To the Editor
Primary lung osteosarcoma (PLO) is an extremely rare extraosseous malignant tumor of the lung. To the best of our knowledge only 31 cases of PLO have been ever reported, including our case [Citation1–9]. From them, only 25 cases are well documented.
A 58-year-old woman was referred to our department after an incidental finding in a routine chest radiograph. The chest x-ray showed a dense mass, around 2 cm in size, located in the upper lobe of the left lung, proximal to the anatomic area of the lingula (). The Computed Tomography (CT) scan of the chest confirmed the presence of the mass (). The tumor was suspect of malignancy and for this reason complete routine preoperative evaluation was performed. Bone scintigraphy was negative. Due to the hard consistency of the tumor a core biopsy under CT guidance was precluded as unreliable. Therefore excisional biopsy through thoraco-tomy was planned for the patient.
A left anterior mini thoracotomy was performed. Wedge resection of the lung parenchyma including the nodule was undertaken using staplers. Frozen section was hard to be cut due to an osseous consistency, malignancy could not be excluded and therefore a left upper lobectomy was performed.
Figure 2. Chest CT scan. A computed tomogram showed a 2.1 cm heterogeneous calcified mass at the lingula of the left lung.
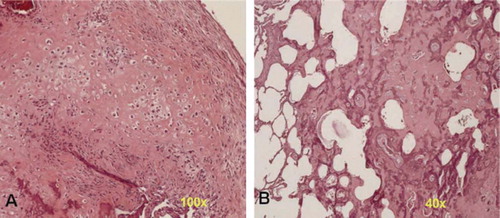
Final histologic examination of the specimen demonstrated macroscopically a tumor of 2.5 cm in size, whitish in colour and harsh in consistency, within the lung parenchyma and without infiltration of the pleura. Microscopically the neoplasm was characterized by: (Citation1) the presence of neoplastic cells responsible for the production of malignant osteoid; (Citation2) areas of both osteoblastic and chondro-blastic tissue and (Citation3) areas of sclerosis (). The dissected lymph nodes were negative for malignancy. The definite diagnosis was ‘‘primary lung osteosarcoma’’.
Figure 3. Chest CT scan. A computed tomogram showed a 2.1 cm heterogeneous calcified mass at the lingula of the left lung.
The patient had an uneventful postoperative course. Chemotherapy and radiation therapy were followed. The patient is alive six months after the operation. No recurrence of the disease has been observed.
Epidemiology
PLO is an extremely rare type of primary lung malignancy accounting only in 0.01% [Citation10]. It is more common in males (60%, 15/25 cases) than females. The average onset age is 61 years (range from 24 to 81 years). The left lung is involved in 68% (17/25 cases).
Clinical features
The mass presents without symptoms in 24% (6/25 cases). In symptomatic patients the most common manifestation is chest pain (9 cases). Other reported symptoms are chills and fever, dyspnea, cough, hemoptysis and interestingly two patients with upper extremity paresthesia.
Diagnosis
For a lung lesion to be considered a PLO, they must adhere to the following criteria: (Citation1) the tumor must be composed of a uniform pattern of sarcomatous tissue excluding in this way the possibility of mixed mesenchymal tumor; (Citation2) osteoid or bone must be formed by the sarcoma and (Citation3) a primary osseous tumor must be excluded [Citation11]. Most cases of PLO are appeared as huge masses on diagnosis. There are no specific clinical symptoms and radiographic findings for the PLO. The initial diagnostic management is that of a common pulmonary mass. The suspicion of a PLO is particularly based on the chest CT scan and bone scintigraphy findings [Citation3]. Calcification of the mass in the chest CTaccompanied by the radio-logic characteristics of malignancy is strongly suggestive of a lung osteosarcoma. Among 13 documented cases, calcification was reported in eight (61%). Unfortunately, the references about the diagnostic value of bone scintigraphy are limited. It is usually performed to rule out primary bone lesion or meta-static bone disease and thus there are not adequate data to evaluate its role in the diagnosis of PLO. Thus the definite diagnosis of a PLO is achieved by more invasive procedures or is a postmortem finding. In the previous studies the establishment of the definite diagnosis was achieved via autopsy in five cases (20%), via transbronchial lung biopsy in two cases (9%) and via fine-needle aspiration (FNA) cytology in five cases (20%). The surgical approach, diagnostic or therapeutic, was the most common method to achieve the definite diagnosis in 13 cases (52%). Due to hard consistency of the tumor the reliability of FNA seems to be uncertain.
