Abstract
Little has been reported on the errors of setup and daily organ motion that occur during radiation therapy (RT) for esophageal cancer. The purpose of this paper was to determine the margins of esophageal motion during RT. Methods and materials. The shift of the esophagus was analyzed in 20 consecutive patients treated with RT for esophageal cancer from November 2007. CT images for RT planning were used as the primary image series. Computed tomography (CT) images were acquired using an Elekta Synergy System, equipped with a kilovoltage-based cone-beam CT (CBCT) unit. The subsequent CBCT image series used for daily RT setup were compared with the primary image series to analyze esophageal motion. CBCT was performed before treatment sessions a total of 10 times in each patient twice a week. The outer esophageal wall was contoured on the CBCT images of all 200 sets. Results. In the 200 sets of CBCT images, the mean (absolute) ± standard deviation (SD) of setup errors were 2 +/− 2 mm (max, 8 mm) in the lateral direction, 4 +/− 3 mm (max, 11 mm) in the longitudinal direction, and 4 +/− 3 mm (max, 13 mm) in the vertical direction. Additionally, the mean ± SD values of daily esophageal motion comparing the CBCT with RT planning CT were 5 +/− 3 mm (max, 15 mm) in the lateral direction and 5 +/− 3 mm (max, 15 mm) in the vertical direction. Conclusions. Our data support the use of target margins (between the clinical target volume and planning target volume) of 9 mm for day-to-day esophageal motion and 8 mm for patient setup in all directions, respectively.
Inter-fraction and intra-fraction motion of critical structures is a significant concern when patients undergo intensity modulated radiation therapy (IMRT). Improper dose modulation can be a result of anatomical motion among other factors. Overdosage to normal tissues can cause toxicity, while underdosage can lead to tumor progression. Image guided radiation therapy (IGRT) has been used in an attempt to minimize the impact of this motion.
Esophageal motion can be attributed to peristalsis, respiratory action, and cardiac action [Citation1]. However, it was not addressed in reviews on inter-fraction and intra-fraction organ motions during RT [Citation2]. Only the limited amount of data is available on the esophageal movement in patients undergoing RT planning [Citation1,Citation3]. The majority of patients with esophageal cancers are treated during free respiration. Thus, cone-beam computed tomography (CBCT) scans acquired during free respiration could provide relevant data on respiration-induced motion. Dieleman et al. [Citation4] performed four-dimensional CT analysis of esophageal mobility during normal respiration and concluded that the distal esophagus showed more mobility than other parts. Thus, they derived margins of mobility for use in treatment planning that can encompass all movement. The present study analyzed the patient setup error and day-to-day esophageal motion during IGRT. The 20 consecutive patients in this study represent the largest analysis heretofore conducted of daily inter-fraction esophageal movement during free respiration.
Materials and methods
Subjects
In this study, both patient setup error and inter-fraction daily shifts of the esophagus were analyzed in 20 consecutive patients with stage I-IVB esophageal cancer treated with chemoradiation with curative intent between November 2007 and May 2008 in University of Tokyo Hospital, Tokyo, Japan. The entire thoracic esophagus in all 20 cases was included within the radiation field. Ten sets of computed tomography (CT) images from each patient were acquired using an Elekta Synergy System (Elekta Ltd, Crawley, UK), equipped with a kilovoltage (kV)-based CBCT unit [Citation5].
The clinical and demographic data of the 20 patients are shown in . The 6th edition of the American Joint Committee on Cancer TNM staging system [Citation6] was used. For each patient, the CT images for RT planning (slice thickness of 5 mm, index of 1 mm, helical pitch of 15, and beam pitch of 15/16) acquired in free respiration by a large-bore CT system (Aquilion/LB, Toshiba, Tokyo, Japan) without any contrast media one or two days before treatment were used as the primary image series. The subsequent CBCT image series (slice thickness of 5 mm) used for daily RT setup were then compared to the primary image series to analyze inter-fraction esophageal motion. CBCT was performed before treatment sessions a total 10 times in each patient: one set of images was acquired twice a week during an overall RT duration of five weeks. The patient setup for RT treatment was carried out daily without referring to the previous data on setup error generated by CBCT and only the automatic bony landmark matching was carried out each time. However, because the CBCT imaging performed after this bone-matching registration (i.e. after correcting for the setup error) was used in the comparison, only day-to-day esophageal motion was taken into account. Automatic matching of anatomic bony landmarks was carried out and part of the image set for the matching was removed (e.g. shoulders, which are easily moved). A bony co-registration based on a window around the vertebral column was used for esophageal treatment since the esophagus is a posterior structure in close proximity to the vertebral column. Only an arm support was used as an immobilization device.
