Abstract
Objective. Respiratory tract infections are the most common indication for antibiotic prescribing in primary care. The value of clinical findings in lower respiratory tract infection (LRTI) is known to be overrated. This study aimed to determine the independent influence of a point of care test (POCT) for C-reactive protein (CRP) on the prescription of antibiotics in patients with acute cough or symptoms suggestive of LRTI, and how symptoms and chest findings influence the decision to prescribe when the test is and is not used. Design. Prospective observational study of presentation and management of acute cough/LRTI in adults. Setting. Primary care research networks in Norway, Sweden, and Wales. Subjects. Adult patients contacting their GP with symptoms of acute cough/LRTI. Main outcome measures. Predictors of antibiotic prescribing were evaluated in those tested and those not tested with a POCT for CRP using logistic regression and receiver operating characteristic (ROC) curve analysis. Results. A total of 803 patients were recruited in the three networks. Among the 372 patients tested with a POCT for CRP, the CRP value was the strongest independent predictor of antibiotic prescribing, with an odds ratio (OR) of CRP ≥ 50 mg/L of 98.1. Crackles on auscultation and a patient preference for antibiotics perceived by the GP were the strongest predictors of antibiotic prescribing when the CRP test was not used. Conclusions. The CRP result is a major influence in the decision whether or not to prescribe antibiotics for acute cough. Clinicians attach less weight to discoloured sputum and abnormal lung sounds when a CRP value is available. CRP testing could prevent undue reliance on clinical features that poorly predict benefit from antibiotic treatment.
Acute cough is one of the most common indications for antibiotic prescribing in primary care. The prognostic and diagnostic value of clinical findings are often overestimated.
When deciding on antibiotic prescribing, GPs place less emphasis on discoloured sputum and chest auscultation findings when they use CRP POCT.
CRP testing could prevent undue reliance on clinical features that poorly predict pneumonia and benefit from antibiotics.
Antibiotic resistance is a growing problem worldwide [Citation1], with a consistent association between the amount of antibiotics used and the frequency of resistant bacteria [Citation2]. Respiratory tract infections account for the large proportion of antibiotics prescribed in primary care [Citation2]. The proportion of patients presenting with acute cough in primary care who were prescribed antibiotics varied from 28% to 92% in a 13-country study, the overall study within which this sub-analysis is located [Citation3].
Diagnostic uncertainty and an over-reliance on abnormal lung sounds on auscultation have been identified as reasons for over-prescribing of antibiotics in patients with acute cough [Citation3,Citation4], and better ways of identifying those who might benefit from antibiotic treatment have been called for [Citation5,Citation6]. Point of care testing (POCT) for C-reactive protein (CRP) was introduced into community clinical practice in the early 1990s. Studies showed that the CRP test was a better predictor of pneumonia than other clinical findings [Citation7] and it was rapidly adopted into routine clinical practice in Scandinavia. In 2005, 42% of Swedish patients consulting a GP for an airway infection were tested for CRP [Citation8]. Antibiotic prescribing increases with increasing CRP levels [Citation9,Citation10] in patients with acute bronchitis and the common cold. This association could be explained by a co-variance between the CRP value and clinical predictors of antibiotic prescribing, so the direct relationship between the CRP test result and antibiotic prescribing remains unclear.
We therefore aimed to use data from the GRACE study of the presentation, management, and outcome of patients with acute cough [Citation3] to explore the influence of CRP test results on GPs’ decision to prescribe antibiotics for acute cough, taking other established predictors for antibiotic prescribing into account. In addition, we aimed to explore whether GPs’ reliance on abnormal lung sounds on auscultation and other clinical findings differed according to whether or not CRP testing was performed.
Material and methods
Networks and patients
GPs and patients from three out of 14 primary care research networks from 13 European countries in the GRACE Network of Excellence [Citation3] took part in the study. The networks from Tromsø, Norway, and Jönköping, Sweden, were chosen, due to the use of CRP testing in these countries, while Cardiff, Wales, was included as a network not using the CRP test, with similar patient characteristics to the Scandinavian networks [Citation3]. Participating GPs were asked to recruit consecutively eligible patients from October–November 2006, and January–March 2007. Patients were eligible when >18 years of age, the consultation was the first in this illness episode, and it was less than 28 days since onset of symptoms, and when immunocompetent.
