Abstract
Excessive sleepiness (ES) is a widespread condition, commonly the result of a sleep/ wake disorder such as obstructive sleep apnea (OSA), shift-work disorder (SWD), or narcolepsy. ES poses significant health and safety concerns in patients. Numerous interventions are available to treat the underlying causes of ES and ES itself, including behavioral measures, mechanical devices, and pharmacologic agents. This review explores the evidence supporting the use of armodafinil to treat ES associated with OSA, SWD, and narcolepsy. Armodafinil is an oral non-amphetamine wake-promoting agent, the R-isomer of racemic modafinil. Armodafinil and modafinil share many clinical and pharmacologic properties and are distinct from central nervous system stimulants; however, the mechanisms of action of modafinil and armodafinil are poorly characterized. Compared with modafinil, the wake-promoting effects of armodafinil persist later in the day. It is for this reason that armodafinil may be a particularly appropriate therapy for patients with persistent ES due to OSA, SWD, or narcolepsy.
Introduction
Excessive sleepiness (ES) is common and may occur as a consequence of a number of sleep/wake disorders including obstructive sleep apnea (OSA), shift-work disorder (SWD), narcolepsy, and jet lag. Although the full extent of its prevalence has not been established, ES is known to be widespread, in part because of the large number of people who are required to perform shift work, work for prolonged periods, or regularly participate in transmeridian fight.Citation1 Findings from the National Sleep Foundation’s 2008 Sleep in America PollCitation2 point to a large proportion of working Americans being affected by a lack of sleep, with 15% of the 1000 respondents having been diagnosed with a sleep/wake disorder. This poll also revealed that 29% of respondents had slept or been drowsy at work in the past month and that 36% had fallen asleep while driving in the past year.Citation2
ES may also arise because of insufficient night-time sleep due to behavioral issues (eg, self-imposed sleep deprivation or poor sleep hygiene), psychiatric conditions, medication, or medical conditions other than sleep/wake disorders.Citation3 Sleep hygiene refers to elements intended to create a mental and environmental state conducive to sleep, eg, a regular sleep/wake pattern, avoidance of stimulants such as caffeine and nicotine close to bedtime, and having a quiet, peaceful place to sleep.Citation4,Citation5 The co-existence of psychiatric disorders and ES is common.Citation6 For example, depression often interferes with sleep behavior and thus the quality of sleep. The side effects of a wide variety of medications, such as benzodiazepines and antihistamines, can cause ES.Citation3 A number of medical conditions can affect the duration and quality of sleep, such as those that interfere with breathing (eg, nasal congestion and chronic obstructive pulmonary disease), Parkinson’s disease, movement disorders, and chronic pain syndromes.Citation7 Both quality and quantity of sleep are important factors in ensuring that an individual feels rested and alert and poor sleep quality in particular has been found to be related to the development of ES.Citation8
This review will discuss the prevalence and management of ES before moving on to its main focus – the use of the wake-promoting agent armodafinil in the treatment of ES. Armodafinil has been approved in the United States for the treatment of patients with ES associated with treated OSA, SWD, and narcolepsy.
Consequences of ES
ES affects not only patients’ health but also their ability to work and drive safely and the extent to which they can function and enjoy day-to-day living.
Clinical consequences
ES is associated with increased rates of cardiovascular mortality, myocardial infarction, and congestive heart failure.Citation9 Moreover, patients with OSA and associated ES are at a higher risk of developing ischemic heart disease than patients who have OSA in isolation.Citation10 Patients with ES are also more likely to develop diabetes than those without ES and, on average, have a higher body mass index; both diabetes and high BMI are characteristics of metabolic syndrome.Citation11 The relationship between OSA, ES, and metabolic syndrome is complex; however, it is thought that these individual factors interact and exacerbate each other, putting the patient at greater risk for further complications.Citation11
ES can lead to significant cognitive sequelae, affecting both attention and memory.Citation12 Patients with ES associated with OSA or shift work are particularly susceptible to reductions in cognitive functioning.Citation13 Depression and ES have a complex and reciprocal relationship: sleep disruption associated with depression can lead patients to experience ES, while mental, social, and work issues caused by persistent ES can also trigger depression.Citation11
Workplace and driving consequences
Individuals with ES associated with OSA are at an increased risk for recent work disability (adjusted odds ratio 13.7; 95% confidence interval [CI], 3.9–48.0) or a work role change due to a lack of coping/poor performance (odds ratio 3.6; 95% CI, 1.1–12.0) compared with individuals without this sleep disorder.Citation14 Moreover, the occurrence of absenteeism is elevated in individuals with ES and is further exacerbated by shift work.Citation15 According to a survey of occupational accidents occurring in the United States in 1988, ES was implicated in 52.5% of all work-related accidents, amounting to an estimated cost of $24.7 billion (based on 1994 calculations; $36.1 billion when adjusted to 2009 values).Citation16
There is substantial evidence that ES contributes to many road traffic crashes, with a survey conducted in the UK revealing that 17% of collisions resulting in injury or death are sleep related.Citation17 This survey also revealed that sleep-related collisions are approximately 50% more likely to result in death or serious injury than other road traffic crashes.Citation17 A review of traffic safety in relation to sleep/wake disorders and ES listed changes in attention and information processing, changes in sensation and perception, “highway hypnosis,” and microsleeping as consequences of ES that led to poor driver performance.Citation18 A combined field and laboratory study by the US Department of Transportation has revealed that many long-haul commercial drivers nap during shiftwork hours and spend a significant part of their time at the wheel in a state of sleep deprivation.Citation19
Quality of life
A recent analysis of 1892 adults with untreated OSA revealed that quality of life (QOL) not only worsened with the severity of the condition, but that it was also at its lowest in those with ES.Citation20 In this study, all domains of the Medical Outcomes Study Short-Form (36-item) Health Survey (SF-36) were significantly negatively affected by ES (P < 0.05).Citation20 ES is also detrimental to QOL in patients with narcolepsy.Citation21,Citation22 In particular, patients with narcolepsy and cataplexy report that ES has a significant negative impact on the role physical subscale of the SF-36.Citation22 Earlier studies have also highlighted the impact of ES on patients’ everyday lives, reporting that patients with sleep-disordered breathing and ES have lower scores on all subscales of the SF-36 when compared with patients who are not excessively sleepy.Citation23–Citation26