Differential diagnosis
Various clinical entities must be excluded prior to establishment of PLO diagnosis:
(a) Metastatic osteosarcoma: The lungs are the predominant site of metastasis of an osseous osteosarcoma [Citation4]. A bone scintigraphy reveals uptake in primary site or rules out skeletal osteosarcoma elsewhere in the body [Citation3];
(b) Carcinosarcoma of the lung: It is characterized by the presence of carcinomatous foci in sarcoma tissue. Immunohistochemical analysis offers the definite diagnosis [Citation4];
(c) Soft tissue sarcoma of the lung: A large group of tumors classified in this category. Differences in clinical presentation, location or morphologic features such as calcification of the mass can be useful in suggesting the appropriate diagnosis, but misleading too [Citation12]. Taking in consideration the common presence of calcification in PLO,
(d) a calcified lung hamartoma;
(e) a calcified primary lung cancer or
(f) a calcified pulmonary carcinoid tumor should also be ruled out [Citation4].
Treatment
There is no clear information for the therapeutic management of PLO. Previous researchers reported that wide excisions and radical resections are thought to be effective for local control of the disease [Citation4]. Aggressive treatment with chemotherapy and radiotherapy is advantageous for others [Citation13]. From the well documented cases in the literature, 17 patients received a combination of treatments and eight of them were alive from 2 to 42 months after diagnosis. In contrast, eight patients did not receive or refused any treatment. In this group of patients the outcome was disappointing - all died within months (the average time was 4.4 months, range 1 to 11). It is therefore ‘‘supposed’’ that the combination of radical surgical resection of the tumor followed by chemotherapy and radiation therapy could offer better results in the management of the PLO.
Prognosis
The outcome of patients with primary lung osteosar-coma is poor. The majority of patients died within months. The only factor that probably improves the prognosis is early diagnosis and treatment. Factors like tumor size, histologic type and kind of therapy cannot accurately be considered as prognostic.
In conclusion, PLO is a rare but aggressive tumor associated with a very poor outcome. The initial management should be that of primary lung cancer objecting to early diagnosis and management that probably improve the prognosis. Surgical resection is the treatment of choice. Even if there is not enough knowledge proving the efficacy of chemotherapy and radiotherapy they are considered as part of treatment modalities.
References
- Niimi R, Matsumine A, Kusuzaki K, Inada Y, Kato Y, Maeda M, . Primary osteosarcoma of the lung: A case report and review of the literature. Med Oncol 2008;25:251–5.
- Danilova IA, Gordeladze AS, Antonova IV. Primary lungosteosarcoma simulating gastric carcinoma. Arkh Patol 2007;69:50–1.
- Yamazaki K, Okabayashi K, Hamatake D, Maekawa S, Yoshida Y, Yoshino I, . Primary osteosarcoma of the lung: A case report. Ann Thorac Cardiovasc Surg 2006;12:126–8.
- Kadowaki T, Hamada H, Yokoyama A, Katayama H, Abe M, Nishimura K, . Two cases of primary pulmonary oste-osarcoma. Intern Med 2005;44:632–7.
- Wagner MS, Reyes CV. Primary chondroblastic osteosar-coma of the lung. Sarcoma 1999;3:193–5.
- Connolly JP, McGuyer CA, Sageman WS, Bailey H. Intratho-racic osteosarcoma diagnosed by CT scan and pleural biopsy. Chest 1991;100:265–7.
- Saito H, Sakai S, Kobayashi T, Ishioroshi Y, Uno Y Primary osteosarcoma of the lung – a case report. Nihon Kyobu Shikkan Gakkai Zasshi 1983;21:153–6.
- Naruke T, Yoneyama T, Shimosato Y Case of primary osteo-genic sarcoma of the lung. Gan No Rinsho 1970;16:664–8.
- Kalengayi R, de Francquen P, Vanderhoeft P, Parmentier R. A case of primary osteosarcoma of the lung. Ann Anat Pathol (Paris) 1970;15:221–30.
- Miller DL, Allen MS. Rare pulmonary neoplasms. Mayo Clin Proc 1993;68:492–8.
- Robinson PG, Shields PG. Uncommon primary malignant tumors of the lung. Thomas W, Shields HC. General Thoracic Surgery, vol. 2, Chapter 119, 6th. Philadelphia, USA: Lippincott Williams & Wilkins Inc.; 2005. p. 1801–30.
- Gladish GW, Sabloff BM, Munden RF, Truong MT, Erasmus JJ, Chasen MH. Primary thoracic sarcomas. Radio-graphics 2002;22:621–37.
- Sordillo PP, Hajdu SI, Magill GB, Golbey RB. Extraosseous osteogenic sarcoma. A review of 48 patients. Cancer 1983;51:727–34.