Abstract
Objective. To analyse drug use in early pregnancy with special focus on socio-demographic factors associated with psychotropic and analgesic drug use. Design. Cross-sectional study. Setting and subjects. A total of 1765 women were invited via their local health care centres, and 1111 participated at 11–16 weeks of pregnancy by filling out a postal questionnaire concerning socio-demographic and obstetric background, stressful life events, and drug use. Main outcome measures. Drug use prior to and early on in pregnancy, socio-demographic factors, smoking, and adverse life events were investigated. Drug categories screened for were psychotropics (collective term for antidepressants, relaxants, and sleep medication), analgesics, hormones, nicotine, vitamins/minerals, and homeopathic medicine. Results. Drug use from the aforementioned drug categories, excluding vitamins/minerals and homeopathic medicine, was reduced by 18% during early pregnancy, compared with six months prior to conception (49% vs. 60%). Psychotropic drug use during early pregnancy was associated with elementary maternal education (p < 0.5), being unemployed (p < 0.001), being single/divorced/separated (p < 0.01), smoking prior to or during pregnancy (p < 0.01), forced to change job/move house (p < 0.001), and psychotropic drug use six months prior to pregnancy (p < 0.001). No items on the stressful life events scale were associated with increased analgesic use, which increased only with multiparity. Conclusions. Use of analgesics and psychotropic drugs seems common in pregnancy. Our results indicate that lack of a support network, stressful life events, and lower status in society may predispose women to more drug use. GPs and midwives responsible for maternity care could take this into account when evaluating risk and gain for women and foetuses in the primary care setting.
Pregnant women are usually excluded from drug trials for ethical reasons.
This study showed that:
Almost half of the women were taking at least one drug during early pregnancy, excluding vitamins/minerals and homeopathic medicine.
Significantly fewer women used drugs during early pregnancy, and those who did used drugs from fewer drug categories than compared with six months prior to pregnancy.
Drug use during early pregnancy had the strongest correlation with drug use six months prior to pregnancy.
Drug use during early pregnancy was associated with adverse life events and lower social position.
Introduction
Drug use during pregnancy is common [Citation1]. The incidence of prescribed drugs ranges from 40% to 93% [Citation2,Citation3] in economically developed countries, some of the range explained by exclusion or respectively inclusion of vitamins. Over-the-counter self-medication is reduced, while prescribed drug use rises [Citation4], with the majority of women taking more than one drug [Citation3,Citation5]. For ethical reasons all pregnant women are excluded from clinical drug trials [Citation6]. Instead, evaluation of drug safety relies on observational studies or large retrospective cohort studies [Citation7]. According to a study by Andrade et al., “approximately one half of all pregnant women are prescribed drugs for which there is no evidence of safety during pregnancy in humans, or for which there is evidence of foetal risk in animals or humans” [Citation5], and some drugs are deemed safe on the Internet even though their effect is unknown [Citation8]. Previous studies have shown that increased maternal age, reported health problems [Citation2], being single [Citation9], multiparity [Citation10], smoking at the time of delivery [Citation10], and high [Citation2] and low [Citation9] maternal educational levels are among socio-demographic and lifestyle factors influencing and increasing drug use during pregnancy. The use of drugs can be required for either pregnancy-related conditions or conditions unrelated to pregnancy [Citation1], but overuse should be avoided. Prescribed antidepressants, hypnotics, and sedatives have been reported in Sweden for around 3% of women in the first trimester and prescribed analgesics (NSAIDs, analgesics, and opioids) for around 4% [Citation11].
About 5000 women give birth per year in Iceland (http://www.statice.is). Primary health care centres (PHCs) all include maternity and well-baby care, and are staffed by general practitioners (GPs), midwives, nurses, and other ancillary staff, including obstetricians at larger PHCs. Maternity care for uncomplicated pregnancies is provided in PHCs [Citation12], and close collaboration with the nearest obstetric unit is universal where the majority of deliveries take place [Citation13,Citation14]. Of Iceland's total population of 320 000, most people live in urban areas, with 70% residing in or near the capital city of Reykjavik.