Management of ES
ES is an underrecognized and undertreated condition, in part because it may not be perceived as a serious problem and hence is not disclosed by patients.Citation3 Patients may not recognize their ES at all or describe it to their physician as tiredness, fatigue, difficulty concentrating, or a lack of energy.Citation27 In addition, ES can be misdiagnosed as depression owing to shared signs such as a lack of motivation, memory disturbances, and diminished interest in activities of daily living.Citation3 To aid in the recognition of ES and potential causative sleep/wake disorders, physicians can ask questions regarding the patient’s sleep quality, assess alertness using simple subjective measures, such as the Epworth Sleepiness Scale (ESS), or use objective measures of ES, such as the Multiple Sleep Latency Test (MSLT) or Maintenance of Wakefulness Test (MWT).Citation28–Citation30 The ESS is the most widely adopted instrument and is useful for identifying ES in clinical practice, particularly in the primary care setting, and is appropriate for monitoring self-reported responses to management/ treatment approaches.Citation28 The MSLT and MWT are most often used by sleep specialists and measure a patient’s ability to fall asleep or remain awake, respectively.Citation29,Citation30 Additional information that a healthcare professional might seek for the identification of ES includes the following: the number of hours of sleep that the patient gets on most nights; whether the patient snores or holds their breath during sleep; whether the patients wake up feeling refreshed most mornings; whether the patient is sleepy or fatigued during waking hours; and whether the patient works night or rotating shifts.
Strategies for the management of ES should begin with an initial assessment to identify the cause of ES and, where possible, to treat any underlying disorder. In many cases, all that may be required is education regarding proper sleep hygiene, in particular, maintaining a regular schedule of activities.Citation5 However, mechanical interventions and/or medication are often necessary to address conditions such as OSA, SWD, or narcolepsy.
Management of sleep/wake disorders causative of ES
Obstructive sleep apnea
OSA is characterized by intermittent full or partial obstruction of the upper airway during sleep leading to abnormal breathing and repetitive episodes of arousal.Citation31 OSA with associated ES is the most frequently reported sleep-related breathing disorder, with an estimated prevalence in the United States of 4% and 2% in middle-aged men and women, respectively.Citation32 Individuals with OSA complain of unrefreshing sleep, ES during the day, low mood, and an inability to concentrate.Citation33
Continuous positive airway pressure (CPAP) therapy is the gold standard treatment for OSA. The CPAP device ensures that the airway remains open, reducing the arousals from sleep that can occur as a consequence of airway collapse and reduced blood oxygen levels.Citation34 Unfortunately, objective ES (as measured using the MSLT) persists in approximately 50% of patients, even when abnormal respiratory events are optimally treated with ≥6 hours of CPAP per night.Citation35 The wakefulness-promoting agent modafinil is recommended by the American Academy of Sleep Medicine (AASM) for the treatment of residual ES in patients with treated OSA.Citation36 Modafinil and its enantiomer armodafinil are approved by the US Food and Drug Administration (FDA) for this indication, based on the results of several large-scale clinical trials.Citation37–Citation41 As armodafinil is a comparatively new medication, it has not yet been incorporated into AASM guidelines for the treatment of ES associated with treated OSA. Stimulants, such as amphetamines, reverse the daytime somnolence seen in some patients on CPAP therapy; however, these agents carry a potential risk for abuse and cardiovascular sequelae and further evidence is required before they can be recommended in this indication.Citation33,Citation36
Shift-work disorder
The homeostatic drive for sleep intensifies with increasing time since the last rest period and is offset during daylight hours by circadian wake-promoting processes. Shift-work schedules cause misalignment of the sleep/wake pattern so that the homeostatic drive for sleep is no longer counteracted by the body’s endogenous circadian rhythm.Citation31,Citation42 SWD is diagnosed by persistent insomnia when trying to sleep and/or ES when trying to stay awake – these symptoms must coincide with the affected individual’s working shifts.Citation31 Approximately 22 million Americans regularly work night, early morning, or rotating shiftsCitation43 and SWD has become a common – although underrecognized – condition as a result. In a US study, 44.8% of night-shift workers and 35.8% of rotating-shift workers were reported to have SWD (as assessed by an ESS score of ≥10), which suggests that up to 45% of individuals who work shifts may be at risk of developing SWD.Citation15 More recently, a study of United Kingdom North Sea oil rig workers has reported that 23% of shift workers have SWD.Citation44
The treatment of SWD encompasses a number of interventions including nonpharmacologic measures, such as improving sleep hygiene, light therapy, and planned nap times.Citation42 Modafinil and armodafinil are FDA approved for the treatment of ES associated with SWD. These non-stimulant wakefulness-promoting agents significantly increased sleep latencies in randomized controlled trials conducted specifically in patients with SWD.Citation45–Citation47 Other pharmacologic options, including melatonin and hypnotics such as zolpidem (to improve daytime sleep) and stimulants such as methamphetamine (to improve night-time alertness), have had varying degrees of success in promoting sleep or wake in shift workers.Citation1,Citation48 However, studies of these agents in SWD are limited, making it difficult to draw firm conclusions as to their utility in patients with this sleep disorder.Citation42
Narcolepsy
Narcolepsy occurs in <1% of individuals in the United StatesCitation49 and is characterized by ES that varies in intensity throughout the day, such that the affected individual has to take frequent naps.Citation31 Indeed, narcolepsy often results in unanticipated sleep episodes lasting from a few seconds to several minutes during periods of reduced stimulation.Citation3
The intrinsic dysfunction in sleep regulation that causes ES in narcolepsy often requires pharmacotherapy to enhance wakefulness. Methylphenidate and dextroamphetamine are approved in this indication, although these medications have the potential for abuse and their use should therefore be monitored closely.Citation50 Sodium oxybate has been shown to significantly reduce ES and cataplexy in patients with narcolepsy in randomized clinical trials and it is the only FDA-approved medication for the treatment of both of these symptoms.Citation51–Citation54 Modafinil and armodafinil have been shown to address ES in patients with narcolepsy in randomized controlled trialsCitation55–Citation57 and are approved by the FDA for this indication.
