthmatic and healthy subjectsAm J Respir Crit Care Med1525387599862
- FletcherCPetoR1977The natural history of chronic airflow obstructionBr Med J116458871704
- FranklinPMoellerAHallGL2006Variability of nitric oxide metabolites in exhaled breath condensateRespir Med100123915885998
- GallefossFBakkePS2003Does smoking affect the outcome of patient education and self-management in asthmatics?Patient Educ Couns4991712527158
- GerritsCMHeringsRMLeufkensHG2003N-acetylcysteine reduces the risk of re-hospitalisation among patients with chronic obstructive pulmonary diseaseEur Respir J21795812765423
- [GINA] Global Initiative for Asthma2002Global strategies for asthma management and prevention. National Institutes of Health, National Heart, Lung and Blood Institute. [online]. NIH Publication, No 02-3659Accessed on December 12, 2007 URL: http://www.ginasthma.com
- GhoshSJanochaAJAronicaMA2006Nitrotyrosine proteome survey in asthma identifies oxidative mechanism of catalase inactivationJ Immunol17655879716622028
- GibsonPGNorzilaMZFakesK1999Pattern of airway inflammation and its determinants in children with acute severe asthmaPediatr Pulmonol282617010497375
- [GOLD] Global Initiative for Chronic Obstructive Lung Disease2002Global initiative for chronic obstructive lung disease. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease NHLBI/WHO Workshop Report [online]. NIH Publication, No 2701Accessed on December 12, 2007 URL: http://www.goldcopd.com
- GompertzSBayleyDLHillSL2001Relationship between airway inflammation and the frequency of exacerbations in patients with smoking related COPDThorax56364111120902
- GopaulNKHalliwellBAnggardEE2000Measurement of plasma F2-isoprostanes as an index of lipid peroxidation does not appear to be confounded by dietFree Radic Res331152710885619
- GoskerHRBastAHaenenGR2005Altered antioxidant status in peripheral skeletal muscle of patients with COPDRespir Med991182515672860
- GuaturaSBMartinezJASantos BuenoPC2000Increased exhalation of hydrogen peroxide in healthy subjects following cigarette consumptionSao Paulo Med J11893810887384
- GutteridgeJM1995Lipid peroxidation and antioxidants as biomarkers of tissue damageClin Chem411819287497639
- HaahtelaTTuomistoLEPietinalhoA2006A 10 year asthma programme in Finland: major change for the betterThorax616637016877690
- HabibMPClementsNCGarewalHS1995Cigarette smoking and ethane exhalation in humansAm J Respir Crit Care Med1511368727735586
- HabibMPTankLJLaneLC1999Effect of vitamin E on exhaled ethane in cigarette smokersChest1156849010084476
- HackettNRHeguyAHarveyBG2003Variability of antioxidant-related gene expression in the airway epithelium of cigarette smokersAm J Respir Cell Mol Biol293314312702543
- HamidQSongYKotsimbosTC1997Inflammation of small airways in asthmaJ Allergy Clin Immunol10044519257786
- HanazawaTKharitonovSABarnesPJ2000Increased nitrotyrosine in exhaled breath condensate of patients with asthmaAm J Respir Crit Care Med1621273611029330
- HarjuTKaarteenaho-WiikRSoiniY2002aDiminished immunoreactivity of gamma-glutamylcysteine synthetase in the airways of smokers’ lungAm J Respir Crit Care Med166754912204877
- HarjuTSoiniYPaakkoR2002bUp-regulation of heme oxygenase-I in alveolar macrophages of newly diagnosed asthmaticsRespir Med964182312117041
- HarjuTHPeltoniemiMJRytilaPH2007Glutathione S-transferase omega in the lung and sputum supernatants of COPD patientsRespir Res84817617905
- HaslamPLBaughmanRP1999Report of ERS Task Force: guidelines for measurement of acellular components and standardization of BALEur Respir J14245810515395
- HattotuwaKGambleEAO’ShaughnessyT2002Safety of bronchoscopy, biopsy, and BAL in research patients with COPDChest12219091212475825
- HeldHDUhligS2000Mechanisms of endotoxin-induced airway and pulmonary vascular hyperreactivity in miceAm J Respir Crit Care Med16215475211029375
- HoLPWoodFTRobsonA2000Atopy influences exhaled nitric oxide levels in adult asthmaticsChest11813273111083682
