Abstract
Aim. To assess the efficacy of continuous therapy (cont) and on-demand therapy (on-demand) as maintenance therapy for gastroesophageal reflux disease (GERD). Methods. Patients with upper GI endoscopy (EGD)-proven GERD who completed 8 weeks of initial therapy were randomized to cont (omeprazole 20 mg od) or on-demand (omeprazole 20 mg on-demand) group. Assessments by the Global Overall Symptom (GOS) scale at baseline (at the start of maintenance therapy) and at 8-week, 16–week, and 24-week visits were made and EGD was performed at 24 weeks. Symptom relief was defined as percentages of patients whose GOS score of 1 or 2. Results. Of the 117 enrolled patients, cont/on-demand was 59/58 and nonerosive reflux disease (NERD)/reflux esophagitis (RE) before the initial therapy was 35/82. Symptom relief in cont/on-demand were 57.6%/48.3% at baseline (n.s.), 66.7%/54.7% at 8 week (n.s.), 64.6%/54.7% at 16 weeks (n.s.), and 66.7%/74.0% at 24 weeks (n.s.). When subjects were divided into NERD and RE, symptom relief in cont/on-demand were 33.3%/41.2% at baseline (n.s.), 43.8%/64.3% at 8 weeks (n.s.), 50.0%/42.9% at 16 weeks (n.s.), and 50.0%/69.2% at 24 weeks (n.s.) in NERD, while those were 68.3%/51.2% at baseline (n.s.), 76.3%/51.3% at 8 weeks (p < 0.05), 70.6%/59.0% at 16 weeks (n.s.), and 72.7%/75.7% at 24 weeks (n.s.) in RE, respectively. At 24-week EGD, all patients in NERD remained as NERD but number of healed patients was significantly higher in cont (85.3%) than in on-demand (44.4%) (p < 0.01) in RE. Conclusions. Since NERD is defined by symptoms, as a result of the limited efficacy of continuous therapy, on-demand therapy would be sufficient as maintenance therapy in NERD patients. Regarding RE, continuous therapy would be recommended in terms of reduced symptoms and maintaining mucosal healing.
Background and aim
The prevalence of gastroesophageal reflux disease (GERD) is increasing in Japan. Indeed, a report from Japan noted that the prevalence of GERD began to increase rapidly from the end of the 1990s [Citation1]. A systematic review reported that the prevalence of GERD was as high as 10–20%, whereas its incidence was as low as 4.5–19.6 per 1000 person-years, suggesting that GERD is likely to persist for many years, on average 18–44 years [Citation2]. In other words, GERD is considered likely to recur. Accordingly, GERD could be considered to be a chronic disease, and, therefore, maintenance therapy as well as initial therapy would be important in the management of GERD. Although a number of studies described the clinical importance of maintenance therapy [Citation3], there are only a few studies regarding maintenance therapy for GERD in Japan [Citation4–7].
Since maintenance therapy would typically span a long period, patients sometimes prefer to take medicine on-demand because of expense (including limitations of medical insurance) and/or compliance. Because on-demand therapy is less expensive than continuous therapy, further studies are worthwhile to confirm the usefulness of this strategy for maintenance therapy for GERD.
There have been some studies regarding on-demand maintenance therapy for GERD [Citation7,8]. However, there has been no study that compared the efficacy of continuous therapy with that of on-demand therapy as maintenance therapy in Japan. Since the therapeutic response might be different in each country, evaluation of maintenance therapy should be performed among Japanese. This study is the first prospective randomized study to compare the efficacy of continuous therapy with on-demand maintenance therapy for GERD in Japan.
Methods
This study was designed as a prospective parallel randomized open-label study at a single university hospital between April 2009 and April 2013. The Juntendo University Ethics Committee approved the study protocol. The performance of this study adhered to the principles of the Declaration of Helsinki for medical research involving human subjects.
