Abstract
Objective. Childbirth is a strong trigger of psychiatric episodes. Nevertheless, use of primary care before these episodes is not quantified. The aim was to study the use of general practice in Denmark from two years before to one year after childbirth in women who developed postpartum psychiatric disorders. Design. A matched cohort study was conducted including women who gave birth in the period 1996–2010. Women were divided into four groups: (i) all mothers with postpartum psychiatric episodes 0–3 months after birth, n = 939; 2: All mothers with a postpartum psychiatric episode 3–12 months after birth, n = 1 436; and (iii) two comparison groups of mothers, total n = 6 630 among 320 620 eligible women. Setting. Denmark. Subjects. Women born in Denmark after 1 January 1960, restricting the cohort to women who gave birth to their first singleton child between 1 January 1996 and 20 October 2010. Main outcome measures. The main outcome measures were consultation rates, consultation rate ratios, and rate differences. Results. Women who developed a psychiatric episode after childbirth had higher GP consultation rates before, during, and after the pregnancy. Women with a psychiatric episode 0–3 months postpartum had 6.89 (95% CI 6.60; 7.18) mean number of consultations during pregnancy, corresponding to 1.52 (95% CI 1.22; 1.82) more visits than the comparison group. Conclusion. Women with a postpartum psychiatric episode had higher use of GP-based primary health care services years before the childbirth, and in this specific group of patients childbirth itself triggered a marked increase in the number of GP contacts postpartum.
Childbirth is a potent trigger of psychiatric episodes; nevertheless, use of primary care before these episodes is not quantified.
Women who developed postpartum psychiatric episodes had significantly more consultations both before and during pregnancy than women without such episodes.
GP contacts increased significantly in the immediate postpartum period for women who developed psychiatric episodes after childbirth.
Among women with no previous records of psychiatric disorders, we found that the mothers who developed postpartum psychiatric episodes may constitute a vulnerable group of women several years before onset of mental disorder.
Introduction
Childbirth is a potent trigger of psychiatric episodes, with and without psychotic features [Citation1–7]. The risk of psychotic episodes is high soon after childbirth and around 0.1% of new mothers are affected [Citation1], whereas up to 15% of all mothers experience depressive symptoms postpartum [Citation2,Citation5,Citation8,Citation9]. An untreated severe postpartum psychiatric episode can have serious consequences including maternal suicide and infanticide [Citation10–12].
Little is known about the prodromal phase, i.e. the period of time from when the first symptoms occur until the specific postpartum disorder is diagnosed [Citation13–15]. Studies have shown that 40–45% of the women who developed postpartum depression had symptom onset during pregnancy [Citation2,Citation16]. In comparison, 50% of the women who developed postpartum psychosis had symptom onset 1–3 days after birth [Citation17]. These figures indicate that, in some women, the first symptoms of an emerging postpartum episode arise already during the pregnancy or perhaps even before, while others have no or a very short prodromal phase.
Identification of psychiatric symptoms during the prodromal phase can allow early diagnosis, treatment, and provision of specific support for women at risk, which may reduce the burden and improve the prognosis of the disease. Additionally, the pregnancy period is an opportune time for intervention because many countries offer free and comprehensive antenatal programmes, including close contact with health-care professionals. In Denmark, the general practitioner (GP) provides first-line medical advice and is the first point of contact when a woman seeks medical attention for mental-health symptoms as all citizens are listed with a specific general practice. A study on the primary health-care-seeking behaviour may provide new information on the aspects of early detection by identifying changes in health-care seeking behaviours, diagnosis, and duration of the prodromal phase. Although most mental disorders are detected and treated in general practice [Citation18], no studies have so far studied health-care-seeking behaviours specifically among women developing postpartum psychiatric episodes. Consequently, we aimed to describe the use of primary health care and the compliance with antenatal care programmes before and during pregnancy in women who subsequently developed a postpartum psychiatric disorder compared with mothers who did not.