In Iceland, the prevalence of drug use during pregnancy is unknown. This study, set in primary maternity care, aims to study the frequency of drug use in early pregnancy and the association with socio-demographic variables. Special focus is placed on analgesic and psychotropic (the collective term for antidepressants, relaxants, and sleep medication) drug use.
Material and methods
The Icelandic “Childbirth and Health” (C&H) study, which was designed and carried out as a cohort study with a longitudinal follow-up in three separate phases, has been described in detail elsewhere [Citation13,Citation14]. Its design and questionnaires were based on a similar study carried out in Sweden in 1999–2000 [Citation15].
This study was based on cross-sectional data from phase I of the C&H study, which took place during early pregnancy at 11 to 16 weeks. A request to participate and a personal introduction were sent to 26 participating health care centres out of the total 45 centres nationwide, of which 13 were in a rural and 13 in an urban setting. The number of pregnant women attending for their first maternity care visit, during a 12-month period from February 2009 to March 2010, at their local health care centres was estimated to be around 3000. Our intension was to reach around 1500 participants from that group. The inclusion criteria were fluency in Icelandic, receiving maternity care in a primary care setting, and being 18 years of age or older. We used the consecutive convenient invitation method, stratified for urban–rural participation, according to the ratio 70:30. Midwives introduced the study both orally and in writing. After obtaining informed consent the researchers were sent relevant information for each participant. Questionnaires, including a correspondence envelope, were sent to 1765 women altogether and one letter of reminder three weeks later. Of these, 1117 women responded in phase I, but six later withdrew their consent, which gave a total of 1111 women (63% of those initially invited).
The questionnaires included a wide range of questions on socio-demographic and obstetric background, social support, perceived health, and drug use. Instrument screening for depression and stressful life events, using the Edinburgh Depression Scale (EDS), and Stressful Life Events scale (SLE), included serious illness of a family member, serious concerns about a family member or death, divorce, or separation, whether the subject had been forced to move house or change jobs, been made redundant, had feelings of insecurity at work, serious financial problems, or been legally prosecuted. One item was added to the original instrument: serious personal illness or accident [Citation16] in SLE. All scales have been translated, re-translated, and evaluated [Citation13]. Each item of the SLE was processed separately in correlation to overall drug use and use of psychotropics and analgesics. Depressive symptoms were evaluated using the EDS, a ten-item self-report scale, developed and validated by Cox et al. [Citation17]. Different cut-off scores have been used to categorize depressive symptoms, thus indicating depressive disorder. During pregnancy the cut-off was set at an EDS score of 15, as recommended by Murray and Cox (1990), with 100% sensitivity and 96% specificity [Citation18–20].
Eight drug categories, including sleep medications, antidepressants, relaxants, analgesics, hormones, nicotine, vitamins/minerals, and homeopathic medicines, were screened for in the questionnaire in early pregnancy and six months prior and these questions were modelled after the Swedish “KUB” study [Citation15]. Possible answers were: seldom, weekly, or daily where the women could mark appropriately from which of the eight drug categories they were currently taking drugs. Vitamins/minerals and homeopathic medicine were excluded in most analyses except for overall drug use and in the descriptive statistics given in .
Written consent was obtained from the head of staff at each health care centre, and the study was approved by the Icelandic Bioethical Committee (VSNb2008010023/03-1) and the Data Protection Authority (S3695/2008 LSL/–).
Statistical methods
Descriptive data are presented as mean values and percentages. Statistical significance was deemed to be at a p-value of 0.05 or less, with a two-sided significance test. A Pearson's chi-squared test was used to assess significance between groups. A logistic regression analysis was undertaken to investigate the association between the use of psychotropic drugs with age, marital status, working status, education, and number of pregnancies.
The statistical software package IBM, SPSS (version 20) was used for all data analysis.
Results
The 1111 women who participated represented 22% of the birth population in Iceland in 2009. The demographic variables of the study group are shown in . Most of the women are in the age group 25–34 years, were married or cohabiting, had good education, and 69% lived in the capital area.
