Abstract
Patients with COPD have high risk for osteoporosis and fractures. Hip and vertebral fractures might impair mobility, and vertebral fractures further reduce lung function. This review discusses the evidence of bone loss due to medical treatment opposed to disease severity and risk factors for COPD, and therapeutic options for the prevention and treatment of osteoporosis in these patients. A review of the English-language literature was conducted using the MEDLINE database until June 2009. Currently used bronchodilators probably lack adverse effect on bone. Oral corticosteroids (OCS) increase bone resorption and decrease bone formation in a dose response relationship, but the fracture risk is increased more than reflected by bone densitometry. Inhaled corticosteroids (ICS) have been associated with both increased bone loss and fracture risk. This might be a result of confounding by disease severity, but high doses of ICS have similar effects as equipotent doses of OCS. The life-style factors should be modified, use of regular OCS avoided and use of ICS restricted to those with evidenced effect and probably kept at moderate doses. The health care should actively reveal risk factors, include bone densitometry in fracture risk evaluation, and give adequate prevention and treatment for osteoporosis.
Introduction
Chronic obstructive pulmonary disease (COPD) is, and will increasingly be, a major cause of morbidity and mortality worldwide.Citation1 COPD develops as a consequence of genetic susceptibility, increasing life span, environment and life-style factors. Aging of the population, shared risk factors, especially tobacco smoking, systemic effects by the disease and side effects of treatment contribute to the fact that COPD patients often have many comorbidities.Citation2–Citation4 among these osteoporosis and increased fracture risk.
Patients with moderate to severe COPD have limitations in physical activity, and fractures inevitably could be a heavy additional burden to their dyspnea. Among the oldest, the often disabling consequences of hip fractures frequently initiate the patients’ need for home care, transfer to nursery homes and shortening of life. Vertebral fractures influence the mobility of the patients, are associated with back pain, and may also increase dyspnea, as increased thoracic kyphosis and decreased rib mobility add a restrictive component to their lung disease,Citation5,Citation6 Hence, effort should be given to secure as good “bone health” as possible in this group of patients.
The aims of this paper are to discuss the potential and observed adverse effect on bone by the medical treatment given to COPD patients, and also discuss to some extent, the contribution by the disease itself, life-style factors and comorbidities. Further, preventive and treatment strategies for osteoporosis are discussed.
Methods
A MEDLINE literature search for English language papers published until June 2009 was conducted using relevant key terms, in addition to examination of reference lists from pivotal studies and reviews.
Medical treatment of COPD
According to the Global initiative for chronic Obstructive Lung Disease’s guidelines (GOLD), www.goldcopd.com, bronchodilator medications are the main symptomatic treatment of COPD and these include short and long-acting β2-agonists and anticholinergics. They increase exercise capacity and health status, whilst long-acting anticholinergics additionally reduce the rate of COPD exacerbations and improve the effectiveness of pulmonary rehabilitation. Theophylline also is effective in COPD, but due to its potential toxicity inhaled bronchodilators are preferred.Citation1
Inhaled corticosteroids (ICS) are recommended for severe COPD patients with repeated exacerbations, as they have been shown to reduce the frequency of exacerbations and thus improve health status. ICS combined with a long-acting β2-agonist (LABA) are more effective than the individual components.Citation1 A recent network meta-analysis by Puhan and coworkers concluded that for mild to moderate COPD, single treatment with LABA or long-acting anticholinergics was the treatment of choice both for symptom control and exacerbation prevention, but for those with FEV1 < 40% predicted, long-acting anticholinergics was as effective as combination treatment in reducing exacerbations.Citation7
Oral corticosteroids (OCS) are recommended for 7 to 10 days with 30 to 40 mg prednisolone in exacerbations in patients with severe COPD, but chronic treatment with OCS should be avoided.Citation1
Osteoporosis
Bone
The skeleton is essential for terrestrial animal life, and human beings have evolved bone light enough to enable rapid mobility and strong enough to avoid disabling fractures during reproductive life.Citation8
Bone mass reaches the peak at age 25 to 30 years.Citation9 After a plateau phase, bone loss occurs throughout life with an age-associated annual bone loss of approximately 0.5% to 1%, but the rate of loss differs by sex, skeletal sites and age. In men, there is a rather constant bone loss from age 25 to 39 years, this increases mainly at the hips at age ≥65 years,Citation10 with further loss of cortical bone above the age of 75 years.Citation11 In women, bone loss begins at age 40 to 44, and is particularly rapid in the total hip at age 50 to 54 with a change of −6.8% over 5 years, with another acceleration in loss after age of 70 years.Citation10,Citation11
Prevalence of osteoporosis
Osteoporosis is the main risk factor for fragility fractures, defined as a fracture occurring after a fall from standing height or minor trauma. The lifetime risk of any fracture at age 50 years is about 50% among women and 20% among men.Citation12 Men at age 75 years have equivalent fracture risk as women aged 65 years.Citation13
Osteoporosis is defined as a skeletal disorder characterized by compromised bone strength predisposing a person to an increased risk for fracture. Bone strength primarily reflects the integration of bone density and bone quality.Citation14 An operational definition of osteoporosis, established by The World Health Organization (WHO), is based on bone mineral density (BMD).Citation15 Bone densitometry results are given as area density, but also as T-scores (standard deviations [SD] compared with young adult sex-matched controls) and Z-scores (compared with age-and sex matched controls). The WHO has defined osteopenia as BMD T-score −1 to −2.5 SD and osteoporosis as T-score below −2.5 SD.Citation15
Measures of BMD, bone quality and bone metabolism
Dual energy absorptiometry (DXA) at the hip is the best predictor of hip fractures and best standardized for the diagnosis of osteoporosis. Spine and hip BMD have similar value for predicting spine fractures,Citation16 but spondylarthrosis and minerals in the aorta might give artificially high values of BMD in the anterior-posterior directed measurements after the age of 60 to 65.Citation17
BMD at these sites are widely used in clinical practice to identify those at increased risk for fracture. However, a majority of fragility fractures occurs in women not being defined as osteoporotic.Citation18 The prediction of fractures in both genders improves if baseline BMD is replaced with change in BMD between measurements in the models.Citation19 Most clinicians, however, have to rely on one measurement estimating the patients fracture risk. Compared to other risk factors, BMD is at least as good in prediction of fracture as blood pressure measurements to predict stroke and level of cholesterol to predict cardiac infarction.Citation20
T-scores between different sites should not be compared, due to site differences regarding accuracy errors, variance in the population and algorithms for edge detections.Citation21 In a study of the same population of a DTX-base, the prevalence of osteoporosis in women aged 50 years or more, ranged from 11% at the hip, 24% at the spine, to 52% at the distal radius.Citation22
Mainly for research purposes, methods like Single X-ray Absorptiometry (SXA), Quantitative Ultrasound (QUS) and Quantitative Computed Tomography (QCT) have been used. Although measurement at a specific site is the best predictor of fracture at that site, forearm SXA is as good as lumbar BMD for prediction of hip fracture,Citation23,Citation24 other non-spine fracturesCitation25 and fragility fractures in general.Citation26 Correspondingly, quantitative ultrasound (QUS) of calcaneus has been used to estimate regional BMD-levels, evaluate bone qualityCitation27 and predict fracture risk,Citation28,Citation29 but this method has poor sensitivity for detecting osteoporosis defined as T-score < −2.5 SD.Citation30
Markers of bone turnover, as alkaline phosphatase, hydroxyproline, osteocalcin, pro-collagen peptides and pyridinium crosslinks, can enhance the predictive value of BMD.Citation20 However, due to large biological variability, they are of uncertain clinical relevance and have not been shown to predict the risk of fractureCitation31,Citation32 or to correlate with changes in BMD.Citation33 They might, however, reflect changes related to antiresorptive therapy more rapidly than changes in BMD.Citation34 In general, corticosteroid (CS) administration is followed by a reduction in bone formation markers, especially serum osteocalcin levels,Citation35–Citation37 and a trend to an increase or no change in bone resorption markers.Citation38
Risk factors for osteoporosis and fracture in COPD
High age and female sex are important risk factors for osteoporosis, with postmenopausal loss of ovarian hormones being the single most important factor. The prevalence of osteoporosis and incidence of fragility fractures differ substantially between populations, with highest figures in post-menopausal women of Northern European descent, especially those living in Scandinavia.Citation12,Citation39–Citation41 Both parental osteoporosis and fragility fractures, as well as previous fracture in the patient, are risk factors for further fracture.Citation42
Patients with COPD are at high risk for osteoporosis and fractures because of lifestyle factors, systemic effects of the disease, treatment and comorbidities (). Smoking is associated with low BMD in a dose-response relationship, not only in current smokers, but even ex-smokers.Citation43,Citation44 Female lungs seem to be more susceptible to harmful effects of tobacco smoking than male lungs.Citation45,Citation46 Increased prevalence of smoke related lung diseases in women and increasing proportion of women among smokers, might affect bone more negatively in women than men, through combined effects of COPD and smoking.
Figure 1 The development of bone mineral density (BMD) throughout life, factors of importance for level of BMD (genetics, sex), COPD-related factors lowering (BMD), and important factors influencing fracture risk in addition to level of BMD.
