Abstract
Conclusion: An epidemiological survey of hospitals and private clinics in Japan regarding idiopathic sudden sensorineural hearing loss (SSNHL) revealed that the incidence of SSNHL was 60.9 per 100 000 population. There were more females than males in the younger generation. Objective: The incidence of SSNHL varies largely by country. Because the Japanese criteria for diagnosing SSNHL have changed in accordance with those widely used in other parts of the world, a clinicoepidemiological study was undertaken using the new criteria. Methods: Ehime, Aichi, and Iwate Prefectures were selected from the western, central, and northeastern regions of Japan, respectively. The subjects for this study were patients who suffered SSNHL between April 1, 2012 and March 31, 2013. Questionnaires were mailed to all hospitals and private clinics in which ENT doctors were working. Initial and final audiograms were requested for 10% of the patients. Results: In all, 78 of 90 hospitals (87%) and 303 of 407 private clinics (74%) responded. It was reported that 1663 patients visited hospitals and 3090 patients visited only private clinics. It was estimated that 6205 SSNHL patients visited hospitals or private clinics in 1 year from a population of 10 145 000. Also, 23% of patients suffered acute low-tone SNHL (female to male ratio; 3:1 in definite cases).
Introduction
Nationwide epidemiological surveys concerning idiopathic sudden sensorineural hearing loss (SSNHL) were conducted, using specific criteria [Citation1], four times by the Research Committees of the Ministry of Health and Welfare in Japan [Citation2–4]. The first, second, third, and fourth surveys were performed on patients who suffered from SSNHL and visited hospitals between July 1, 1971 and June 30, 1973; between January 1 and December 31, 1987; between January 1 and December 31, 1993; and between January 1 and December 31, 2001 [Citation2–4]. The criteria for SSNHL that have been used for nearly 40 years in Japan did not provide concrete figures for the hearing levels. In 2012, the Research Committee of the Ministry of Health and Welfare for Acute Profound Deafness established new criteria that defined hearing levels for SSNHL as 30 dB or more over three consecutive frequencies, in accordance with the definition widely used in other parts of the world () [Citation5].
Table I. Criteria for diagnosis of sudden deafness*.
Using the new criteria, the committee performed an epidemiological study of SSNHL on patients who visited hospitals or private ENT clinics during 1 year from April 1, 2012. This study presents the current status of SSNHL in Japan.
Material and methods
Because we expected that many SSNHL patients visited only private ENT clinics, both hospitals and private clinics were included in this study, unlike previous surveys of hospitals only. To perform this study, Ehime, Aichi, and Iwate Prefectures were selected (). Ehime, Aichi, and Iwate Prefectures are located in the western, central, and northeastern regions of Japan, respectively. They contain the fourth largest city in Japan (Nagoya), provincial cities, and rural areas. Moreover, the incidence of SSNHL in each of these three prefectures was at the average level found in the 2001 national survey [Citation6].
Figure 1. The three prefectures selected for the epidemiological study of sudden sensorineural hearing loss (SSNHL) in Japan.

In April 2012, letters were mailed to all hospitals with ENT clinics and to private ENT clinics to inform them of the purpose of the survey with the new criteria for defining SSNHL. The subjects for this study were patients who suffered SSNHL between April 1, 2012 and March 31, 2013.
An intermediate survey was conducted in the autumn of 2012 to collect the number of patients and referrals from or to other hospitals or private clinics in Aichi. The final survey to collect the patient data was conducted in June or July 2013 in Ehime, Aichi, and Iwate, and it included date of birth, sex, date of onset of SSNHL, date of first clinic visit, and the presence or absence of referral from or to other hospitals or private clinics. Information regarding the patients’ date of birth, sex, date of onset, and presence or absence of referral was used to identify duplicate patients. In case there was response only to the intermediate survey, and not to the final survey, we used the average monthly number of patients in the intermediate survey to estimate the annual number of patients in each hospital or clinic on the assumption of no seasonal difference. In the final survey, initial and final audiograms were requested for those patients whose birthday was the 3rd, 13th, or 23rd day of the month.
All data, including the hearing thresholds in the audiograms, were entered into a computer. From the audiogram data, the grade of the initial audiogram () [Citation7] and the recovery rate, defined by the Ministry of Health and Welfare in Japan () [Citation8], were obtained. From the audiograms, we also investigated the number of patients suffering acute low-tone sensorineural hearing loss (ALHL). In this study, we used criteria for ALHL described in the previous literature [Citation9].
Table II. Criteria for the grading of hearing loss in idiopathic sudden sensorineural hearing loss (SSNHL)*.
Table III. Hearing improvement as defined by the Ministry of Health and Welfare in Japan*.