Material and methods
Study design
We conducted a population-based matched comparative study (matched cohort study) to describe the number of primary health care contacts in mothers during a period from two years before to one year after childbirth. We identified and included women born in Denmark after 1 January 1960, and restricted the cohort to women who gave birth to their first singleton child between 1 January 1996 and 20 October 2010, to ensure complete follow-up for each individual mother in the entire study period (i.e. from two years before birth of their child to one year after).
Study population
We identified all women who experienced a postpartum psychiatric episode defined as first-time inpatient or outpatient psychiatric contact for any type of psychiatric diagnosis made up to 12 months after the delivery. The women were divided into two case groups: Case group 1: Mothers who developed a postpartum psychiatric episode 0–3 months (0–90 days) after birth and case group 2: Mothers who developed a postpartum psychiatric episode 3–12 months (91–360 days) after birth. For each mother with a record of a postpartum psychiatric episode (case groups 1 and 2) we identified up to three women for comparative purposes defined in two comparison groups. These women were matched on the following criteria: maternal age at childbirth (+/- two years), health-care provider (the general practice where the woman was listed), and the following three calendar periods: childbirths from 1 January 1996 to 31 December 2000; from 1 January 2001 to 31 December 2005; and from 1 January 2006 up to 20 October 2010. This match aimed to reduce any potential bias from age, changes in health seeking behaviours, and treatment options over time, local/national geographical differences and differences in health-care preferences among the individual providers. Note that the definition of groups described above resulted in four groups in total for our study: Case group 1 vs. a matched comparison group, and Case group 2 vs. a matched comparison group.
Data resources and study variables
We used information from three different nationwide registers. Linkage between and within the registers was based on the unique personal identification number, which is assigned to all Danish citizens at birth or at immigration. We used data from the Danish Civil Registration System on date of birth, personal identification numbers, and daily updated information on vital status and migration [Citation19].
Information on psychiatric episodes was derived from the Danish Psychiatric Central Research Register [Citation20], which holds information on all contacts with psychiatric inpatient and outpatient facilities in Denmark during the entire study period. The diagnostic classification system used was the International Classification of Diseases, tenth version (ICD-10) [Citation21]. A psychiatric episode was defined as any type of contact for any psychiatric diagnoses with a psychiatric in- or outpatient treatment facility. To describe details regarding specific diagnoses information on diagnostic groups was also extracted from the register, including the following ICD-10 codes: F20–29 (schizophrenia-like disorders), F30–39 (mood/affective disorders), F40–48 (neurotic, stress-related, and somatoform disorders), F50–59 (behavioural syndromes), remaining F-diagnoses and other diagnoses related to mental health problems. To restrict the analyses to include only first-time episodes of mental disorders, women with a record of any type of mental disorder before the date of childbirth were excluded.
The Danish National Health Service Register contains information on activities in the tax-funded public health-care system, including services delivered by the general practitioners (GPs) [Citation22]. The register also contains information on administrative data (used for remuneration purposes), information on citizens and health-care providers, as well as information on a range of basic and additional health-care services such as for example consultations, talking therapy, laboratory results, and psychometric tests. All Danes are entitled to health care services and approximately 98% of the population are listed with a GP [Citation23]. For the present study we counted provided face-to-face surgery consultations in general practice coded 0101 in daytime and out-of-hours service (codes 80, 81, 82, 83, 89). Furthermore, we included information on specific services including GP-provided talk therapy (coded 6101) and depression tests (coded 2147 or 2149). We also included information on visits to GPs conducted as part of the national antenatal care programme offered to all pregnant women, specifically pregnancy-related visits at weeks 6–10, 24, and 35 of gestation (coded 8110, 8120, or 8130 respectively).
Statistical analyses
For women who developed psychiatric episodes during 0–3 months and 3–12 months postpartum and the two matched comparison groups the mean number of monthly visits to the GP was calculated, as was the number of psychometric tests, talking therapy sessions, and scheduled antenatal visits. Estimates and corresponding 95% confidence intervals (95% CI) were calculated using a negative binominal regression model applying cluster-robust variance estimation to account for heterogeneity between strata. Corrections were made for age. The main outcome measures were consultation rates, consultation rate ratios, and rate differences. Data were analysed using Stata 12.0 (StataCorp LP, TX, USA).