- HoidalJRNiewoehnerDE1982Lung phagocyte recruitment and metabolic alterations induced by cigarette smoke in humans and in hamstersAm Rev Respir Dis126548526289710
- HolzORichterKJorresRA1998Changes in sputum composition between two inductions performed on consecutive daysThorax538369624289
- HorvathIDonnellyLEKissA2004Exhaled nitric oxide and hydrogen peroxide concentrations in asthmatic smokersRespiration71463815467323
- HorvathIDonnellyLEKissA1998Raised levels of exhaled carbon monoxide are associated with an increased expression of heme oxygenase-1 in airway macrophages in asthma: a new marker of oxidative stressThorax53668729828853
- HorvathIHuntJBarnesPJ2005Exhaled breath condensate: methodological recommendations and unresolved questionsEur Respir J265234816135737
- HurstJRDonaldsonGCPereraWR2006Use of plasma biomarkers at exacerbation of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med1748677416799074
- IchinoseMSugiuraHYamagataS2000Increase in reactive nitrogen species production in chronic obstructive pulmonary disease airwaysAm J Respir Crit Care Med162701610934109
- IschiropoulosHZhuLChenJ1992Peroxynitrite-mediated tyrosine nitration catalyzed by superoxide dismutaseArch Biochem Biophys29843171416974
- JacksonASSandriniACampbellC2007Comparison of biomarkers in exhaled breath condensate and bronchoalveolar lavageAm J Respir Crit Care Med175222717110649
- JanssenLJ2001Isoprostanes: an overview and putative roles in pulmonary pathophysiologyAm J Physiol Lung Cell Mol Physiol280L1067L108211350785
- JatakanonALimSBarnesPJ2000Changes in sputum eosinophils predict loss of asthma controlAm J Respir Crit Care Med161647210619799
- JefferyPK1999Differences and similarities between chronic obstructive pulmonary disease and asthmaClin Exp Allergy29Suppl 2142610421818
- JonesPWAgustiAG2006Outcomes and markers in the assessment of chronic obstructive pulmonary diseaseEur Respir J278223216585091
- JonesRDHancockJTMoriceAH2000NADPH oxidase: a universal oxygen sensor?Free Radic Biol Med294162411020663
- KasielskiMNowakD2001Long-term administration of N-acetylcysteine decreases hydrogen peroxide exhalation in subjects with chronic obstructive pulmonary diseaseRespir Med954485611421501
- KawikovaIBarnesPJTakahashiT19968-Epi-PGF2 alpha, a novel noncyclooxygenase-derived prostaglandin, constricts airways in vitroAm J Respir Crit Care Med15359068564103
- KeatingsVMBarnesPJ1997Granulocyte activation markers in induced sputum: comparison between chronic obstructive pulmonary disease, asthma, and normal subjectsAm J Respir Crit Care Med155449539032177
- KellyCAKotreCJWardC1987Anatomical distribution of bronchoalveolar lavage fluid as assessed by digital subtraction radiographyThorax4262483310313
- KellyEAJarjourNN2003Role of matrix metalloproteinases in asthmaCurr Opin Pulm Med9283312476081
- KellyFJMudwayIBlombergA1999Altered lung antioxidant status in patients with mild asthmaLancet354482310465176
- KharitonovSAAlvingKBarnesPJ1997Exhaled and nasal nitric oxide measurements: recommendationsEur Respir J101683939230267
- KharitonovSA2004Exhaled markers of inflammatory lung diseases: ready for routine monitoring?Swiss Med Wkly1341759215106031
- KharitonovSABarnesPJ2000Clinical aspects of exhaled nitric oxideEur Respir J167819211106225
- KharitonovSABarnesPJ2002Biomarkers of some pulmonary diseases in exhaled breathBiomarkers713212101782
- KharitonovSABarnesPJ2001bExhaled markers of pulmonary diseaseAm J Respir Crit Care Med163169372211401895
- KharitonovSABarnesPJ2001aDoes exhaled nitric oxide reflect asthma control? Yes, it does!Am J Respir Crit Care Med164727811549522
- KharitonovSAChungKFEvansD1996aIncreased exhaled nitric oxide in asthma is mainly derived from the lower respiratory tractAm J Respir Crit Care Med1531773808665033
- KharitonovSADonnellyLEMontuschiP2002Dose-dependent onset and cessation of action of inhaled budesonide on exhaled nitric oxide and symptoms in mild asthmaThorax578899612324677
