Abstract
Aim: Tracheobronchial anatomy for bronchoscopy education is challenging. 3D printing (3DP) is a promising technology to design bronchoscopy simulators. Materials & m ethods: We created a 3DP tracheobronchial model and color-coded the airways to train first-year pulmonary fellows. A pre- and post-test, practical test and post-test questionnaires were used to evaluate the curriculum implementation. Results: For six fellows the pre- and post-test mean score improved from 11.5/22 (SD = ±1.71) to 16.2/22 (SD = ±2.79). Practical testing mean was 34.5/54 (SD = ±5.82). Questionnaires rated the 3DP model favorably. Conclusion: Our pilot curriculum using a color-coded 3DP model demonstrated improvement in airway identification with favorable ratings by fellows. We posit conceptual frameworks in play and how we address them in future models.
Plain language summary
Bronchoscopy is a procedure where a flexible tube is inserted into a patient’s lungs to diagnose or treat medical conditions. Identifying the anatomy correctly in the procedure is difficult. We created a 3D-printed model of the lung airways with color-coded sections to facilitate training of the procedure and learning the anatomy. Pulmonary fellows trained using the model and showed improvement in their ability to identify lung airways. This curriculum demonstrates a novel use of 3D printing to create a color-coded model to teach complex lung airway anatomy.
Tweetable abstract
The authors of this article created a 3D-printed tracheobronchial model showing improvement in pulmonary fellow anatomy learning.
Training in bronchoscopy remains highly variable among pulmonary training programs, suggesting variable outcomes in competency [Citation1]. Bronchoscopy is a critical skill in pulmonary and critical care medicine, facilitating diagnostic and therapeutic interventions within the lungs. Competency of bronchoscopy follows an apprenticeship model using volume-based certification in most programs [Citation1,Citation2]. Despite prolonged duration of training, bronchoscopic anatomy identification appears to be suboptimal. Pulmonologists are trained to identify anatomy down to the tertiary segmental branches. However, one study of pulmonary fellows showed a 71% success rate in correctly identifying and accessing the target airway on command. Interestingly, there was minimal correlation between number of bronchoscopies performed and accuracy [Citation3]. The American College of Chest Physicians 2015 Expert Panel Report on bronchoscopy training recommended use of high fidelity simulation, knowledge and skills acquisition assessment, and continuing education, signifying a push from the mantra of “see one, do one, teach one” to “see one, simulate many, do one competently” [Citation1,Citation2,Citation4]. Given these findings, we sought to develop a novel 3DP bronchoscopy simulator and curriculum as a targeted intervention to facilitate learning the fundamentals of tracheobronchial anatomy.
Current options for bronchoscopy simulation vary widely [Citation1,Citation4]. Commercial bronchoscopy manikins, ranging in cost from $2000 to $7000 [Citation5], provide haptic feedback but less realistic feel. They are limited to modeled approximations of anatomy and are not modifiable [Citation6]. Virtual reality high-fidelity simulators enable adaptation of scenario, physiologic realism and accurate anatomy [Citation7]. Yet, these simulators cost $25,000 to >$100,000 [Citation8] and have limitations in haptic feedback. In one study, participants rated virtual reality simulation as less useful than manikins or animal models [Citation9]. These current simulator options are variably implemented across training programs and are often secondary to volume-based learning from patient procedures [Citation1]. 3D-printed (3DP) models are lower cost alternatives ($100–300) [Citation10]. In a randomized, single-blind study, experienced proceduralists rated 3DP simulators as more anatomically realistic than commercial models [Citation10]. 3DP allows use of CT scans to generate true representative anatomy, selection of materials for desired model characteristics and modifications in an iterative fashion [Citation6]. One study demonstrated equalization in time to access a target bronchus between novices and experienced residents after both groups trained using a 3DP simulator [Citation11]. A study using 3DP to create a radial endobronchial ultrasound simulator revealed 26% improved scoring on low-difficulty models and 52% improved scoring on high-difficulty models compared with no simulation [Citation12].
A variety of studies have explored the evaluation and use of 3DP bronchoscopy simulators, noting their cost–effectiveness, perceived realism and ability to improve time-to-complete or quality of technical skills [Citation13]. We highlight two studies with evaluation of anatomy learning to contrast our novel approach from existing literature. Parotto et al. assembled a 3DP model using a publicly available model repository, color coding major macroscopic segments though not precisely following anatomic delineations. Formative assessment included pre- and post-tests on bronchoscopic procedural knowledge and performance scoring including ability to identify and enter secondary lobar bronchi. The study noted improvements in test scores, quality of performance and time to complete tasks [Citation14]. DeBoer et al. created an uncolored 3DP model from a patient CT, using self-directed training of residents on the model. Learners were instructed to reach target secondary lobar bronchi and identify color markers placed within. The authors noted improved number of markers identified correctly and time to complete assessment [Citation15].