Patients with GERD who had completed at least 8 weeks of initial proton pump inhibitor (PPI) therapy were recruited for this study. Eligible patients were those with a diagnosis of GERD by upper GI endoscopy of either the modified Los Angeles (LA) classification grade M, A, B, C, or D before the initial PPI treatment and who provided written informed consent to participate in this study. Grade M indicates a minimal change in modified LA classification that expresses erythematous changes (red ones) and acanthotic changes (white ones) [Citation9]. Excluded were patients with cancer, serious liver disease, kidney disease, heart disease, a hematological disorder, gastric ulcers, and/or duodenal ulcers. Also excluded were pregnant or nursing women as well as those hoping for pregnancy. Ineligible were patients who participated in other clinical trials that could influence the results of this trial within 1 month before the start of the present study. A past history of an adverse reaction to omeprazole, and being judged as inappropriate for a clinical trial by a physician were also reasons for exclusion.
Patients were randomly assigned at a 1:1 ratio to either the continuous group (omeprazole 20 mg od) or the on-demand group (omeprazole 20 mg on-demand up to 1 tablet a day) for 24 weeks. Randomization was conducted using a computer-generated randomization list that was created by a third party.
Patients' symptoms and quality of life (QOL) were assessed by the Global Overall Symptom (GOS) scale and the Japanese version of the Quality of Life in Reflux and Dyspepsia (QOLRAD-J) at baseline, 8 weeks, 16 weeks, and 24 weeks. For 24 weeks, patients recorded on a chart daily the chief symptom on that day or whether no symptom was present as well as tablet usage. Upper GI endoscopy was performed at 24 weeks.
The GOS consisted of the following 8 items in this study: (1) stomach pain, (2) heartburn, (3) regurgitation, (4) postprandial fullness, (5) vomiting, (6) belching, (7) early satiety, and (8) bloating. Their severity was measured on a 7-point Likert scale as follows: 1 = no problem (no symptoms); 2 = minimal problem (can be easily ignored without effort); 3 = mild problem (can be ignored with effort); 4 = moderate problem (cannot be ignored but does not influence daily activities); 5 = moderately severe problem (cannot be ignored and occasionally limits daily activities); 6 = severe problem (cannot be ignored and often limits concentration on daily activities); and 7 = very severe problem (cannot be ignored, markedly limits daily activities and often requires rest) [Citation10]. Symptom relief was defined as a GOS score of 1 (no problem) or 2 (minimal problem) for each item.
Our first aim was to compare the percentage of patients who achieved symptom relief at 4, 8, 16, and 24 weeks in each study group with relief from symptoms as the primary endpoint. We also compared between-group scores of QOLRAD-J at each visit and the percentage of patients who were symptom free for ≥6 days a week as noted in the daily chart, with results of these comparisons being secondary endpoints.
Sample size calculations were based on an estimated symptom relief rate of 0.9 for the continuous group and 0.7 for the on-demand group. Using these criteria, with a power of 0.8 at the 0.05 two-sided significance level, 124 patients were required to participate in the study.
Results of the primary and secondary endpoints were analyzed using data from all patients who had at least one assessment of efficacy after the initiation of study treatment. Inter-group differences in the proportion of patients reaching the primary and secondary endpoints were analyzed using the chi-square test and Fisher's exact test. QOLRAD-J scores were compared by the Mann–Whitney's U test. Statistical significance was defined as p < 0.05 (two-sided).
Results
Of the 119 patients who were enrolled and provided informed consent, a patient who received a histamine-2 receptor antagonist as an initial treatment and a patient who received only a 4-week PPI initial treatment regimen were excluded from this study. Of the remaining 117 patients, 59 were randomly allocated to the continuous group and 58 to the on-demand group. shows the characteristics of the patients at the time of enrollment. There were no significant differences in GOS scores between the two groups at the time of randomization. shows the average of the QOLRAD-J scores for each group at each visit, with no significant between-group differences at the time of randomization. Of the 117 participants, completing the GOS were 54 and 53 in the continuous group and on-demand group, respectively, at 8 weeks, 48 and 53, respectively, at 16 weeks, and 45 and 50, respectively, at 24 weeks. The number of patients in each group who answered the QOLRAD-J was the same except at 16 weeks when 49 patients in the continuous group completed the instrument.
Table I. Characteristics of study patients at baseline.
Table II. Alterations in Quality of Life in Reflux and Dyspepsia, Japanese version scores during maintenance therapy.