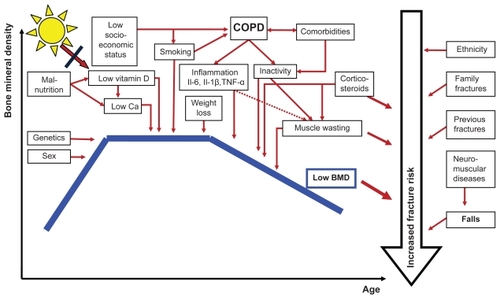
Furthermore, inactivity is an important risk factor for osteoporosis and fractures, partly due to increased risk for falling. A physically active life has been found to nearly halve the incidence of hip fractures in the older population,Citation47 and appendicular lean mass accounts for most of the explained variance among factors being positively associated with BMD.Citation41
COPD patients, as well as patients with other chronic diseases, often have deficient calcium (Ca) and vitamin D nutritional status,Citation48,Citation49 and the latter is frequently accentuated because of little exposure to sunlight. Weight loss is also associated with decreased BMDCitation50–Citation52 and a recent review reported BMD to be 3% to 7% higher for every 10 kg increase in weight.Citation43 Correspondingly, a recent study found that ≥5% weight loss was associated with a 33% increased risk of forearm fractures.Citation53
In the recent years, a detrimental effect on bone also caused by COPD itself has been suggested.Citation3,Citation54 Among many possible explanations, most current evidence indicates that this is a result of mediators, cytokines (interleukin [Il]-6, Il-1β and TNF-α) or activated inflammatory cells reaching the systemic circulation from inflammation in the lungs.Citation3,Citation4 The extent of this contribution is unclear, but the fact that patients on OCS have higher risk of fractures compared to untreated patients with similar underlying inflammatory diseasesCitation55 indicates that this is not one of the main causes of the influence on bone.
Medicine-induced osteoporosis in COPD
Many studies have addressed this subject, but the main problem or limitation of many of these studies are the power to reveal any effect, and, in case of effect, to differentiate between possible effects by medication, disease severity and factors mentioned above. There have been a few large, randomized, double-blind, clinical trials (RCT), many observational case-control and cohort studies, in addition to many meta-analyses. Some larger and important studies are based on registers as the UK General Practice Research Database (GPRD) (190,000 to 240,000 cases using CS).Citation56,Citation57 and Danish data based on the National Hospital Discharge Register and others (>125,000 fracture cases).Citation58
How can adverse effects on bone be measured?
Outcomes such as fractures, or surrogate measures of fracture risk, as BMD and biochemical markers for bone turnover, might be relevant for studies on adverse effects on bone. RCT including fractures as primary outcome would give the best evidence of such an effect. However, even as lifetime fracture risk is high, only a small number of subjects at risk actually sustain a fracture during few years observation time. For example, in any year, fractures occur in 1 to 2 per 100 women aged 65 years, 6 to 10 per 100 women aged 75 years, and only 1 to 2 per 2,000 of the 15% of women <60 years of age with osteoporosis.Citation59 Even for BMD, there are problems with the power of studies. Wisniewski et al calculated that a prospective study comparing a dose of 1 mg beclomethasone dipropionate (BDP) equivalents with placebo, would require 2,500 individuals in each limb for 95% power to detect the difference of 0.1 SD in BMD found in their cross-sectional study.Citation60
Airway obstruction, COPD and bone
Airflow obstruction is associated with increased risk of osteoporosis compared with normal lung function.Citation61,Citation62 COPD is an independent predictor of BMD reductionCitation63–Citation65 and vertebral fracture risk.Citation66 Studies have shown more than two-fold prevalence of osteoporosis in CS-naïve COPD patients, compared both with healthy controlsCitation67 and asthma patients.Citation68 Increasing disease severity increases the risk for osteoporosis,Citation29,Citation61,Citation69 and in severe COPD osteoporosis and osteopenia have been found in as many as 66% and 31%, respectively.Citation70
Correspondingly, the fracture risk is positively associated with COPD severity.Citation71 In mild COPD the fracture risk is similar to what was found in the European Vertebral Osteoporosis Study (EVOS),Citation72 with a prevalence of vertebral deformity of 12% in both genders aged 50 to 79 years,Citation73 but more COPD patients than healthy, had at least 1 severe vertebral fracture (OR = 3.75).Citation6 Nuti et al reported at least 1 vertebral fractures in about 40% of COPD patients, with a strong association between disease severity and fractures, especially in men,Citation71 and in a recent Norwegian study, the number of vertebral deformities was almost twice as high in GOLD stage III compared to II in women.Citation74 In the large Danish register study, comparing subjects with and without COPD, COPD adjusted for use of CS was associated with increased risk for hip and vertebral fracture (relative risk [RR] 1.63 and 1.23), but not for forearm fractures. Comparing those with and without asthma, revealed an asthma-related increased risk for only hip fracture (RR 1.32).Citation58
Vertebral compression fractures often are asymptomatic, and among severe COPD patients, not previously diagnosed compression fractures were found in 24%.Citation75 A prospective study revealed that compared to subjects without COPD, incident COPD patients had increased risk for osteoporosis and fracture (RR 3.1 and 1.6, respectively) within the first year after diagnosis.Citation2
Treatment of COPD and effect on bone
Oral glucocorticoids
A GPRD study documented that women aged ≥85 years using ≥7.5 mg prednisolone daily had an excess in number of hip fracture cases of 1.4 cases per 100 patients per year compared to non-users, and as many as 47% and 72% of all hip and vertebral fractures, respectively, could be attributed to OCS.Citation76 Walsh et al found that patients on OCS for ≥6 months compared to controls had increased risk of osteoporotic fractures of the vertebrae (OR 10), hip (OR 6), and ribs or sternum (OR 3.2).Citation77
In a comprehensive meta-analysis van Staa et al found strong correlations between cumulative dose and bone loss and between daily dose (>5 mg prednisolone) and risk of fracture. The fracture risk increased within 3 to 6 months after the start of OCS, and decreased after stopping therapy. The increased risk remained independent of underlying disease, age and gender.Citation78 Later, van StaaCitation79 reviewed several large population based studies on fracture risk in CS users, and found consistent increased fracture risk in CS users in the hip (RR 1.61 to 2.01) and spine (RR 2.60 to 4.16). Only one study from the GPRD showed a minor increased risk for forearm fractures compared to controls (RR 1.09).Citation57 In a study by Angeli et al including 551 post-menopausal women given CS for different diseases, the adjusted prevalence of asymptomatic vertebral fractures was 38% for asthma/COPD. No significant association, however, was found between fractures and CS cumulative dose or duration of therapy.Citation80
These studies confirm that the vertebral bodies are affected earlier and more severely than cortical bone of the long bones (radius, humerus) during OCS treatment.Citation81 Different patterns of loss have also been demonstrated within the lumbar spine with greater damage to the trabecular bone than the cortical bone of the spinosi and apophyseal area.Citation82
Dose response relationship
There have been discussions on a threshold dose above which oral CS cause bone loss. The two large register-based studies both found increased risk for hip and vertebral fractures in a dose response relationship above daily doses as low as 2.5 mg prednisone equivalents,Citation57,Citation58 and similar results have later been demonstrated by de Vries et alCitation56 (). In line with this, Li et al found that COPD patients with a fracture history, reported treatment with higher doses of prednisone compared to those without fractures.Citation70
Table 1 Adjusted odds ratio for fracture risk at different sites by daily dose of prednisolone in UK General Practice Research Database (GPRD) and Danish large register studies
However, opposed to this, recent analyses of the Danish registerCitation83 and the Dutch PHARMO-RLS databaseCitation84 did not find any increase in overall fracture risk for prednisolone doses <7.5 mg per day. This could be a result of less residual confounding due to adjustments for proxies for disease severity and other risk factors for fractures. A limitation of register-based studies, is lack of individual life style data, but inclusion of such data rather should weaken the association between CS use and fracture.