Armodafinil
Armodafinil and its use in the three indications described above will be the focus of the remainder of this article.
Pharmacology
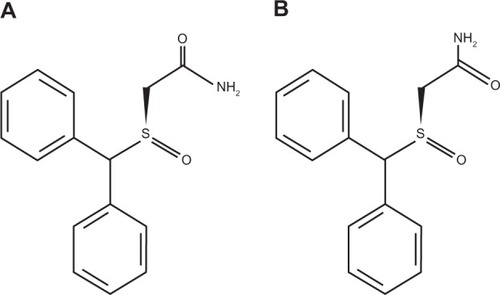
Armodafinil (2-[R-(diphenylmethyl)sulfinyl]acetamide; ) is the R-enantiomer of racemic modafinil and shares many of the properties and characteristics of modafinil. Like modafinil, armodafinil is an orally administered wake-promoting agent that is clinically and pharmacologically distinct from central nervous system stimulants.Citation58,Citation59
Figure 1 Structure of (A) R-modafinil and (B) S-modafinil. Armodafinil comprises only R-modafinil, while racemic modafinil comprises a mixture of both R- and S-modafinil.
Pharmacodynamics
The modes of action of armodafinil and modafinil are currently not fully understood, although it is likely that they involve selective effects on catecholaminergic signaling in the central nervous system via dopaminergic, noradrenergic, and serotonergic receptors.Citation60–Citation62 These effects are not well defined and despite ex-vivo assays showing binding of modafinil to the dopamine transporter and inhibition of dopamine reuptake, modafinil is not a direct or an indirect dopamine receptor agonist.Citation63 Hypocretin (or orexin)-producing neurons within the hypothalamus (postulated as preventing inappropriate changes in consciousness) are believed to be activated by modafinil to release dopamine and norepinephrine to promote wakefulness,Citation64 and this activity may also account for the observed clinical effect of armodafinil.Citation61,Citation62 Furthermore, modafinil may potentiate wakefulness by increasing electrical coupling at gap junctions between neurons.Citation65
Pharmacokinetics
A 200 mg dose of armodafinil, when administered orally, is readily absorbed, with a maximum plasma drug concentration of 5.44 ± 1.64 μg/mL being achieved in approximately 2 hours.Citation66 These values are comparable with those for modafinil (). With once-daily dosing, armodafinil reaches its steady state after approximately 7 days.Citation67 The bioavailability of armodafinil is unaffected by food, although the rate of absorption is delayed by approximately 2–4 hours when armodafinil is taken postprandially.Citation67 Armodafinil is widely distributed outside the vascular system, but it does not have a high affinity for tissues.Citation67 It is unlikely to interact with highly protein-bound drugs, although it does bind with albumin to a moderate degree.Citation63
Table 1 Pharmacokinetic parameters of armodafinil and modafinil
Armodafinil is metabolized by amide hydrolysis followed by sulfone formation via the cytochrome P450 (CYP) 3A4/5 enzyme pathway.Citation63 Dosage adjustment to sustain clinical efficacy may be necessary if patients are receiving concomitant medications that are also metabolized via this pathway (eg, steroidal contraceptives, cyclosporine, midazolam, and triazolam).Citation63 Like modafinil, armodafinil moderately inhibits the activity of CYP2C19, and medications that are metabolized via this enzyme (eg, diazepam) may display prolonged elimination, requiring lower doses of these agents to be administered when given concomitantly with armodafinil.Citation68
Elimination of armodafinil is monophasic with a mean elimination half-life of approximately 15 hours.Citation67 This contrasts with the elimination half-life of the S-enantiomer, which is approximately three- to fourfold shorter than that of armodafinil and is responsible for racemic modafinil’s biphasic elimination profile. As a consequence of their different elimination profiles, armodafinil is present at higher concentrations than modafinil from 4–6 hours after administration.Citation67 Greater systemic availability of armodafinil compared with modafinil on a milligram-by-milligram basis (as indicated by a markedly greater area under the plasma drug concentration–time curve []) may result in improved wakefulness later in the day in individuals with ES.Citation66
Dose reductions of armodafinil should be considered in patients with severe hepatic impairment owing to a reduction in observed oral clearance and an increase in the steady-state concentration of modafinil in this patient group.Citation63 Similarly, dose reductions should be considered in elderly patients in whom elimination may be delayed.
