Abstract
Objectives: To identify patients’ beliefs or behaviors related to treatment adherence and to assess association between asthma control and adherence in Asian patients with asthma. Methods: We conducted a cross-sectional observational study of adult patients with asthma from specialist clinics in six Asian countries. Patients who were deemed by their treating physicians to require a maintenance treatment with an inhaler for at least 1 year were recruited. Patients completed a 12-item questionnaire related to health beliefs and behaviors, the 8-item Morisky Medication Adherence Scale (MMAS-8), the Asthma Control Test (ACT™), and the Standardized Asthma Quality of Life Questionnaire (AQLQ-S). Results: Of the 1054 patients recruited, 99% were current users of inhaled corticosteroids. The mean ACT score was 20.0 ± 4.5 and 64% had well-controlled asthma. The mean MMAS-8 score was 5.5 ± 2.0 and 53% were adherent. Adherence was significantly associated with patients’ understanding of the disease and inhaler techniques, and with patients’ acceptance of inhaler medicines in terms of benefits, safety, convenience, and cost (p < 0.01 for all). In multivariate analysis, three questions related to patients’ acceptance of inhaler medicines remained significantly associated with poor adherence, after adjusting for potential confounders: “I am not sure inhaler type medicines work well” (p = 0.001), “Taking medicines more than once a day is inconvenient” (p = 0.002), and “Sometimes I skip my inhaler to use it over a longer period” (p < 0.001). Conclusions: Our study showed that patients’ acceptance of the benefits, convenience and cost of inhaler medications have a significant impact on treatment adherence in the participating Asian countries.
Introduction
Asthma is a chronic inflammatory disease of the airways associated with increased airway responsiveness. Although effective treatments are available, the disease burden is still substantial [Citation1–4], often owing to poor adherence to prescribed asthma medications, particularly inhaled corticosteroids (ICS) [Citation5,Citation6].
Poor adherence to maintenance treatment such as ICS has been identified to be associated with higher rates of emergency room visits or hospitalization [Citation6] and poorer asthma control [Citation5]. Studies have shown that improved treatment adherence resulted in better clinical outcomes [Citation7–9]. However, improving adherence to medication remains a challenge in practice because factors contributing to poor adherence are diverse and multifaceted. Furthermore, not all factors are modifiable and therefore are not amenable to interventions.
Patients’ perceptions of the disease and treatment play an important, yet often overlooked role in adherence to treatment. Patients’ decisions to follow recommended treatment are influenced to a large extent by their beliefs and attitudes concerning the disease and treatment. For instance, patients often do not adhere to their long-term treatment regimen due to a misguided belief that it is not necessary to take their medications when they are asymptomatic [Citation10], or due to concerns with dependency or adverse effects associated with long-term treatment [Citation11]. They often adhere to their prescribed medications only when they believe that their treatment provides more benefit than harm [Citation12].
Understanding patients’ perceptions of the disease and treatment can increase the chances of achieving better treatment outcomes. Regular consultations with healthcare professionals provide opportunities for enhanced communication and support, and patient education, which can lead to improved adherence [Citation13]. In addition, efforts to identify barriers to adherence and enhance patients’ understanding of their disease and treatment can contribute to improved disease control and better clinical outcomes [Citation14].
Patients have diverse beliefs and attitudes concerning their disease and treatment, which are significantly influenced by their personal, cultural and socioeconomic environment. There is little information available regarding the influence of patient beliefs and behaviors on adherence in patients with asthma in Asia. We conducted an observational study of adult patients with asthma in six Asian countries. This report describes patients’ perceptions of their disease and treatment as well as the current status of asthma control and adherence in the participating countries in Asia. It also describes potentially modifiable beliefs and behaviors that are related to treatment non-adherence in the region.
Methods
Study design and population
This was a cross-sectional observational study of patients with asthma who were recruited by pulmonologists, respiratory physicians or allergists in China, Korea, Malaysia, Taiwan, Thailand and Vietnam between January and June 2012. Patients were at least 18 years of age, with an established diagnosis of asthma [Citation15], and were deemed by their treating physicians to require a maintenance treatment with either ICS alone or combined with long-acting beta agonists (LABA) for at least 1 year. Patients with other clinically significant respiratory diseases or with a main diagnosis of chronic obstructive pulmonary disease (COPD) were excluded.