Increased fracture risk by duration of OCS use has been found in studies on patients with rheumatoid arthritis and lupus,Citation85–Citation87 and both WalshCitation77 and de VriesCitation56 with coworkers have reported a substantial increased risk for fractures with increasing cumulative dose of CS. Walsh found that the highest compared to lowest cumulative quartile (median prednisolone dose 61 g versus 5 g) had an increased risk ranging from 2 for all fractures to 9 for vertebral fractures.Citation77 Results from two RCTs, however, indicated that not the cumulative, but the daily CS dose was a strong predictor for vertebral fracture, with 60% increase in risk for each 10 mg increase in prednisolone dose.Citation88 Based on an administrative US database, Steinbuch et al reported dose response relationship for both duration and dose of OCS. Long and continuous use of CS resulted in a significant 5-fold increased risk of hip and 6 fold increased risk of vertebral fractures. Adding high doses of prednisolone to this, the RR increased to 7-fold for hip and 17-fold for vertebral fractures.Citation89
CS related bone loss is most rapid during the first 6 months of OCS treatment (on average 5%), after which there seems to be a slower but steady loss of bone (1% to 2% per year).Citation90,Citation91
An increased risk for fractures has been shown for doses above 5 mg/day within 3 to 6 months after initiation of OCS therapy,Citation78,Citation89 and for doses of ≥10 mg prednisolone for less than 60 days with an increasing trend by time.Citation83 Vestergaard and coworkers also found an effect of lower doses within 60 days, but this effect did not last beyond 2 months, and was probably an effect of confounding by indication. Correspondingly, van Staa found increased fracture risk even before OCS was initiated.Citation57
Avoidance of continuous use has been believed to reduce adverse effects on bone.Citation92 Alternate, in stead of daily use of OCS has not been found to reduce bone loss in adults.Citation93,Citation94 However, long-time sporadic use has been reported to be associated with a 2-fold increased fracture risk, compared to a 6-fold increased fracture risk in those with continuous use of OCS Citation89. In a GPRD study, patients with previous cumulative dose CS ≤ 1 g with intermittent high-dose CS (daily dose ≥15 mg) only had a small increased risk, whilst those with a daily dose ≥30 mg and cumulative exposure >5 g had a relative risk of hip/femur and vertebral fracture of 3.13 and 14.42, respectively.Citation56
Treatment of exacerbations is an important exposure for OCS in COPD patients. Dubois et al showed that OCS courses were associated with more harmful effects against bone compared to continuous OCS treatment regimens (>10 mg prednisolone/day).Citation95 The study indicated alarming bone loss of a cumulative dose above 1 g of prednisolone equal to 2 to 3 OCS courses. Corresponding effect on lumbar BMD has been reported in asthma patients receiving more than 2.5 courses of OCS compared to fewer.Citation96
Reversible effect
Regaining of BMD to normal levels was found in the 1990s in patients cured for Cushing diseaseCitation97 and patients having stopped OCS therapy.Citation87,Citation98 Newer register studies showed that the increased risk of fracture in OCS-users mostly disappeared within one year after stopping therapy, most pronounced for vertebral fractures, but even the risk for hip fractures was reduced towards baseline levels.Citation57,Citation58,Citation83 There is a rapid decrease in fracture risk beginning already three months after stopping CS treatment,Citation56 but the time for fracture risk to return to normal, depend on the cumulative dose used, from 6 months after cumulative dose of less than 1 g prednisolone to at least 15 months at higher cumulative dose and daily dose above 15 mg.Citation56 However, at cumulative doses >10 g there is both a thinning and perforation of the trabeculae of such an extent that bone recovery is precluded after withdrawal of CS.Citation99
OCS and BMD
Due to disruption of collagen structure and bone architecture, rather than demineralization by CS treatment,Citation100,Citation101 the increased fracture risk in OCS users seems to be mostly independent of BMD. This explains why adjustments for BMD have not changed substantially the relative fracture rate in OCS,Citation102 and why CS users compared to non-users have higher risk for vertebral fractures at the same levels of BMD.Citation88
However, bone loss due to OCS can be measured by BMD. This was first found after short time use in patients with rheumatoid arthritis and chronic fatigue syndrome;Citation98,Citation103 a mean daily dose of 7.5 mg prednisolone for 20 weeks led to 9% increased loss in trabecular bone compared to placebo.Citation98 Corresponding effects of OCS on BMD are found in COPD patients.
ICS and bone
Medication for inhalation was developed in order to ensure high deposition in the airways with lowest possible systemic side effects. Even though the gastrointestinal absorption of ICS like budesonide (BUD) and fluticasone (FLU) is very low compared to BDP and triamcinolone (TCA),Citation104 the active medication deposited in the airway, will reach the systemic circulation. Adverse effects on bone could be possible, and reviewers have found reason to concern about this.Citation105,Citation106
ICS and fractures
Randomized controlled trials (RCT)
As part of a systematic review and meta-analysis of RCT, Drummond et al included three larger studies on ICS with fractures as secondary outcome.Citation107 The studies compared combined salmeterol (SAL)/fluticasone (FLU) with each components alone and placebo for a period of 3 years in 6,112 COPD patients,Citation36 FLU with placebo in 751 patients with moderate to severe COPD,Citation108 and BUD with placebo in 1,277 smokers with mild COPD for 3 years.Citation73 Despite use of rather high doses (FLU 500 μg twice daily and BUD 400 μg twice daily), no difference in fracture risk was found between the treatment groups. A Cochrane review of seven RCT found no effects of 2 to 3 years use of conventional doses of ICS on BMD or fracture risk, but very high doses were associated with increase in markers of bone turnover.Citation31 Altogether the studies included cases with mild to severe COPD, doses considered as moderate to high, but the follow-up time was short compared to what is the case for most COPD patients.
Observational studies
Knowledge on potential effects of ICS on bone could be derived from studies including asthma patients, as these lack many of the negative life-style factors characteristic of COPD patients. Lipworth et al in 2002 reviewed available literature on ICS and systemic adverse effects published from 1966 through 1998, and found that all ICS, but especially FLU (at doses above 800 μg), exhibited dose-related adrenal suppression, a risk factor for bone loss. Data on bone turnover, however, were not included in these studies.Citation109
In 2003 Richy et al reviewed all controlled trials having data on ICS, and BMD/markers/fractures in asthma, COPD and healthy persons.Citation110 Data from the included studies showed that all considered ICS, compared with placebo or controls, appeared to affect bone markers or lumbar BMD in asthma, COPD or in healthy adults, but the study lacked power to investigate fracture risk. TCA led to the most deleterious effects on bone, followed by BDP and BUD. There was a dose response relationship, both regarding daily dose and duration of ICS use, and bone loss. Assuming a linear bone loss in CS-induced osteoporosis, use of TCA 1 mg/day during 20 years would lead to an estimated 6.7% decrease in BMD compared with unexposed asthma or COPD controls, whereas corresponding figure for BUD would be 2.4%. However, as the authors discussed, there might be not-linear time-effect model due to compensatory mechanisms in patients exposed to ICS on a long-term basis. Furthermore, two of the studiesCitation73,Citation111 included specifically smokers, who where older than in the other studies. Excluding these, rendered the results non-significant, suggesting that an effect of aging, smoking and higher cumulative dose of ICS might have influenced the results.
Based on the Danish register, Vestergaard et al found a limited increase in the risk of any fracture, but not hip, spine or forearm fractures, in ICS-users of more than 7.5 mg prednisolone equivalents per day (equivalent to 1875 μg of BUD per day).Citation58 Van Staa et al based on GPRD data, four years earlier, had reported increased risk for fracture at all these sites, and even in a dose-response relationship effect by ICS. However, they did neither find differences in fracture risk between the ICS and bronchodilator groups compared with non-users, nor between users of different ICS (BUD, FLU and BDP).Citation112 Restricting a study to elderly women in the same database, Hubbard et al, found ICS-use to be associated with increased fracture risk (OR 1.19 adjusted for OCS) and in a dose response relationship.Citation113 Including disease severity indicators as confounders in a study from the same database, de Vries et al found that the crude two-fold fracture risk at the hip in patients on high dose ICS (>1.6 mg) was reduced to similar risk as non-users of ICS,Citation66 and later they found similar result in a Dutch study.Citation84
However, even recent studies have reported a small increase in fracture risk by ICS, but mainly with use of higher doses.Citation71,Citation114,Citation115
CS have less influence on appendicular bone than hip and spine. Even so, in a cross-sectional population-based study in Norway, current users of only ICS had 2% lower forearm BMD compared to ICS-naïve individuals, and additional use of OCS was associated with 8% lower BMD.Citation116 Similar results were found during a follow-up study for 5 years,Citation117 but despite the possibility to adjust for both diseases severity, other risk factors and individual life style factors, lack of any dose response relationship between ICS-use and BMD, could indicate confounding by disease severity.
The studies do not fully preclude adverse effects of at least high dose ICS on bone, but what is the clinical relevance of such an effect? Weatherall et al addressed this in a recent systematic review and meta-analysis of 5 case-control studies of ICS use.Citation118 The random-effects odds ratio of relative risk for a non-vertebral fracture was 1.12 (95% confidence interval 1.00 to 1.26) per 1.0 mg increase in the daily dose of BDP or equivalent. This risk was considerably less than other common risk factors for fracture in the older adult, with figures of: 1 or more falls 4.7, use of antipsychotic medication 2.8, body mass index <18.5 kg/m2 2.4, cerebrovascular disease 1.9, use of hypnotic medication 1.7, and being a current smoker 1.5.Citation118
What dose level of ICS is used in COPD?
Mild asthma is very responsive to CS, and most of the therapeutic effect of ICS is obtained at doses around 400 to 500 μg of BDP equivalents, with the mean dose achieving the maximum benefit being around 1,000 μg/day.Citation119,Citation120 CS suppress the multiple inflammatory genes that are activated through recruitment of the enzyme histone deacetylase 2 (HDAC2). Smoking, however, contributes to steroid resistanceCitation121 through negative effect on HDAC2.Citation122 Hence, for optimal CS response, COPD patients and smoking asthma patients need higher CS doses compared with non-smokers. As the introduction of ICS combined with LABA in asthma patients has led to asthma control at lower ICS doses,Citation123 the concern for negative effects on bone among these patients are minimized compared to smokers with asthma or COPD. Even though significant differences between single ICS and combination therapy on BMD and bone metabolism markers were not found, a study indicated more favorable pattern for the combination therapy.Citation124
RCTs on the effect of ICS on different outcomes in COPD patients have mostly used higher doses of ICS than is generally used in asthma patients. Daily doses of FLU have been 500 μg twice daily,Citation36,Citation108,Citation125–Citation128 BUD 320 to 400 μg twice dailyCitation73,Citation129–Citation131 and TCA 1,200 μg/day.Citation111 Recently, however, Ferguson et al published a RCT reporting a similar reduction in annual rate of exacerbation by FLU/SAL 250/50 μg/mg twice daily (30% compared with SAL) as reported in previous studies of double ICS dose.Citation132 Two other studies of shorter duration (24 weeks) showed that FLU/SAL 250/50 bid improved lung function and reduced severity of dyspnea compared with individual components and placebo, but these had not power to study exacerbations.Citation133,Citation134 Further studies on defining the lowest dose needed to reach the desirable effects of ICS are therefore warranted. Today there is a discrepancy between the size of doses used in the majority of studies and doses prescribed in the clinic. In the US, higher doses than FLU/SAL 250/50 and BUD/FOR 320/9 μg/mg twice daily are currently not approved for use in COPD.