Stemming from these data, we sought to integrate 3DP model bronchoscopy training into our Pulmonary and Critical Care Medicine Fellowship at University of California, San Francisco (UCSF). Here we present curriculum data as a proof of concept in using a modified 3DP tracheobronchial tree to facilitate learning of tracheobronchial anatomy beyond the secondary lobar bronchi into the more challenging tertiary segmental bronchi (e.g., right- lower lobe medial basal segment). We uniquely utilize color coding as a specified cognitive learning resource to facilitate the learning of this challenging anatomy. To the best of our knowledge, no other curriculum has employed 3DP capabilities in this manner to facilitate learning to this level of anatomic branching.
Materials & methods
Model development
We partnered with UCSF Anatomy faculty and the UCSF Makers Lab staff for the Advanced 3D Printing for Health Science Students course [Citation16] to develop the model, selecting a deidentified CT Aortic protocol with 6.125-mm slice thickness after reviewing radiographically for anatomic accuracy of airways. Model generation was completed using 3D Slicer (3D Slicer Software, Brigham and Women’s Hospital, Harvard Medical School, MA, USA) and Blender (Blender Foundation, Amsterdam, Netherlands). We subsequently partnered with the UCSF Center for Advanced 3D+ Technologies to print higher fidelity training models and half-size take-home models. The 3DP model used in the curriculum cost $300. Funding was provided through the UCSF Makers Lab and the Nina Ireland Program for Lung Health.
Model design
We used an iterative design-based approach to develop and revise the model () [Citation17]. We aimed to create an anatomically accurate model with color-coded airways to be used for simulated bronchoscopy training. The models were printed with the colors directly embedded. The coloring on the first models proved to be excessive, generating overwhelming visual input and overlap of color hues made identification challenging. Subsequent models started coloring at the lobar airways, with proximal orientation relying on the anterior cartilaginous rings. The color coding of the model was simplified by using the same colors for analogous left and right-sided airways. The colors were correlated to the airways via a legend (Appendix E1).
(A) From left to right second–fourth iteration of the model. (B) Half-size take home color-coded models. (C ) Bronchoscopic view of right-upper lobe. On the left is the anterior segment colored orange, at the top is the apical segment colored light gray, and on the right is the posterior segment colored yellow.
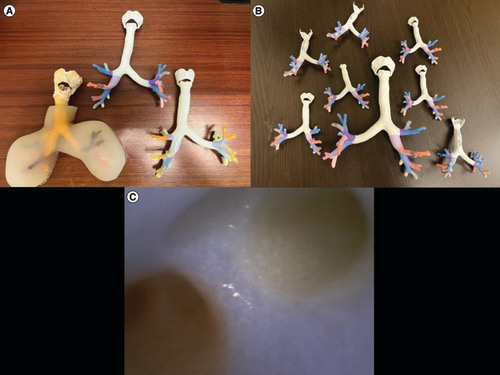
A degree of material transparency was favored to allow confirmation of bronchoscope position externally. The ends of segments were left open to facilitate removal of internal material after printing and to allow for the introduction of foreign bodies and other manipulations.
Curriculum implementation
We created a pre- and post-test focusing on anatomy identification (Appendix E2). Video recordings of bronchoscopic access of airways on the commercial model were provided and participants were asked to identify either the lobar or segmental airway. Tests were administered electronically via Qualtrics (Qualtrics, UT, USA). Eight questions were multiple choice (2 points each) and two questions were short answer (3 points each), with a total of 22 points. The pre test was distributed 3 days before the first training session.
The first-year fellows completed a training protocol on bronchoscopy and tracheobronchial airway anatomy for one hour (Appendix E3). Two to three fellows underwent the training protocol at a given time. Disposable AmbuScopes and an Ambu aView screen (Ambu Inc., MD, USA) were used. The model was stabilized by hand by the instructor. The training protocol began with 10 min of basic bronchoscope principles and handling. Next, the fellows practiced navigating the airways in a systematic manner on the 3DP color-coded tracheobronchial model using the color legend for airway identification for 40 min. Fellows learned the anatomy to the extent of all the tertiary segmental bronchi. Finally, the fellows were asked to navigate to target airways (with access to the color legend) for 10 min. Afterward, fellows were provided half-sized color-coded tracheobronchial models along with a color legend for home review ().