- KharitonovSAGonioFKellyC2003Reproducibility of exhaled nitric oxide measurements in healthy and asthmatic adults and childrenEur Respir J21433812661997
- KharitonovSARobbinsRAYatesD1995Acute and chronic effects of cigarette smoking on exhaled nitric oxideAm J Respir Crit Care Med152609127543345
- KharitonovSAYatesDRobbinsRA1994Increased nitric oxide in exhaled air of asthmatic patientsLancet34313357904001
- KharitonovSAYatesDHChungKF1996bChanges in the dose of inhaled steroid affect exhaled nitric oxide levels in asthmatic patientsEur Respir J91962018777950
- KimCKChungCYChoiSJ2000Bronchoalveolar lavage cellular composition in acute asthma and acute bronchiolitisJ Pediatr1375172211035831
- KimJSHackleyGHOkamotoK2001Sputum processing for evaluation of inflammatory mediatorsPediatr Pulmonol32152811477732
- KinnulaVL2005aFocus on antioxidant enzymes and antioxidant strategies in smoking related airway diseasesThorax6069370016061713
- KinnulaVL2005bProduction and degradation of oxygen metabolites during inflammatory states in the human lungCurr Drug Targets Inflamm Allergy44657016101523
- KinnulaVLCrapoJD2003Superoxide dismutases in the lung and human lung diseasesAm J Respir Crit Care Med16716001912796054
- KinnulaVLCrapoJDRaivioKO1995Generation and disposal of reactive oxygen metabolites in the lungLab Invest733197603038
- KinnulaVLIlumetsHMyllarniemiM20078-Isoprostane as a marker of oxidative stress in nonsymptomatic cigarette smokers and COPDEur Respir J2951517050565
- KirbyJGHargreaveFEGleichGJ1987Bronchoalveolar cell profiles of asthmatic and nonasthmatic subjectsAm Rev Respir Dis136379833304046
- KneepkensCMLepageGRoyCC1994The potential of the hydrocarbon breath test as a measure of lipid peroxidationFree Radic Biol Med17127607959173
- KoFWLauCYLeungTF2006Exhaled breath condensate levels of 8-isoprostane, growth related oncogene alpha and monocyte chemoattractant protein-1 in patients with chronic obstructive pulmonary diseaseRespir Med100630816213701
- KostikasKPapatheodorouGPsathakisK2003Oxidative stress in expired breath condensate of patients with COPDChest12413738014555568
- LangePParnerJVestboJ1998A 15-year follow-up study of ventilatory function in adults with asthmaN Engl J Med33911942009780339
- LarstadMLohCLjungkvistG2002Determination of ethane, pentane and isoprene in exhaled air using a multi-bed adsorbent and end-cut gas-solid chromatographyAnalyst1271440512475031
- LeafDAKleinmanMTHamiltonM1997The effect of exercise intensity on lipid peroxidationMed Sci Sports Exerc29103699268960
- LeuppiJDSalomeCMJenkinsCR2001Predictive markers of asthma exacerbation during stepwise dose reduction of inhaled corticosteroidsAm J Respir Crit Care Med1634061211179114
- LiuJThomasPS2005Exhaled breath condensate as a method of sampling airway nitric oxide and other markers of inflammationMed Sci Monit11MT53MT6216049390
- LohLCKanabarVD’AmatoM2005Sputum induction in corticosteroid-dependant asthmatics: risks and airway cellular profileAsian Pac J Allergy Immunol231899616572738
- LouhelainenNRytilaPObaseY2008The value of sputum 8-isoprostane in detecting oxidative stress in mild asthmaJ Asthma451495418350407
- LundbergJONordvallSLWeitzbergE1996Exhaled nitric oxide in paediatric asthma and cystic fibrosisArch Dis Child7532368984919
- MaestrelliPEl MesslemaniAHDeFO2001Increased expression of heme oxygenase (HO)-1 in alveolar spaces and HO-2 in alveolar walls of smokersAm J Respir Crit Care Med16415081311704604
- MaziakWLoukidesSCulpittS1998Exhaled nitric oxide in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med15799810029517624
- MetsoTHaahtelaTSeveusL2002aIdentification of intracellular markers in induced sputum and bronchoalveolar lavage samples in patients with respiratory disorders and healthy personsRespir Med969182612418590
- MetsoTRytilaPPetersonC2001Granulocyte markers in induced sputum in patients with respiratory disorders and healthy persons obtained by two sputum-processing methodsRespir Med95485511207017