Table I. Characteristics of participants in the Childbirth and Health Study 2009.
indicates the consumption pattern and answers according to the possible response categories. At least one drug from the drug categories screened for was taken by 92% of the women. Vitamins and minerals were most widely used by 88%, and 65% used them on a daily basis as recommended. After their exclusion the prevalence of drug use was 49%. Analgesic drug use was most prominent (46%), and collectively the use of psychotropic drugs was a very distant third (6%). Homeopathic medicine was second (7%) but consequently excluded from all further analyses.
Women were asked to report in the questionnaire whether they were diagnosed with a chronic disease. Ninety (8%) replied “yes” and listed which disease they had. Thirty-nine reported having asthma, 13 hypertension, 13 thyroidal disease, six allergies, four rheumatism, four fibromyalgia, three migraine, two attention deficit hyperactivity disorder, two epilepsy, two polycystic ovaries, and two achalasia.
Table II. Type and consumption pattern of self-reported drug use during early pregnancy.
gives a comparison of some factors associated with drug use during pregnancy, excluding vitamins/minerals and homeopathic medicine. Multiparity, employment status, and drug use six months prior to pregnancy were significantly associated with increased drug use in all categories. Use of psychotropic drugs during pregnancy was associated with elementary maternal education, being unemployed, being single/divorced/separated, smoking during pregnancy, psychotropic drug use six months prior to pregnancy, and depressive symptoms. A total of 46 women had an EDS score ≥ 15 indicating depressive symptoms, and eight of them (17%) reported psychotropic drug use, whereas 41 woman (4%) out of 1060 took psychotropic drugs during early pregnancy and had EDS scores below 15. Prior induced abortion or difficulties in conceiving were not associated with drug use. A logistic regression analysis using psychotropic drugs as dependent variable and the variables in as independent variables showed that working status (p = 0.02) and age (p = 0.04) had a significant association with this drug use.
Table III. Analysis of variables that might influence drug use during early pregnancy: overall, psychotropics, and analgesics.1
shows the analysis of associations between SLE and drug use during pregnancy. Psychotropic drug use was associated with separation or divorce, being forced to change jobs or move house p < 0.001, not shown in table), or having serious financial problems. No items in the SLE scale were associated with increased analgesic use. Furthermore, women who had been made redundant had more overall drug use during early pregnancy (p < 0.029, not shown in table). Six months prior to pregnancy 60% of the women included in this study took at least one drug from the aforementioned categories, with the exclusion of vitamins, minerals, and homeopathic medicines (), of whom 10% took items from more than one drug category. With the same exclusion, 49% of the women were taking at least one drug during early pregnancy from these drug categories, around 5% of them from more than one drug category. This represents an 18% total reduction of overall drug use from these categories compared with six months earlier, which has a statistical significance of p < 0.001.
Figure 1. Number of women taking drugs from one, two, three, and four drug categories (excluding vitamins/minerals and homeopathic medicine) six months prior to and at 11–16 weeks of gestation.
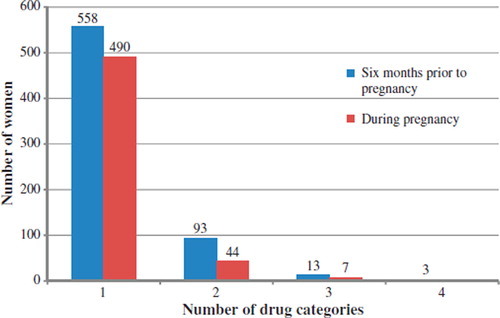
Table IV. Stressful life events and association with drug use during pregnancy.1. .