Ethics approval of the study documents was obtained in all participating centers prior to the start of the study (Appendix). Informed consent was obtained from all patients prior to their participation in the study. The study was conducted in accordance with the International Conference on Harmonization (ICH) Good Clinical Practice (GCP) guidelines, all applicable regulatory requirements, and the ethical principles that are outlined in the Declaration of Helsinki.
Study assessments
During the single study visit, demographic data, exacerbation history in the previous year, current treatment information and medical history including comorbidities were collected. Relevant laboratory findings within the past 1 year were also collected, if available. Asthma exacerbation was defined as deterioration in asthma requiring treatment with systemic corticosteroids, or an increase from a stable maintenance dose, for at least 3 days. Courses of corticosteroids separated by 1 week or more were treated as separate exacerbations. Reversibility was defined as an increase in post-bronchodilator forced expiratory volume in 1 s (FEV1) by 12% or more, and at least 200 ml [Citation16]. Patients completed a 12-item questionnaire pertaining to health beliefs and behaviors, the 8-item Morisky Medication Adherence Scale (MMAS-8), the Asthma Control Test (ACT™), and the Standardized Asthma Quality of Life Questionnaire (AQLQ-S).
Questionnaires
Validated local language version of the questionnaires was used in each country. The questionnaires were administered by trained study personnel. If patients had difficulty in filling out the questionnaires, study personnel helped them to understand the questions. Study personnel reviewed the questionnaires for completeness.
The 12-item questionnaire was developed based on patient interviews and in-depth discussion with regional clinicians experienced in the management of Asian patients with asthma. It comprises questions pertaining to patients’ beliefs and behaviors, which were regarded as relevant to treatment adherence. Responses were scored on a 5-point scale, ranging from “strongly disagree” to “strongly agree”. The MMAS-8 assesses medication-adherence behaviors related to the use of inhalers. An MMAS-8 score of 8 indicates “high adherence”, 6 to <8 indicates “medium adherence”, and <6 indicates “low adherence” [Citation17].
The ACT assesses the level of asthma control during the previous 4 weeks. An ACT score of ≥20 indicates “well-controlled” asthma, 16 to 19 indicates “not well-controlled” asthma, and ≤15 indicates “very poorly controlled” asthma [Citation18]. The AQLQ-S assesses the quality of life (QoL) during the previous 2 weeks. An AQLQ score of 1 to <3 indicates “severe impairment”, a score of 3 to <6 indicates “moderate or some impairment”, and a score of 6 to 7 indicates “minimal or no impairment” [Citation19].
Statistical analysis
Patient demographic and clinical characteristics, treatment information, and beliefs and behaviors were summarized for the overall study population using descriptive statistics. AQLQ-S score and clinical events were also summarized by asthma control level. In addition, asthma control levels and patient beliefs or behaviors were summarized by adherence level. Comparisons between groups used the Chi-square test, Fisher’s exact test or one-way ANOVA, where appropriate. Univariate and multivariate Poisson regression analyses with robust estimation were performed to estimate the associations between patient beliefs or behaviors and treatment adherence. Variables related to demographic and clinical characteristics, medical history, treatment, health beliefs and behaviors, asthma control, and QoL, which had a p value of <0.2 in the univariate analyses were entered into a multivariate backward selection model. Variables with a p value of ≤0.1 were retained in the model. All statistical analyses were performed using SPSS (Version 20; Chicago, IL, USA).
Results
Patient characteristics and medical history
Among 1054 patients who completed the questionnaires, 61.8% were female and the mean age was 53.0 ± 14.4 years. The mean duration of asthma since diagnosis was 11.4 ± 11.2 years and 82.3% had adult-onset asthma. Eighty-one percent had at least one comorbidity, and the mean ACT score, AQLQ score and MMAS-8 score were 20.0 ± 4.5, 5.28 ± 1.15 and 5.53 ± 2.03, respectively. Over two-thirds of the patients (64.4%) had well-controlled asthma. Fifty-three percent had high or medium medication adherence. Other demographic and clinical characteristics are summarized in .
Table 1. Demographic and clinical characteristics
A substantial proportion of patients reported asthma exacerbations (35.1%), hospitalizations or emergency room visits (15.6%), or lost days of work (13.4%) due to asthma exacerbations in the previous year. The median number of scheduled clinic visits in the previous year was 5.0 (0.0–24.0), with 75.4% of the patients having four or more scheduled visits. Ninety-nine percent of the patients were current users of ICS (). A quarter of the patients (24.9%) used a rescue medication at least twice per week in the previous 4 weeks ().
