Abstract
Electron microscopy is a powerful tool for the assessment of complex lesions in nontumor renal pathology, however it is a time-consuming procedure. We evaluated a simple method to assess morphological signs of chronic rejection in renal allograft that seems to have prognostic significance.
Dear Sir
From the pioneering reports of Monga et al. [Citation1–3] most authors agree that basement membrane multilayering of intertubular capillaries in renal allografts is a significant clue to chronic alloimmune injury [Citation4]. Although some lamination of the interstitial capillary basement membrane has been reported in diverse native kidney injuries, such as leptospirosis [Citation5], cyclosporin toxicity, membranoproliferative glomerulonephritis, lupus nephritis, cryoglobulinemic nephritis and thrombotic microangiopathy [Citation6], large series have shown that six or more lamina densa layers surrounding the lumen of peritubular capillaries is, practically, pathognomonic of chronic alloimmune injury [Citation4,Citation6]. However, electron microscopy is a time-consuming procedure and some experts have reported that more than 3 layers of basement membrane in peritubular capillaries are very uncommon in settings other than chronic rejection [Citation4,Citation6,Citation7]. As multilayering of the basement membrane reflects a reparative response to repeated endothelial injuries [Citation8–10] and there are several reports relating submicroscopic capillary abnormalities with c4d deposition [Citation9,Citation11], it appears a reasonable assumption to consider that, in the absence of other causes of endothelial stress, this lesion could be accepted as sign of current or previous alloimmune reaction in the setting of kidney transplantation. Thus, we hypothesized that searching for three or more layers of basement membrane in at least two of three capillaries in the periglomerular interstice could be an easy and reasonable routine practice with diagnostic and prognostic implications. Since hepatitis C virus (HCV) has been related to kidney allograft chronic rejection [Citation12], we also evaluated the relationship between intertubular capillary abnormatities and HCV infection.
We reviewed 49 unselected samples corresponding to 49 kidney-transplanted patients who underwent a biopsy because of proteinuria or renal function derangement. In all cases, we examined one to three glomeruli with at least three mesangial areas and three intertubular capillaries in the adjacent interstitium. We divided our samples in two groups: (A) those that showed three or more layers of lamina densa covering at least the 50% of the contour of at least two of three peritubular capillaries (Figure 1) and (B) those that did not meet this criterion. The following parameters were analyzed in both groups: time after transplantation, association with transplant glomerulopathy, relationship with C4d deposition in peritubular capillaries and HCV infection, and graft outcome. Differences in time after transplantation between both groups were analyzed by Mann-Whitney U test, relationship of capillary lesions with transplant glomerulopathy, c4d deposition and HCV infection were studied using Fisher's exact test, and the outcome of the graft was evaluated by log-rank test on Kaplan Meyer survival curves.
summarizes our results. Group A included 16 patients and group B had 33 patients. In 6 cases (1 of group A and 5 of group B) glomerular submicroscopic structures could not be assessed because of global sclerosis. In group A the lapse between transplant and biopsy ranged from 5 to 167 months (mean 73 months), 5 of 15 patients showed transplant glomerulopathy, 5 of 11 presented c4d deposition in peritubular capillaries, 5 of 12 were infected with HCV, and 4 of the 16 patients returned to the dialysis program 0, 2, 15, and 16 months after the diagnosis of the lesion (follow-up: range, 0–74 months; mean, 13 months). In group B time from transplant to biopsy ranged from 0 to 198 months (mean, 38 months), none of 28 the samples in which glomeruli were suitable for examination showed transplant glomerulopathy, 6 of 27 samples exhibited c4d deposition in peritubular capillaries, 4 of 29 patients were infected with HCV, and at the end point of our study 1 patient had returned to dialysis 57 months after the biopsy (follow-up: range, 0–66 months; mean, 20 months).
FIGURE 1. (A) Periglomerular capillary showing 3–4 layers of lamina densa in the basement membrane (EM original 10000x). (B) Same sample of A. Detail of a glomerulus with no relevant abnormalities (EM, original 1500x).
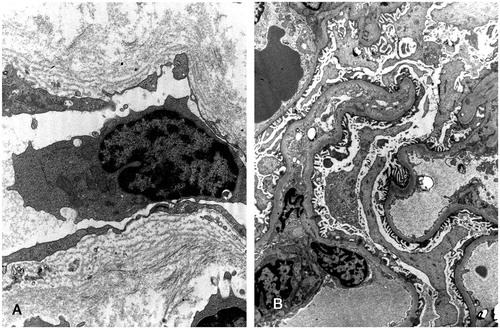
TABLE 1. Summary of the results.
From our series we deduce that moderate basement membrane multilayering shows a tendency to be associated with c4d deposits and HCV infection. On the other hand, intertubular capillary abnormalities show close relationship with transplant glomerulopathy and are a sign of relative poor graft outcome. Thus, three or more layers of lamina densa in intertubular capillaries of the periglomerular interstice seem to be a predictive lesion in kidney allografts and this lesion appears to be more sensitive to detect chronic rejection than glomerular abnormalities.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Monga G, Mazzuco G, Novara R, Reale L. Intertubular capillary changes in kidney allografts: an ultrastructural study in patients with transplant glomerulopathy. Ultrastruct Pathol 1990;14: 201–8
- Monga G, Mazucco G, Messina M, et al. Intertubular capillary changes in kidney allografts: a morphologic investigation on 61 renal specimens. Mod Pathol 1992;5: 125–30
- Mazzuco G, Motta M, Segoloni G, Monga G. Intertubular capillary changes in the cortex and medulla of transplanted kidney and their relationship with transplant glomerulopathy: an ultrastructural study of 12 transplantectomies. Ultrastruct Pathol 1994;18: 533–7
- Ivanyi B, Fahmy H, Brown H, et al. Peritubular capillaries in chronic renal allograft rejection: a quantitative ultrastructural study. Hum Pathol 2000;31: 1129–38
- Zollinger HU, Colombi A, Schiltknecht J. New clinical and ultrastructural aspects in leptospirosis icterohaemorrhagica (Weil's disease): a clinical, light- and electron microscopic study. Virchows Arch A Pathol Anat 1971;354: 336–48
- Drachenberg CB, Steinberger E, Hoehn-Saric E, et al. Specificity of intertubular capillary changes: comparative ultrastructural studies in renal allografts and native kidneys. Ultrastruct Pathol 1997;21: 227–33
- Chicano SL, Cornell LD, Selig MK, et al. Distinctive ultrastructural features of chronic allograft glomerulopathy: new formation of circumferential glomerular basement membrane. Lab Invest 2006;86: 260A–1A
- Lajoie G. Antibody-mediated rejection of human renal allografts: an electron microscopic study of peritubular capillaries. Ultrastruct Pathol 1997;21: 235–42
- Solez K, Colvin RB, Racusen LC, et al. Banff ‘05 meeting report: differential diagnosis of chronic allograft injury and elimination of chronic allograft nephropathy (‘CAN'). Am J Transplant 2007;7: 518–26
- Colvin RB, Nickeleit V. Renal transplant pathology. In: Jennette JC, Olson JL, Schwartz MM, Silva FG, eds. Heptinstall's Pathology of the Kidney, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2007:1347–490
- Regele H, Bohmig GA, Habicht A, et al. Capillary deposition of complement split product C4d in renal allograft is associated with basement membrane injury in peritubular capillaries: a contribution of humoral immunity to chronic allograft rejection. J Am Soc Nephrol 2002;13: 2371–80
- Morales JM, Bloom R, Roth D. Kidney transplantation in the patient with hepatitis C virus infection. Contrib Nephrol 2012;176: 77–86