Discussion
The C&H study is the most comprehensive study on pregnancy and maternity care carried out in a PHC setting in Iceland. Almost half of the women report using some drug during early pregnancy, excluding vitamins and minerals, despite a reduction of nearly one-fifth compared with six months before. Most of the reported drug use is occasional analgesic use and factors influencing drug use in our results were similar to those in existing literature [Citation2,Citation9,Citation10]. Drug use six months prior to pregnancy was significantly correlated with overall drug use and even psychotropic and analgesic drug use. Increased drug use was seen with multiparity as well as in the face of adverse events, such as being made redundant and having a serious financial crisis. Being single, unemployed, smoking prior to and during pregnancy, and low level of education increase the consumption of psychotropic drugs. Of these, the rate of antidepressant drug use at some point in pregnancy doubled between 1999 and 2003 [Citation21]. The prevalence of psychotropic drug use in the study cohort is double what was reported in the Swedish study by Stephanson et al. [Citation11], but the prevalence of anti-depressive drugs is similar in both countries in early pregnancy. This assertion assumes that the reported use of antidepressants in the study cohort is SSRIs only, whereas tricyclic antidepressants and monoamine oxidase inhibitors are uncommon in contemporary practice [Citation22]. Looking at the EDS scores over 15, indicative of a major depressive episode [Citation22], one-fifth of the women with a clinically significant score were receiving psychotropic drugs and were subsequently undertreated. However, as we did not have further information on treatment alternatives, it might be that they received non-pharmacological treatment for depression. All but one woman in the study cohort reported continuing use of psychotropic drugs in early pregnancy as compared with six months prior. Analgesic drug use is high, with almost half of the women using them occasionally, but this includes both over-the-counter and prescribed drug use. It is worth mentioning that all drugs containing codeine were only available on prescription at the time of the study. It is difficult to evaluate the exact exposure, risk, or gain of analgesic use described as seldom during early pregnancy, which is the most prevalent drug use in the study cohort although a recent Norwegian study has indicated that paracetamol might have an adverse effect on neurological development, irrelevant of in which trimester exposure took place [Citation30]. For comparison one-tenth of women use prescribed analgesics in Sweden [Citation11]. Most of the analgesic drug use reported here is considered to be over-the-counter. No correction was made for the sporadic use of paracetamol for the influenza period whereas the women in this study were included from February 2009 till March 2010 at a fairly even rate. All were asked for current drug use during the time of inclusion so this would include sporadic use for influenza; however, the women were not asked why they were taking current drugs. Despite this, sporadic use of paracetamol cannot account for nearly every other woman using analgesics during early pregnancy and previous studies have shown that occasional drug use tends to be underreported, while agreement is high for drugs used for chronic conditions [Citation11].
The main strength of this study is the large sample of pregnant women who took part in the first phase, or approximately 22% of all pregnant women in Iceland. The participants are considered to be representative of the national population, with the possible exception of education, indicating that our participants possibly had a higher level of education than average [Citation13,Citation14]. Furthermore, the questionnaires, which are modelled after the Swedish “Experience of Pregnancy and Delivery” study, have been well evaluated and standardized [Citation13,Citation15].
The main limitation of this study was the self-reported information gathered on drug use during early pregnancy, which was not confirmed by prescription data from the medical records. Selection bias as well as response bias must also be taken into consideration. Although we used the convenience sampling method we do consider selective bias to be unlikely because the invited women who were asked to answer the questionnaires on their general health, experience, and attitude towards their pregnancy were healthy pregnant women. The study had thus no focus on specific diseases or matters that could be easily selected out. A possible response bias could, however, exist, as those who answered the questionnaires were possibly more motivated to do so, compared with those who were willing to participate at first invitation but did not return the questionnaire. Although response bias could be related to the questions raised, we do not believe the questions regarding drug use to be provocative or sensitive. The questions in the questionnaire regarding drug use were general in wording; specific drug names and doses were not used, and the possible answers were seldom, every week, and daily, which greatly limits information on exposure and dosing. No distinction was made between over-the-counter and prescription drugs in any drug category, which in turn might explain the relatively high incidence of drug use during pregnancy as analgesics taken seldom are by far the largest variable. Common drugs used during pregnancy such as antibiotics were not included [Citation4,Citation9,Citation23], nor any of the known or suspected teratogenic drugs. Women needing these drugs during early pregnancy would receive maternity care from a specialist clinic [Citation12] rather than a PHC. The threshold for taking drugs during conception and the first weeks of gestation seems low, even though the risk of adverse outcome for the foetus is somewhat unknown [Citation24]. Socially unacceptable or embarrassing behaviour tends to go underreported [Citation7], such as using sleep medication and relaxants during pregnancy.