Results
During the study period, 939 women were diagnosed with a first-time psychiatric episode 0–3 months postpartum, while 1 436 women were diagnosed with a first-time psychiatric episode 3–12 months postpartum. For these cases, there were 6 630 matched women in the two comparison groups (2 662 and 3 968 women, respectively). At the time of childbirth, the average age was 28.4 years for the women who had a psychiatric episode 0–3 months postpartum, and 27.2 years for the women who had a psychiatric episode 3–12 months postpartum. For the matched comparison groups, the average age was 28.4 and 27.3 years, respectively.
The 939 women with first-time psychiatric episodes 0–3 months postpartum were given the following specific diagnoses: Schizophrenia-like disorders (n = 34), mood/affective disorders (n = 310), neurotic, stress-related, and somatoform disorders (n = 425), behavioural syndromes (n = 67), and remaining F-diagnoses and other diagnoses related to mental health problems (n = 103). Similarly, the 1 436 women diagnosed with first-time psychiatric episodes 3–12 months postpartum were given the following diagnoses: Schizophrenia-like disorders (n = 29), mood/affective disorders (n = 432), neurotic, stress-related, and somatoform disorders (n = 654), behavioural syndromes (n = 109), and remaining F-diagnoses and other diagnoses related to mental health problems (n = 212).
At any time point from 24 months before until the time of childbirth, women who later developed a postpartum psychiatric episode had more contacts with general practice than the two comparison groups ( and ). For women who developed a psychiatric episode 0–3 months postpartum, the mean number of consultations during pregnancy was 6.89 (95% CI 6.60; 7.18), which corresponds to 1.52 (95% CI 1.22; 1.82) additional mean visits compared with their comparison group (). For women who developed a psychiatric episode 3–12 months postpartum, the mean number was 7.10 (95% CI 6.87; 7.33), which corresponds to 1.47 (95% CI 1.23; 1.72) visits more than their comparison group ().
Figure 1. Mean number of ordinary consultations and consultation rate ratios from two years before until one year after childbirth in women with psychiatric episodes 0–3 months postpartum compared with women with no psychiatric episode (n = 939 and n = 2 662, respectively).
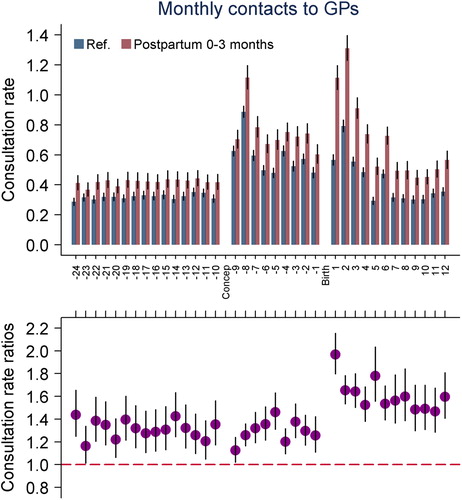
Figure 2. Mean number of ordinary consultations and consultation rate ratios from two years before until one year after childbirth in women with psychiatric episodes 3–12 months postpartum compared with women with no psychiatric episodes (n = 1 436 and n = 3 968 respectively).
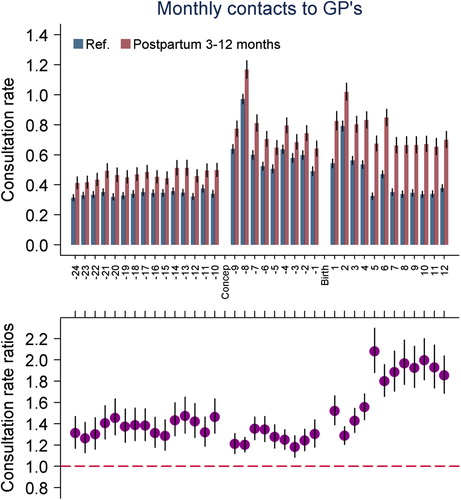
Table I. Mean number of contacts with GPs from two years before childbirth until one year after childbirth in mothers with a psychiatric episode 0–3 months postpartum vs. the comparison group.1
Table II. Mean number of contacts with GPs from two years before childbirth until one year after childbirth in mothers with a psychiatric episode 3–12 months postpartum vs. the comparison group.1
Before childbirth the provision of depression tests was similar in women who later developed a psychiatric episode and their disease-free counterparts. This changed after childbirth, and significantly more tests were administered to women who were subsequently referred to treatment at psychiatric facilities 0–3 months postpartum (18%), than in their comparison group (1%) (results not shown). Similarly, at any time before childbirth GP-provided talking therapy was infrequent for both case groups and comparison groups. Shortly after childbirth, a marked increase in GP-provided talking therapy was observed in women who developed psychiatric symptoms 0–3 months postpartum (23%), but not in the comparison group (1%) (results not shown).