Table I. Patient and tumor characteristics.
CBCT imaging
To generate a set of CBCT images, the typical patient dose was 15.1 mGy (120 kV, 40 mA, 40 ms, 640 frames, 360°data collection), based on the weighted CT dose index (CTDIW), and this radiation dose was expected to have almost no effect on the total dose in the treatment. The outer esophageal wall was contoured on the CBCT images of all 200 sets from the esophageal orifice to the esophago-gastric junction under the mediastinal window setting (window width, 350 HU; window level, 40 HU). Only one radiation oncologist (HY), who was experienced with the RT planning system and had utilized it for routine planning, was involved in the contouring process.
Measurements method
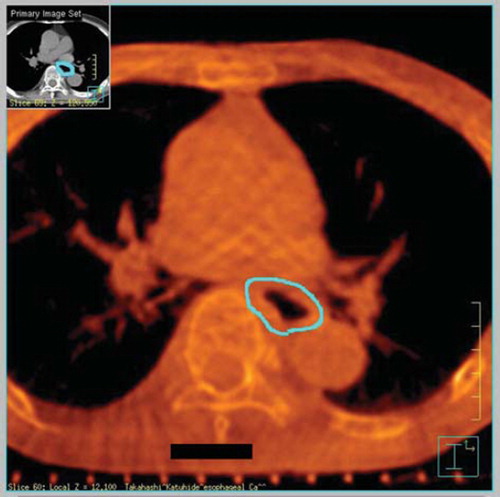
After bone-matching registration, the primary and pretreatment CT image series were fused and compared using a Pinnacle3 treatment-planning workstation (Philips Healthcare, Andover, MA, USA; ADAC, Milpitas, CA, USA). A case with the outer esophageal wall contoured on the CBCT image is shown in . Inter-fraction motion was measured using approximately 50 axial CT images of 5-mm slices from the esophageal inlet to the esophago-gastric junction. The measurements were done in the anterior-posterior and right-left (lateral) directions on all slices and then the maximum deviation between esophageal walls delineated in the each CBCT after the bone matching registration and the planning CT images across all scans were used. Therefore, all values of the inter-fraction motion were positive.
Figure 1. CBCT image of the middle thoracic region, scanned under free respiration and processed after transferring data onto a Pinnacle3 workstation for planning of RT. A case with the outer esophageal wall contoured on the CBCT images (sky-blue contour).
The formalism of Stroom et al. for margin derivation [Citation7] (= 2.0Σ + 0.7σ) and van Herk et al. [Citation8] (= 2.5Σ + 0.7σ) were used to evaluate the values as margin for setup error and daily esophageal motion error. However, another new optimization algorithm for the determination of treatment margins around moving and deformable targets like esophagus in radiotherapy proposed by Redpath & Muren [Citation9] was not used this time.
Results
Setup errors
In the 200 sets of CBCT images, the mean and SD values of the patient setup errors were 0 +/− 2 mm in the lateral direction, 0 +/− 3 mm in the longitudinal direction, and 0 +/− 4 mm in the vertical direction. The composite (all) SD was defined simply as the average of the individual SDs in each direction. The value of SD (=Σ) of the absolute value of the setup error in all 200 data was 2 mm (lateral), 3 mm (longitudinal), and 3 mm (vertical), respectively. The mean of the absolute value of the setup error in all 200 data was 2 mm (max, 8 mm) in the lateral direction, 4 mm (max, 11 mm) in the longitudinal direction, and 4 mm (max, 13 mm) in the vertical direction (). Based on the setup error for each patient, the maximum of SD was 4 mm in the lateral direction (case no. 14), 6 mm in the longitudinal direction (case no. 7), and 6 mm in the vertical direction (cases 5 and 18). The frequencies of setup errors >2 mm on the lateral, longitudinal, and vertical axes were 48%, 60%, and 73%, respectively, and the frequencies of errors >5 mm were 11%, 31%, and 30%, respectively. The patient setup error was corrected only by parallel translation, so the lag of rotation was not considered. According to the formalism of Stroom for margin derivation, the evaluation value as margin for setup error was 4 mm of right-left direction, 6 mm of dorsal-ventral direction, and 6 mm of cranio-caudal direction, and additionally, according to van Herk 5 mm, 8 mm, and 8 mm ().