The second bronchoscopy training session, two hours in duration, was held 7 weeks after the initial. An abbreviated training protocol was repeated. Practical testing occurred individually on an unmarked commercial Nakhosteen Bronchoscopy Model (Coburger Lehrmittelanstalt, Coburg DE), with fellows asked to identify each of the tertiary airways then access targets on command. Scoring was completed using a modified Bronchoscopy Skills and Assessment Tool (BSTAT) [Citation18] scale focusing on anatomic identification (Appendix E4).
The day after the second session, the post-test and evaluation questionnaire were distributed using Qualtrics. The latter asked fellows to rate the curriculum using a Likert-scale and to provide qualitative feedback (Appendix E5).
Statistical analysis
Pre- and post-tests were compared using Student’s paired t-test, with p-value < 0.05 considered significant.
Results
Pre- & post-test
Six out of seven first-year fellows completed the pretest. The number of prior bronchoscopies ranged from 0 to 1. Mean score was 11.5/22 (SD = ±1.71). In the pretest, no segments were accurately identified by all the participants and the most misidentified target was the left-lower lobe lateral segment (0/6). The same respondents completed the post-test, with a mean score of 16.2/22 (SD = ±2.79). Number of prior bronchoscopies at this time ranged from 5 to 50. The most misidentified targets were the left-lower lobe lateral segment (2/6) and right-upper lobe anterior segment (2/6). The left-upper lobe apicoposterior, right-middle lobe lateral, left-lower lobe superior and left-upper lobe anterior segments along with the lingula were identified by all the participants (6/6). The mean difference between the pre- and post-test was 4.67, p = 0.004. See for more details.
Table 1. Participant results of pre-, post- and practical tests.
Practical test
Mean score on the practical examination was 34.5/54 (SD = ±5.82) (). The most common error was incorrect landmark referencing such as missing the right-upper lobe then trying to identify the remainder of the segments with an incorrect baseline. The second most common error was missing the right-lower lobe superior segment or confusing it for the right-middle lobe. This was more common when ‘backing into’ the right lung, that is, the scope is oriented with the left lung at the top of the screen and the right lung at the bottom, and anterior to the right when in the trachea. High scorers deliberately reoriented themselves and reset until they were confident in their baseline landmarks.
Questionnaire
Four out of the six fellows completed the questionnaire (). Comments remarked on the model’s success as a visual tool for bronchoscopy and orientation. Potential areas for improvement were the need for more distinct coloring, inability to achieve endoscopic views of the take-home models and desire for more hands-on practice time. Suggestions included a map with bronchoscopic views for the take-home models and restructuring the legend to indicate the colors and labels on an image of the model.
Table 2. Results of the questionnaire.
Discussion
This pilot curriculum utilized a novel 3DP model designed to facilitate learning of tracheobronchial anatomy down to the tertiary segmental branches via color-coded airways. Fellows underwent guided bronchoscopy practice and were given take home models for review. To evaluate fellows’ learning, we conducted pre- and post-curriculum didactic testing along with practical testing on airway identification. Finally, fellow feedback was elicited through a subsequent questionnaire.
We found a small improvement in pre- and post-curriculum didactic airway identification. Despite variability in number of patient bronchoscopies completed from 5 to 50, these did not correlate with either didactic or practical scoring. This is contextualized by prior recommendations to consider competency at 50 or 100 bronchoscopies, suggesting the importance of deliberate practice [Citation19]. Questionnaires rated the 3DP model and curriculum highly for bronchoscopy training and learning tracheobronchial anatomy. Take home models were variably used, but with favorable response as a learning tool.
Despite being fundamental to bronchoscopy training, the investigation of tracheobronchial anatomy learning is limited. The Bronchoscopy Skills and Task Assessment Tool uses anatomy identification for almost half of its scoring, whereas the Ottawa Bronchoscopy Assessment Tool consolidates it into one out of 12 parameters [Citation18,Citation20]. As noted previously, one study of pulmonary fellows showed a 71% success rate in correctly accessing the target airway on command. Of the six fellows with over 200 bronchoscopies, only three accurately accessed all of the targets. Of the six fellows with under 200 bronchoscopies, zero accessed all of the targets [Citation3]. The practical testing in our training program revealed a similar success rate of 64%, albeit only evaluating early first-year fellows having completed up to 50 bronchoscopies.