Efficacy of armodafinil
In preclinical studies, a rat model of sleep deprivation was used to explore the efficacy of armodafinil in comparison with the stimulant D-methamphetamine for promoting wakefulness.Citation69 The agents had equivalent wakefulness-promoting effects, as measured by their impact on sleep/wake patterns and body temperature. However, unlike d-methamphetamine, armodafinil did not induce symptoms of sleep deprivation such as acute rebound hypersomnolence.Citation69
To date, the only head-to-head study of armodafinil and modafinil was performed using healthy subjects.Citation70 Based on direct comparison of their pharmacokinetic/pharmacodynamic profiles, the prolonged half-life of armodafinil may be associated with improved wakefulness and sustained attention for a longer time after dosing than modafinil.Citation70 When administered as single doses to sleep-deprived healthy volunteers, both armodafinil and modafinil demonstrated significant wake fulness-promoting effects compared with placebo.Citation70 Using the MWT to measure sustained wakefulness and the Psychomotor Vigilance Task to measure sustained attention (ie, vigilance and reaction time), armodafinil and modafinil had significant positive effects on these parameters (P< 0.0001 for both agents in both tests). However, compared with modafinil, armodafinil treatment resulted in fewer lapses in wakefulness and attention between 6 and 13.5 hours after administration, indicating that armodafinil may have comparatively prolonged effects.Citation70 Armodafinil may therefore represent a useful pharmacologic option for patients with ES associated with OSA, SWD, or narcolepsy who wish to stave off sleepiness for long periods.
Armodafinil for the treatment of ES associated with OSA
Two Phase 3 studies, which together randomized >650 patients with OSA to treatment, have compared the efficacy and safety of armodafinil and placebo ().Citation38,Citation39 The patients enrolled in these studies had residual ES despite use of appropriately titrated CPAP therapy and were randomized to receive armodafinil 150 mg/day or placeboCitation38 or armodafinil 150 or 250 mg/day or placebo.Citation39 The results of these studies have also been reported in a combined analysis.Citation40
Table 2 Wakefulness-promoting effects of armodafinil in the treatment of ES associated with OSA, SWD, and narcolepsy
Armodafinil was associated with a significant increase in mean sleep latency from baseline to the final visit at week 12 as measured using the MWT in all studies. In the study by Roth et al,Citation39 the mean change in sleep latency at the final visit was +1.9 minutes with armodafinil vs −1.7 minutes in patients given placebo (P< 0.001). In the study conducted by Hirshkowitz et al,Citation38 patients receiving armodafinil experienced an increase in sleep latency of +2.3 minutes vs − 1.3 minutes in those given placebo (P< 0.001). The combined analysisCitation40 reported that sleep latency increased by 2.0 minutes in patients administered armodafinil and decreased by 1.5 minutes in patients given placebo (P< 0.0001; ). Nighttime sleep was not adversely affected by armodafinil and patients’ compliance with CPAP therapy was high (a mean of approximately 7 hours/night). In addition, armodafinil had sustained benefits late in the waking day compared with placebo, as demonstrated by higher MWT scores at 15:00, 17:00, and 19:00 hours.Citation40
Improrements in patients’ clinical condition (evaluated using the Clinical Global Impression of Change scale [CGI-C]) were significantly greater in the armodafinil-treated group than in the placebo group (P< 0.001) at all timepoints in the study of patients with OSA performed by Roth et al.Citation39 Similarly in the second OSA study conducted by Hirshkowitz et al,Citation38 the proportion of patients with at least minimal improvement in their clinical condition at the final visit was significantly higher in the armodafinil group compared with the placebo group (P < 0.01).
Cognitive performance was significantly improved with armodafinil compared with placebo in patients with OSA.Citation40 The Cognitive Drug Research battery of tests was used to assess cognitive performance (memory and attention) at six timepoints during the day; the mean (± standard deviation) change from baseline in quality of long-term episodic secondary memory at the final visit was 10.2 (±31.7) units for the armodafinil group compared with −0.7 (±46.3) units for the placebo group (P < 0.01).Citation40
Armodafinil for the treatment of ES in patients with SWD
Armodafinil displayed significant benefits compared with placebo in a 12-week phase 3, randomized, double-blind, multicenter study of 245 patients with SWD ().Citation46 Subjects included in this study were permanent or rotating night-shift workers with SWD who worked $5 nights per month, had a mean sleep latency of ≤6 min (as assessed using the MSLT), and had experienced ES during night shifts for ≥3 months.Citation46
Patients in this study had baseline mean sleep latencies of 2.3 and 2.4 minutes in the armodafinil and placebo groups, respectively; both values indicate severe sleepiness. At the end of the study, patients in the armodafinil group had significantly increased sleep latencies compared with the placebo group (3.1 vs 0.4 minutes, respectively; P < 0.001).Citation46 At the final visit, CGI-Improvement ratings were improved in a significantly greater proportion of patients in the armodafinil group compared with the placebo group (79% vs 59%, respectively; P = 0.001).Citation46 In addition, at the final visit, armodafinil significantly improved the quality of episodic secondary memory and the power and continuity of attention compared with placebo (all P ≤ 0.001).Citation46
Armodafinil for ES in patients with narcolepsy
The efficacy and safety of armodafinil for the treatment of ES in narcolepsy were demonstrated in a phase 3, placebo-controlled study of 194 patients ().Citation55 In this study, patients were randomized to receive armodafinil 150 or 250 mg/day or placebo for 12 weeks.
Daytime (09:00–15:00 hours) sleep tendency assessed using the MWT was found to be significantly improved with armodafinil (+1.9 minutes for both armodafinil groups combined) relative to placebo (−1.9 minutes; P < 0.01). These benefits were sustained late in the waking day (15:00–19:00 hours) as demonstrated by sleep latency improvements from baseline of 1.6 minutes for both armodafinil groups combined, while a reduction of 1.2 minutes was observed in patients in the placebo group (P < 0.05 vs armodafinil).Citation55
At the final visit, the proportion of patients who had at least minimal improvement in their CGI-C ratings was significantly higher in the active-treatment groups compared with placebo (P < 0.0001).Citation55 Armodafinil demonstrated significant improvements compared with placebo in power of attention, quality of episodic secondary memory, and speed of memory (all P < 0.05).Citation55 Improvements were observed at the week 4 visit and were maintained throughout the 12-week study period.