Table II. Setup error in three dimension.
Esophageal motion errors
Additionally, the means ± SD’s of daily esophageal motion comparing the CBCT with RT planning CT were 5 +/− 3 mm (max, 15 mm) in the lateral direction and 5 +/− 3 mm (max, 15 mm) in the vertical direction (). A maximum shift in the lateral direction was found at the upper thoracic site in 79 sets (39.5%), at the middle thoracic site in 63 sets (31.5%), and at the lower thoracic site in 58 sets (29.0%). Moreover, there were shifts on the left side in 136 sets (68.0%) and on the right side in 64 sets (32.0%). A maximum shift in the vertical direction was found at the upper thoracic site in 49 sets (24.5%), at the middle thoracic in 80 sets (40%), and at the lower thoracic in 71 sets (35.5%). The motion was the same in the upper or the lower esophagus. Also, shifts were noted to the anterior direction in 88 sets (44.0%) and to the posterior direction in 112 sets (56%). Based on each patient's daily esophageal motion, the maximum SD was 4 mm in both vertical (cases 6 and 11) and lateral directions (case 3). According to Stroom, the evaluation value as margin for daily organ motion error was 7 mm of right-left direction and 7 mm of dorsal-ventral direction, and additionally, according to van Herk, 8 mm and 9 mm ().
Table III. Organ motion error.
Clinical results
Though the median follow up time has been only nine months, six patients (30%) have died of esophageal cancer and two patients (10%) who are still alive have loco-regional and/or distant recurrences of esophageal cancer. To date, there has been no non-hematological toxicity of grade 3 and acute or sub-acute esophagitis or pneumonitis.
Discussion
Brief summary of main points
In this study patient setup error and inter-fraction motion of the esophagus were examined during RT in 20 patients. To our knowledge, this is the first report of the study of inter-fraction esophageal motion during day-to-day RT in patients with esophageal cancer. In fact, corrections for the setup errors have already been made in our method using CBCT and thus the setup errors are pertinent for our patients. The interesting aspect of our data is the remaining internal organ motion of the esophagus. In this study, the inter-fraction error was defined as the difference between day-to-day esophageal positions after eliminating daily setup error. This inter-fraction error included tumor motion due to the patient’s random movement, cardiac motion, peristaltic motion and respiratory motion (i.e. intra-fraction motion).
Main findings in relation to other studies
The kV CBCT was used for determining setup error in this study. The different interaction mechanisms of kV photons with tissues and image transducers offer improved imaging compared with megavoltage (MV) photons. This capability enhances the localization of target volumes and adjacent organs at risk during treatment compared with MV electronic portal imaging. The scatter component should not have as much an impact with MV CBCT compared with kV CBCT. The use of MV photos for imaging is a departure from the general preference for kV beams in imaging. The visibility of large low-contrast objects in tomographic images depends on the contrast-to-noise ratio. Contrast is determined by the differential attenuation of the beam through different bodily tissues. Most importantly, the image sequence from rotation fluoroscopy can be used in filtered back-projection to reconstruct an x-ray volumetric image. Recently, Xu et al. [Citation10] utilized CBCT measurements before and after treatment in the same day in order to detect intra-fraction tumor position errors (including 19 head and neck, 25 thoracic and 10 abdominal-pelvic tumors). Guckenberger et al. [Citation11] used CBCT scanning for the evaluation of setup errors and demonstrated the feasibility of its use in day-to-day clinical practice.
Esophageal movement was not addressed in an earlier review on inter-fraction and intra-fraction organ motion during RT [Citation2]. In our study, the daily esophageal motion were 5 +/− 3 mm (max, 15 mm) in the left-right direction and 5 +/− 3 mm (max, 15 mm) in the anterio-posterior direction. These values were almost similar to those of the following previous reports. Measurements of lower esophageal sphincter pressure during quiet respiration revealed lateral esophageal motion of 6 +/− 2 mm in the abdominal portion and 4 +/− 1 mm in the thoracic region [Citation12]. Cine-fluoroscopic barium swallow images of the esophagus in 51 patients undergoing catheter ablation for atrial fibrillation indicated that lateral shifts of more than 20 mm occurred in a majority of patients [Citation13]. Daily online CT images in a study of six IGRT-treated patients were reported to show maximal motion in the distal esophagus, and indicated that margins of 2 ∼ 5 mm could account for all motion [Citation14]. A study of esophageal positions at the extreme phases of respiration in six patients suggested that a margin of 5 ∼ 6 mm was sufficient to account for variations in organ position [Citation15]. Hashimoto et al. [Citation1] analyzed the motion during quiet respiration in 13 patients with implanted fiducial markers inserted into the esophageal wall and it was 4 +/– 2 mm, 8 +/– 4 mm, and 4 +/– 3 mm for the medio-lateral, cranio-caudal, and antero-posterior directions, respectively. According to Dieleman et al. [Citation4], margins that would have incorporated all esophageal movement in the medio-lateral and dorsoventral (anterior-posterior) directions were 5 mm proximally, 7 mm and 6 mm in the mid-esophagus, and 9 mm and 8 mm in the distal esophagus, as determined by 4D-CT. According to Guerrero et al. [Citation16], the displacement of the esophageal tumors, which estimated from breath-hold CT imaging using the 3-D optical flow method, was non-uniform and up to 14 mm.