Factors that contribute to the difficulty of endoscopic anatomy identification include few distinct identifying landmarks and needing to maintain 3D visuospatial orientation. The number of airway branches is not significantly large, yet the limited features to reference can generate confusion, particularly if orientation is lost. The disembodying and disorientating nature of the procedure makes orientation difficult.
One possible explanation is that of spatial memory categorized by egocentric and allocentric reference frames. The ‘first person’ perspective of the bronchoscope lens is egocentric and the ‘third person’ perspective of the bronchoscope tip in the tracheobronchial tree is allocentric. With an egocentric viewpoint, spatial relationships of each airway need to be processed relative to the bronchoscope ‘eye’ and updated individually as movement occurs even when out of view. Alternatively, an allocentric viewpoint enables a top-down view with the simpler visualization of the bronchoscope tip within a tracheobronchial tree [Citation21].
We seek to navigate the complex egocentric-allocentric division inherent in bronchoscopy to facilitate learning tracheobronchial anatomy and the involved spatial reasoning. Our 3DP model serves as a ‘bridging tool’ to make the grasp of these concepts more tangible to a novice via providing ‘attentional anchors’ such as color coded segments to contextualize the anatomy learning [Citation22]. Use of symmetric left and right colors implicitly instructs presence of analogous structures, though the exceptions must still be noted. Stemming from questionnaire results, adjacent colors have been changed for more contrast and the legend shows color-coded nomenclature superimposed on an image of the model.
A new insight is the challenge of learning from an egocentric spatial perspective. To facilitate egocentric and allocentric coordination, we have created an enclosure wherein the model and screen are adjacent in the learner’s field of view. The base and walls are clearly marked with directional arrows indicating anterior, posterior, superior, inferior, medial and lateral. Furthermore, the next model iteration will have a line on the anterior aspect from the trachea to the distal segments, serving as an internal anchor. These implementations contrast 3DP with commercial models or patient procedures, where such learning tools cannot be readily employed.
Based on results of this pilot curriculum, we plan to formally study the 3DP model compared with a commercial bronchoscopy simulator. Medical students and residents will serve as novices randomized to each arm. Recordings of their training and testing along with post-interviews will provide supplementary qualitative data to better understand the learning process, their interaction with simulators, and the impact of using the designed 3DP trainer.
Conclusion
In summary, 3DP is a powerful tool for iteratively generating teaching models. 3DP models are well suited for learning anatomy and procedural skills but should also be considered creatively in other contexts. Just as educators create chalk talks or diagrams, they may use the expansive capabilities of 3DP for novel teaching instruments. In our case, we have developed a color-coded bronchoscopy simulator intended to bridge the gaps in tracheobronchial anatomy education and bronchoscopy visuospatial acumen. Moving forward, we will continue with the iterative process of refining its features while simultaneously studying its impact and efficacy.
Learning tracheobronchial anatomy for bronchoscopy is challenging.
We created a novel 3D-printed simulator with color-coded pulmonary lobes and segments to facilitate anatomy education.
Pulmonary and Critical Care Medicine fellows at University of California, San Francisco trained bronchoscopy and learned tertiary segmental bronchial anatomy via a curriculum implementing this model.
Pre- and post-test didactic scores improved from 11.5/22 (SD = ±1.71) to 16.2/22 (SD = ±2.79).
Mean score on practical examination identifying pulmonary segments using an unmarked commercial manikin was 34.5/54 (SD = ±5.82).
Fellow feedback remarked on the model’s success as a visual tool for bronchoscopy and orientation.
Potential areas for improvement were the need for more distinct coloring, inability to achieve endoscopic views of the take-home models and desire for more hands-on practice time.
There appears to be minimal to no correlation between number of patient bronchoscopies performed and accurate anatomy identification.
We posit that lack of identifying features and the disorienting nature of the procedure make tertiary segmental airway identification challenging.
We employ the conceptual framework of spatial memory from egocentric and allocentric reference frames to understand the challenging nature.
An egocentric bronchoscopy perspective has limited field of view, requiring continuous updating of spatial memory to reference orientation and relative location to landmarks.
An allocentric top-down perspective of the full model has a simpler process of noting the location of the bronchoscope tip within the tracheobronchial tree.
Our next iteration of the model and curriculum seeks to encourage tandem processing of egocentric and allocentric views by placing bronchoscope screen and tracheobronchial model adjacent and providing orientation markers for referencing.
This short communication details the ability of 3DP to uniquely and iteratively generate models targeted to address key learning objectives.
Ethical conduct of research
The authors state that they have obtained informed consent from the participants involved.