- MetsoTVengePHaahtelaT2002bCell specific markers for eosinophils and neutrophils in sputum and bronchoalveolar lavage fluid of patients with respiratory conditions and healthy subjectsThorax574495111978925
- MondinoCCiabattoniGKochP2004Effects of inhaled corticosteroids on exhaled leukotrienes and prostanoids in asthmatic childrenJ Allergy Clin Immunol114761715480313
- MontuschiPBarnesPJRobertsLJ2004Isoprostanes: markers and mediators of oxidative stressFASEB J18179180015576482
- MontuschiPCollinsJVCiabattoniG2000Exhaled 8-isoprostane as an in vivo biomarker of lung oxidative stress in patients with COPD and healthy smokersAm J Respir Crit Care Med1621175710988150
- MontuschiPCorradiMCiabattoniG1999Increased 8-isoprostane, a marker of oxidative stress, in exhaled condensate of asthma patientsAm J Respir Crit Care Med1602162010390403
- MorrowJDHillKEBurkRF1990A series of prostaglandin F2-like compounds are produced in vivo in humans by a non-cyclooxygenase, free radical-catalyzed mechanismProc Natl Acad Sci USA87938372123555
- MorrowJDRobertsLJ2002The isoprostanes: their role as an index of oxidant stress status in human pulmonary diseaseAm J Respir Crit Care Med166S25S3012471085
- MurtzMFrechBUrbanW1999High-resolution cavity leak-out absorption spectroscopy in the 10-ìm regionApp Phys682439
- NagaiKBetsuyakuTKondoT2006Long term smoking with age builds up excessive oxidative stress in bronchoalveolar lavage fluidThorax6149650216537669
- NathanCXieQW1994Regulation of biosynthesis of nitric oxideJ Biol Chem2691372587514592
- NelsonBVSearsSWoodsJ1997Expired nitric oxide as a marker for childhood asthmaJ Pediatr13042379063418
- [NHLBI/WHO] National Heart, Lung and Blood Institute; World Health Organization2002Global strategy for asthma management and preventionWorkshop Report. Publication No 02–3659
- NicholasBSkippPMouldR2006Shotgun proteomic analysis of human-induced sputumProteomics6439040116819730
- NicholsonJKLindonJCHolmesE1999‘Metabonomics’: understanding the metabolic responses of living systems to pathophysiological stimuli via multivariate statistical analysis of biological NMR spectroscopic dataXenobiotica291181910598751
- NiewoehnerDEKleinermanJRiceDB1974Pathologic changes in the peripheral airways of young cigarette smokersN Engl J Med29175584414996
- NightingaleJARogersDFBarnesPJ1998Effect of repeated sputum induction on cell counts in normal volunteersThorax5387909624290
- NorzilaMZFakesKHenryRL2000Interleukin-8 secretion and neutrophil recruitment accompanies induced sputum eosinophil activation in children with acute asthmaAm J Respir Crit Care Med1617697410712320
- NowakDAntczakAKrolM1996Increased content of hydrogen peroxide in the expired breath of cigarette smokersEur Respir J965278726926
- OhbayashiH2002Matrix metalloproteinases in lung diseasesCurr Protein Pept Sci34092112370004
- OkazawaAKawikovaICuiZH19978-Epi-PGF2alpha induces airflow obstruction and airway plasma exudation in vivoAm J Respir Crit Care Med155436419032175
- PaggiaroPLChanezPHolzO2002Sputum inductionEur Respir J Suppl373s8s12361361
- PapiARomagnoliMBaraldoS2000Partial reversibility of airflow limitation and increased exhaled NO and sputum eosinophilia in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med1621773711069811
- ParediPKharitonovSABarnesPJ2002Analysis of expired air for oxidation productsAm J Respir Crit Care Med166S31S3712471086
- ParediPKharitonovSABarnesPJ2000aElevation of exhaled ethane concentration in asthmaAm J Respir Crit Care Med1621450411029360
- ParediPKharitonovSALeakD2000bExhaled ethane, a marker of lipid peroxidation, is elevated in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med1623697310934055
- ParksWCShapiroSD2001Matrix metalloproteinases in lung biologyRespir Res210911686860