Open-label studies
Two noncomparative open-label studies of armodafinil that focused primarily on patient-reported outcomes have also been completed. These studies enrolled 1071 patients with OSA, SWD, or narcolepsy. One studyCitation71 exclusively enrolled patients who had taken part in any of the aforementioned placebo-controlled, double-blind studies, while the other was also open to subjects who had not participated in the earlier trials.Citation72 Patients’ overall clinical condition was significantly improved with armodafinil compared with baseline values.Citation71,Citation72 At the final visit, between 75% and 98% of patients with OSA, narcolepsy, or SWD were deemed to have at least a minimal clinical improvement according to CGI-C ratings.Citation71,Citation72 Furthermore, 66% of armodafinil-treated patients with ES associated with OSA or narcolepsy perceived their clinical condition as “very much improved” or “much improved.”Citation73
Impact of armodafinil on patient-focused outcomes
As ES associated with sleep/wake disorders has such a serious impact on patients’ daily lives, it is important to assess armodafinil’s treatment effects from the patient’s perspective. Armodafinil has been studied with regard to a number of patient-focused aspects.
Subjective sleepiness
In clinical studies of armodafinil, ES has been measured subjectively using either the ESS or the Karolinska Sleepiness Scale (KSS). ESS scores in patients with treated OSA and residual ES showed that almost half (49%) of patients in the armodafinil group responded to treatment compared with one-quarter (26%) of patients in the placebo group.Citation40 Use of the ESS also enabled investigators to establish that patients with ES associated with OSA treated with armodafinil experienced improvements in their ability to engage in activities of daily living at all study visits (P < 0.0001).Citation40 Furthermore, armodafinil significantly improved ESS scores compared with placebo in patients with OSA (P < 0.01).Citation74
Armodafinil was effective in reducing subjective ES in patients with narcolepsy.Citation55 At the final visit, 21%, 25%, and 7% of patients with narcolepsy who were given armodafinil 150 mg, armodafinil 250 mg, or placebo, respectively, had an ESS score indicative of normal alertness (P < 0.05).Citation55
The KSS is particularly useful for assessing the intrusion of sleep into states of wakefulness.Citation75 Using the KSS, patients with SWD treated with armodafinil reported a significant reduction in ES at week 12 compared with those given placebo (P ≤ 0.01).Citation46
Data derived from electronic diaries completed by patients with SWD revealed that armodafinil significantly reduced maximum ES during the night shift (P < 0.001 vs placebo) and demonstrated that armodafinil was associated with a twofold reduction in ES during the commute home (P < 0.01 vs placebo).Citation46 Electronic diaries used in a study of patients with narcolepsy revealed that armodafinil reduced the number of unintended daily sleep episodes by between 33% and 44% compared with 10% in the placebo group (P < 0.0001).Citation55 In addition, the mean number of daily naps were reduced by between 41% and 44% in the armodafinil-treated group compared with 22% in patients who received placebo (P < 0.01).Citation55
Fatigue
In a study of patients with OSA-associated ES with or without depression, a significant reduction in fatigue (P < 0.01) was reported by armodafinil-treated patients vs the placebo group when assessed using the Brief Fatigue Inventory (BFI).Citation76 Patients with narcolepsy have also reported significantly better relief from the fatigue associated with ES (P < 0.001) when treated with armodafinil vs placebo.Citation55 In an open-label extension study of patients with OSA, SWD, or narcolepsy, armodafinil was associated with an overall improvement from baseline in fatigue and a reduction in worst fatigue, as measured using the BFI.Citation71
Quality of life
Although data on the impact of armodafinil on patients’ QOL have not been explicitly reported, 71% of patients who were administered armodafinil in a recent open-label study reported an improved ability to engage in daily activities.Citation73 The improvements seen in patient-reported outcomes, including subjective ES, cognitive function, and fatigue, are likely to have a positive impact on patients’ lives and well-being.
Safety and tolerability of armodafinil
Armodafinil was generally well tolerated in randomized trials and open-label extension studies of patients with OSA, SWD, or narcolepsy.Citation40,Citation46,Citation55,Citation71,Citation72 Adverse events were reported to be mild to moderate in intensity, with the most common events being headache, nasopharyngitis, anxiety, and insomnia.Citation40,Citation46,Citation55,Citation71 In the randomized studies of patients with OSA, narcolepsy, and SWD, headache occurred in 17%, 22%, and 12% of these patients, respectively ().Citation40,Citation46,Citation55 In the two open-label studies, headache occurred in 17%Citation72 and 25%Citation71 of patients. Overall, no clinically meaningful changes in mean laboratory variables, vital sign measurements, electrocardiogram, or physical examination findings were reported for patients treated with armodafinil.Citation72
Table 3 The most commonly reported adverse events (≥5% of patients) occurring in patients with OSA, narcolepsy, or SWD treated with armodafinil (150 or 250 mg/day)Citation40,Citation46,Citation55
Patient compliance with armodafinil therapy was good, with similar discontinuation rates to those reported with placebo.Citation77 Of the patients treated with armodafinil in the randomized trials, less than 12% in any study withdrew from study treatment because of an emergent adverse event. Approximately 6% of patients who received placebo in these studies withdrew due to adverse events.Citation38–Citation40,Citation55
Conclusions
The personal, social, and economic implications of ES associated with OSA, SWD, or narcolepsy are immense, putting individuals at increased risk for serious health problems, work-related accidents, and road traffic crashes. Treating the underlying cause of ES in patients is vital in order to address this potentially serious issue. However, pharmacotherapy may be required in patients who experience residual ES despite adequate therapy for OSA and in those who have narcolepsy-related ES. Furthermore, some patients who experience ES as a symptom of SWD may not be able to alter their work schedule and may not find their condition abates with behavioral treatments; such patients may, therefore, also require medication to remain wakeful.