The study protocol was approved by the Ethics Review Committees of Nagoya University, Iwate Medical University, and Ehime University. Statistical analyses were performed using Stata ver. 11.2 (Stata Corp., College Station, TX, USA) including 95% confidence interval (CI), Student’s t tests, and chi-squared tests. Results were regarded as significant when p < 0.05.
Results
The response rate, number of patients, population, and incidence of SSNHL in each prefecture are shown in . In Iwate, all hospitals and private clinics responded; however, in Ehime and Aichi, not all hospitals and private clinics responded. The estimated number of patients was obtained by assuming that the number of patients was the same between hospitals that did and did not respond, taking into account hospital size, as shown in . In a similar manner, the estimated number of patients who visited only private clinics was also obtained. The actual number of patients reported to have visited hospitals was 265, 1249, and 149 in Ehime, Aichi, and Iwate, respectively. The actual number of patients who visited only private clinics was 614, 2044, and 432 in Ehime, Aichi, and Iwate, respectively. Of the total 4753 patients, 65.0% visited only private clinics. The female-to-male ratio was 1.22:1.00. It was estimated that the number of patients was 1019 (95% CI, 934–1105) in Ehime, 4582 (95% CI, 4257–4907) in Aichi, and 581 in Iwate. In total, it was estimated that 6182 (95% CI, 5847–6517) SSNHL patients visited hospitals or private clinics in 1 year in a population of 10 145 000; the incidence of SSNHL was 60.9 (95% CI, 57.6–64.2) per 100 000.
Table IV. Results of the epidemiological survey in three prefectures in Japan.
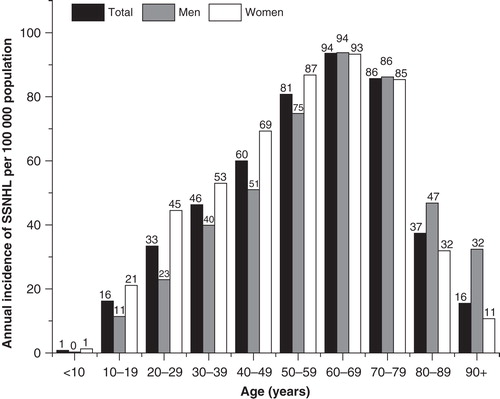
shows the incidence of SSNHL in each age group. The incidence increased from 9 per 100 000 for patients younger than 20 years to 94 per 100 000 for patients in the age range 60–69 years. The percentage of patients younger than 20 years was 3.2%. The youngest patient was aged 8 years and the oldest patient was aged 96 years. The average age was 54.2 years (SD = 17.1). There was a tendency for more females than males to be affected in the younger age groups.
Figure 2. Distribution of annual incidence of sudden sensorineural hearing loss (SSNHL) for men and women, in each age group.
The season of onset was divided into Japanese spring (March–May), summer (June–August), autumn (September–November), and winter (December–February). The number of patients reported in each season from the final survey was 966, 1094, 1103, and 936 in spring, summer, autumn, and winter, respectively. There were no significant differences between the four seasons.
In patients from whom initial and final audiograms were obtained, 98.2% of the patients had hearing loss of 30 dB or more over three consecutive frequencies on the initial audiograms. Because the recovery rate is significantly associated with the interval between the onset of SSNHL and the diagnosis, the recovery rate of patients who visited ENT doctors with hearing loss of 30 dB or more over three consecutive frequencies within 2 weeks after the onset of SSNHL in each grade was assessed (). The presence or absence of vertigo was not considered because we did not obtain such information. The complete recovery rate was 67%, 37%, 32%, and 4%, for grades 1, 2, 3, and 4, respectively. When the final hearing level was graded, as shown in , grade 2 patients who visited an ENT doctor within 2 weeks after the onset of SSNHL had a final hearing level of grade 1 in 75% of cases and grade 2 in 23% of cases. Those patients classified as grade 3 at the first visit had a final hearing level of grade 1, grade 2, and grade 3 in 45%, 26%, and 26% of cases, respectively. The patients with grade 4 at the first visit had a final hearing level of grade 1 in 21%, grade 2 in 4%, grade 3 in 46%, and grade 4 in 29% of cases.
Table V. Final hearing outcome in each grade of sudden sensorineural hearing loss (SSNHL).
In patients whose initial audiograms had hearing loss of 30 dB or more over three consecutive frequencies, 23% of the patients had hearing loss corresponding to the criteria of ALHL. Definite and probable cases were 18% and 5%, respectively. There were 56 patients (42 female and 14 male) with definite ALHL and 16 patients (6 female and 10 male) with probable ALHL. In the definite group, the number of ALHL patients who were female was more than those who were male (p < 0.01). The average age of the definite and probable ALHL patients was 43.0 years (SD = 14.7) and 63.7 years (SD = 9.0), respectively. The age of the definite ALHL patients was significantly younger than that of the patients with SSNHL (ALHL patients excluded) (p < 0.01).