Data collection
Clinicians recorded aspects of patients’ history, symptoms, comorbidities, clinical findings, and their management including antibiotic prescription on a case report form (CRF). GPs indicated the presence or absence of symptoms and then rated whether each of the symptoms constituted “no problem”, “mild problem”, “moderate problem”, or a “severe problem” for the patient. The colour of any sputum produced was noted. The GPs recorded chest examination findings, and the patient's body temperature was recorded using a disposable TempaDot strip provided in each individual patient study pack.
The clinicians were also asked to agree or not with the statement “the patient wanted me to prescribe antibiotics for them”, which was called “perceived patient preference for antibiotics”. Use of a POCT for CRP was registered on the CRF, and the results were recorded. The CRP test kits used were NycoCard® CRP Single Test, Axis-Shield PoC AS, Oslo, Norway, and QuickRead® CRP, Orion Diagnostica, Espoo, Finland. The measurement range was 8–160 mg/L for the QuickRead® system, and 8–200 for the NycoCard® system.
Data management
All CRF data were entered via a remote secure data entry portal onto the GRACE online site, which was compliant with regulatory guidelines. CRP-related data registered in Tromsø and Jönköping were managed by the national network facilitators.
Analysis
The study population was divided into three groups, the Scandinavian patients tested for CRP, the Scandinavian patients not tested for CRP, and the Welsh patients, none of whom were tested for CRP. Symptoms rated as “no problem” or “minor problem” were registered as not present, while symptoms rated as “moderate problem” or “severe problem” were registered as present. Perceived patient preference for antibiotic treatment was grouped as “present”, when the GP agreed, or strongly agreed, with the statement “the patient wanted me to prescribe antibiotics for him/her”, while GP responses that “the patient did not want me to prescribe antibiotics for him/her” or “not applicable”, were grouped as “not present”. We merged comorbidity into “any comorbidity” and the four categories of abnormal lung sounds () to “any abnormal lung sound”. The CRP value was divided into three groups: CRP < 20 mg/L, between 20 mg/L and 50 mg/L, and ≥ 50 mg/L.
Table I. Prevalence of patient characteristics, symptoms, and findings in 803 primary care patients with acute cough categorized by CRP testing and network.
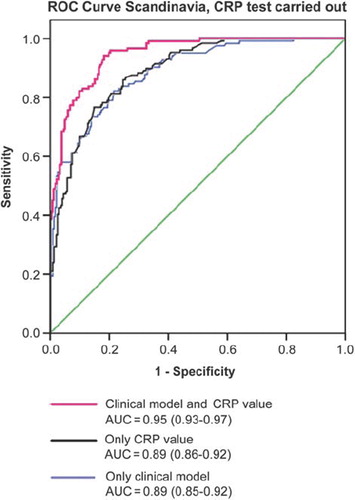
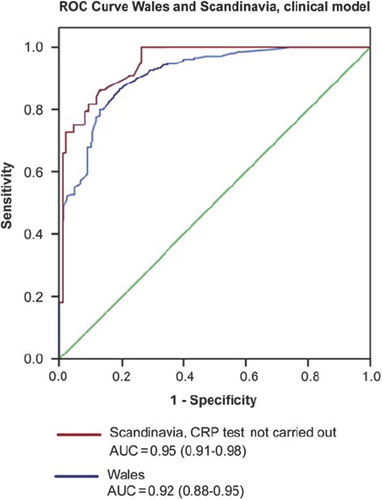
Percentages of antibiotic prescribing and corresponding 95% confidence intervals were calculated by comorbidity, symptoms, and findings. Variables significantly associated with antibiotic prescribing at a 10% level in the univariate analyses were entered into a two-level logistic regression, with the patients as first level and GPs as second level, and with antibiotic prescribing as the independent variable. The predictive value of a model including the clinical predictors that attained statistical significance (at a 10% level) for prescribing antibiotics was evaluated in the three subgroups using receiver operating characteristics (ROC) curve analyses. In the CRP tested subgroup, ROC curves evaluated the predictive value of the CRP results and of the clinical model together with the CRP results. Probabilities of prescribing by CRP as a continuous variable were used in these analyses. Statistical significances of differences in area under curve (AUC) in the ROC analyses were evaluated by calculating 95% confidence intervals. SPSS 16.0 and the R statistical programming language and environment were used in the statistical analyses.
Results
A total of 803 patients were recruited in the three networks. The CRP test was used in all 23 practices in the Norwegian and Swedish networks, for 33% to 100% of patients in each practice. Of the 81 physicians recruiting patients in the Scandinavian networks, nine did not use the CRP test, but these GPs recruited only 15 of a total of 503 patients. Some 73% of the Scandinavian patients were tested with the CRP-test, 91% in Norway and 67% in Sweden. In Wales, the test was not used as a near-patient test.