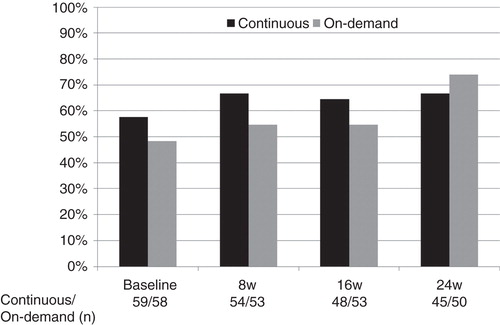
We analyzed data from the GOS, QOLRAD-J, and daily chart using the full analysis set. This term is used to describe the analysis set that included all randomized subjects in this study. In the analysis using the full analysis set, percentages of patients who achieved symptom relief in the continuous and on-demand groups according to the GOS were 57.6 and 48.3 at baseline (n.s.), 66.7 and 54.7 at 8 weeks (n.s.), 63.3 and 54.7 at 16 weeks (n.s.), and 66.7 and 75.5 at 24 weeks (n.s.), respectively (). There were no statistically significant differences between the two groups for the QOLRAD-J at each visit ().
Figure 1. Percentages of patients who achieved symptom relief in the continuous and on-demand groups according to GOS scores at baseline and at the 4-, 8-, 16-, and 24-week visits. There were no significant between-group differences in the percentage of patients who achieved symptom relief at any visit.
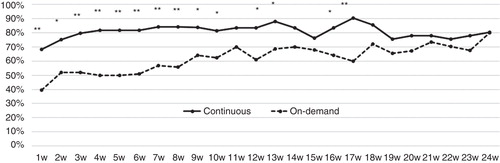
From information on the daily charts, we assessed the number of tablets consumed per week () and the number of days per week during which symptoms were present. We defined symptom relief as a patient being free of symptoms according to chart records for 6 or more days per week. The percentage of patients who achieved symptom relief each week is shown in . Mean pill consumption during the 24-week maintenance period ranged from 6.2 to 6.9 tablets per week in the continuous group but gradually decreased in the on-demand group from 3.0 to 1.8 tablets per week. Interestingly, significantly more patients in the continuous group achieved symptom relief during two thirds of the 24 weeks of maintenance therapy, specifically from week 1 to week 10 and during weeks 12, 13, 16, and 17. However, this difference disappeared in the last 7 weeks.
Figure 2. Mean number of consumed tablets per week recorded on a daily chart. Data are shown with standard deviation.
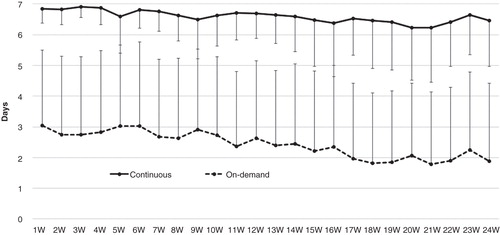
Figure 3. Percentage of patients who were symptom free for 6 or more days a week as recorded on a daily chart. **p < 0.01, *p < 0.05 versus on-demand group.
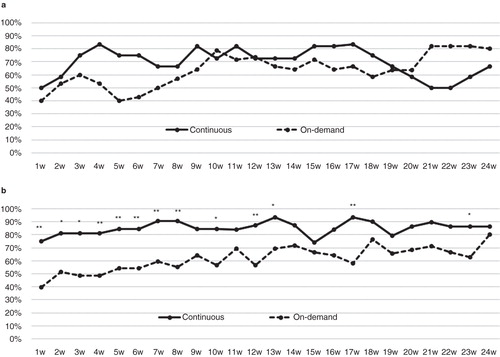
In this study, 35 patients were diagnosed as grade M before the initial therapy. Since therapeutic efficacy in the maintenance period might be different between nonerosive reflux disease (NERD) and reflux esophagitis (RE), we compared symptom relief as determined by the GOS and information on the daily chart between NERD (Grade M) and RE (Grade ≥ A). shows information on the study patients according to whether they were classified as Grade M or Grade ≥ A. Percentages of patients who achieved symptom relief according to the GOS were not significantly different for Grade M between the continuous and on-demand groups, but among Grade ≥ A, significantly more patients in the continuous group than in the on demand group experienced symptom relief at 8 weeks (). Regarding information on the daily chart, continuous group patients with Grade ≥ A achieved significant symptom relief not only during two thirds of the maintenance period but also at the end of period in comparison with the on-demand group; however, there were no significant between-group differences in patients with Grade M ().