Limitations of this study
The possible sources of methodological errors in assessing inter-fraction esophageal motion in this study could involve (a) inaccurate contouring of the outer esophageal wall on CBCT and/or planning CT images (i.e. human error), (b) mistakes in fusing CBCT images after correcting setup errors on the planning CT image on the Pinnacle3 workstation because the form or relative position of the chest wall and/or vertebral bone might be different, (c) correcting the setup error only by parallel translation, and not considering the lag of rotation and the longitudinal displacement could not be evaluated with our method, and, therefore, the error in the longitudinal direction was also detected as the error in the left-right or anterior-posterior directions, (d) the difference in the speed at which free breathing scans were acquired with the conventional CT and the CBCT, and (e) the CBCT is a slow scan over approximately 2 minutes and it therefore blurs the intra-fraction motion which is predominantly respiratory motion with a period of about 4 seconds. The probability of the first error (a) was minimized by having only a single experienced radiation oncologist (i.e. not multiple clinicians) contouring the outer esophageal wall and by expanding the image significantly. The other potential errors (b and c) were not formally evaluated in this study; however, images displayed on the Pinacle3 workstation were checked to make sure they were not significantly out of position after they were fused (). The slow scan blurs the esophageal outline and makes accurate delineation more difficult (e). So in this study, only the intra-fraction esophageal motion during treatment could not be extracted.
In this study, the margin recipes of Stroom [Citation7] and van Herk [Citation8] were used in order to evaluate errors of setup and daily esophageal motion. In addition, Redpath & Muren [Citation9] proposed a new optimization algorithm for the determination of treatment margins around moving and deformable targets like bladder or esophagus in radiotherapy. The algorithm is completely empirical and is based on an iterative method of determining margins around the planning clinical target volume (CTV) to provide the optimum coverage of the envelope of CTV positions observed during treatment. The major advantage with this approach is that it can be used on non-solid organs, circumventing any assumptions on the nature of the geometrical uncertainties. In this study, this empirical approach was not used. Therefore, our chosen method may be the limitation to detect the structure of the esophageal wall and this may not be the ideal approach. We are currently planning to introduce this empirical algorithm for determining margin of CTV.
Impact of the findings for future work
In our study, the motion was the same in the upper or the lower esophagus but this is contrary to the findings of other authors such as Dieleman et al. [Citation4]. The reason may be that the whole thoracic esophagus was analyzed which was difficult to identify the esophageal tumor on the CBCT. It may be necessary to determine whether the movement of the tumor bearing part of the esophagus was the same as the parts without gross tumor involvement. This is a problem for future study.
The present study is the first study to evaluate inter-fraction esophageal motion with patients in the supine position on the linear accelerator bed during RT and under free respiration. It cannot be concluded from this study who requires CBCT or whether every patient needs CBCT imaging. The change in mean esophageal position arising from twice-weekly imaging of individual patients was very small. This finding could be interpreted to mean that target volume coverage was fully adequate and that therefore costly daily imaging is not required.
In the present study, the patient setup error was not small, and therefore using twice-weekly CBCT might not be enough to reach the levels of target margin confidence. In the era of modern IGRT systems, the daily registration performed using CBCT was assumed to be necessary in order to minimize the setup error. The use of IGRT with CBCT will most likely benefit treatments such as IMRT for head and neck cancer, prostate cancer [Citation17,Citation18], or breast cancer; stereotactic RT for lung cancer or brain tumor; and patients with tumors commonly associated with organ motion, such as gastric cancer or urinary bladder cancers.