The three groups were similar as regards age, gender, and symptoms (see ). Fewer comorbidities and abnormal lung sounds were recorded in the Scandinavian patients who were not tested for CRP compared with the two other groups. “Perceived patient preference for antibiotics” was recorded less frequently in the Scandinavian subgroups (16% in the group tested for CRP and 18% in the group not tested for CRP) than in Wales (55%).
The GPs in Wales prescribed antibiotics more frequently than their Scandinavian colleagues, whereas prescription rates were similar in the two Scandinavian networks (). In the Scandinavian patients not tested for CRP, 64% of patients with previous lung disease were prescribed an antibiotic, compared with 46% in the subgroup who were tested for CRP. This difference did not reach statistical significance. Similar prescription rates attached to symptoms were found in the two Scandinavian subgroups.
Table II. Frequency of antibiotics prescribed by patient characteristics, symptoms, and findings in 803 primary care patients with acute cough categorized by PoC CRP testing and network.
Chest findings were more strongly associated with antibiotic prescriptions in the Scandinavian patients not tested with the CRP test compared with tested patients (73% vs. 55%, p < 0.05). In Wales 92% of the patients with abnormal lung sounds were prescribed antibiotics.
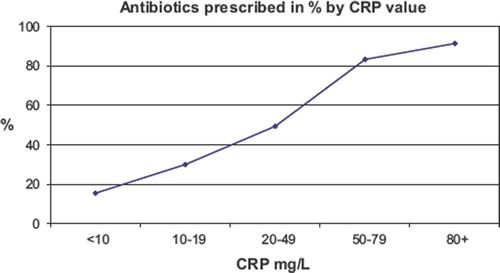
The CRP value was strongly associated with antibiotic prescribing in those tested for CRP ().
Figure 1. Frequency of prescribing antibiotics by CRP value in 372 Scandinavian patients with acute cough.
Perceived patient preference for antibiotics was associated with antibiotic prescribing in approximately 85% in all three countries (see ).
In the multivariate logistic regression, gender, age, and previous illnesses did not significantly predict antibiotic prescribing (). Discoloured sputum was the only symptom that was statistically significantly associated with antibiotic prescribing (with an OR of 3.3) in the Welsh subgroup. Crackles on chest auscultation were the strongest independent predictor of antibiotic prescribing in all three groups with ORs of 37.7, 9.5, and 17.2 in the Welsh patients, and the Scandinavian patients tested and not tested for CRP, respectively.
Table III. Predictive value (odds ratio) for prescribing antibiotics of patients’ characteristics, symptoms, and findings determined by multivariate logistic regression in 803 primary care patients with acute cough categorized by PoC CRP testing and network.
In the group where CRP testing was done, the CRP value was the strongest predictor of antibiotic prescribing. A CRP value ≥ 20 and < 50 had an OR of 8.9, while a CRP value ≥ 50 mg/L had an OR of 98.1, when compared with values < 20mg/L.
Perceived patient preference for antibiotics was a strong predictor of antibiotic prescribing in all three groups. In those tested for CRP, it was the second strongest predictor with an OR of 22.6. In the Welsh group it was also the second strongest predictor after crackles, with an OR of 6.2, and it was the strongest predictor in the group where CRP testing was not done, with an OR of 47.2.
The ROC curve analyses show the predictive value of a clinical model based on discoloured sputum, the four abnormal auscultatory findings, and perceived patient preference for antibiotics. The AUC of this “clinical findings only” model was largest in the Scandinavian subgroup not tested for CRP (AUC = 0.95) followed by the Welsh subgroup (AUC = 0.92) compared with those patients who were tested for CRP (AUC = 0.89) (). In the subgroup tested for CRP, similar AUCs were found for the “clinical findings only” model and for the “CRP only” model, whereas a significantly greater AUC was found for a model combining the clinical model and the CRP value, called “clinical model plus CRP” (AUC = 0.95, 95% CI = 0.93–0.97).
Figure 2. The ROC curve shows the predictive value of “the clinical model only” for antibiotic prescribing in the Welsh subgroup (n = 300) and the Scandinavian subgroup not tested for CRP (n = 131). Discoloured sputum, the four abnormal lung sounds and perceived patient preference for antibiotics are the variables included in the model.