Discussion
This study revealed that the annual incidence of SSNHL in Japan was 60.9 per 100 000 population. The incidence was much higher than rates reported previously in Japan [Citation2–4]. This difference may be because of the inclusion in the survey of private ENT clinics. The present survey revealed that 65% of SSNHL patients visited only private ENT clinics. The previous reports in Japan did not include patients who visited only private clinics [Citation2–4,6,10,11]. The present investigation included private clinics but selected only three prefectures in Japan. This was a limitation of the study. The incidence reported here was higher than the 27/100 000 reported from the United States [Citation12] but lower than the 160–300/100 000 reported from Germany [Citation13,14]. The incidence of SSNHL may be related to whether or not private clinics or outpatient (ambulatory) treatment are included. In Japan, the estimated annual number of patients with SSNHL increased over the years 1972 to 2001 [Citation4]. Because these earlier surveys were carried out using the old criteria, it is difficult to compare the previous and present surveys for investigation of trends in the incidence of SSNHL in Japan. This study revealed that the percentage of hearing loss corresponding to definite ALHL increased to 18% from 9% that was reported previously using the old criteria [Citation10]. However, it seems that the annual number of SSNHL patients who visited hospitals did not increase compared with investigations conducted 10 years ago. Wu et al. [Citation15] examined the incidence of SSNHL in Taiwan from the country’s National Health Insurance program database, capturing inpatient medical claims for more than 20 million people. They found an annual incidence of 10.21 per 100 000 in 2002. The most suitable method for conducting such surveys may vary by country. In Japan, which has a population of 128 million, there are about 10 000 ENT doctors, and half of them own private clinics. Direct communication using questionnaires administered directly to ENT doctors working in both hospitals and private clinics may be a more useful method of investigating the incidence of SSNHL in Japan.
The incidence of SSNHL was 72.0, 61.7, and 44.6 per 100 000 in the prefectures of Ehime, Aichi, and Iwate, respectively. The area of Iwate is 2.69 times larger than that of Ehime and 2.96 times larger than that of Aichi. The number of ENT doctors in Iwate is the lowest per population among the three prefectures. The influence of the large earthquake that hit eastern Japan on March 11, 2011 still remains in Iwate. Such social factors may be associated with the low incidence of SSNHL found in Iwate. The percentage of grade 1 SSNHL was 40%, 34%, and 29% in Ehime, Aichi, and Iwate Prefectures, respectively. It is probable that many patients with mild symptoms did not consult doctors in Iwate.
The present study demonstrated that the incidence of SSNHL was high in the 50s, 60s, and 70s age groups in Japan. There was a tendency for the peak of the incidence to move to the older generation compared with that of previous surveys in Japan [Citation4]. Because aging of the Japanese society is proceeding quickly, the number of aged people will increase more in the future. In the younger generation, the number of females with SSNHL was more than that of males. This tendency was associated with the incidence of definite ALHL in young females. Alexander and Harris [Citation12] reported that men were more likely to be affected than women in patients older than 55 years. On the contrary, Klemm et al. [Citation14] described an overall female preponderance in Germany. Our study revealed that there were more female patients in the younger generation, including those with definite ALHL. Previous studies have reported that some patients with ALHL or SSNHL had evidence of endolymphatic hydrops on MRI [Citation9,16]; therefore, some cases of SSNHL may be associated with Ménière’s disease.
Regarding the recovery of hearing after SSNHL, we used criteria determined by the Research Committee of the Ministry of Health and Welfare in Japan (). The criteria, which are often described as Furuhashi’s criteria in Western countries [Citation17,18], utilize both the final hearing level and the size of the hearing gain, as per Siegel’s criteria [Citation19]. It was found that the proportion with marked recovery was greater for grade 3 patients than for grade 2 patients (). This reversal phenomenon may depend on utilization of the size of the hearing gain in the criteria. In the present study, we also evaluated hearing outcome utilizing only the hearing levels. The final hearing grade was recorded for each grade identified from the initial audiogram. The distribution of the final hearing grade for each initial hearing grade indicated that the grading method is useful for the evaluation of hearing outcome after SSNHL. It was obvious that patients with grade 4 SSNHL, who accounted for 8% of the total SSNHL patients, had the worst hearing outcome. By analyzing hearing outcome in each grade of SSNHL, we found that the degree of hearing recovery found in the present study was not significantly different compared with previous studies undertaken 30 or 40 years ago in Japan [Citation20]. It does not seem that treatment methods for SSNHL changed much during this period in Japan [Citation11].
