Three papers on lifestyle interventions for the metabolic syndrome were published in the December 2014 issue of the Scandinavian Journal of Primary Health Care (SJPHC). One paper by Hrafnkelsson et al. presented a cluster randomized controlled trial (RCT) of an exercise and nutrition intervention in Icelandic schoolchildren [Citation1]. Another paper by Liira et al. reported from an RCT exercise intervention in Finnish men [Citation2]. A third paper reported a mixed-methods study where Miettola & Viljanen identified groups of middle-aged Finnish men and women who, based on their Sense of Coherence (SOC) profile and metabolic syndrome statuses, were or were not suitable for possible lifestyle interventions [Citation3]. While both RCTs by Hrafnkelsson et al. and Liira and et al. [Citation1,Citation2] failed to show significant improvements in main outcome measures such as blood pressure and metabolic blood markers, the third exploratory study by Miettola & Viljanen [Citation3] gave a potential answer to why they failed. Obviously not every person who would benefit from a lifestyle change will eventually change habits and therefore lifestyle interventions probably will need very cleverly tailored designs to succeed. Miettola & Viljanen suggested individualized interventions built on assessments of personal potentials based on needs, attitudes, and motivation, which they call “a salutogenic approach to intervention” [Citation3].
Exercise prescriptions have become popular in primary care [Citation4–6] and were in an SJPHC editorial by Sigurdsson in 2013 (last author in Hrafnkelsson 2014) suggested to “be among the first and most commonly utilized prescriptions given by GPs and other primary care providers” [Citation7]. Unfortunately, there is no clear-cut evidence to back this suggestion according to systematic reviews [Citation8,Citation9]. My first thought was, wrongly it later appeared, that Sigurdsson wrote his editorial influenced by positive initial results from the Icelandic school trial where significantly lower intervention group blood pressure results disappeared in regression cluster analyses. Instead Sigurdsson states, rightly in my opinion, that the many observational and cohort studies showing positive effects of physical activity promotion should not be ignored as in the BMJ systematic reviews [Citation8,Citation9] (personal communication). My own anecdotal clinical experience with exercise prescriptions is limited to patients with mainly psychological disturbances for whom they seem to have been useful. However, the hard evidence for the benefit of exercise prescriptions in this group is not striking either [Citation10].
The reasons for this lack of effect from standardized lifestyle interventions are doubtless manifold [Citation11]. Miettola & Viljanen [Citation3] have come up with a few suggestive answers on how to improve metabolic syndrome status by lifestyle interventions based on their sequential mixed-methods study. They thus combined data from a population-based health survey with 480 participants of whom 43 purposively selected participants were interviewed individually. Both genders, all age groups, and three different metabolic syndrome statuses – confirmed, liable, and not liable to metabolic syndrome – were represented. Antonovsky's salutogenic theory of SOC [Citation12] was used as an analytical framework for assessing messages and meanings of respondents’ stories to create six different lifestyle profile typologies. Through this procedure the authors present a well-ordered person-centred salutogenically tailored model of metabolic syndrome prevention that remains to be tested in future empirical research.
Liira in 2010 [Citation13] suggested holistic approaches in order to succeed with lifestyle interventions: “We need to design interventions where efficacy is maximized by using synergistic strategies: knowledge management, social marketing, and partnerships with other professionals in communities”. She also emphasized that “Physical activity should be fun, moderate, and cumulative. With the aid of the school system, public sports facilities, and physical education professionals in communities, low-threshold opportunities for physical activity can be offered to all.” Her suggestions ring even more true today after so many studies have shown that standardized lifestyle interventions are not a magic bullet to fight illness caused by a sedentary way of life.
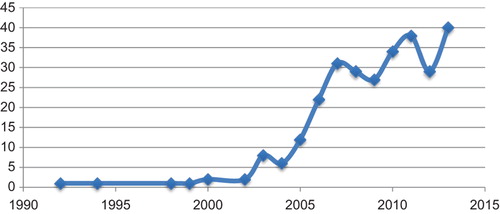
In summary, three papers in the December 2014 issue of our journal investigated the same topic: lifestyle interventions against the metabolic syndrome showing a recently stagnating yet considerable growth in the number of MEDLINE publications, while publications with negative results have started to emerge (). Two RCT-designed interventions failed to show significant effects, whereas a third mixed-methods paper suggested a tailored person-centred intervention [Citation1–3].
References
- Hrafnkelsson H, Magnusson KT, Thorsdottir I, Johannsson E, Sigurdsson EL. Result of school-based intervention on cardiovascular risk factors. Scand J Prim Health Care 2014;32:149–55.
- Liira H, Engberg E, Leppävuori J, From S, Kautiainen H, Liira J, Remes-Lyly T, Tikkanen H, Pitkälä K. Exercise intervention and health checks for middle-aged men with elevated cardiovascular risk: A randomized controlled trial. Scand J Prim Health Care. 2014;32:156–62.
- Miettola J, Viljanen AM. A salutogenic approach to prevention of metabolic syndrome: A mixed-methods population study. Scand J Prim Health Care 2014;32:217–25.
- Lawton BA, Rose SB, Elley CR, Dowell AC, Fenton A, Moyes SA. Exercise on prescription for women aged 40–74 recruited through primary care: Two year randomised controlled trial. BMJ 2008;337:a2509.
- Romé A, Persson U, Ekdahl C, Gard G. Physical activity on prescription (PAP): Costs and consequences of a randomized, controlled trial in primary healthcare. Scand J Prim Health Care 2009;27:216–22.
- Pescatello, Linda S., ed. ACSM's guidelines for exercise testing and prescription. Baltimore, MD: Lippincott Williams & Wilkins; 2014.
- Sigurdsson EL. Up and running: An underutilized prescription in primary care. Scand J Prim Health Care 2013;31:1–2.
- Pavey TG, Taylor AH, Fox KR, et al. Effect of exercise referral schemes in primary care on physical activity and improving health outcomes: Systematic review and metaanalysis. BMJ 2011;343:d6462.
- Orrow G, Kinmonth A-L, Sanderson S, et al. Effectiveness of physical activity promotion based in primary care: Systematic review and meta-analysis of randomised controlled trials. BMJ 2012;344:e1389.
- Ravindran AV, da Silva TL. Complementary and alternative therapies as add-on to pharmacotherapy for mood and anxiety disorders: A systematic review. J Affect Disord 2013;150:707–19.
- Leijon ME, Faskunger J, Bendtsen P, Festin K, Nilsen P. Who is not adhering to physical activity referrals, and why? Scand J Prim Health Care 2011;29:234–40.
- Antonovsky, A. Unraveling the mystery of health. San Francisco: Jossey-Bass; 1987.
- Liira H. How to promote exercise in primary care. Scand J Prim Health Care 2010;28:130–1.