Discussion
The CRP test results had a considerable influence on the decision whether or not to prescribe antibiotics for acute cough. This was not surprising, considering the strong association between CRP value and antibiotic prescribing found in two Swedish studies [Citation9,Citation10]. What this study adds is the fact that GPs also emphasize the CRP value in the presence of chest signs and symptoms, reducing the impact of findings such as wheezes and discoloured sputum. The added value of the CRP test in clinical decision-making is clearly demonstrated by the ROC curves (see ). This implies that GPs use the test to modify the role of clinical findings that poorly predict pneumonia and benefit from antibiotic treatment. [Citation4,Citation11–13].
The Welsh GPs perceived a patient preference for antibiotics more than three times more frequently than their Scandinavian colleagues. Since this perceived preference was associated with a similar prescription rate of over 80% in all three groups, the difference in perceiving this preference between Welsh and Scandinavian GPs probably accounted for much of the difference in antibiotic prescribing. GPs perception of patients’ preferences for prescriptions in general has been found to predict prescribing more strongly than actual self-reported patient preferences [Citation14–16].
Comparing the two Scandinavian subgroups
The prescription rates of antibiotics were similar in the Scandinavian networks, whether or not a POCT CRP was done. This may be explained by the selection for testing. Most patients who were not tested were treated by GPs who regularly used the test. The GPs probably did not feel that there would be added diagnostic value from the CRP test in this subgroup, since the clinical presentation was sufficient to guide the decision whether or not to prescribe antibiotics. The strong influence of clinical variables in the no-test subgroup was indicated by the high AUC score of 0.95 in the clinical model. The patients not tested were less severely ill, and had less comorbidity and abnormal lung sounds than patients tested for CRP (see ).
Comparison with previous studies
Macfarlane et al. found that discoloured sputum, history of fever, abnormal findings on chest examination, and the presence of “other factors” (such as patient preference for antibiotics) were highly significant predictors of antibiotic prescribing [Citation17]. The overall prescription rate was 75%, but increased to 95% when discoloured sputum or abnormal chest findings were present, which is similar to the prescription rates for the Welsh patients in the current study. Cals et al. found that in the Netherlands, a low antibiotic prescribing country [Citation2], auscultation abnormalities strongly predicted antibiotic prescribing [Citation18]. Interestingly, all patients with crackles on auscultation in the study by Hopstaken et al. [Citation4], also from the Netherlands, were prescribed antibiotics.
Strengths and limitations
We were able to consider and adjust for a number of important factors that have already been found to be associated with GP prescribing of antibiotics for patients with acute cough. The high value of the AUCs suggests that we have identified important explanatory variables. Differences in culture and clinical practice may have influenced GPs’ emphasis on different symptoms and clinical findings.
Implications for clinical practice and future research
Although GPs in the Nordic countries commonly use CRP values to inform their treatment decisions, it has not been clear whether this leads to a reduction in unnecessary antibiotics. In a recent study on LRTI in primary care, Cals et al. demonstrated that both the CRP test and improved consultation skills contributed significantly to decreased antibiotic prescribing without compromising the safety of the patients [Citation18]. Patients from Norway and Sweden with acute cough recovered at a similar rate to patients from high-prescribing countries [Citation3].
Evidence-based antibiotic prescribing can be promoted in several ways [Citation19]. The use of POCT CRP testing reduced the weight given to other clinical findings. The lower antibiotic prescribing rate and similar recovery rates in Norway and Sweden compared with other European countries [Citation3] suggests that CRP testing may reduce unnecessary prescribing by preventing over-reliance on clinical findings in patients presenting to primary care with acute cough. GPs outside Scandinavia have also shown interest in implementing the CRP test [Citation12,Citation18,Citation20]. Although GPs are concerned about feasibility and performance, they are generally strongly supportive of the introduction of POCT to improve management of common infections in primary care [Citation21].
Ethical approval
Ethic review committees in each country approved the study.
Acknowledgements
The authors acknowledge those members of the GRACE team who helped gather all these data thus making this paper possible. They would also like to thank the patients who willingly participated in the GRACE study.
Competing interest statement
All authors declare that there are no competing interests.
Funding
The study was funded through the GRACE study by the 6th Framework Program of the European Commission (Reference: LSHM-CT-2005-518226). The General Practice Research Unit at the University of Tromsø is funded by the Norwegian Government. The first author's PhD project is also funded by the General Practice Research Fund (Norwegian Medical Association).
References
- Grundmann H. EARSS Annual Report 2006 Report No. ISBN-13: 978-90-6960-183-0.
- Goossens H, Ferech M, Vander Stichele R, Elseviers M. Outpatient antibiotic use in Europe and association with resistance: A cross-national database study. Lancet 2005; 365:579–87.