In conclusion, an epidemiological survey of SSNHL conducted among hospitals and private clinics in Japan revealed that the incidence of SSNHL was 60.9 per 100 000 population. The incidence was high in the 50s, 60s, and 70s age groups. There were more females than males in the younger generation. When hearing outcome was evaluated in each grade of SSNHL, there were no significant differences between the present and past results. To improve the results of treatment for SSNHL of various etiologies, elucidation of the mechanisms of SSNHL is required for development of the most effective treatment for each etiology.
Acknowledgments
We thank all otolaryngologists who cooperated by answering the questionnaires. This work was supported by the Acute Profound Deafness Research Committee of the Ministry of Health, Labour and Welfare in Japan. We also thank Dr Yasuyo Takayanagi who encouraged and supported our study of SSNHL.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Nomura Y. Diagnostic criteria for sudden deafness, mumps deafness and perilymphatic fistula. Acta Otolaryngol Suppl 1988;456:7–8.
- Nakashima T, Yanagita N, Ohno Y, Kanzaki J, Shitara T. Comparative study on sudden deafness by two nationwide epidemiological surveys in Japan. Acta Otolaryngol Suppl 1994;514:14–16.
- Nakashima T, Itoh A, Misawa H, Ohno Y. Clinicoepidemiologic features of sudden deafness diagnosed and treated at university hospitals in Japan. Otolaryngol Head Neck Surg 2000;123:593–7.
- Teranishi M, Katayama N, Uchida Y, Tominaga M, Nakashima T. Thirty-year trends in sudden deafness from four nationwide epidemiological surveys in Japan. Acta Otolaryngol 2007;127:1259–65.
- Nomura Y. Morphological aspects of inner ear disease. Tokyo: Springer. 2014.
- Teranishi M, Katayama N, Uchida Y, Toda J, Nakashima T, Kitamura K. Investigation of annual numbers of patients with sudden deafness treated in each district using the data by a nationwide epidemiological survey. Otol Jpn 2007;17:621–6.
- Kanzaki J, Taiji H, Ogawa K. Evaluation of hearing recovery and efficacy of steroid treatment in sudden deafness. Acta Otolaryngol Suppl 1988;456:31–6.
- Furuhashi A, Matsuda K, Asahi K, Nakashima T. Sudden deafness: long-term follow-up and recurrence. Clin Otolaryngol 2002;27:458–63.
- Shimono M, Teranishi M, Yoshida T, Kato M, Sano R, Otake H, et al. Endolymphatic hydrops revealed by magnetic resonance imaging in patients with acute low-tone sensorineural hearing loss. Otol Neurotol 2013;34:1241–6.
- Matsuda K, Misawa H, Teranishi M, Hosokawa M, Nakashima T. Acute low-tone sensorineural hearing loss – with nationwide epidemiological study of sudden deafness. Audiol Jpn 2002;45:197–202.
- Nakashima T, Tominaga M, Ishida IM, Uchida Y, Teranishi M, Toda J, et al. A nationwide epidemiological survey regarding sudden deafness in 2001 – factors influencing its prognosis. Audiol Jpn 2004;47:109–18.
- Alexander TH, Harris JP. Incidence of sudden sensorineural hearing loss. Otol Neurotol 2013;34:1586–9.
- Suckfull M. Perspectives on the pathophysiology and treatment of sudden idiopathic sensorineural hearing loss. Dtsch Arztebl Int 2009;106:669–75.
- Klemm E, Deutscher A, Mosges R. A present investigation of the epidemiology in idiopathic sudden sensorineural hearing loss. Laryngorhinootologie 2009;88:524–7.
- Wu CS, Lin HC, Chao PZ. Sudden sensorineural hearing loss: evidence from Taiwan. Audiol Neurootol 2006;11:151–6.
- Chen X, Zhang XD, Gu X, Fang ZM, Zhang R. Endolymphatic space imaging in idiopathic sudden sensorineural hearing loss with vertigo. Laryngoscope 2012;122:2265–8.
- Labatut T, Daza MJ, Alonso A. Intratympanic steroids as primary initial treatment of idiopathic sudden sensorineural hearing loss. The Hospital Universitario Ramon y Cajal experience and review of the literature. Eur Arch Otorhinolaryngol 2013;270:2823–32.
- Filipo R, Attanasio G, Cagnoni L, Masci E, Russo FY, Cartocci G, et al. Long-term results of intratympanic prednisolone injection in patients with idiopathic sudden sensorineural hearing loss. Acta Otolaryngol 2013;133:900–4.
- Siegel LG. The treatment of idiopathic sudden sensorineural hearing loss. Otolaryngol Clin North Am 1975;8:467–73.
- Nakashima T, Ueda H, Misawa H, Itoh A, Tominaga M. The results of nationwide epidemiological surveys on sudden deafness analyzed by the grading system determined by the Research Committee on Acute Profound Deafness of the Ministry of Health and Welfare in Japan. Audiol Jpn 2000;43:98–103.