Patient perceptions regarding disease and treatment
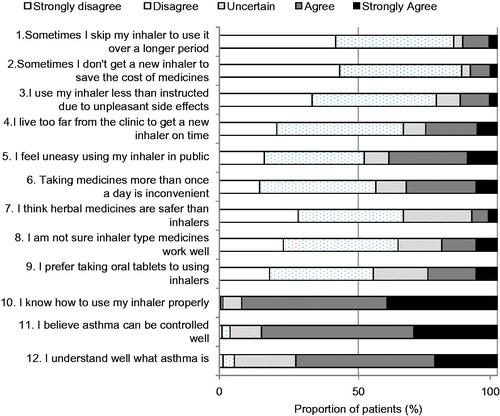
Within the study population, 72.5% reported that they understood the disease well, 84.8% believed that the disease can be controlled well, and 92.1% knew how to use the inhaler (). The majority did not reduce inhaler use due to unpleasant side effects (78.2%) or to reduce costs (84.2–87.2%). However, a substantial proportion of patients were uncertain about the effectiveness of inhaler medicines (35.7%), felt that taking medicines more often than once-daily was inconvenient (32.8%), or felt uneasy about using an inhaler in public (39.0%). Over one-quarter felt that it was inconvenient to get a new inhaler on time due to travel distance (25.8%), or showed a preference for oral medicines over inhaler medicines (25.0%).
Relationship between asthma control, QoL, clinical events, and adherence
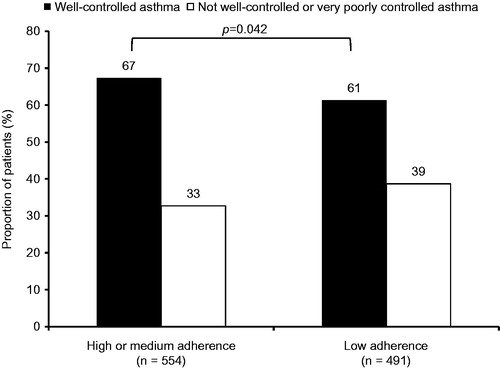
Better asthma control was significantly associated with better QoL (p < 0.001). The mean AQLQ-S score was 5.83 ± 0.81 in the “well-controlled” group, 4.73 ± 0.80 in the “not well-controlled” group and 3.71 ± 0.98 in the “very poorly controlled” group (). Patients with better asthma control were less likely to have asthma exacerbations (25.8%, 44.1% and 62.2% respectively for worsening levels of asthma control), hospitalizations or emergency room visits (8.4%, 21.3% and 37.8% respectively) (p < 0.001 for all). They were also less likely to have lost days of work (6.6%, 16.3% and 37.9% respectively) (p < 0.001) (). Treatment adherence showed a marginally significant association with asthma control (p = 0.042) (). Patients with high or medium adherence were more likely to have well-controlled asthma than those with low adherence (67.3% vs. 61.3%).
Table 2. Impact of asthma control on quality of life and clinical events
Impact of patient perceptions on adherence
There was a sizable difference in beliefs and behaviors held by high or medium adherent patients and low adherent patients. Adherence was significantly associated with patients’ self- reported understanding of the disease (Q11–12) and inhaler techniques (Q10), and with patients’ acceptance of inhaler medicines in terms of benefits (Q8, 9), safety (Q3, 7), convenience (Q4–6), and cost (Q1, 2) (p < 0.01 for all) (). Compared with patients with high or medium adherence, those with low adherence were less likely to report that they understood the disease well (79.2% vs. 65.2%) or that they knew how well inhaler medicines work (73.7% vs. 53.9%). They were more likely to believe that herbal medicines are safer than inhalers (12.5%) compared with those with high or medium adherence (6.1%). More patients with low adherence indicated that they used inhalers less often than instructed due to side effects (20.0% vs. 7.2%) compared with those with high or medium adherence. Patients with low adherence were also more likely to prefer oral tablets to inhalers (31.2% vs. 18.8%) or to prefer once-daily dosing (44.5% vs. 22.2%) than patients with high or medium adherence. They were also more likely to report feeling uneasy about using an inhaler in public (50.1% vs. 28.7%) or that it was inconvenient to get a new inhaler (35.5% vs. 17.4%), or to skip inhaler use to reduce costs (22.0% vs. 3.6%) ().