- Butler CC, Hood K, Verheij T, Little P, Melbye H, Nuttall J, . Variation in antibiotic prescribing and its impact on recovery in patients with acute cough in primary care: Prospective study in 13 countries. BMJ 2009;338:b2242.
- Hopstaken RM, Butler CC, Muris JW, Knottnerus JA, Kester AD, Rinkens PE, . Do clinical findings in lower respiratory tract infection help general practitioners prescribe antibiotics appropriately? An observational cohort study in general practice. Fam Pract 2006;23:180–7.
- Little P, Rumsby K, Kelly J, Watson L, Moore M, Warner G, . Information leaflet and antibiotic prescribing strategies for acute lower respiratory tract infection: A randomized controlled trial. JAMA 2005;293:3029–35.
- Wood F, Simpson S, Butler CC. Socially responsible antibiotic choices in primary care: A qualitative study of GPs’ decisions to prescribe broad-spectrum and fluroquinolone antibiotics. Fam Pract 2007;24:427–34.
- Melbye H, Straume B, Brox J. Laboratory tests for pneumonia in general practice: The diagnostic values depend on the duration of illness. Scand J Prim Health Care 1992;10: 234–40.
- Andre M, Vernby A, Odenholt I, Lundborg CS, Axelsson I, Eriksson M, . Diagnosis-prescribing surveys in 2000, 2002 and 2005 in Swedish general practice: Consultations, diagnosis, diagnostics and treatment choices. Scand J Infect Dis 2008;40:648–54.
- Andre M, Schwan A, Odenholt I. The use of CRP tests in patients with respiratory tract infections in primary care in Sweden can be questioned. Scand J Infect Dis 2004;36: 192–7.
- Engstrom S, Molstad S, Lindstrom K, Nilsson G, Borgquist L. Excessive use of rapid tests in respiratory tract infections in Swedish primary health care. Scand J Infect Dis 2004;36:213–8.
- Melbye H, Straume, B., Aasebø, U., Dale K. Diagnosis of pneumonia in adults in general practice: Relative importance of typical symptoms and abnormal chest signs evaluated against a radiographic reference standard. Scand J Prim Health Care 1992;10:226–33.
- Hopstaken RM, Muris JW, Knottnerus JA, Kester AD, Rinkens PE, Dinant GJ. Contributions of symptoms, signs, erythrocyte sedimentation rate, and C-reactive protein to a diagnosis of pneumonia in acute lower respiratory tract infection. Br J Gen Pract 2003;53:358–64.
- Hopstaken RM, Stobberingh EE, Knottnerus JA, Muris JW, Nelemans P, Rinkens PE, . Clinical items not helpful in differentiating viral from bacterial lower respiratory tract infections in general practice. J Clin Epidemiol 2005;58: 175–83.
- Cockburn J, Pit S. Prescribing behaviour in clinical practice: patients’ expectations and doctors’ perceptions of patients’ expectations––a questionnaire study. BMJ 1997;315:520–3.
- Coenen S, Michiels B, Renard D, Denekens J, Van Royen P. Antibiotic prescribing for acute cough: The effect of perceived patient demand. Br J Gen Pract 2006;56:183–90.
- Macfarlane J, Holmes W, Macfarlane R, Britten N. Influence of patients’ expectations on antibiotic management of acute lower respiratory tract illness in general practice: Questionnaire study. BMJ 1997;315:1211–14.
- Macfarlane J, Lewis SA, Macfarlane R, Holmes W. Contemporary use of antibiotics in 1089 adults presenting with acute lower respiratory tract illness in general practice in the UK: Implications for developing management guidelines. Respir Med 1997;91:427–34.
- Cals JW, Butler CC, Hopstaken RM, Hood K, Dinant GJ. Effect of point of care testing for C reactive protein and training in communication skills on antibiotic use in lower respiratory tract infections: Cluster randomised trial. BMJ 2009;338:b1374.
- Tan T, Little P, Stokes T. Antibiotic prescribing for self limiting respiratory tract infections in primary care: Summary of NICE guidance. BMJ 2008;337:a437.
- Lingard H, Zehetmayer S, Maier M. Bacterial superinfection in upper respiratory tract infections estimated by increases in CRP values: A diagnostic follow-up in primary care. Scand J Prim Health Care 2008;26:211–15.
- Butler CC, Simpson S, Wood F. General practitioners’ perceptions of introducing near-patient testing for common infections into routine primary care: A qualitative study. Scand J Prim Health Care 2008;26:17–21.