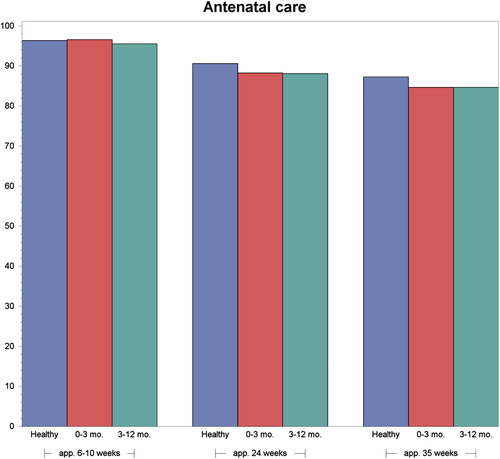
The majority of all mothers attended the three planned antenatal care check-ups at the GP clinic. Non-compliance with the antenatal care programme was slightly higher in the group of women who developed a postpartum psychiatric episode than in the comparison group, but not to a clinically significant level ().
Discussion
In this population-based matched comparative study, women with first-time postpartum psychiatric episodes had consistently more consultations with general practice than women with no such episodes. This was observed from two years before childbirth, although it is likely also to be present before this time point. Shortly after birth, the numbers of consultations, psychometric tests, and talk therapies provided by the GPs increased markedly among women diagnosed with psychiatric diagnoses postpartum.
Compliance with antenatal care
Approximately 85% of women experience some mood disturbances during the postpartum period, but for most women the symptoms are mild and cause no impairment of functions and require no treatment [Citation24]. However, approximately 0.1% of all new mothers experience an acute postpartum psychiatric episode, often with psychotic features [Citation1,Citation25]. Such episodes are considered psychiatric emergencies due to the risk of infanticide and/or maternal suicide [Citation10,Citation11]. Despite struggling with the personal challenges related to the psychiatric episode, mothers with perinatal depression or anxiety have been shown to be as likely to attend well-baby visits and receive immunizations as their healthy counterparts [Citation26]. This result conforms to the observation in our study, which shows that women who develop a postpartum psychiatric episode comply with the national antenatal care programme just as much as pregnant women who remain healthy after giving birth. Importantly, depression assessment has been shown to be well accepted by patients during prenatal care (23). Regardless of symptom severity, the perinatal period provides several occasions to identify and manage mild, moderate, and severe mental illness because of the increased level of contact with the GP and other health professionals through routine antenatal care and postnatal visits (24).
Early identification of postpartum psychiatric illness
Many women and their GPs mistakenly believe that even serious mood symptoms are typical postpartum reactions, and some women may be too afraid or embarrassed to disclose their depressive symptoms [Citation24]. Much may be gained from early identification and management of postpartum depression [Citation27], but our study revealed no time points at which symptoms are most likely to occur, as the women had a general tendency towards increased help-seeking behaviours long before birth. However, our findings indicate that the women are well known to the GP, and this may form a potential for systematic early detection of mood disorders. The fact that the women attend the GP for guidance, especially the antenatal screening programme, confirms that it is possible to provide efficient health care during the pregnancy, even for vulnerable groups.
There is a strong link between bipolar affective disorders and postpartum psychosis, and half of all patients with bipolar disorders treated in secondary care are able to report prodromes [Citation28]. However, this has only little predictive value for the many women who experience their first psychiatric (bipolar) episode after childbirth with no antecedent history of mental health problems [Citation29]. Unfortunately, this makes postpartum psychiatric episodes difficult – if not impossible – to predict [Citation29].