Figure 3. Comparison of patients’ perceptions among high or medium adherent patients and low adherent patients
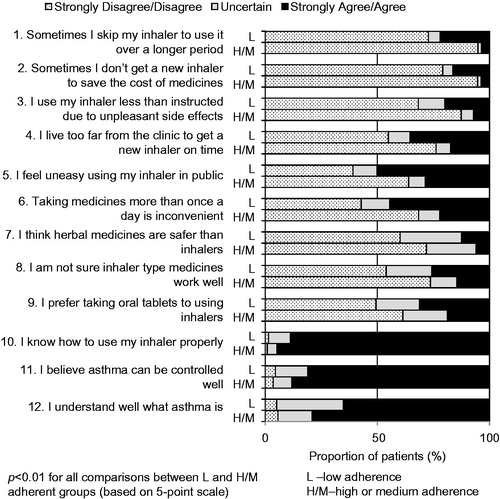
In multivariate analysis, three questions related to patients’ acceptance of inhalers in terms of benefits, convenience, and cost remained significantly associated with poor adherence, after adjusting for potential confounders: “I am not sure inhaler type medicines work well” (p = 0.001), “Taking medicines more than once a day is inconvenient” (p = 0.002) and “Sometimes I skip my inhaler to use it over a longer period” (p < 0.001) (). Patients who strongly agreed that they were not sure whether inhaler medicines work well were at significantly higher risk of poor adherence than those who disagreed (RR 0.69; CI 0.54–0.87) or strongly disagreed (RR 0.65; CI 0.50–0.83). There was a non-significant trend of higher risk of poor adherence in patients who strongly agreed that taking medicines more than once a day was inconvenient, compared with those who disagreed (RR 0.86; 95% CI 0.69–1.08) or strongly disagreed (RR 0.80; 95% CI 0.60–1.06). Patients who strongly agreed that they sometimes skipped their inhaler to use it over a longer period were at significantly higher risk of poor adherence than those who disagreed (RR 0.51; 95% CI 0.40–0.64) or strongly disagreed (RR 0.50; 95% CI 0.40–0.63). Other significant factors are listed in .
Table 3. Results of multivariate analysis for significant factors affecting adherence
Discussion
This study examined patients’ perceptions of asthma management as well as the current status of asthma control and adherence in the participating Asian countries. It also identified three potentially modifiable patient beliefs and behaviors that were related to non-adherence to ICS in the region.
Our study showed that the study population generally had a good understanding of the disease and the necessity of maintenance treatment. The majority of the patients reported that they understood the disease, knew how to use inhalers properly, and did not reduce inhaler use due to unpleasant side effects or to reduce costs (73–92%). However, a substantial proportion of the patients (25–39%) were uncertain about the effectiveness of inhaler medicines, felt uneasy or that it was inconvenient using an inhaler, or preferred oral medicines. These findings highlight the need to enhance patients’ acceptance of inhalers.
Previous studies of Asian and non-Asian asthma patients showed that asthma control was not optimal in a large proportion of patients (44–57% had not well-controlled or poorly controlled asthma) and a high disease burden exists [Citation1,Citation2,Citation4,Citation20]. There was high usage of rescue medications (51–72%) and a substantial proportion of patients needed urgent care (hospitalization or emergency room visits) (17–40%) [Citation1,Citation2,Citation4,Citation20]. Compared with these previous reports, our study showed better asthma management, with a higher proportion of patients who had well-controlled asthma (64%) and lower use of urgent care (16%). The better asthma management observed in our study could be related to the study setting from which the study population was recruited. In our study, patients were recruited from specialist clinics where they received better medical attention, whereas in the other surveys, patients were recruited from the community.
Although asthma was generally well managed in the study population, a substantial burden persists. Of note, only 61.7% of patients did not use a rescue inhaler in the previous 4 weeks despite high usage of ICS and 14.8% used a rescue inhaler at least once per day during the last 4 weeks. In addition, adherence to treatment was poor among patients, with nearly half (47%) having low adherence. This is considerably higher than that reported in a European community-based survey (non-adherent or highly non-adherent: 24%) [Citation1]. These findings urge clinicians to recognize that there is considerable room for improvement in asthma care and treatment adherence in the participating countries.