Table III. Patients' characteristics at baseline according to classification of Grade M and Grade ≥ A.
Figure 4. Percentages of patients classified as (a) Grade M or (b) Grade ≥ A who achieved symptom relief in the continuous and on-demand groups according to the GOS. *p < 0.05 versus on-demand group.
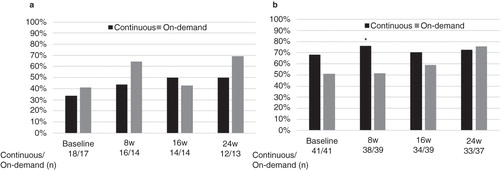
Figure 5. Percentages of patients classified as (a) Grade M or (b) Grade ≥ A who were symptom free for ≥6 days a week in the continuous and on-demand groups according to daily chart entries. **p < 0.01, *p < 0.05 versus on-demand group.
Twenty-eight patients in Grade M and 70 patients in Grade ≥ A undertook upper GI endoscopy at 24 weeks. Regarding the endoscopic findings, all patients in Grade M did not develop RE. Among patients with Grade ≥ A, 49 were healed and 21 were not healed (Grade A: 14, B: 5, C: 2, D: 0) at 24 weeks, respectively. Number of healed patients was significantly higher in continuous group (85.3%) than in on-demand group (44.4%) (p < 0.01).
Discussion
There have been some studies regarding on-demand therapy for GERD. Of those that compared on-demand and continuous arms in patients with RE and/or NERD, continuous treatment provided the better outcome [Citation11–13], but in another report, significantly more patients were willing to continue taking on-demand PPI than comply with continuous administration [Citation14]. A recent meta-analysis revealed that on-demand therapy with a PPI is superior to once-daily treatment (RR: 0.52; 95% CI: 0.34, 0.79) in terms of mild GERD [Citation8]. Accordingly, conflicting published results might have been caused by differences in various factors, such as study design and patient population.
About half of the study patients achieved symptom relief defined as a GOS score of 1 (no problem) or 2 (minimal problem) for each item at the time of randomization with no significant difference between the two groups, and the lack of significance was sustained during the 24-week maintenance period. This result indicated that neither continuous nor on-demand therapy made any difference in symptoms from 8 weeks or later. From information in the daily charts, about 70–80% of patients in the continuous group achieved resolution of symptoms at the beginning of the maintenance period, while only 40–50% of patients in the on-demand group achieved resolution of symptoms during the initial period but this percentage gradually increased during the maintenance period. The between-group difference was large, especially in the early phase, such as before 8 weeks. The reason might be because of the difference in pill consumption between the two groups. Patients would be taken a PPI everyday as the initial therapy before the baseline, but in those who were allocated to the on-demand group, mean tablet usage was only 3 tablets per week, which means a near cessation of therapy. This would induce daily symptoms in the on-demand group from the first week until 17 weeks.
In fact, up to 8 weeks of initial therapy was approved by the health insurance in Japan and 4–8 weeks' duration provided sufficient efficacy to lead to mucosal healing by many studies regarding initial therapy for GERD [Citation15]. Although the 8 weeks of initial therapy was given by consensus, it might be short to control symptoms. Indeed, increases in relief of symptoms that paralleled decreasing tablet usage in the on-demand group were observed in this study.
What mechanism would contribute to the dissociation between endoscopic mucosal healing and persistent symptoms? Reflux symptoms are known to be generated by acid regurgitation in contact with impaired mucosa such as dilated intercellular spaces (DIS) and alterations in tight junctions [Citation16]. Our experimental study revealed that dispersion of tight junction was observed in macroscopically healed esophageal mucosa by PPI [Citation17]. The presence of these microscopic changes after the initial therapy might have led to residual symptoms in patients in the on-demand group who took only 3 tablets per week. This study also demonstrated that symptom improvement was achieved after 3 months in the on-demand group. In fact, an investigation of the reversibility of DIS in GERD by omeprazole therapy revealed that 3 and in some cases 6 months of therapy led to recovery in more than 90% of cases [Citation18]. This phenomenon provided a clue on how long a period is adequate for initial therapy of GERD and suggested that at least another 8 weeks of continuous therapy should be necessary to focus on sustaining a good QOL as measured by GOS. In other words, 3 tablets per week during the early phase of maintenance therapy should be an insufficient dose.