Strengths and limitations
Our population-based study obtained complete data on prospectively recorded primary health-care use for all women diagnosed with postpartum psychiatric episodes in Denmark and for a matched sample of women of the same age and with the same health-care provider. The data were not collected for the purpose of the present study and were independent of the memory of the GPs and the study participants. Data for our study were based on information from the Danish health-care system, which offers free access to primary health care for all Danish citizens. The registration of consultations and diagnostic procedures in the Danish National Health Service Register is expected to be valid and complete as the GPs code all activities for remuneration [Citation30]. Since GPs in Denmark are gatekeepers to the secondary health-care system, the vast majority of women in need of specialized psychiatric treatment will see their GP first. As in all population-based register studies we only had data on women who sought care and were diagnosed, but we did not have specific information on why the individual women sought care. It is likely that a proportion of women with mainly mild to moderate postpartum psychiatric episodes were treated either in general practice or referred to private practising psychologists/psychiatrists, and consequently not treated at a psychiatric treatment facility. Our study was limited by lack of important clinical information, such as the severity of symptoms and the results of psychometric tests performed by the GP. Finally, residual confounding cannot be ruled out since unmeasured patient characteristics may have influenced our results.
Conclusion
Women with a first-time postpartum psychiatric episode had significantly more general practice consultations than women in the comparison groups, both before and during pregnancy and in the postpartum period. The numbers of GP-provided contacts, talking therapy sessions, and use of a depression test increased significantly in the immediate postpartum period, thus indicating that psychiatric symptoms do not appear until (or are first recognized) after birth. In combination, these results indicate that mothers who experience a postpartum psychiatric episode may constitute a vulnerable group of women years before onset of the mental disorder. Also, the results indicate that childbirth itself may trigger a marked increase in the need for GP consultations, probably due to psychiatric symptoms, signifying a short prodromal phase for some women.
Source of funding
This study was supported by unrestricted research grants from the Lundbeck Foundation: The Initiative for Integrative Psychiatric Research (iPSYCH) and Mental Health in Primary Care (MEPRICA). Trine Munk-Olsen receives funding from NIMH (National Institute of Mental Health), grant number: R01MH104468.
The funders had no involvement in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Declaration of interest
There are no conflicts of interest in connection with the paper. The authors alone are responsible for the content and writing of the paper.
Henrik Søndergaard Pedersen had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- Munk-Olsen T, Laursen TM, Pedersen CB, Mors O, Mortensen PB. New parents and mental disorders: A population-based register study. JAMA 2006;296:2582–9.
- Wisner KL, Sit DK, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry 2013; Mar 13:1–9.
- Di FA, Forty L, Gordon-Smith K, Heron J, Jones L, Craddock N, et al. Perinatal episodes across the mood disorder spectrum. JAMA Psychiatry 2013;70:168–75.
- Munk-Olsen T, Gasse C, Laursen TM. Prevalence of antidepressant use and contacts with psychiatrists and psychologists in pregnant and postpartum women. Acta Psychiatr Scand 2011; Nov 25.
- Howard LM, Molyneaux E, Dennis CL, Rochat T, Stein A, Milgrom J. Non-psychotic mental disorders in the perinatal period. Lancet 2014;384:1775–88.
- Jones I, Chandra PS, Dazzan P, Howard LM. Bipolar disorder, affective psychosis, and schizophrenia in pregnancy and the post-partum period. Lancet 2014;384:1789–99.
- Bergink V, Lambregtse-van den Berg MP, Koorengevel KM, Kupka R, Kushner SA. First-onset psychosis occurring in the postpartum period: A prospective cohort study. J Clin Psychiatry 2011; Aug 23.
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: A systematic review of prevalence and incidence. Obstet Gynecol 2005; 106:1071–83.
- O’Hara MW, Swain AM. Rates and risk of postpartum depression: A meta-analysis. Int Rev Psychiatry 1996;8: 37–54.