Our results further extend the evidence that asthma control is significantly associated with clinical outcomes, work productivity, QoL, and treatment adherence level [Citation5–8]. Patients with better asthma control were less likely to have asthma exacerbations, hospitalizations or emergency room visits, and lost days of work than those with poorer control. They also had better QoL. Patients with higher adherence were more likely to have well-controlled asthma than those with lower adherence. These findings emphasize the need to improve adherence in this region to achieve better asthma control and consequently improve clinical outcomes, work productivity and QoL of patients.
Our study showed that patients’ acceptance of the benefits, convenience and cost of inhalers were important predictors of medication adherence in the study population. Similarly, previous studies in Western populations reported that adherence was related to patients’ perceptions of the necessity and benefits of ICS [Citation11,Citation12]. However, additional factors, such as friends’ or family’s opinions on patients’ medications and patients’ concerns about the safety of ICS treatment, have also been identified to be related to adherence [Citation12]. The use of different questionnaires which captured various aspects of patients’ perceptions of asthma management might have partly contributed to the differences in factors identified. In this study, we observed patients’ preference for oral tablets and patients’ perceptions that herbal medicines are safer than inhalers were related to lower adherence. These may originate from the traditional use of herbal medicines via an oral route in Asian countries. Therefore, identifying patients’ beliefs and behaviors related to specific populations or geographical regions will be the first step to improve adherence.
We observed that a substantial proportion of patients with low adherence were unsure of the effectiveness of inhaler medications, felt that taking medicines more than once a day was inconvenient, or skipped inhaler use to reduce costs. This indicates the need to take coordinated efforts to enhance patients’ understanding of their treatment as well as to provide more convenient dosing options and more affordable medications. Such efforts will help to promote better adherence in Asian patients with asthma.
Our findings need to be interpreted in light of the study limitations. First, data on medication adherence, asthma control, and QoL were self-reported and were collected at a single visit. Therefore, the estimates may be subjected to recall bias. Objective measurements as well as longitudinal follow up of these outcomes may provide more reliable estimates. In addition, an assessment of health literacy to ensure that patients could read and clearly understand the questionnaires would have been helpful in improving the accuracy of estimation. Nonetheless, in this study, the consistent administration of questionnaires by study personnel who received training in questionnaire administration reduced bias to some extent. Next, our study recruited patients from specialist clinics and the majority of them were receiving maintenance treatment. Consequently, the level of asthma control may be overestimated. Further, we observed a marginally significant association between asthma control and adherence. A more significant association could potentially be observed in subgroup analyses comparing asthma control of high adherent patients with low adherent patients. However, due to the relatively small sample size of the high adherent group (n = 198), we were unable to perform subgroup analyses among the three groups—high, medium, and low adherence. In addition, it was not possible to study the impact of ICS on treatment adherence, since nearly all the patients were current ICS users. Finally, the proportion of patients with available data for laboratory tests was small. Hence, we were unable to evaluate the impact of certain physical conditions, such as lung function, on treatment adherence. Future studies in a larger cohort may allow these subgroups to be studied.
Conclusions
Our study shows that treatment adherence is poor and that a significant disease burden persists in the region. This indicates considerable room for improvement in asthma management. Our study shows that patients’ acceptance of the benefits, convenience and cost of inhaler medications have a significant impact on treatment adherence in the participating Asian countries. These factors should be considered when devising strategies to improve adherence in the region.
Declaration of interest
Dr. W. Boonsawat has received speaker’s honoraria from AstraZeneca, GlaxoSmithKline, MSD, Nycomed, Otsuka, and Boehringer Ingelheim. Dr. V. N. Nguyen has received speaker’s honoraria and research funds from GlaxoSmithKline, AstraZeneca, Sanofi Aventis and Pfizer. Dr. C. Wang has received honoraria for consulting and presentation, and research funds from GlaxoSmithKline, AstraZeneca and Boehringer Ingelheim. Dr. N. Kwon is an employee of GlaxoSmithKline and owns stocks in GlaxoSmithKline. The other authors declare they have no competing interests. The study was funded by GlaxoSmithKline. Statistical support was provided by Dr Liang Shen and editorial support by Hui Hwa Choo of Research2Trials Clinical Solutions Pte Ltd and was funded by GlaxoSmithKline.
Copyright
Permission to use the MMAS-8 was granted by Dr. Donald E. Morisky (University of California, Los Angeles). ACT is a trademark of QualityMetric (Lincoln, RI). Permission to use the AQLQ-S was granted by Professor Elizabeth F. Juniper (McMaster University, Canada).