For CS exposure during exacerbations, Stallberg et al in a RCT found no difference between 2 weeks of high-dose BUD/FOR combination and prednisolone 30 mg.Citation135 Even if all patients were given one dose of prednisolone 30 to 50 mg before randomization, the total CS exposure in those getting ICS would be about one-third of those receiving OCS.
Bone turnover and influence of inflammation
In all individuals there is a continuous bone remodeling, and in adults about 25% of trabecular and 3% of cortical bone are replaced each year.Citation136 Central cells in this balance are osteoclasts, which resorb bone, and osteoblasts, which replace lost bone with new matrix, which subsequently mineralizes. Osteocytes and their canicular network serve as mechanosensors, and play a role in the repair of bone microdamage.Citation137 There is a close interaction between osteoblasts and osteoclasts, mainly mediated by receptor activator of NF-κB ligand (RANKL) and osteoprotegerin (OPG). RANKL is expressed on the surface of osteoblasts, and its expression increases in response to different pro-resorptive signals such as proinflammatory cytokines, CS, estrogen deficiency and excess of parathyroid hormone.Citation138 RANKL is the critical stimulator of the differentiation and activity of ostoclasts leading to bone resorption. OPG is a decoy receptor that is secreted by osteoblasts and reduces bone resorption by binding to RANKL.Citation139,Citation140
The influence of inflammatory diseases on bone is thoroughly discussed in a recent review by Hardy and Cooper.Citation140 Shortly, inflammatory cells also express or secrete RANKL, or produce cytokines (TNF-α and interleukins) promoting bone resorption independent of osteoblasts.Citation141 Why increased bone resorption is not followed by bone formation is unclear, but at least TNF-α inhibit the differentiation of osteoblasts.Citation142
Interestingly, inflammation modifies the action of the enzymes, 11β-hydroxysteroid dehydrogenases (11β-HSDs) responsible for the intracellular CS metabolism. One of these converts inactive CS such as cortisone and prednisone to their active counterparts cortisol and prednisolone. Exposure to proinflammatory cytokines increases the levels of autocrine generated cortisol in the osteoblasts, leading to decreased bone formation through direct effect on osteoblasts, as well as increased osteoclast activity due to upregulation of RANKL and downregulation of OPG.Citation139,Citation143 The 11β-HSDs might contribute to the individual heterogeneity in the response to CS therapy. A common polymorphism in the efflux transporter P-glycoprotein which is associated with CS sensitivity might also confer susceptibility to CS-induced osteoporosis.Citation144
The pathogenesis of CS-induced osteoporosis
shows the bone cells and mechanisms being involved in CS-induced bone loss. The loss occurs in two phases, a rapid early phase, probably due to excessive bone resorption, and a slower, progressive phase due to impaired bone formation.Citation145,Citation146 In the first phase CS increase the expression of RANKL and macrophage colony stimulating factor, while decreasing the expression of OPG in stromal and osteoblastic cells, thereby favoring osteoclast differentiation and bone resorption.Citation139 Furthermore, CS decrease the apoptosis of mature osteoclasts leading to a prolonged bone resorption.Citation147 The excess resorption, however, falls with long-term CS, probably due to inhibition of differentiation of osteoclast precursors.Citation147
Figure 2 Diagram showing the direct and indirect effects of glucocorticoids on bone leading to glucocorticoid-induced osteoporosis and fractures. Reproduced with permission from Canalis E, Mazziotti G, Giustina A, Bilezikian JP. Glucocorticoid-induced osteoporosis: pathophysiology and therapy. Osteoporos Int. 2007;18(10):1319–1328.Citation149 Copyright © 2007 Taylor & Francis.
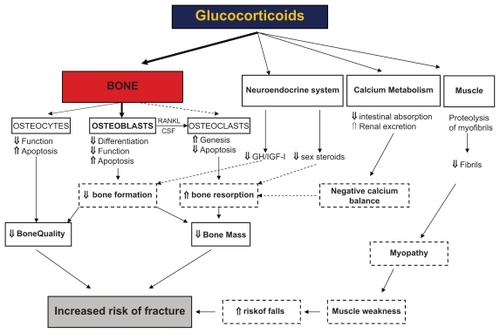
In the second phase, inhibition of proliferation, differentiation as well as maturation of osteoblasts, lead to impairment of bone formation.Citation148,Citation149
CS also exert negative effects on osteocytes by disturbing their mechanosensor function and inducing apoptosis.Citation150 This reduces the strength of bone, independently of changes in bone remodeling and architecture,Citation151 and might partly explain why patients treated with CS experience fractures at a higher BMD level than non-CS users. Additionally, CS have an indirect, negative effect on bone formation by reducing the expression of insulin like growth factor (IGF)1.Citation145 Low levels of gonadal steroids increase bone resorption.Citation152 However, even though CS decrease the level of these hormones, the adverse effects are still observed in patients with maintained menstrual cycle activity implying that the adverse effects of CS are largely independent of hypogonadism.Citation153
Secondary hyper-parathyroid state, due to the effects of CS as inhibitors of calcium absorption from the gastrointestinal tract and calcium reabsorption in the renal tubuli, has been postulated, but studies have not reported association between CS and increased parathyroid hormone.Citation145
Other pathophysiological mechanisms are discussed, among these, redirection of differentiation of bone marrow stromal cells from cells of the osteoblastic lineage to the adipocyte lineage,Citation145 and inhibition of osteoblast differentiation by opposing Wnt-β-catenin signaling.Citation154 The relative importance of the various components is not yet known.
CS initially mainly affect trabecular bone due to higher metabolic activity, but with prolonged use cortical bone is also affected.Citation146 Muscle weakness and atrophy is also a consequence of OCS treatment. The changes particularly involve the pelvic girdle musculature, with less involvement of the shoulder girdle and distal musculature. It generally occurs within weeks to months after initiation of OCS. In stable patients with COPD, a 2-week course of 30 mg prednisolone was not associated with muscle weakness.Citation155
Osteoporosis and fractures associated with other medication
Bronchodilators
Overstimulation of the adrenergic system has been associated with a low BMD or increased bone fragility,Citation156 and according to experimental studies, activation of the β2-receptors on osteoblasts leads to production of RANKL resulting in increased osteoclastogenesis and reduced BMD.Citation157 Bonnet et al showed that the β2-agonists salbutamol and clenbuterol reduced bone mineral content and increased the level of bone resorption markers. Opposed to clenbuterol, however, salbutamol did not seem to have any effect on bone microarchitecture or anabolic effect on muscles. Corresponding to these results, a meta-analysis of 7 studies assessing fracture risk in patients using β-blockers concluded that their use was associated with a 28% reduction in hip fracture risk and a 14% reduction in the risk for any fracture.Citation158
Use of convenient doses of β2-agonists probably does not affect bone. In 2 large case-control studies increased risk of fractures associated with β2-agonist treatment was found.Citation159,Citation160 Adjustments for use of OCS and disease severity, substantially reduced the excess risk found in β2-agonist users, and causal effect of the latter seems unlikely as there was no dose dependent relation between use of inhaled short-acting β2-agonists and fractures, in as much oral β2-agonists were associated with an increase in fracture risk at low, but not higher doses.Citation160
A study in rats indicated that theophylline treatment promoted skeletal calcium loss,Citation161 and some effect on bone turnover markers were reported in a study including patients with mild asthma on theophylline treatment.Citation162 However, no increased fracture risk by theophylline was found in a study by Vestergaard et al,Citation160 and for anticholinergics, de Vries et al found similar risk of hip/femur fracture between users of β2-agonists, ICS and anticholinergics,Citation159 indicating these effects to be caused by underlying disease instead of medications. Anticholinergics and theophylline might have beneficial effects on systemic inflammation and comorbidities of COPD, but this is not proven yet.Citation4 Interestingly, low-dose theophylline might also reverse CS resistance in COPD.
Risk estimation
Prior presence of other important risk factors enhances the adverse effects on bone by life style, COPD itself and treatment, and bone densitometry should be considered (). For patients having lost height the possibility of undiagnosed vertebral compression fractures should be considered.
Table 2 Dual energy absorptiometry measurements – recommendations
Thresholds for treatment of osteoporosis previously have been at fixed T-scores given by bone densitometry. Opposed to postmenopausal osteoporosis with a recommended threshold at T-score −2.5 SD for initiating of treatment, the threshold in patients on CS treatment should be higher due to the adverse effect on bone not reflected by bone densitometry. The American College of Rheumatology has set cut off at −1 compared to −1.5 SD in the UK guidelines.Citation163 This is supported by current evidence of CS effect on bone, and encourages more focus on estimation of absolute long-term fracture probability.