There are many kinds of QOL scores regarding GERD. In this study, we employed the QOLRAD-J since the heartburn version of QOLRAD is one of the best-characterized disease-specific instruments for use in patients with GERD [Citation19]. It was originally developed in English and has been validated in several languages including Japanese [Citation20]. A study employing this questionnaire after eradication of Helicobacter pylori demonstrated that QOLRAD-J scores improved significantly after 1 year in Japanese subjects [Citation21]. The validation study from Japan demonstrated that mean scores in each domain with GERD subjects were 5.4 for Emotional distress, 5.6 for Sleep disturbance, 5.2 for Food/drink problems, 6.2 for Physical/social functioning, and 5.3 for Vitality, while all except one of the healthy comparison subjects chose a score of 7 (none of the time) for all items [Citation20]. As shown in , mean scores for each domain were above 6 at baseline, and were higher than in the previous report of GERD subjects. Since baseline values in this study were already established after at least 8 weeks of treatment, this initial therapy would result in higher scores. During the 24-week evaluation, none of the items differed between groups. A study that assessed QOL during 6 months of maintenance therapy using the QOLRAD showed that the QOL was slightly different in favor of the continuous rather than the on-demand treatment arm at the end of the maintenance phase [Citation12]. However, findings of our study revealed that both therapies for maintenance treatment provided an equal effect on QOL.
Patients with NERD are common in Japan. The proportions of patients with NERD and RE were 58.6% and 41.4%, respectively, and many of the RE patients (87%) had a mild form (grades A and B) [Citation1]. In fact, we previously reported that 97.4% of RE was mild in our patient population [Citation22]. Therefore, this study was designed to include patients with both RE and NERD to reflect ordinary clinical settings in Japan. Only 6% of patients had grade C or D and 30% had grade M, which was similar to previous studies and would be representative of clinical settings.
Although functional impairment such as impaired lower esophageal sphincter pressure, motility abnormalities, and percentage time of acid regurgitation is milder than in RE [Citation23], heartburn severity and intensity have been reported to be either similar or high compared to RE [Citation24,25]. Furthermore, therapeutic response to PPI was lower for heartburn than for RE [Citation26–28]. In this maintenance study, the percentage of patients with grade M who achieved symptom relief was as low as 30–40% at baseline, and this trend continued and fluctuated during the entire period in both the continuous and on-demand arms (). A similar trend was observed in notations in the daily chart as shown in . Percentage of patients with symptom relief in the continuous group decreased after the 20th week and this percentage fluctuated during the entire period in both groups (). A recent meta-analysis revealed that in patients with NERD defined as heartburn, normal upper GI endoscopy, and positive pH study, the estimated complete symptom response rate after 4-week PPI therapy was comparable to the response rate in patients with RE; meanwhile studies in which NERD was defined as only heartburn or heartburn and normal upper GI endoscopy provided low response rate. The latter criteria likely included patients without reflux disease (e.g. functional heartburn) [Citation29]. The pH study was not performed in this study; therefore, certain number of patients with NERD in this study might not be reflux disease. This might be the reason of the low symptom-relief rate in NERD.
As far as we know, there is no study about maintenance therapy of NERD. Of course, precise diagnosis of NERD is important but to perform the pH study to all subjects suspecting NERD is distant. Since NERD is usually diagnosed by reflux symptoms without abnormal endoscopic findings in the esophagus in daily clinical settings [Citation30], the goal of treatment is symptom relief regardless continuous or on-demand therapy. Therefore, it stands to reason that on-demand therapy is suitable for NERD as maintenance therapy.
In patients with grade ≥ A, a significant number of patients achieved symptom relief at 8 weeks in the continuous arm, and 68–76% of patients in the continuous arm achieved symptom relief from baseline to the end of study, while symptom relief gradually increased in the on-demand arm from 51% to 76% (). In addition, the difference was clearly demonstrated in the daily chart. That is, more than 80% of patients in the continuous arm achieved symptom relief from the second week to the end of the study but symptom relief gradually increased in the on-demand group (). In addition to symptom relief, number of healed patients was significantly higher in continuous group than in on-demand group at 24 weeks upper GI endoscopy. These results demonstrated that continuous therapy provided not only reduced symptoms but also maintained mucosal healing.