The clinical trial results reported herein indicate that armodafinil produces statistically and clinically significant reductions in ES in patients with OSA, SWD, and narcolepsy. For example, a mean sleep latency of ≤5 minutes, as measured using the MSLT, is considered pathological. In the study by Czeisler et al,Citation46 enrolled patients with SWD had a mean sleep latency of 2.3–2.4 minutes at baseline, which was improved to >5 minutes (above the cutoff for pathological sleepiness) at the final visit in patients given armodafinil. This >3-minute increase in sleep latency indicates that the biologic sleep drive of these patients has diminished and that their general functionality has improved. In addition, findings from these randomized and open-label clinical studies show armodafinil to be well tolerated with mild to moderate adverse events. Armodafinil may also improve memory and attention in patients with ES.Citation40,Citation46 Moreover, the wakefulness-promoting effects of armodafinil are of a similar magnitude to those of modafinil. However, the effects of armodafinil may persist for longer than those of modafinil,Citation70 indicating that armodafinil is a useful option for patients who may wish to remain alert later in the day.
Studies of the effect of armodafinil on ES in other patient groups are ongoing or planned and include patients with mild or moderate closed traumatic brain injury (NCT00893789) and patients with sarcoidosis (NCT00555347). Armodafinil is also being investigated as a treatment for jet lag and initial results have been favorable in this indication.Citation78 Further studies of armodafinil may expand its clinical value; however, more safety and efficacy studies are required before armodafinil can be recommended for promoting wakefulness in a wider context, such as instances where public safety or welfare may be an issue. Additional research to elucidate how armodafinil (and modafinil) promote wakefulness would be beneficial, as the mechanisms of action of these agents remain poorly understood at this time.
Acknowledgments
Editorial support was provided by Jane Bryant of Anthemis Consulting Ltd and was funded by Cephalon Inc, Frazer, PA, who provided a medical accuracy review. The authors were not compensated and retained full editorial control over the content of the paper.
Disclosures
Dr Rosenberg has received research funding from Cephalon Inc, Pfizer Inc, sanofi-aventis, Respironics, Neurogen, Vanda Pharmaceuticals, Merck, and GlaxoSmithKline.
Dr Bogan is a shareholder and employee of SleepMed Inc.; acts as a consultant to Cephalon Inc., GlaxoSmithKline, and Jazz Pharmaceuticals; has conducted industry-funded research for Actelion Pharmaceuticals Ltd, Addrenex Pharmaceuticals Inc., Apnicure Inc., Arena Pharmaceuticals Inc., Boehringer Ingelheim, Cephalon Inc., Evotec, GlaxoSmithKline, Jazz Pharmaceuticals, Johnson and Johnson, Eli Lilly and Co., Merck & Co. Inc., Neurogen Corporation, Novartis, Philips, Pfizer Inc., ResMed, sanofi-aventis, Schwarz Pharma, Sensory Medical Inc., Sepracor Inc., Vanda Pharmaceuticals Inc., Ventus Medical, and XenoPort Inc.; and has taken part in speaker bureau engagements for Cephalon Inc., Jazz Pharmaceuticals sanofi-aventis, and Sepracor Inc.
References
- SackRLAuckleyDAugerRRCircadian rhythm sleep disorders: part I, basic principles, shift work and jet lag disorders. An American Academy of Sleep Medicine reviewSleep200730111460148318041480
- National Sleep Foundation2008 Sleep in America PollWashington DCNational Sleep Foundation2008
- ThorpyMJLiebermanJA3rdRothTOwensGSPatient identificationAm J Manag Care200713Suppl 6S132S13918041874
- National Heart, Lung, and Blood Institute Working Group on InsomniaInsomnia: assessment and management in primary careAm Fam Physician199959113029303810392587
- NeubauerDNCurrent and new thinking in the management of comorbid insomniaAm J Manag Care200915SupplS24S3219298103
- SateiaMJUpdate on sleep and psychiatric disordersChest200913551370137919420207
- ParishJMSleep-related problems in common medical conditionsChest2009135256357219201722
- PilcherJJGinterDRSadowskyBSleep quality versus sleep quantity: relationships between sleep and measures of health, well-being and sleepiness in college studentsJ Psychosom Res19974265835969226606
- NewmanABSpiekermanCFEnrightPDaytime sleepiness predicts mortality and cardiovascular disease in older adults. The Cardiovascular Health Study Research GroupJ Am Geriatr Soc200048211512310682939
- ElwoodPHackMPickeringJHughesJGallacherJSleep disturbance, stroke, and heart disease events: evidence from the Caerphilly cohortJ Epidemiol Community Health2006601697316361457
- BixlerEOVigontzasANLinHMCalhounSLVela-BuenoAKalesAExcessive daytime sleepiness in a general population sample: the role of sleep apnea, age, obesity, diabetes, and depressionJ Clin Endocrinol Metab20059084510451515941867
- Ferini-StrambiLBaiettoCDi GiolaMRCognitive dysfunction in patients with obstructive sleep apnea (OSA): partial reversibility after positive airway pressure (CPAP)Brain Res Bull2003611879212788211
- DeanBAguilarDShapiroCImpaired health status, daily functioning, and work productivity in adults with excessive sleepinessJ Occup Environ Med20105214414920134351
- OmachiTAClamanDMBlancPDEisnerMDObstructive sleep apnea: a risk factor for work disabilitySleep200932679179819544756
- DrakeCLRoehrsTRichardsonGWalshJKRothTShift work sleep disorder: prevalence and consequences beyond that of symptomatic day workersSleep20042781453146215683134