The quality of care, organisation, and tasks in general practice in Iceland are similar to practices in the other Nordic countries [Citation25,Citation26]. This includes good continuity of care in general [Citation27], as well as an awareness of shared decision-making [Citation28] and focusing on methods to maintain a healthy lifestyle in order to minimize drug use [Citation29]. This platform, however, gives GPs a unique position to identify women at risk, scrutinize earlier drug use, and make appropriate plans for further drug use during their pregnancies. This could even include occasional analgesic use whereas a recent Norwegian study has indicated that paracetamol during pregnancy was associated with adverse psychomotor, behavioural, and temperamental outcomes for the child [Citation30]. Stressful life events, especially those regarding women's financial and personal situation, seem to be precipitating factors for drug use during early pregnancy and should be checked on by maternity personnel for timely interventions. Furthermore, detailed studies focusing primarily on drug use during pregnancy are needed in the primary care setting.
Acknowledgements
The authors would like to thank the Childbirth & Health steering group (Olof Asta Olafsdottir and Thora Steingrimsdottir together with two of the authors; JAS, HK). The study received support from the Research Fund of the Icelandic College of Family Physicians, the Primary Health Care of the Capital Area, Iceland, Icelandic Midwifery Association Research Fund, and the Landspitali (Icelandic National Hospital) University Hospital Research Fund.
Declaration of interest
There are no conflicts of interest in connection with the paper. The authors alone are responsible for the content and writing of the paper.
References
- Van Hasselt JG, Andrew MA, Hebert MF, Tarning J, Vicini P, Mattison DR. The status of pharmacometrics in pregnancy: Highlights from the 3rd American conference on pharmacometrics. Br J Clin Pharmacol 2012;74:932–9.
- Donati S, Baglio G, Spinelli A, Grandolfo ME. Drug use in pregnancy among Italian women. Eur J Clin Pharmacol 2000;56:323–8.
- Nordeng H, Eskild A, Nesheim B, Jacobsen G. Drug use in pregnancy among parous Scandinavian women. J Epidemiol 2001;11:97–103.
- Odalovic M, Vezmar Kovacevic S, Nordeng H, Ilic K, Sabo A, Tasic L. Predictors of the use of medications before and during pregnancy. Int J Clin Pharmacol 2013;35: 408–16.
- Andrade SE, Gurwitz JH, Davis RL, Chan KA, Finkelstein JA, Fortman K, et al. Prescription drug use in pregnancy. Am J Obstet Gynecol 2004;191:398–407.
- Grzeskowiak LE, Gilbert AL, Morrison JL. Exposed or not exposed? Exploring exposure classification in studies using administrative data to investigate outcomes following medication use during pregnancy. Eur J Clin Pharmacol 2012;68:459–67.
- Grzeskowiak LE, Gilbert AL, Morrison JL. Investigating outcomes associated with medication use during pregnancy: A review of methodological challenges and observational study designs. Reprod Toxicol 2012;33:280–9.
- Peters SL, Lind JN, Humphrey JR, Friedman JM, Honein MA, Tassinari MS, et al. Safe lists for medications in pregnancy: Inadequate evidence base and inconsistent guidance from web-based information, 2011. Pharmacoepidemiol Drug Saf 2013;22:324–8.
- Olesen C, Thrane N, Henriksen TB, Ehrenstein V, Olsen J. Associations between socio-economic factors and the use of prescription medication during pregnancy: A population-based study among 19,874 Danish women. Eur J Clin Pharmacol 2006;62:547–53.
- Nordeng H, Hansen C, Garthus-Niegel S, Eberhard-Gran M. Fear of childbirth, mental health, and medication use during pregnancy. Arch Women Ment Health 2012;15:203–9.