Supplemental Appendix
Download MS Word (28 KB)Supplementary data
To view the supplementary data that accompany this paper please visit the journal website at: www.tandfonline.com/doi/suppl/10.2217/3dp-2023-0005
Financial & competing interests disclosure
Funding for the 3DP model used in the curriculum was provided by the University of California, San Francisco Makers Lab (CA, USA) and the University of California Nina Ireland Program for Lung Health (CA, USA). The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Additional information
Funding
References
- ErnstA, WahidiMM, ReadCAet al.Adult bronchoscopy training: current state and suggestions for the future: CHEST Expert Panel Report. Chest148(2), 321–332 (2015).
- LeeHJ, CorbettaL. Training in interventional pulmonology: the European and US perspective. Eur. Respir. Rev.30(160), 200025 (2021).
- CrawfordSW, ColtHG. Virtual reality and written assessments are of potential value to determine knowledge and skill in flexible bronchoscopy. Respiration71(3), 269–275 (2004).
- SchertelA, GeiserT, HautzWE. Man or machine? Impact of tutor-guided versus simulator-guided short-time bronchoscopy training on students learning outcomes. BMC Med. Educ.21(1), 123 (2021).
- Global Technologies. Bronchoscopy Model - Broncho Boy. GTSimulators.com, https://www.gtsimulators.com/products/bronchoscopy-model-broncho-boy-cla9
- HoBHK, ChenCJ, TanGJSet al.Multi-material three dimensional printed models for simulation of bronchoscopy. BMC Med. Educ.19(1), 236 (2019).
- ColtHG, CrawfordSW, GalbraithO. Virtual reality bronchoscopy simulation: a revolution in procedural training. Chest120(4), 1333–1339 (2001).
- KennedyCC, MaldonadoF, CookDA. Simulation-based bronchoscopy training. Chest144(1), 183–192 (2013).
- DeutschES, ChristensonT, CurryJ, HossainJ, ZurK, JacobsI. Multimodality education for airway endoscopy skill development. Ann. Otol. Rhinol. Laryngol.118(2), 81–86 (2009).
- PedersenTH, GysinJ, WegmannAet al.A randomised, controlled trial evaluating a low cost, 3D-printed bronchoscopy simulator. Anaesthesia72(8), 1005–1009 (2017).
- GhazyA, ChabanR, VahlCF, DorweilerB. Development and evaluation of 3-dimensional printed models of the human tracheobronchial system for training in flexible bronchoscopy. Interact. Cardiovasc. Thorac. Surg.28(1), 137–143 (2019).
- RidgersA, LiJ, Coles-BlackJet al.Teaching radial endobronchial ultrasound with a three-dimensional-printed radial ultrasound model. ATS Sch.2(4), 606–619 (2021).
- LeongTL, LiJ. 3D printed airway simulators: adding a dimension to bronchoscopy training. Respirology25(11), 1126–1128 (2020).
- ParottoM, JiansenJQ, AboTaibanAet al.Evaluation of a low-cost, 3D-printed model for bronchoscopy training. Anaesthesiol. Intensive Ther.49(3), 189–197 (2017).
- DeBoerEM, WagnerJ, KroehlMEet al.Three-dimensional printed pediatric airway model improves novice learners’ flexible bronchoscopy skills with minimal direct teaching from faculty. Simul. Healthc.13(4), 284–288 (2018).
- University of California, San Francisco. Advanced 3D Printing Elective . UCSF Libraryhttps://www.library.ucsf.edu/use/makerslab/advanced-3d-printing-elective/
- vanden Akker J, GravemeijerK, McKenneyS, NieveenN. Introducing educational design research. In: Educational Design Research (1st Edition).vanden Akker J, GravemeijerK, McKenneyS, NieveenN ( Eds). Routledge, Oxon, England, 1–51 (2006).
- DavoudiM, OsannK, ColtHG. Validation of two instruments to assess technical bronchoscopic skill using virtual reality simulation. Respiration76(1), 92–101 (2008).
- JantzMA, McGaghieWC. It’s time for a STAT assessment of bronchoscopy skills. Am. J. Respir. Crit. Care Med.186(8), 703–705 (2012).
- VoducN, AdamsonR, KashgariAet al.Development of learning curves for bronchoscopy: results of a multicenter study of pulmonary trainees. Chest158(6), 2485–2492 (2020).
- BurgessN. Spatial memory: how egocentric and allocentric combine. Trends Cogn. Sci.10(12), 551–557 (2006).
- AbrahamsonD. Embodied design: constructing means for constructing meaning. Educ. Stud. Math.70(1), 27–47 (2009).