- PeltoniemiMKaarteenaho-WiikRSailyM2004Expression of glutaredoxin is highly cell specific in human lung and is decreased by transforming growth factor-beta in vitro and in interstitial lung diseases in vivoHum Pathol351000715297967
- PeltoniemiMJRytilaPHHarjuTH2006Modulation of glutaredoxin in the lung and sputum of cigarette smokers and chronic obstructive pulmonary diseaseRespir Res713317064412
- PerssonMGZetterstromOAgreniusV1994Single-breath nitric oxide measurements in asthmatic patients and smokersLancet34314677904005
- PierrouSBrobergPO’DonnellRA2007Expression of genes involved in oxidative stress responses in airway epithelial cells of smokers with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med1755778617158281
- PizzichiniEPizzichiniMMEfthimiadisA1996Indices of airway inflammation in induced sputum: reproducibility and validity of cell and fluid-phase measurementsAm J Respir Crit Care Med154308178756799
- PizzichiniMMPizzichiniEEfthimiadisA1998Asthma and natural colds. Inflammatory indices in induced sputum: a feasibility studyAm J Respir Crit Care Med1581178849769279
- PostleADGonzalesLWBernhardW2006Lipidomics of cellular and secreted phospholipids from differentiated human fetal type II alveolar epithelial cellsJ Lipid Res4713223116513897
- RabeKFHurdSAnzuetoA2007Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med1765325517507545
- RaherisonCBaldiITunon-De-LaraJM2003Asthma phenotypes according to the timing of smoking onset in young adultsInt J Tuberc Lung Dis7849212701840
- RahmanI2004Reproducibility of oxidative stress biomarkers in breath condensate: are they reliable?Eur Respir J23183414979486
- RahmanIAdcockIM2006Oxidative stress and redox regulation of lung inflammation in COPDEur Respir J282194216816350
- RahmanIBiswasSK2004Non-invasive biomarkers of oxidative stress: reproducibility and methodological issuesRedox Rep91254315327743
- RahmanIMacNeeW1999Lung glutathione and oxidative stress: implications in cigarette smoke-induced airway diseaseAm J Physiol277L1067L108810600876
- RahmanIMacNeeW2000Oxidative stress and regulation of glutathione in lung inflammationEur Respir J165345411028671
- RahmanIMacNeeW1998Role of transcription factors in inflammatory lung diseasesThorax53601129797762
- RahmanIMorrisonDDonaldsonK1996Systemic oxidative stress in asthma, COPD, and smokersAm J Respir Crit Care Med1541055608887607
- RahmanIvan SchadewijkAACrowtherAJ20024-Hydroxy-2-nonenal, a specific lipid peroxidation product, is elevated in lungs of patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med166490512186826
- RajJUAliferisCCaprioliRM2007Genomics and proteomics of lung disease: conference summaryAm J Physiol Lung Cell Mol Physiol293L45L5117468134
- RepineJEBastALankhorstI1997Oxidative stress in chronic obstructive pulmonary disease. Oxidative Stress Study GroupAm J Respir Crit Care Med156341579279209
- RobbinsRAFloreaniAAVon EssenSG1996Measurement of exhaled nitric oxide by three different techniquesAm J Respir Crit Care Med153163158630613
- RytilaPRehnTIlumetsH2006Increased oxidative stress in asymptomatic current chronic smokers and GOLD stage 0 COPDRespir Res76916646959
- RytilaPHLindqvistAELaitinenLA2000Safety of sputum induction in chronic obstructive pulmonary diseaseEur Respir J151116910885433
- SaettaM1999Airway inflammation in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med160S17S2010556163
- SaettaMTuratoGMaestrelliP2001Cellular and structural bases of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med1631304911371392
- SalehDErnstPLimS1998Increased formation of the potent oxidant peroxynitrite in the airways of asthmatic patients is associated with induction of nitric oxide synthase: effect of inhaled glucocorticoidFASEB J12929379707165
- ScanlonPDConnettJEWallerLA2000Smoking cessation and lung function in mild-to-moderate chronic obstructive pulmonary disease. The Lung Health StudyAm J Respir Crit Care Med1613819010673175
- SeemungalTADonaldsonGCBhowmikA2000Time course and recovery of exacerbations in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med16116081310806163