- LegerDThe cost of sleep-related accidents: a report for the National Commission on Sleep Disorders ResearchSleep199417184937677805
- FlatleyDReynerLAHorneJASleep-related crashes on sections of different road types in the UK (1995–2001)LondonDepartment of Transport, Road Safety Research Report No 522004
- Pandi-PerumalSRVersterJCKayumovLSleep disorders, sleepiness and traffic safety: a public health menaceBraz J Med Biol Res200639786387116862276
- US Department of TransportationEffects of sleep schedules on commercial motor vehicle driver performance2000 Available from: http://www.fmcsa.dot.gov/documents/execsumm-e1.pdfAccessed Dec 22, 2009
- LopesCEstevesAMBittencourtLRATufikSMelloMTRelationship between the quality of life and the severity of obstructive sleep apnea syndromeBraz J Med Biol Res2008411090891318820762
- DodelRPeterHNoelkerCHealth-related quality of life in patients with narcolepsySleep Med200787–873374117512797
- OzakiAInoueYNakajimaTHealth-related quality of life among drug-naïve patients with narcolepsy with cataplexy, narcolepsy without cataplexy, and idiopathic hypersomnia without long sleep timeJ Clin Sleep Med20084657257819110887
- BaldwinCMGriffthKANietoFJO’ConnorGTWaslebenJARedlineSThe association of sleep-disordered breathing and sleep symptoms with quality of life in the Sleep Heart Health StudySleep2001249610511204058
- BrionesBAdamsNStraussMRelationship between sleepiness and general health statusSleep1996195835888899938
- ReimerMAFlemonsW WQuality of life in sleep disordersSleep Med Rev2003733534914505600
- SforzaEJanssensJ PRochatTIbanezVDeterminants of quality of life in patients with sleep-related breathing disordersEur Respir J200321468268712762357
- ChervinRDSleepiness, fatigue, tiredness, and lack of energy in obstructive sleep apneaChest2000118237237910936127
- JohnsM WA new method for measuring daytime sleepiness: the Epworth sleepiness scaleSleep19911465405451798888
- CarskadonMADementWCMitlerMMRothTWestbrookPRKeenanSGuidelines for the Multiple Sleep Latency Test (MSLT): a standard measure of sleepinessSleep198695195243809866
- LittnerMRKushidaCWiseMPractice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness testSleep20052811312115700727
- American Academy of Sleep MedicineInternational Classification of Sleep DisordersDiagnostic and Coding Manual2nd Ed.Westchester, ILAmerican Academy of Sleep Medicine2005
- YoungTPaltaMDempseyJSkatrudJWeberSBadrSThe occurrence of sleep-disordered breathing among middle-aged adultsN Engl J Med199332817123012358464434
- SmithIEQuinnellTGPharmacotherapies for obstructive sleep apnoea: where are we now? Drugs200464131385139915212557
- SullivanCEIssaFGBerthon-JonesMEvesLReversal of obstructive sleep apnoea by continuous positive airway pressure applied through the naresLancet1981182258628656112294
- WeaverTEMaislinGDingesDFRelationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioningSleep200730671171917580592
- MorgenthalerTIKapenSLee-ChiongTPractice parameters for the medical therapy of obstructive sleep apneaSleep20062981031103516944671
- BlackJEHirshkowitzMModafinil for treatment of residual excessive sleepiness in nasal continuous positive airway pressure-treated obstructive sleep apnea/hypopnea syndromeSleep200528446447116171291
- HirshkowitzMBlackJEWesnesKNieblerGAroraSRothTAdjunct armodafinil improves wakefulness and memory in obstructive sleep apnea/hypopnea syndromeRespir Med2007101361662716908126
- RothTWhiteDSchmidt-NowaraWEffects of armodafinil in the treatment of residual excessive sleepiness associated with obstructive sleep apnea/hypopnea syndrome: a 12-week, multicenter, double-blind, randomized, placebo-controlled study in nCPAP-adherent adultsClin Ther200628568970616861091
- RothTRipponGAAroraSArmodafinil improves wakefulness and long-term episodic memory in nCPAP-adherent patients with excessive sleepiness associated with obstructive sleep apneaSleep Breath2008121536217874255
- SchwartzJRHirshkowitzMErmanMKSchmidt-NowaraWModafinil as adjunct therapy for daytime sleepiness in obstructive sleep apnea: a 12-week open-label studyChest200312462192219914665500
- SchwartzJRRothTShift work sleep disorder: burden of illness and approaches to managementDrugs200666182357237017181377
- McMenaminTMA time to work: recent trends in shift work and fexible schedulesMonth Lab RevDec 2007:315 Available from: http://www.bls.gov/opub/mlr/2007/12/art1full.pdfAccessed Oct 15, 2009
- WaageSMoenBEPallesenSShift work disorder among oil rig workers in the North SeaSleep200932455856519413151
- CzeislerCAWalshJKRothTModafinil for excessive sleepiness associated with shift-work disorderN Engl J Med2005353547648616079371
- CzeislerCAWalshJKWesnesKAAroraSRothTArmodafinil for treatment of excessive sleepiness associated with shift work disorder: a randomized controlled studyMayo Clin Proc2009841195897219880686
- ErmanMKRosenbergRfor the US Modafinil Shift Work Sleep Disorder Study GroupModafinil for excessive sleepiness associated with chronic shift-work sleep disorder: effects on patient functioning and health-related quality of lifePrim Care Companion J Clin Psychiatry20079318819417632651
- HartCLHaneyMNasserJFoltinRWCombined effects of methamphetamine and zolpidem on performance and mood during simulated night shift workPharmacol Biochem Behav200581355956815936062
- LongstrethWTJrTonTGKoepsellTGersukVHHendricksonAVeldeSPrevalence of narcolepsy in King County, Washington, USASleep Med200910442242619013100
- WiseMSArandDLAugerRRBrooksSNWatsonNFfor the American Academy of Sleep MedicineTreatment of narcolepsy and other hypersomnias of central originSleep200730121712172718246981