- Appleby L, Mortensen PB, Faragher EB. Suicide and other causes of mortality after post-partum psychiatric admission. Br J Psychiatry 1998;173:209–11.
- Spinelli MG. Maternal infanticide associated with mental illness: Prevention and the promise of saved lives. Am J Psychiatry 2004;161:1548–57.
- Laursen TM, Munk-Olsen T, Mortensen PB, Abel KM, Appleby L, Webb RT. Filicide in offspring of parents with severe psychiatric disorders: A population-based cohort study of child homicide. J Clin Psychiatry 2011;72: 698–703.
- Conus P, Ward J, Hallam KT, Lucas N, Macneil C, McGorry PD, et al. The proximal prodrome to first episode mania: A new target for early intervention. Bipolar Disord 2008;10:555–65.
- Howes OD, Falkenberg I. Early detection and intervention in bipolar affective disorder: Targeting the development of the disorder. Curr Psychiatry Rep 2011;13:493–9.
- Esterberg M, Compton M. Family history of psychosis negatively impacts age at onset, negative symptoms, and duration of untreated illness and psychosis in first-episode psychosis patients. Psychiatry Res 2012;197:23–8.
- Heron J, O’Connor TG, Evans J, Golding J, Glover V. The course of anxiety and depression through pregnancy and the postpartum in a community sample. J Affect Disord 2004; 80:65–73.
- Heron J, Robertson BE, McGuinness M, Craddock N, Jones I. No “latent period” in the onset of bipolar affective puerperal psychosis. Arch Womens Ment Health 2007;10: 79–81.
- Ban L, Gibson JE, West J, Fiaschi L, Oates MR, Tata LJ. Impact of socioeconomic deprivation on maternal perinatal mental illnesses presenting to UK general practice. Br J Gen Pract 2012;62:e671–e678.
- Pedersen CB. The Danish Civil Registration System. Scand J Public Health 2011;39(7 Suppl):22–5.
- Mors O, Perto GP, Mortensen PB. The Danish Psychiatric Central Research Register. Scand J Public Health 2011;39 (7 Suppl):54–7.
- World Health Organization. WHO ICD-10: Psykiske lidelser og adfærdsmæssige forstyrrelser. Klassifikation og diagnostiske kriterier [WHO ICD-10: Mental and behavioural disorders: Classification and diagnostic criteria]. Copenhagen: Munksgaard; 1994.
- Andersen JS, Olivarius NF, Krasnik A. The Danish National Health Service Register. Scand J Public Health 2011;39 (7 Suppl):34–7.
- Pedersen KM, Andersen JS, Sondergaard J. General practice and primary health care in Denmark. J Am Board Fam Med 2012;25(Suppl 1):S34–S38.
- Cohen LS, Wang B, Nonacs R, Viguera AC, Lemon EL, Freeman MP. Treatment of mood disorders during pregnancy and postpartum. Psychiatr Clin North Am 2010; 33:273–93.
- Kendell RE, Chalmers JC, Platz C. Epidemiology of puerperal psychoses. Br J Psychiatry 1987;150:662–73.
- Farr SL, Dietz PM, Rizzo JH, Vesco KK, Callaghan WM, Bruce FC, et al. Health care utilisation in the first year of life among infants of mothers with perinatal depression or anxiety. Paediatr Perinat Epidemiol 2013;27:81–8.
- Tait L, Heron J. Management of postnatal depression in primary care: A window of opportunity. Br J Gen Pract 2010;60:801–2.
- Mantere O, Suominen K, Valtonen HM, Arvilommi P, Isometsa E. Only half of bipolar I and II patients report prodromal symptoms. J Affect Disord 2008;111:366–71.
- Blackmore ER, Rubinow DR, O’Connor TG, Liu X, Tang W, Craddock N, et al. Reproductive outcomes and risk of subsequent illness in women diagnosed with postpartum psychosis. Bipolar Disord 2013; May 7.
- Olivarius NF, Hollnagel H, Krasnik A, Pedersen PA, Thorsen H. The Danish National Health Service Register. A tool for primary health care research. Dan Med Bull 1997; 44:449–53.