Supplementary Material
Download PDF (138.8 KB)Acknowledgements
The authors thank all the investigators who contributed to the study.
References
- Demoly P, Gueron B, Annunziata K, Adamek L, Walters RD. Update on asthma control in five European countries: results of a 2008 survey. Eur Respir Rev 2010;19:150–157
- Lai CK, Ko FW, Bhome A, De Guia FS, Wong GW, Zainudin BM, Nang AN, et al. Relationship between asthma control status, the Asthma Control Test and urgent health-care utilization in Asia. Respirology 2011;16:688–697
- Nathan RA, Meltzer EO, Blaiss MS, Murphy KR, Doherty DE, Stoloff SW. Comparison of the Asthma in America and Asthma Insight and Management surveys: did asthma burden and care improve in the United States between 1998 and 2009? Allergy Asthma Proc 2012;33:65–76
- Thompson PJ, Salvi S, Lin J, Cho YJ, Eng P, Abdul Manap R, Boonsawat W, et al. Insights, attitudes, and perceptions about asthma and its treatment: findings from a multinational survey of patients from 8 Asia-Pacific countries and Hong Kong. Respirology 2013;18:957–967
- Clatworthy J, Price D, Ryan D, Haughney J, Horne R. The value of self-report assessment of adherence, rhinitis and smoking in relation to asthma control. Prim Care Respir J 2009;18:300–305
- Rust G, Zhang S, Reynolds J. Inhaled corticosteroid adherence and emergency department utilization among Medicaid-enrolled children with asthma. J Asthma 2013;50:769–775
- Dalcin Pde T, Grutcki DM, Laporte PP, Lima PB, Viana VP, Konzen GL, Menegotto SM, et al. Impact of a short-term educational intervention on adherence to asthma treatment and on asthma control. J Bras Pneumol 2011;37:19–27
- Gamble J, Stevenson M, Heaney LG. A study of a multi-level intervention to improve non-adherence in difficult to control asthma. Respir Med 2011;105:1308–1315
- Small M, Anderson P, Vickers A, Kay S, Fermer S. Importance of inhaler-device satisfaction in asthma treatment: real-world observations of physician-observed compliance and clinical/patient-reported outcomes. Adv Ther 2011;28:202–212
- Halm EA, Mora P, Leventhal H. No symptoms, no asthma: the acute episodic disease belief is associated with poor self-management among inner-city adults with persistent asthma. Chest 2006;129:573–580
- Menckeberg TT, Bouvy ML, Bracke M, Kaptein AA, Leufkens HG, Raaijmakers JA, Horne R. Beliefs about medicines predict refill adherence to inhaled corticosteroids. J Psychosom Res 2008;64:47–54
- Foster JM, Smith L, Bosnic-Anticevich SZ, Usherwood T, Sawyer SM, Rand CS, Reddel HK. Identifying patient-specific beliefs and behaviours for conversations about adherence in asthma. Intern Med J 2012;42:e136–e144
- Corsico AG, Cazzoletti L, de Marco R, Janson C, Jarvis D, Zoia MC, Bugiani M, et al. Factors affecting adherence to asthma treatment in an international cohort of young and middle-aged adults. Respir Med 2007;101:1363–1367
- Park J, Jackson J, Skinner E, Ranghell K, Saiers J, Cherney B. Impact of an adherence intervention program on medication adherence barriers, asthma control, and productivity/daily activities in patients with asthma. J Asthma 2010;47:1072–1077
- National Institute of Health (NIH). Guidelines for the Diagnosis and Management of Asthma – Expert Panel Report 3, 2007. US Department of Health and Human Services, Bethesda, MD; NIH Publication No. 07-4051
- American Thoracic Society. Lung function testing: selection of reference values and interpretative strategies. American Thoracic Society. Am Rev Respir Dis 1991;144:1202–1218
- Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich) 2008;10:348–354
- Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P, Murray JJ, Pendergraft TB. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol 2004;113:59–65
- Juniper EF, Buist AS, Cox FM, Ferrie PJ, King DR. Validation of a standardized version of the Asthma Quality of Life Questionnaire. Chest 1999;115:1265–1270
- Holt S, Sheahan D, Mackey B, Jacobsen C. Use of Asthma Control Test (ACT) affects New Zealand primary care doctors' perception of asthma control. N Z Med J 2011;124:99–101