Many osteoporosis risk-assessment tools have been developed,Citation164 and WHI Hip Fracture Risk Calculator (www.hipcalculator.fhcrc.org) and the FRAX tool (www.shef.ac.uk/FRAX), for example, could be useful supplements to BMD assessments.Citation164,Citation165 However, the tools are based on cohort studies, and the data might not be representative for all populations. Further, there is limited increase in risk score compared to use of BMD alone. For example, at age 50 the gradient of hip fracture risk per SD change in risk score was 2.0, 3.68 and 4.23 with use of clinical factors, BMD and both, respectively.Citation166
Recommendations for treatment of COPD patients
Health care professionals ought to be well aware of adverse effect on bone from CS therapy, but risk evaluation is performed to a limited extent. In a US study in 2002 of osteoporosis intervention in patients on CS treatment, bone densitometry was performed in 9% of men and 27% of women exposed to OCS and in 4% of men and 23% of women exposed to ICS.Citation168
One important aspect of COPD treatment should be to avoid bone loss and fragility fractures. This involves change in life style, treatment to allow for increased physical activity, keep CS exposure as low as possible, Calcium and vitamin D and anti-resorptive therapy (). An important challenge is to succeed in communication with all COPD patients. Especially, lower socioeconomic classes have high prevalence of COPD, but also less adherence to behavior advice.
Table 3 Recommendations for prevention and treatment of osteoporosis in COPD patients
Calcium and vitamin D supplementation reduce fracture risk,Citation171 and early start reduced fracture risk by 12% in one study.Citation172 Interestingly, a dose-dependent association between vitamin D levels and pulmonary function has been found, and vitamin D supplement might extend beyond the protective effect on bone, and influence the inflammation in the lungs and interfere with comorbidities of COPD.Citation49
Sex hormone treatment also reduces fracture risk.Citation171 Estrogen preserves bone in post-menopausal women independently of CS use,Citation173 but its use is currently limited due to concern for side effects like cardiovascular disease and breast cancer. Such treatment, however, should be considered in hypogonadal premenopausal women exposed to CS, because of limited experience with bisphosphonates beyond 10 to 12 years.Citation164,Citation174
Anti-resorptive therapy should be considered early during OCS treatment, as increased bone loss starts immediately after the beginning of treatment in a daily dose relationship.Citation175 Bisphosphonates have been reported to be the most effective of evaluated agents for managing CS-induced osteoporosis, and this effect is enhanced further with concomitant use of vitamin D and calcium.Citation176 There is strong evidence of reduced fracture risk for most of the bisphosphonates, including the intra-venous alternative zoledronic acid.Citation171 The main effect of bisphosphonates is the inhibition of bone resorption, but they have also been shown to prevent osteoblast and osteocyte apoptosis,Citation177 and could thereby preserve the integrity of the osteocyte network and the osteoblast lifetime.
The American College of Rheumatology recommends bisphosphonates in all men and postmenopausal women in whom long-term (>3 months) CS treatment with daily dose ≥5 mg is initiated, and if T-scores at the spine or hip are below −1 SD independent of OCS dose.Citation174 The UK guidelines suggest this treatment in patients with high risk for osteoporosis; users of ≥7.5 mg OCS, previous experience of a fragility fracture or other risk factors for osteoporosis. Among patients with low risk of osteoporosis, anti-resorptive treatment should be considered if T-score < −1.5 SD or decline in vertebral BMD ≥ 4% after 1 year of CS treatment,Citation163 Vestergaard et al recommended fracture prevention independent of BMD status in patients reaching a yearly cumulative dose of about 800 to 900 mg prednisolone.Citation83 This equals 2 courses of prednisolone or a daily dose of 2.5 mg prednisolone for 1 year.
Anabolic drugs like the parathyroid hormone analogue teriparatide stimulate bone formation through effects on osteoblasts and osteocytes, and may therefore more directly target the main pathophysiological mechanism in CS induced osteoporosis. Teriparatide has been found to be superior to alendronate in CS-induced osteoporosis, both regarding change in BMD and morphometric vertebral fractures,Citation178,Citation179 but there is so far weak evidence for hip fracture reduction.Citation171 In postmenopausal women with osteoporosis, strontium ranelate also has been found to reduce fracture risk.Citation180 The treatment has combined anabolic and anti-catabolic effect, in addition to effect on BMD due to incorporation of strontium into hydroxyapatite instead of calcium. This strengthens the correlation between increase in BMD and reduction in fracture risk, compared to other osteoporosis therapies, and might thereby increase the value of follow-up BMD as a marker of therapeutic efficacy. However, studies of the effect of strontium ranelate in CS-induced osteoporosis have not been published.Citation180
Conclusions
Among available treatments for COPD, only CS-treatment has documented adverse effects of clinical significance. CS have both direct adverse effects on bone and indirect effects due to muscle weakening and atrophy. These effects are dose dependent both regarding daily dose, duration and cumulative dose. Less negative effects are seen by sporadic compared to continuous use, but lower continuous doses have less detrimental effects on bone than frequent high-dose course of OCS. High doses of ICS seem to increase bone loss, but the extent of this effect is discussed because it is difficult to differentiate between the effect of ICS dose used, other risk factors, prior or concomitant use of OCS and not at least, disease severity. The health care should increase focus on healthy lifestyle and use of limited CS doses, as well as be aware of potential osteoporosis development in this group of patients. Studies on the effectiveness of use of long-acting anticholinergics or use of combinations with moderate ICS doses in severe COPD are warranted, as well as development of new anti-inflammatory drugs with specific effects on COPD inflammation and minor adverse effect on bone.
Disclosures
Dr Arnulf Langhammer is the project leader of the Lung Study in the Nord-Trøndelag Health Study (HUNT). The Lung Study was partly funded through a non-demanding grant from AstraZeneca Norway in 1995–97 (HUNT 2) and 2006–08 (HUNT 3). AstraZenca is the producer of the ICS budesonide and the long-acting β2-agonist formoterol. He has also received salaries as a speaker and member of advisory boards for many different pharmaceutical companies. Additionally, in his work as general practitioner, he has participated in many multi-center studies for pharmaceutical companies. In medical practice he is joint-owner of a DXA bone densitometer.
Dr Siri Forsmo declares no conflicts of interest.
Dr Unni Syversen has received salaries as a speaker and member of several advisory boards for different pharmaceutical companies and has also participated in multicenter trials for several pharmaceutical companies.
References
- RabeKFHurdSAnzuetoAGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med2007176653255517507545
- SorianoJBVisickGTMuellerovaHPayvandiNHansellALPatterns of comorbidities in newly diagnosed COPD and asthma in primary careChest200512842099210716236861
- DecramerMRennardSTroostersTCOPD as a lung disease with systemic consequences – clinical impact, mechanisms, and potential for early interventionCOPD20085423525618671149
- BarnesPJCelliBRSystemic manifestations and comorbidities of COPDEur Respir J20093351165118519407051
- SchlaichCMinneHWBrucknerTReduced pulmonary function in patients with spinal osteoporotic fracturesOsteoporos Int1998832612679797911
- PapaioannouAParkinsonWFerkoNPrevalence of vertebral fractures among patients with chronic obstructive pulmonary disease in CanadaOsteoporos Int2003141191391714551675
- PuhanMABachmannLMKleijnenJterRGKesselsAGInhaled drugs to reduce exacerbations in patients with chronic obstructive pulmonary disease: a network meta-analysisBMC Med20097219144173
- CummingsSRMeltonLJEpidemiology and outcomes of osteoporotic fracturesLancet200235993191761176712049882
- MatkovicVJelicTWardlawGMTiming of peak bone mass in Caucasian females and its implication for the prevention of osteoporosis. Inference from a cross-sectional modelJ Clin Invest19949327998088113412
- BergerCLangsetmoLJosephLChange in bone mineral density as a function of age in women and men and association with the use of antiresorptive agentsCMAJ2008178131660166818559803
- RiggsBLMeltonLJRobbRAA population-based assessment of rates of bone loss at multiple skeletal sites: evidence for substantial trabecular bone loss in young adult women and menJ Bone Miner Res200823220521417937534