- Stephansson O, Granath F, Svensson T, Haglund B, Ekbom A, Kieler H. Drug use during pregnancy in Sweden – assessed by the Prescribed Drug Register and the Medical Birth Register. Clin Epidemiol 2011;3:43–50.
- Sigurdsson JA. The GP's role in maternity care. Scand J Prim Health Care 2003;21:65.
- Kristjansdottir H, Steingrimsdottir T, Olafsdottir O, Bjornsdottir A, Sigurdsson JA. Childbirth and Health. Ljosmaedrabladid (Icelandic Journal of Midwifery) 2012: 13–21.
- Erlingsdottir A, Sigurdsson EL, Jonsson JS, Kristjansdottir H, Sigurdsson JA. Smoking during pregnancy: Childbirth and Health Study in Primary Care in Iceland. Scand J Prim Health Care 2014;32:11–6. doi: 10.3109/02813432. 2013.869409. Epub 2014 Feb 17.
- Hildingsson I, Waldenström U, Rådestad I. Women's expectations on antenatal care as assessed in early pregnancy: Number of visits, continuity of caregiver and general content. Acta Obstet Gynecol Scand 2002;81:118–25.
- Rosengren A, Orth-Gomér K, Wedel H, Wilhelmsen L. Stressful life events, social support, and mortality in men born in 1933. BMJ 1993;307:1102–5.
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987;150:782–6.
- Rubertsson C, Wickberg B, Gustavsson P, Rådestad I. Depressive symptoms in early pregnancy, two months and one year postpartum: Prevalence and psychosocial risk factors in a national Swedish sample. Arch Women Ment Health 2005;8:97–104.
- Rubertsson C, Waldenstrom U. Depressive mood in early pregnancy: Prevalence and women at risk in a national Swedish sample. J Reproductive and Infant Psychology 2003;21:113–23.
- Murray D, Cox J. Screening for depression during pregnancy with the Edinburgh Depression Scale (EPDS). J Reprod Infant Psychol 1990;8:99–107.
- Yonkers KA, Wisner KL, Stewart DE, Oberlander TF, Dell DL, Stotland N et al. The management of depression during pregnancy: A report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. Obstet Gynecol 2009;114:703–13.
- Matthey S, Henshaw C, Elliott S, Barnett B. Variability in use of cut-off scores and formats on the Edinburgh Postnatal Depression Scale: Implications for clinical and research practice. Arch Women Ment Health 2006;9:309–15.
- Gagne JJ, Maio V, Berghella V, Louis DZ, Gonnella JS. Prescription drug use during pregnancy: A population-based study in Regione Emilia-Romagna, Italy. Eur J Clin Pharmacol 2008;64:1125–32.
- Källén BA, Otterblad Olausson P. Maternal drug use in early pregnancy and infant cardiovascular defect. Reprod Toxicol 2003;17:255–61.
- Aaraas IJ, Hetlevik I, Roksund G, Steinert S. “Caring for people where they are”: Addressing the double challenge of general practice at the 17th Nordic Congress of General Practice in Tromsø 2011. Scand J Prim Health Care 2010;28:194–6.
- Sigurdsson JA. Milestones in the development of Nordic general practice. Scand J Prim Health Care 2013; 31:3–5.
- Hetlevik Ø, Gjesdal S. Personal continuity of care in Norwegian general practice: A national cross-sectional study. Scand J Prim Health Care 2012;30:214–21.
- Liira H. Patient information for better health outcomes in primary care. Scand J Prim Health Care 2011;29:65–6.
- Hrafnkelsson H, Sigurdsson G, Magnusson KT, Sigurdsson EL, Johannsson E. Fat mass increase in 7-year-old children: More bone area but lower bone mineral density. J Bone Miner Metab 2013;31:442–8.
- Brandlistuen RE, Ystorm E, Nulman I ,Koren G, Nordeng H. Prenatal paracetamol exposure and child neurodevelopment: A sibling-controlled cohort study. Int J Epidemio. 2013;1–12. Oct 24 [Epub ahead of print].