Conclusions
Both the patient setup error and day-to-day esophageal movements were detected in every patient in this study. The highest amounts of motion were distributed across various sites in the esophagus. However, the amount of motion did not appear to be clinically significant provided an appropriate internal target volume was considered. Our data support the use of target margins of 9 mm for day-to-day esophageal motion and 8 mm for patient setup error of motions in all directions. Also, when using daily kV CBCT during RT in order to minimize the setup error, only day-to-day motion of esophagus should be considered since it was found to be so small that the radiation field for esophageal cancer can be reduced.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Hashimoto T, Shirato H, Kato M, Yamazaki K, Kurauchi N, Morikawa T, . Real-time monitoring of a digestive tract marker to reduce adverse effects of moving organs at risk (OAR) in radiotherapy for thoracic and abdominal tumors. Int J Radiat Oncol Biol Phys 2005;61:1559–64.
- Langen KM, Jones DT. Organ motion and its management. Int J Radiat Oncol Biol Phys 2001;50:265–78.
- Kahn D, Zhou S, Ahn SJ, Hollis D, Yu X, D’Amico TA, . “Anatomically-correct” dosimetric parameters may be better predictors for esophageal toxicity than are traditional CT-based metrics. Int J Radiat Oncol Biol Phys 2005;62:645–51.
- Dieleman EM, Senan S, Vincent A, Lagerwaard FJ, Slotman BJ, van Sörnsen de Koste JR. Four-dimensional computed tomographic analysis of esophageal mobility during normal respiration. Int J Radiat Oncol Biol Phys 2007;67:775–80.
- Amer A, Marchant T, Sykes J, Czajka J, Moore C. Imaging doses from the Elekta Synergy X-ray cone beam CT system. Br J Radiol 2007;80:476–82.
- AJCC (American Joint Committee on Cancer) Cancer Staging Manual, 6th, Greene, FL, Page, DL, Fleming, ID, . New York: Springer-Verlag; 2002. 223–40.
- Stroom JC, Heijmen BJ. Geometrical uncertainties, radiotherapy planning margins, and the ICRU-62 report. Radiother Oncol 2002;64:75–83.
- van Herk M, Remeijer P, Rasch C, Lebesque JV. The probability of correct target dosage: Dose-population histograms for deriving treatment margins in radiotherapy. Int J Radiat Oncol Biol Phys 2000;47:1121–35.
- Redpath AT, Muren LP. An optimisation algorithm for determination of treatment margins around moving and deformable targets. Radiother Oncol 2005;77:194–201.
- Xu F, Wang J, Bai S, Li Y, Shen Y, Zhong R, . Detection of intrafractional tumour position error in radiotherapy utilizing cone beam computed tomography. Radiother Oncol 2008;89:311–9.
- Guckenberger M, Meyer J, Vordermark D, Baier K, Wilbert J, Flentje M. Magnitude and clinical relevance of translational and rotational patient setup errors: A cone-beam CT study. Int J Radiat Oncol Biol Phys 2006;65:934–42.
- Welch RW, Gray JE. Influence of respiration on recordings of lower esophageal sphincter pressure in humans. Gastroenterology 1982;83:590–4.
- Good E, Oral H, Lemola K, Han J, Tamirisa K, Igic P, . Movement of the esophagus during left atrial catheter ablation for atrial fibrillation. J Am Coll Cardiol 2005;46: 2107–10.
- Sasidharan S, Allison R, Jenkins T, Wolfe M, Mota H, Sibata C. Interfraction esophagus motion study in image guided radiation therapy (IGRT). No. 152. Proceedings of the 47th Annual ASTRO Meeting. Int J Radiat Oncol Biol Phys 2005;63(Suppl):S91–S92.
- Giraud P, Yorke E, Ford EC, Wagman R, Mageras GS, Amols H, . Reduction of organ motion in lung tumors with respiratory gating. Lung Cancer 2006;51:41–51.
- Guerrero T, Zhang G, Huang TC, Lin KP. Intrathoracic tumour motion estimation from CT imaging using the 3D optical flow method. Phys Med Biol 2004;49:4147–61.
- Pinkawa M, Pursch-Lee M, Asadpour B, Gagel B, Piroth MD, Klotz J, . Image-guided radiotherapy for prostate cancer. Implementation of ultrasound-based prostate localization for the analysis of inter- and intrafraction organ motion. Strahlenther Onkol 2008;184:679–85.
- Guckenberger M, Flentje M. Intensity-modulated radiotherapy (IMRT) of localized prostate cancer: A review and future perspectives. Strahlenther Onkol 2007;183:57–62.