- US Xyrem Multicenter Study GroupA randomized, double-blind, placebo-controlled multicenter trial comparing the effects of three doses of orally administered sodium oxybate with placebo for the treatment of narcolepsySleep2002251424911833860
- US Xyrem Multicenter Study GroupSodium oxybate demonstrates long-term efficacy for the treatment of cataplexy in patients with narcolepsySleep Med20045211912315033130
- Xyrem International Study GroupA double-blind placebo-controlled study demonstrates sodium oxybate is effective for the treatment of excessive daytime sleepiness in narcolepsyJ Clin Sleep Med20051439139717564408
- Xyrem International Study GroupFurther evidence supporting the use of sodium oxybate for the treatment of cataplexy: a double-blind, placebo-controlled study in 228 patientsSleep Med20056541542116099718
- HarshJRHaydakRRosenbergRThe efficacy and safety of armodafinil as treatment for adults with excessive sleepiness associated with narcolepsyCurr Med Res Opin200622476177416684437
- US Modafinil in Narcolepsy Multicenter Study GroupRandomized trial of modafinil for the treatment of pathological somnolence in narcolepsyAnn Neurol199843188979450772
- US Modafinil in Narcolepsy Multicenter Study GroupRandomized trial of modafinil as a treatment for the excessive daytime somnolence of narcolepsyNeurology20005451166117510720292
- WongYNKingS PSimcoeDOpen-label, single-dose pharmacokinetic study of modafinil tablets: influence of age and gender in normal subjectsJ Clin Pharmacol199939328128810073328
- WongYNSimcoeDHartmanLNA double-blind, placebo-controlled, ascending-dose evaluation of the pharmacokinetics and tolerability of modafinil tablets in healthy male volunteersJ Clin Pharmacol199939130409987698
- FerraroLFuxeKTanganelliSTomasiniMCRambertFAAntonelliTDifferential enhancement of dialysate serotonin levels in distinct brain regions of the rat by modafinil: possible relevance for wakefulness and depressionJ Neurosci Res200268110711211933055
- MitchellHABogenpohlJ WLilesLCBehavioral responses of dopamine beta-hydroxylase knockout mice to modafinil suggest a dual noradrenergic – dopaminergic mechanism of actionPharmacol Biochem Behav200891221722218703079
- QuWMHuangZLXuXHMatsumotoNUradeYDopaminergic D1 and D2 receptors are essential for the arousal effect of modafinilJ Neurosci200828348462846918716204
- Food and Drug AdministrationFDA-approved Labeling Text for NDA 21-875/NUVIGIL™ (armodafinil) Tablets2007 June 15 Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2007/021875lbl.pdfAccessed Oct 15, 2009
- RaoYLiuZ WBorokEProlonged wakefulness induces experience-dependent synaptic plasticity in mouse hypocretin/orexin neuronsJ Clin Invest2007117124022403318060037
- BeckPOdleAWallace-HuittTSkinnerRDGarcia-RillEModafinil increases arousal determined by P13 potential amplitude: an effect blocked by gap junction antagonistsSleep200831121647165419090320
- DarwishMKirbyMHellriegelETRobertsonPJrArmodafinil and modafinil have substantially different pharmacokinetic profiles despite having the same terminal half lives: analysis of data from three randomized, single-dose, pharmacokinetic studiesClin Drug Investig2009299613623
- DarwishMKirbyMHellriegelETYangRRobertsonPJrPharmacokinetic profile of armodafinil in healthy subjects: pooled analysis of data from three randomized studiesClin Drug Investig200929287100
- DarwishMKirbyMRobertsonPJrHellriegelETInteraction profile of armodafinil with medications metabolized by cytochrome P450 enzymes 1A2, 3A4 and 2C19 in healthy subjectsClin Pharmacokinet2008471617418076219
- WisorJ PDementWCAimoneLWilliamsMBozyczko-CoyneDArmodafinil, the R-enantiomer of modafinil: wake-promoting effects and pharmacokinetic profile in the ratPharmacol Biochem Behav200685349249917134745
- DingesDFAroraSDarwishMNieblerGEPharmacodynamic effects on alertness of single doses of armodafinil in healthy subjects during a nocturnal period of acute sleep lossCurr Med Res Opin200622115916716393442
- BlackJHullSGTillerJYangRHarshJRMaintenance of efficacy, safety and tolerability of armodafinil: an open-label extension studySleep200932SupplA139 [Abstract No. 0419]
- SchwartzJRKhanAMcCallVWeintraubJTillerJA 12-month or more open-label study of the efficacy and tolerability of armodafinilSleep200932SupplA50A51 [Abstract No. 0148]
- SchwartzJRBeckerPMTillerJBoganRKArmodafinil improves patient-reported outcomes in patients with excessive sleepiness associated with obstructive sleep apnea or narcolepsySleep200932SupplA190 [Abstract No. 0580]
- KrystalAHarshJYangRRipponGLankfordAA randomised, double-blind, placebo-controlled study with armodafinil in patients with residual excessive sleepiness associated with CPAP-treated obstructive sleep apnoea and comorbid depressive disordersPoster presented at the 19th Meeting of the European Neurological Society2009 June 20–24Milan, Italy [Abstract No. P353]
- AkerstedtTGillbergMSubjective and objective sleepiness in the active individualInt J Neurosci1990521–229372265922
- HullSLankfordAVinceBNieblerGEAroraSArmodafinil improves fatigue in patients with excessive sleepiness due to obstructive sleep apnea/hypopnea syndromePoster presented at the American Psychiatric Association Annual Meeting2006 May 25Toronto, Canada [Abstract No. 127]
- RussoMPharmacotherapy of excessive sleepiness: focus on armodafinilClin Med Ther20091415432
- BoganRTillerJYangRYouakimJRothTArmodafinil for excessive sleepiness associated with jet lag disorderSleep200932SupplA52 [Abstract No. 0153]