- HolroydCCooperCDennisonEEpidemiology of osteoporosisBest Pract Res Clin Endocrinol Metab200822567168519028351
- Dawson-HughesBTostesonANMeltonLJIIIImplications of absolute fracture risk assessment for osteoporosis practice guidelines in the USAOsteoporos Int200819444945818292975
- NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and TherapyJAMA20012856785795
- Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study GroupWorld Health Organ Tech Rep Ser199484311297941614
- CummingsSRBatesDBlackDMClinical use of bone densitometry: scientific reviewJAMA2002288151889189712377088
- SteigerPCummingsSRBlackDMSpencerNEGenantHKAge-related decrements in bone mineral density in women over 65J Bone Miner Res1992766256321414480
- SirisESChenYTAbbottTABone mineral density thresholds for pharmacological intervention to prevent fracturesArch Intern Med2004164101108111215159268
- BergerCLangsetmoLJosephLAssociation Between Change in Bone Mineral Density (BMD) and Fragility Fracture in Women and MenJ Bone Miner Res2008
- KanisJADiagnosis of osteoporosis and assessment of fracture riskLancet200235993211929193612057569
- KanisJAGluerCCAn update on the diagnosis and assessment of osteoporosis with densitometry. Committee of Scientific Advisors, International Osteoporosis FoundationOsteoporos Int200011319220210824234
- OrimoHSugiokaYFukunagaMThe Committee of the Japanese Society for Bone and Mineral Research for Development of Diagnostic criteria of Osteoporosis: Diagnostic criteria of primary osteoporosisJ Bone Miner Metab199816139150
- CummingsSRBlackDMNevittMCBone density at various sites for prediction of hip fractures. The Study of Osteoporotic Fractures Research GroupLancet1993341883772758093403
- MarshallDJohnellOWedelHMeta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fracturesBMJ1996183127041125412598634613
- BlackDMCummingsSRGenantHKNevittMCPalermoLBrownerWAxial and appendicular bone density predict fractures in older womenJ Bone Miner Res1992766336381414481
- WasnichRBone mass measurement: prediction of riskAm J Med1993955A6S10S8256798
- GluerCCQuantitative ultrasound techniques for the assessment of osteoporosis: expert agreement on current status. The International Quantitative Ultrasound Consensus GroupJ Bone Miner Res1997128128012089258759
- HansDrgent-MolinaPSchottAMUltrasonographic heel measurements to predict hip fracture in elderly women: the EPIDOS prospective studyLancet199634890265115148757153
- VriezeAde GreefMHWijkstraPJWempeJBLow bone mineral density in COPD patients related to worse lung function, low weight and decreased fat-free massOsteoporos Int20071891197120217347789
- NayakSOlkinILiuHMeta-analysis: accuracy of quantitative ultrasound for identifying patients with osteoporosisAnn Intern Med20061441183284116754925
- JonesAFayJKBurrMStoneMHoodKRobertsGInhaled corticosteroid effects on bone metabolism in asthma and mild chronic obstructive pulmonary diseaseCochrane Database Syst Rev20021CD00353711869676
- BarnesPJPedersenSBusseWWEfficacy and safety of inhaled corticosteroids. New developmentsAm J Respir Crit Care Med19981573 Pt 2S1S539520807
- ScanlonPDConnettJEWiseRALoss of bone density with inhaled triamcinolone in Lung Health Study IIAm J Respir Crit Care Med2004170121302130915374846
- CivitelliRRmamento-VillarealRNapoliNBone turnover markers: understanding their value in clinical trials and clinical practiceOsteoporos Int200920684385119190842
- JohnellOPauwelsRLofdahlCGBone mineral density in patients with chronic obstructive pulmonary disease treated with budesonide TurbuhalerEur Respir J20021961058106312108857
- CalverleyPMAndersonJACelliBSalmeterol and fluticasone propionate and survival in chronic obstructive pulmonary diseaseN Engl J Med2007356877578917314337
- SosaMJodarESaavedraPPostmenopausal Canarian women receiving oral glucocorticoids have an increased prevalence of vertebral fractures and low values of bone mineral density measured by quantitative computer tomography and dual X-ray absorptiometry, without significant changes in parathyroid hormoneEur J Intern Med2008191515618206602
- MinisolaSDelFRPiemonteSBiochemical markers in glucocorticoid-induced osteoporosisJ Endocrinol Invest2008317 Suppl283218791348
- LofthusCMOsnesEKFalchJAEpidemiology of hip fractures in Oslo, NorwayBone200129541341811704490
- CauleyJALuiLYEnsrudKEBone mineral density and the risk of incident nonspinal fractures in black and white womenJAMA2005293172102210815870413
- ChiuGRAraujoABTravisonTGHallSAMcKinlayJBRelative contributions of multiple determinants to bone mineral density in menOsteoporos Int2009325 [Epub ahead of print]
- LindsayRSilvermanSLCooperCRisk of new vertebral fracture in the year following a fractureJAMA2001285332032311176842
- PapaioannouAKennedyCCCranneyARisk factors for low BMD in healthy men age 50 years or older: a systematic reviewOsteoporos Int200920450751818758880
- YanbaevaDGDentenerMACreutzbergECWesselingGWoutersEFSystemic effects of smokingChest200713151557156617494805
- LanghammerAJohnsenRGulsvikAHolmenTLBjermerLSex differences in lung vulnerability to tobacco smokingEur Respir J20032161017102312797498
- Ben-ZakenCSParePDManSFSinDDThe growing burden of chronic obstructive pulmonary disease and lung cancer in women: examining sex differences in cigarette smoke metabolismAm J Respir Crit Care Med2007176211312017413125
- RutherfordOMIs there a role for exercise in the prevention of osteoporotic fractures?Br J Sports Med199933637838610597845
- FrancoCBPaz-FilhoGGomesPEChronic obstructive pulmonary disease is associated with osteoporosis and low levels of vitamin DOsteoporos Int2009320 [Epub ahead of print]
- JanssensWLehouckACarremansCBouillonRMathieuCDecramerMVitamin D Beyond Bones in COPD: Time to ActAm J Respir Crit Care Med2009179863063619164701
- HannanMTFelsonDTwson-HughesBRisk factors for longitudinal bone loss in elderly men and women: the Framingham Osteoporosis StudyJ Bone Miner Res200015471072010780863
- ZhaiGHartDJValdesAMNatural history and risk factors for bone loss in postmenopausal Caucasian women: a 15-year follow-up population-based studyOsteoporos Int20081981211121718305885
- ForsmoSLanghammerAScheiBPast and current weight change and forearm bone loss in middle-aged women: the Nord-Trondelag Health Study, NorwayMenopause2009515 [Epub ahead of print]
- OmslandTKScheiBGronskagABWeight loss and distal forearm fractures in postmenopausal women: The Nord-Trondelag health study, NorwayOsteoporos Int200937 [Epub ahead of print]
- AgustiASorianoJBCOPD as a systemic diseaseCOPD20085213313818415812
- van StaaTPGeusensPPolsHAdeLCLeufkensHGCooperCA simple score for estimating the long-term risk of fracture in patients using oral glucocorticoidsQJM200598319119815728400
- de VriesFBrackeMLeufkensHGLammersJWCooperCvan StaaTPFracture risk with intermittent high-dose oral glucocorticoid therapyArthritis Rheum200756120821417195223
- van StaaTPLeufkensHGAbenhaimLZhangBCooperCUse of oral corticosteroids and risk of fracturesJ Bone Miner Res2000156993100010841167
- VestergaardPRejnmarkLMosekildeLFracture risk associated with systemic and topical corticosteroidsJ Intern Med2005257437438415788008
- SeemanEOsteoporosis: trials and tribulationsAm J Med19971032 A74S87S9302899
- WisniewskiAFLewisSAGreenDJMaslankaWBurrellHTattersfieldAECross sectional investigation of the effects of inhaled corticosteroids on bone density and bone metabolism in patients with asthmaThorax199752108538609404371
- SinDDManJPManSFThe risk of osteoporosis in Caucasian men and women with obstructive airways diseaseAm J Med20031141101412543283
- LekamwasamSTrivediDPKhawKTAn association between respiratory function and hip bone mineral density in older men: a cross-sectional studyOsteoporos Int200516220420715197543
- EastellRTreatment of postmenopausal osteoporosisN Engl J Med1998338117367469494151
- BiskobingDMCOPD and osteoporosisChest2002121260962011834678
- OharaTHiraiTMuroSRelationship between pulmonary emphysema and osteoporosis assessed by CT in patients with COPDChest200813461244124918641115
- de VriesFvan StaaTPBrackeMSCooperCLeufkensHGLammersJWSeverity of obstructive airway disease and risk of osteoporotic fractureEur Respir J200525587988415863646
- BoltonCEIonescuAAShielsKMAssociated loss of fat-free mass and bone mineral density in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2004170121286129315374843
- KatsuraHKidaKA comparison of bone mineral density in elderly female patients with COPD and bronchial asthmaChest200212261949195512475832
- KjensliAMowinckelPRygMSFalchJALow bone mineral density is related to severity of chronic obstructive pulmonary diseaseBone200740249349717049326
- LiLBrennanKJGaughanJPCiccolellaDEKuzmaAMCrinerGJAfrican Americans and men with severe COPD have a high prevalence of osteoporosisCOPD20085529129718972277
- NutiRSivieroPMaggiSVertebral fractures in patients with chronic obstructive pulmonary disease: the EOLO StudyOsteoporos Int200920698999818931817
- O’NeillTWFelsenbergDVarlowJCooperCKanisJASilmanAJThe prevalence of vertebral deformity in european men and women: the European Vertebral Osteoporosis StudyJ Bone Miner Res1996117101010188797123