Conclusions
Since NERD is defined by symptoms, as a result of the limited efficacy of continuous therapy, on-demand therapy would be sufficient as maintenance therapy in NERD patients. Regarding RE, continuous therapy would be recommended in terms of reduced symptoms and maintaining mucosal healing.
Declaration of interest: A Nagahara has served as a speaker for Astra Zeneca.
References
- Fujiwara Y, Arakawa T. Epidemiology and clinical characteristics of GERD in the Japanese population. J Gastroenterol 2009;44:518–34.
- Armstrong D. Systematic review: persistence and severity in gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2008;28:841–53.
- Nagahara A, Hojo M, Asaoka D, Watanabe S. Maintenance therapy of gastroesophageal reflux disease. Clin J Gastroenterol 2010;3:61–8.
- Tsuzuki T, Okada H, Kawahara Y, Takenaka R, Nasu J, Ishioka H, et al. Proton pump inhibitor step-down therapy for GERD: a multi-center study in Japan. World J Gastroenterol 2011;17:1480–7.
- Fujimoto K, Hongo M; Maintenance Study Group. Safety and efficacy of long-term maintenance therapy with oral dose of rabeprazole 10 mg once daily in Japanese patients with reflux esophagitis. Intern Med 2011;50:179–88.
- Fujimoto K, Hongo M; Maintenance Study Group. Risk factors for relapse of erosive GERD during long-term maintenance treatment with proton pump inhibitor: a prospective multicenter study in Japan. J Gastroenterol 2010;45:1193–200.
- Yoshida N, Kamada K, Tomatsuri N, Suzuki T, Takagi T, Ichikawa H, et al. Management of recurrence of symptoms of gastroesophageal reflux disease: synergistic effect of rebamipide with 15 mg lansoprazole. Dig Dis Sci 2010;55:3393–8.
- Jiang YX, Chen Y, Kong X, Tong YL, Xu SC. Maintenance treatment of mild gastroesophageal reflux disease with proton pump inhibitors taken on-demand: a meta-analysis. Hepatogastroenterology 2013;60:1077–82.
- Hongo M. Minimal changes in reflux esophagitis: red ones and white ones. J Gastroenterol 2006;41:95–9.
- Sakurai K, Nagahara A, Inoue K, Akiyama J, Mabe K, Suzuki J, et al. Efficacy of omeprazole, famotidine, mosapride and teprenone in patients with upper gastrointestinal symptoms: an omeprazole-controlled randomized study (J-FOCUS). BMC Gastroenterol 2012;12:42.
- Cibor D, Ciećko-Michalska I, Owczarek D, Szczepanek M. Optimal maintenance therapy in patients with non-erosive reflux disease reporting mild reflux symptoms—a pilot study. Adv Med Sci 2006;51:336–9.
- Morgan DG, O'Mahony MF, O'Mahony WF, Roy J, Camacho F, Dinniwell J, et al. Maintenance treatment of gastroesophageal reflux disease: an evaluation of continuous and on-demand therapy with rabeprazole 20 mg. Can J Gastroenterol 2007;21:820–6.
- Tepes B, Stabuc B, Kocijancic B, Ivanusa M. Maintenance therapy of gastroesophageal reflux disease patients with omeprazole. Hepatogastroenterology 2009;56:67–74.
- Tsai HH, Chapman R, Shepherd A, McKeith D, Anderson M, Vearer D, et al. Esomeprazole 20 mg on-demand is more acceptable to patients than continuous lansoprazole 15 mg in the long-term maintenance of endoscopy-negative gastro-oesophageal reflux patients: the COMMAND Study. Aliment Pharmacol Ther 2004;20:657–65.
- Khan M, Santana J, Donnellan C, Preston C, Moayyedi P. Medical treatments in the short term management of reflux oesophagitis. Cochrane Database Syst Rev 2007:CD003244.
