We read with great interest the recent article by Sadaka et al. [Citation1] describing their experience regarding the safety and usefulness of intracranial pressure monitor (ICPM) placement by neurointensivists in the management of severe traumatic brain injury (TBI). Their central message is that adequately trained neurointensivists working in a neurointensive care setting with neurosurgeon availability on site at a level I trauma centre in the US can insert ICPMs safely. We agree and, furthermore, have shown in a UK setting that trained general intensivists in district general hospitals without neurosurgeons on site can also safely insert ICPMs [Citation2].
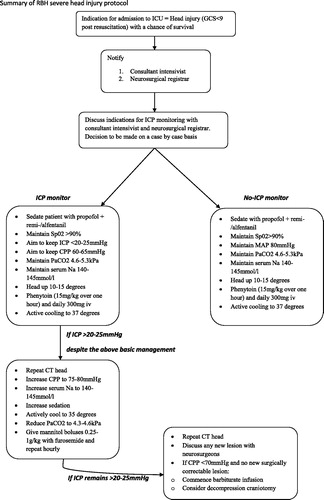
In our study, 28 out of 44 adult patients presenting with severe TBI underwent insertion of ICPM by six different consultant general intensivists. This was performed according to a local protocol () following discussion and advice from the regional neurosurgical unit. The primary indication for ICPM insertion was monitoring and prevention of secondary brain injury. In our series we experienced a 7% ICPM malfunction rate and no other complications. Specifically one ICPM was damaged externally and another would not give readings. Similarly Sadaka et al. [Citation1] did not report any clinically significant complications. ICH and intracranial infection are potentially devastating problems best managed by neurosurgeons. There is an old adage in medicine: ‘If you cannot deal with the complications, you should not perform the procedure’. Insertion of ICPM by neurointensivists exemplifies this. However, as with spinal abscess or haematoma after epidural insertion or pneumothorax or haemothorax after central line or chest drain insertion, dealing with the complications requires prompt recognition of signs and symptoms of deterioration and appropriate specialist referral rather than intensivist expertise at craniotomy, laminectomy or thoracotomy.
Despite our favourable results relating to successful ICPM insertion by non-neurosurgeons we still aim to transfer all patients with severe TBI to a specialist neurointensive care unit with on-site neurosurgery, regardless of their need for immediate neurosurgical intervention. Recent studies from the UK trauma audit and research network (TARN) group provide robust evidence for the benefits of management of severe TBI patients in specialist neuroscience centres. Fuller et al. [Citation3] conducted a retrospective cohort study using information from the TARN database to investigate the temporal trends in head injury management in the UK following the introduction of National Institute for Health and Care Excellence (NICE) guidelines on head injuries and the recommendation that severe TBI patients should be managed in specialist neuroscience centres. They showed a 12% reduction in adjusted log odds of death per annum since 2003, with a decrease in the number of patients managed entirely in non-specialist centres from 31% to 19% [Citation3]. In a similar study conducted by the same group it was found that severe TBI management in a non-specialist centre was associated with an 11% increase in crude mortality [Citation4]. These studies provide strong evidence for the drive to manage severe TBI in specialist neurosciences centres.
In reality there is often a disparity between supply and demand for acute neurosurgical beds in many countries, giving rise to the practical difficulty for managing such patients in general hospitals. We believe that it is only under such circumstances of limited resource that ICPM insertion by intensivists outside of a specialist neurointensive care setting should be considered. It is of utmost importance to discuss and receive advice from the regional neurosciences unit and ensure ongoing liaison with neurosurgeons.
The authors state that ‘timely treatment of patients with severe TBI is affected by the availability and commitment of neurosurgeons’ [1] and cite this as a reason for ICPM insertion by neurointensivists. We do believe this is an indication for such practice where neurosurgeons may not be available on site in district hospitals but should always be available at specialist neuroscience centres. Early CT brain should be performed alongside detailed history and examination. All relevant imaging should be transferred for neurosurgical review immediately. Only then can an informed decision regarding the need for ICPM insertion be made.
In the UK there is a government drive to promote and expand trauma services. We, therefore, hope there will be a reduced need to consider ICPM insertion by non-neurosurgeons. We hope that all patients with severe TBI will secure a bed at a specialist neuroscience centre to ensure they receive optimal care. If this includes ICPM insertion this should be performed in a centre where, should complications arise, they can be managed efficiently and effectively.
Unlike our US counterparts the neurointensivists here are not specifically trained to insert ICPMs as it is not part of the intensive care curriculum. Proper training is necessary for performing any procedure and the authors correctly mention the need for this in their conclusion. The UK model of workplace-based assessments to demonstrate competence may be useful in this regard [Citation5].
Important questions remain unanswered by this paper. For example, it would be interesting to know how many of the 38 patients went on to require neurosurgical interventions and why. What were the mortality and morbidity in this sub-set of patients? Were ICPM inserted only in patients who may have been deemed more likely to have a favourable outcome? How does this group of patients treated by neurointensivists compare to their local neurosurgical practice? Is there a protocol to follow for ICPM insertion by neurointensivists and did they discuss all cases with the neurosurgical team?
We commend the authors on reporting their experience on this important topic. However, we encourage caution in generalizing its results or popularizing such practice with a potential for reducing neurosurgeon involvement in the decision-making processes for such patients.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Sadaka F, Kasal J, Lakshmanan R, Palagiri A. Placement of intracranial pressure monitors by neurointensivists: case series and a systematic review. Brain injury 2013;27:600--604
- Rasul FT, Pereira EA, Waldmann C, Bojanic S. Effective management of severe traumatic brain injury in a district hospital. British Journal of Neurosurgery 2012;26:736–742
- Fuller G, Bouamra O, Woodford M, Jenks T, Patel H, Coats TJ, Oakley P, Mendelow AD, Pigott T, Hutchinson PJ, et al. Temporal trends in head injury outcomes from 2003 to 2009 in England and Wales. British Journal of Neurosurgery 2011;25:414–421
- Fuller G, Bouamra O, Woodford M, Jenks T, Patel H, Coats TJ, Oakley P, Mendelow AD, Pigott T, Hutchinson PJ, et al. The effect of specialist neurosciences care on outcome in adult severe head injury: a cohort study. Journal of Neurosurgical Anesthesiology 2011;23:198–205
- Pereira EA, Madder H, Millo J, Kearns CF. Neurosciences intensive care medicine in initial neurosurgical training. British Journal of Neurosurgery 2009;23:193–196