- ShahidSKKharitonovSAWilsonNM2005Exhaled 8-isoprostane in childhood asthmaRespir Res67916042771
- SilvestriMSpallarossaDFrangova YourukovaV1999Orally exhaled nitric oxide levels are related to the degree of blood eosinophilia in atopic children with mild-intermittent asthmaEur Respir J13321610065675
- SimpsonJLTimminsNLFakesK2004Effect of saliva contamination on induced sputum cell counts, IL-8 and eosinophil cationic protein levelsEur Respir J237596215176693
- SimpsonJLWoodLGGibsonPG2005Inflammatory mediators in exhaled breath, induced sputum and salivaClin Exp Allergy351180516164445
- SippelJMHoldenWETillesSA2000Exhaled nitric oxide levels correlate with measures of disease control in asthmaJ Allergy Clin Immunol1066455011031334
- SmithADCowanJOBrassettKP2005Use of exhaled nitric oxide measurements to guide treatment in chronic asthmaN Engl J Med35221637315914548
- SmithCMAndersonSD1990Inhalational challenge using hypertonic saline in asthmatic subjects: a comparison with responses to hyperpnoea, methacholine and waterEur Respir J3144512178963
- SuYHanWGiraldoC1998Effect of cigarette smoke extract on nitric oxide synthase in pulmonary artery endothelial cellsAm J Respir Cell Mol Biol19819259806747
- SugiuraHIchinoseMYamagataS2003Correlation between change in pulmonary function and suppression of reactive nitrogen species production following steroid treatment in COPDThorax5829930512668791
- SutherlandERCrapoJDBowlerRP2006N-acetylcysteine and exacerbations of chronic obstructive pulmonary diseaseCOPD319520217361500
- TaubeCHolzOMuckeM2001Airway response to inhaled hypertonic saline in patients with moderate to severe chronic obstructive pulmonary diseaseAm J Respir Crit Care Med1641810511734428
- TetleyTD2005Inflammatory cells and chronic obstructive pulmonary diseaseCurr Drug Targets Inflamm Allergy46071817305517
- TwaddellSHGibsonPGCartyK1996Assessment of airway inflammation in children with acute asthma using induced sputumEur Respir J9210488902474
- van AalderenWMSprikkelmanABHoekstraMO1999Is childhood asthma an inflammatory disease?Allergy54Suppl 4962710422750
- van BeurdenWJHarffGADekhuijzenPN2002An efficient and reproducible method for measuring hydrogen peroxide in exhaled breath condensateRespir Med9619720311908513
- van DalenCJKettleAJ2001Substrates and products of eosinophil peroxidaseBiochem J358233911485572
- Van HoydonckPGWuytsWAVanaudenaerdeBM2004Quantitative analysis of 8-isoprostane and hydrogen peroxide in exhaled breath condensateEur Respir J231899214979489
- Vlachos-MayerHLeighRSharonRF2000Success and safety of sputum induction in the clinical settingEur Respir J16997100011153606
- WaltersEHGardinerPV1992Bronchoalveolar lavage findings and bronchial hyperreactivityRespiration59Suppl 1681579738
- WardRWoltmannGWardlawAJ1999Between-observer repeatability of sputum differential cell counts. Influence of cell viability and squamous cell contaminationClin Exp Allergy292485210051730
- WarkPAJohnstonSLMoricI2002Neutrophil degranulation and cell lysis is associated with clinical severity in virus-induced asthmaEur Respir J19687511852895
- WarkPASimpsonJLHensleyMJ2001Safety of sputum induction with isotonic saline in adults with acute severe asthmaClin Exp Allergy3117455311696051
- WilsonAMLeighRHargreaveFE2006Safety of sputum induction in moderate-to-severe smoking-related chronic obstructive pulmonary diseaseCOPD3899317175671
- WoodLGGibsonPGGargML2003Biomarkers of lipid peroxidation, airway inflammation and asthmaEur Respir J211778612570126
- WoodLGGargMLSimpsonJL2005Induced sputum 8-isoprostane concentrations in inflammatory airway diseasesAm J Respir Crit Care Med1714263015579724
- WuWSamoszukMKComhairSA2000Eosinophils generate brominating oxidants in allergen-induced asthmaJ Clin Invest10514556310811853
- ZayasuKSekizawaKOkinagaS1997Increased carbon monoxide in exhaled air of asthmatic patientsAm J Respir Crit Care Med156114039351613