- Bredenoord AJ. Mechanisms of reflux perception in gastroesophageal reflux disease: a review. Am J Gastroenterol 2012;107:8–15.
- Oguro M, Koike M, Ueno T, Asaoka D, Mori H, Nagahara A, et al. Dissociation and dispersion of claudin-3 from the tight junction could be one of the most sensitive indicators of reflux esophagitis in a rat model of the disease. J Gastroenterol 2011;46:629–38.
- Calabrese C, Bortolotti M, Fabbri A, Areni A, Cenacchi G, Scialpi C, et al. Reversibility of GERD ultrastructural alterations and relief of symptoms after omeprazole treatment. Am J Gastroenterol 2005;100:537–42.
- Wiklund IK, Junghard O, Grace E, Talley NJ, Kamm M, Veldhuyzen van Zanten S, et al. Quality of Life in Reflux and Dyspepsia patients. Psychometric documentation of a new disease-specific questionnaire (QOLRAD). Eur J Surg Suppl 1998:41–9.
- Hongo M, Kinoshita Y, Shimozuma K, Kumagai Y, Sawada M, Nii M. Psychometric validation of the Japanese translation of the Quality of Life in Reflux and Dyspepsia questionnaire in patients with heartburn. J Gastroenterol 2007;42:807–15.
- Hirata K, Suzuki H, Matsuzaki J, Masaoka T, Saito Y, Nishizawa T, et al. Improvement of reflux symptom related quality of life after Helicobacter pylori eradication therapy. J Clin Biochem Nutr 2013;52:172–8.
- Nagahara A, Hojo M, Asaoka D, Sasaki H, Oguro M, Mori H, et al. Clinical feature of asymptomatic reflux esophagitis in patients who underwent upper gastrointestinal endoscopy. J Gastroenterol Hepatol 2012;27:53–7.
- Fass R. Erosive esophagitis and nonerosive reflux disease (NERD): comparison of epidemiologic, physiologic, and therapeutic characteristics. J Clin Gastroenterol 2007;41:131–7.
- Miwa H, Minoo T, Hojo M, Yaginuma R, Nagahara A, Kawabe M, et al. Oesophageal hypersensitivity in Japanese patients with non-erosive gastro-oesophageal reflux diseases. Aliment Pharmacol Ther 2004;20:112–17.
- Nagahara A, Miwa H, Minoo T, Hojo M, Kawabe M, Osada T, et al. Increased esophageal sensitivity to acid and saline in patients with nonerosive gastro-esophageal reflux disease. J Clin Gastroenterol 2006;40:891–5.
- Miwa H, Inoue K, Ashida K, Kogawa T, Nagahara A, Yoshida S, et al. Japan TREND study group. Randomised clinical trial: efficacy of the addition of a prokinetic, mosapride citrate, to omeprazole in the treatment of patients with non-erosive reflux disease - a double-blind, placebo-controlled study. Aliment Pharmacol Ther 2011;33:323–32.
- Kinoshita Y, Ashida K, Hongo M; Japan Rabeprazole Study Group for NERD. Randomised clinical trial: a multicentre, double-blind, placebo-controlled study on the efficacy and safety of rabeprazole 5 mg or 10 mg once daily in patients with non-erosive reflux disease. Aliment Pharmacol Ther 2011;33:213–24.
- Miwa H, Sasaki M, Furuta T, Koike T, Habu Y, Ito M, et al. ACID-RELATED SYMPTOM (ARS) RESEARCH GROUP. Efficacy of rabeprazole on heartburn symptom resolution in patients with non-erosive and erosive gastro-oesophageal reflux disease: a multicenter study from Japan. Aliment Pharmacol Ther 2007;26:69–77.
- Weijenborg PW, Cremonini F, Smout AJ, Bredenoord AJ. PPI therapy is equally effective in well-defined non-erosive reflux disease and in reflux esophagitis: a meta-analysis. Neurogastroenterol Motil 2012;24:747–57, e350.
- Ronkainen J, Aro P, Storskrubb T, Johansson SE, Lind T, Bolling-Sternevald E, et al. High prevalence of gastroesophageal reflux symptoms and esophagitis with or without symptoms in the general adult Swedish population: a Kalixanda study report. Scand J Gastroenterol 2005;40:275–85.