- PauwelsRALofdahlCGLaitinenLALong-term treatment with inhaled budesonide in persons with mild chronic obstructive pulmonary disease who continue smoking. European Respiratory Society Study on Chronic Obstructive Pulmonary DiseaseN Engl J Med1999340251948195310379018
- KjensliAFalchJARygMHigh prevalence of vertebral deformities in COPD patients: relation to disease severityEur Respir J20093351018102419129288
- JorgensenNRSchwarzPHolmeIHenriksenBMPetersenLJBackerVThe prevalence of osteoporosis in patients with chronic obstructive pulmonary disease: a cross sectional studyRespir Med2007101117718516677808
- van StaaTPAbenhaimLCooperCZhangBLeufkensHGPublic health impact of adverse bone effects of oral corticosteroidsBr J Clin Pharmacol200151660160711422020
- WalshLJWongCAOborneJAdverse effects of oral corticosteroids in relation to dose in patients with lung diseaseThorax200156427928411254818
- van StaaTPLeufkensHGCooperCThe epidemiology of corticosteroid-induced osteoporosis: a meta-analysisOsteoporos Int2002131077778712378366
- van StaaTPThe pathogenesis, epidemiology and management of glucocorticoid-induced osteoporosisCalcif Tissue Int200679312913716969593
- AngeliAGuglielmiGDovioAHigh prevalence of asymptomatic vertebral fractures in post-menopausal women receiving chronic glucocorticoid therapy: a cross-sectional outpatient studyBone200639225325916574519
- LaneNELukertBThe science and therapy of glucocorticoid-induced bone lossEndocrinol Metab Clin North Am19982724654839669150
- ReidIREvansMCStapletonJLateral spine densitometry is a more sensitive indicator of glucocorticoid-induced bone lossJ Bone Miner Res1992710122112251456089
- VestergaardPRejnmarkLMosekildeLFracture risk associated with different types of oral corticosteroids and effect of termination of corticosteroids on the risk of fracturesCalcif Tissue Int200882424925718414920
- de VriesFPouwelsSLammersJWUse of inhaled and oral glucocorticoids, severity of inflammatory disease and risk of hip/ femur fracture: a population-based case-control studyJ Intern Med2007261217017717241182
- MichelBABlochDAWolfeFFriesJFFractures in rheumatoid arthritis: an evaluation of associated risk factorsJ Rheumatol19932010166616698295176
- Ramsey-GoldmanRDunnJEHuangCFFrequency of fractures in women with systemic lupus erythematosus: comparison with United States population dataArthritis Rheum199942588289010323443
- TonFNGunawardeneSCLeeHNeerRMEffects of low-dose prednisone on bone metabolismJ Bone Miner Res200520346447015746991
- van StaaTPLaanRFBartonIPCohenSReidDMCooperCBone density threshold and other predictors of vertebral fracture in patients receiving oral glucocorticoid therapyArthritis Rheum200348113224322914613287
- SteinbuchMYouketTECohenSOral glucocorticoid use is associated with an increased risk of fractureOsteoporos Int200415432332814762652
- AdachiJDIoannidisGCalcium and vitamin D therapy in corticosteroid-induced bone loss: what is the evidence?Calcif Tissue Int1999654332610485987
- LukertBPRaiszLGGlucocorticoid-induced osteoporosis: pathogenesis and managementAnn Intern Med199011253523642407167
- AdinoffADHollisterJRSteroid-induced fractures and bone loss in patients with asthmaN Engl J Med198330952652686866051
- GluckOSMurphyWAHahnTJHahnBBone loss in adults receiving alternate day glucocorticoid therapy. A comparison with daily therapyArthritis Rheum19812478928987259801
- RuegseggerPMediciTCAnlikerMCorticosteroid-induced bone loss. A longitudinal study of alternate day therapy in patients with bronchial asthma using quantitative computed tomographyEur J Clin Pharmacol19832556156206662161
- DuboisEFRoderEDekhuijzenPNZwindermanAESchweitzerDHDual energy X-ray absorptiometry outcomes in male COPD patients after treatment with different glucocorticoid regimensChest200212151456146312006428
- MatsumotoHIshiharaKHasegawaTUmedaBNiimiAHinoMEffects of inhaled corticosteroid and short courses of oral corticosteroids on bone mineral density in asthmatic patients: a 4-year longitudinal studyChest200112051468147311713121
- ManningPJEvansMCReidIRNormal bone mineral density following cure of Cushing’s syndromeClin Endocrinol (Oxf)19923632292341563076
- LaanRFvan RielPLvan de PutteLBvan ErningLJvan’t HofMALemmensJALow-dose prednisone induces rapid reversible axial bone loss in patients with rheumatoid arthritis. A randomized, controlled studyAnn Intern Med1993119109639688105737
- DalleCLBertoldoFValentiMTHistomorphometric analysis of glucocorticoid-induced osteoporosisMicron20053678645652
- ReidIRGlucocorticoid-induced osteoporosisBaillieres Best Pract Res Clin Endocrinol Metab2000142279219811035907
- WalshLJLewisSAWongCAThe impact of oral corticosteroid use on bone mineral density and vertebral fractureAm J Respir Crit Care Med2002166569169512204867
- KanisJAJohanssonHOdenAA meta-analysis of prior corticosteroid use and fracture riskJ Bone Miner Res200419689389915125788
- McKenzieRReynoldsJCO’FallonADecreased bone mineral density during low dose glucocorticoid administration in a randomized, placebo controlled trialJ Rheumatol20002792222222610990237
- BaptistAPReddyRCInhaled corticosteroids for asthma: are they all the same?J Clin Pharm Ther200934111219125898
- TattersfieldAEHarrisonTWHubbardRBMortimerKSafety of inhaled corticosteroidsProc Am Thorac Soc20041317117516113431
- RossiGACerasoliFCazzolaMSafety of inhaled corticosteroids: room for improvementPulm Pharmacol Ther2007201233516359896
- DrummondMBDasenbrookECPitzMWMurphyDJFanEInhaled corticosteroids in patients with stable chronic obstructive pulmonary disease: a systematic review and meta-analysisJAMA2008300202407241619033591
- BurgePSCalverleyPMJonesPWSpencerSAndersonJAMaslenTKRandomised, double blind, placebo controlled study of fluticasone propionate in patients with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trialBMJ200032072451297130310807619
- LipworthBJSystemic adverse effects of inhaled corticosteroid therapy: A systematic review and meta-analysisArch Intern Med1999159994195510326936
- RichyFBousquetJEhrlichGEInhaled corticosteroids effects on bone in asthmatic and COPD patients: a quantitative systematic reviewOsteoporos Int200314317919012730758
- Lung Health Study Research GroupEffect of inhaled triamcinolone on the decline in pulmonary function in chronic obstructive pulmonary diseaseN Engl J Med2000343261902190911136260
- van StaaTPLeufkensHGCooperCUse of inhaled corticosteroids and risk of fracturesJ Bone Miner Res200116358158811277277
- HubbardRBSmithCJSmeethLHarrisonTWTattersfieldAEInhaled corticosteroids and hip fracture: a population-based case-control studyAm J Respir Crit Care Med200216612 Pt 11563156612406825
- HubbardRTattersfieldASmithCWestJSmeethLFletcherAUse of inhaled corticosteroids and the risk of fractureChest200613041082108817035441
- Pujades-RodriguezMSmithCJHubbardRBInhaled corticosteroids and the risk of fracture in chronic obstructive pulmonary diseaseQJM2007100850951717609226
- LanghammerANorjavaaraEde VerdierMGJohnsenRBjermerLUse of inhaled corticosteroids and bone mineral density in a population based study: the Nord-Trondelag Health Study (the HUNT Study)Pharmacoepidemiol Drug Saf200413856957915317039
- LanghammerAForsmoSLilleengSJohnsenRBjermerLEffect of inhaled corticosteroids on forearm bone mineral density: the HUNT study, NorwayRespir Med200710181744175217433653
- WeatherallMJamesKClayJDose-response relationship for risk of non-vertebral fracture with inhaled corticosteroidsClin Exp Allergy20083891451145818537983
- MasoliMWeatherallMHoltSBeasleyRClinical dose-response relationship of fluticasone propionate in adults with asthmaThorax2004591162014694240
- MasoliMHoltSWeatherallMBeasleyRDose-response relationship of inhaled budesonide in adult asthma: a meta-analysisEur Respir J200423455255815083753
- BarnesPJImmunology of asthma and chronic obstructive pulmonary diseaseNat Rev Immunol20088318319218274560
- AdenugaDYaoHMarchTHSeagraveJRahmanIHistone deacetylase 2 is phosphorylated, ubiquitinated, and degraded by cigarette smokeAm J Respir Cell Mol Biol200940446447318927347
- BatemanEDHurdSSBarnesPJGlobal strategy for asthma management and prevention: GINA executive summaryEur Respir J200831114317818166595
- PasaogluGGokHMunganDSonelBYalcinPMisirligilZDoes the combination of inhaled steroids with long acting beta2 agonists decrease the risk for osteoporosis? A 1-year prospective follow-up studyRheumatol Int200627214114616932963
- AaronSDVandemheenKLFergussonDTiotropium in combination with placebo, salmeterol, or fluticasone-salmeterol for treatment of chronic obstructive pulmonary disease: a randomized trialAnn Intern Med2007146854555517310045
- KardosPWenckerMGlaabTVogelmeierCImpact of salmeterol/ fluticasone propionate versus salmeterol on exacerbations in severe chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2007175214414917053207
- WedzichaJACalverleyPMSeemungalTAHaganGAnsariZStockleyRAThe prevention of chronic obstructive pulmonary disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromideAm J Respir Crit Care Med20081771192617916806
- ZhengJPYangLWuYMThe efficacy and safety of combination salmeterol (50 microg)/fluticasone propionate (500 microg) inhalation twice daily via accuhaler in Chinese patients with COPDChest200713261756176317951625
- CalverleyPMBoonsawatWCsekeZZhongNPetersonSOlssonHMaintenance therapy with budesonide and formoterol in chronic obstructive pulmonary diseaseEur Respir J200322691291914680078
- SzafranskiWCukierARamirezAEfficacy and safety of budesonide/formoterol in the management of chronic obstructive pulmonary diseaseEur Respir J2003211748112570112
- VestboJSorensenTLangePBrixATorrePViskumKLong-term effect of inhaled budesonide in mild and moderate chronic obstructive pulmonary disease: a randomised controlled trialLancet199935391671819182310359405
- FergusonGTAnzuetoAFeiREmmettAKnobilKKalbergCEffect of fluticasone propionate/salmeterol (250/50 microg) or salmeterol (50 microg) on COPD exacerbationsRespir Med200810281099110818614347
- MahlerDAWirePHorstmanDEffectiveness of fluticasone propionate and salmeterol combination delivered via the Diskus device in the treatment of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med200216681084109112379552
- HananiaNADarkenPHorstmanDThe efficacy and safety of fluticasone propionate (250 microg)/salmeterol (50 microg) combined in the Diskus inhaler for the treatment of COPDChest2003124383484312970006
- StallbergBSelroosOVogelmeierCAnderssonEEkstromTLarssonKBudesonide/formoterol as effective as prednisolone plus formoterol in acute exacerbations of COPD. A double-blind, randomised, non-inferiority, parallel-group, multicentre studyRespir Res2009101119228428
- ManolagasSCJilkaRLBone marrow, cytokines, and bone remodeling. Emerging insights into the pathophysiology of osteoporosisN Engl J Med199533253053117816067
- ThornberryNALazebnikYCaspases: enemies withinScience19982815381131213169721091
- HofbauerLCKhoslaSDunstanCRLaceyDLBoyleWJRiggsBLThe roles of osteoprotegerin and osteoprotegerin ligand in the paracrine regulation of bone resorptionJ Bone Miner Res200015121210646108
- HofbauerLCGoriFRiggsBLStimulation of osteoprotegerin ligand and inhibition of osteoprotegerin production by glucocorticoids in human osteoblastic lineage cells: potential paracrine mechanisms of glucocorticoid-induced osteoporosisEndocrinology1999140104382438910499489
- HardyRCooperMSBone loss in inflammatory disordersJ Endocrinol2009201330932019443863
- LorenzoJHorowitzMChoiYOsteoimmunology: interactions of the bone and immune systemEndocr Rev200829440344018451259
- GilbertLHeXFarmerPInhibition of osteoblast differentiation by tumor necrosis factor-alphaEndocrinology2000141113956396411089525
- CooperMSSensitivity of bone to glucocorticoidsClin Sci (Lond)2004107211112315113280
- LovasKGjesdalCGChristensenMGlucocorticoid replacement therapy and pharmacogenetics in Addison’s disease: effects on boneEur J Endocrinol20091606993100219282465
- CanalisEMechanisms of glucocorticoid action in boneCurr Osteoporos Rep2005339810216131429
- YaoWChengZBusseCPhamANakamuraMCLaneNEGlucocorticoid excess in mice results in early activation of osteoclastogenesis and adipogenesis and prolonged suppression of osteogenesis: a longitudinal study of gene expression in bone tissue from glucocorticoid-treated miceArthritis Rheum20085861674168618512788
- WeinsteinRSChenJRPowersCCPromotion of osteoclast survival and antagonism of bisphosphonate-induced osteoclast apoptosis by glucocorticoidsJ Clin Invest200210981041104811956241
- EijkenMKoedamMvanDMBuurmanCJPolsHAvan LeeuwenJPThe essential role of glucocorticoids for proper human osteoblast differentiation and matrix mineralizationMol Cell Endocrinol200624812879316413958
- CanalisEMazziottiGGiustinaABilezikianJPGlucocorticoid-induced osteoporosis: pathophysiology and therapyOsteoporos Int200718101319132817566815
- LaneNEYaoWBaloochMGlucocorticoid-treated mice have localized changes in trabecular bone material properties and osteocyte lacunar size that are not observed in placebo-treated or estrogen-deficient miceJ Bone Miner Res200621346647616491295
- O’BrienCAJiaDPlotkinLIGlucocorticoids act directly on osteoblasts and osteocytes to induce their apoptosis and reduce bone formation and strengthEndocrinology200414541835184114691012
- EastellRRole of oestrogen in the regulation of bone turnover at the menarcheJ Endocrinol2005185222323415845915
- MillerKKLeeEELawsonEADeterminants of skeletal loss and recovery in anorexia nervosaJ Clin Endocrinol Metab20069182931293716735492
- OhnakaKTanabeMKawateHNawataHTakayanagiRGlucocorticoid suppresses the canonical Wnt signal in cultured human osteoblastsBiochem Biophys Res Commun2005329117718115721290
- HopkinsonNSManWDDayerMJAcute effect of oral steroids on muscle function in chronic obstructive pulmonary diseaseEur Respir J200424113714215293616
- BonnetNPierrozDDFerrariSLAdrenergic control of bone remodeling and its implications for the treatment of osteoporosisJ Musculoskelet Neuronal Interact2008829410418622078
- BonnetNBenhamouCLBrunet-ImbaultBSevere bone alterations under beta2 agonist treatments: bone mass, microarchitecture and strength analyses in female ratsBone200537562263316157516
- WiensMEtminanMGillSSTakkoucheBEffects of antihypertensive drug treatments on fracture outcomes: a meta-analysis of observational studiesJ Intern Med2006260435036216961672
- deVFPouwelsSBrackeMUse of beta-2 agonists and risk of hip/femur fracture: a population-based case-control studyPharmacoepidemiol Drug Saf200716661261916998945
- VestergaardPRejnmarkLMosekildeLFracture risk in patients with chronic lung diseases treated with bronchodilator drugs and inhaled and oral corticosteroidsChest200713251599160717890464
- FortenberyEJMcDermottMTDuncanWEEffect of theophylline on calcium metabolism and circulating vitamin D metabolitesJ Bone Miner Res1990543213242343772
- OnerPGurdolFOner-IyidonYKolanciCBuyukozturkSEvaluation of the effect of low-dose oral theophylline therapy on some bone turnover markers and serum prolidase I activity in mild asthmaticsPharmacol Res199940218919310433880
- CompstonJUS and UK guidelines for glucocorticoid-induced osteoporosis: similarities and differencesCurr Rheumatol Rep200461666914713404
- LimLSHoeksemaLJSherinKScreening for osteoporosis in the adult U.S. population: ACPM position statement on preventive practiceAm J Prev Med200936436637519285200
- KanisJAJohnellOOdenAJohanssonHMcCloskeyEFRAX and the assessment of fracture probability in men and women from the UKOsteoporos Int200819438539718292978
- KanisJAOdenAJohnellOThe use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and womenOsteoporos Int20071881033104617323110
- ShakerJLLukertBPOsteoporosis associated with excess glucocorticoidsEndocrinol Metab Clin North Am2005342341–ix15850846
- CheMEttingerBNguyenMTPressmanARJohnstonJHigh-dose corticosteroid exposure and osteoporosis intervention in adultsAnn Allergy Asthma Immunol200697449750117069105
- LacasseYBrosseauLMilneSPulmonary rehabilitation for chronic obstructive pulmonary diseaseCochrane Database Syst Rev20023CD00379312137716
- CooperCBThe connection between chronic obstructive pulmonary disease symptoms and hyperinflation and its impact on exercise and functionAm J Med200611910 Suppl 1213116996896
- QaseemASnowVShekellePHopkinsRJrForcieaMAOwensDKPharmacologic treatment of low bone density or osteoporosis to prevent fractures: a clinical practice guideline from the American College of PhysiciansAnn Intern Med2008149640441518794560
- TangBMEslickGDNowsonCSmithCBensoussanAUse of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: a meta-analysisLancet2007370958865766617720017
- GuGHentunenTANarsMHarkonenPLVaananenHKEstrogen protects primary osteocytes against glucocorticoid-induced apoptosisApoptosis200510358359515909120
- Recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis: 2001 update. American College of Rheumatology Ad Hoc Committee on Glucocorticoid-Induced OsteoporosisArthritis Rheum20014471496150311465699
- van StaaTPLeufkensHGAbenhaimLZhangBCooperCOral corticosteroids and fracture risk: relationship to daily and cumulative dosesRheumatology (Oxford)200039121383138911136882
- AminSLavalleyMPSimmsRWFelsonDTThe comparative efficacy of drug therapies used for the management of corticosteroid-induced osteoporosis: a meta-regressionJ Bone Miner Res20021781512152612162505
- PlotkinLIAguirreJIKousteniSManolagasSCBellidoTBisphosphonates and estrogens inhibit osteocyte apoptosis via distinct molecular mechanisms downstream of extracellular signal-regulated kinase activationJ Biol Chem200528087317732515590626
- SaagKGShaneEBoonenSTeriparatide or alendronate in glucocorticoid-induced osteoporosisN Engl J Med2007357202028203918003959
- LangdahlBLMarinFShaneETeriparatide versus alendronate for treating glucocorticoid-induced osteoporosis: an analysis by gender and menopausal statusOsteoporos Int200947 [Epub ahead of print]
- O’DonnellSCranneyAWellsGAAdachiJDReginsterJYStrontium ranelate for preventing and treating postmenopausal osteoporosisCochrane Database Syst Rev20064CD005326
