To the Editor
We report on a case of neutropenic enterocolitis during first-line chemotherapy with carboplatin and etoposide in a young patient with small cell lung cancer (SCLC).
Case presentation
The patient was a 46-year-old woman with SCLC, extensive disease, without previous medical history and in good health at time of diagnosis (performance status according to ECOG = 1). First line chemotherapy with carboplatin, AUC 5, and etoposide 120 mg/m2 day 1–3 was initiated. Six cycles were planned. Chemotherapy was given every three weeks. The first cycle was tolerated well.
Ten days after the second cycle, the patient was admitted to the hospital presenting with fever, abdominal pain, vomiting and diarrhea since one week (CTC grade 4). Physical examination revealed diffuse abdominal pain. Bowel sounds were scanty but present. Laboratory data revealed severe hemotological toxicity with CTC grade 4 leukopenia (0.6 mia/L), neutropenia (0.03 mia/L) and thrombocytopenia (15 mia/L). Hemoglobin was not suppressed. C-reactive protein (CRP) was 325 mg/L. Sodium was 120 mM, other electrolytes, liver function tests and creatinine were within normal range.
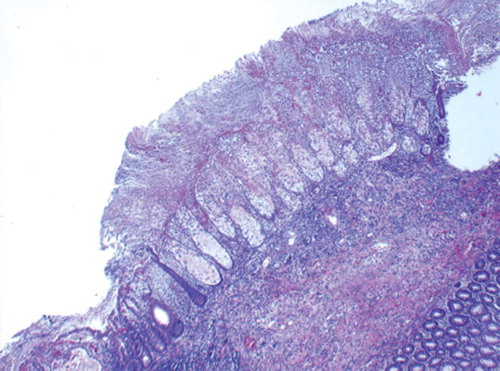
A plain abdominal radiograph showed suspicion of colonic wall thickening particularly on the left side. Initial medical management consisted of bowel rest, fluid resuscitation and intravenous antibiotics. The patient rapidly deteriorated and was admitted to the intensive care unit with severe hypotension and tachycardia. A contrasted abdominal CT scan demonstrated massive bowel wall thickening and edema, and ascites ( and ). The clinical picture worsened successively and on the third day laparotomy was carried out on vital indication. The patient underwent total colectomy and ileostomy. Histopathological analysis concluded ischemic necrosis of bowel wall and pseudomembranous inflammation (). Blood cultures were positive for Escherichia coli and Klebsiella pneumoniae. Stool cultures were negative.
Figure 1. Abdominal CT scan with intravenous contrast shows extensive bowel wall thickening (pancolitis) with surrounding fatty stranding and ascites. Normal findings in rectum.
Figure 2. Maximum Intensity Projection of Abdominal CT scan with intravenous contrast shows no central vascular compromise of superior and inferior mesenteric arteries, ruling out the differential diagnosis of ischemic large vessel disease.
Figure 3. High-powered micrograph of hematoxylin and eosin stained colonic mucosa showing focal lesion of necrosis and eruptive mass of mucus, and cellular debris. Neutrophils are attached to the surface. There are varying degrees of ischemic necrosis. Acute and chronic inflammation as well as edema is seen in lamina propria and submucosa.
Seventeen days postoperatively the patient was transferred from the intensive care unit back to the clinical ward and slowly recovered. A new CT scan showed pulmonary progression, and the patient was given a third cycle of chemotherapy in reduced dose. Thirteen days after the third cycle, the patient was readmitted. She developed progressive neck swelling and died in the clinical picture of fulminant vena cava superior syndrome. No autopsy was performed.
Discussion
Neutropenic enterocolitis (NE) is caused by a combination of neutropenia and mucosal injury. Neutropenia allows gastrointestinal microorganisms to invade the bowel wall and proceed unimpeded. Mucosal injury is most often caused by the cytotoxic effect associated with chemotherapy, but in fact severe neutropenia alone may cause mucosal ulceration [Citation1]. The condition has been described in the treatment of hemotological disease, solid tumors and in non-oncologic diseases associated with neutropenia [Citation1,Citation2]. Several chemotherapeutic agents have been reported in conjunction with NE [Citation3–5].
NE typically presents with fever, abdominal pain and neutropenia [Citation1]. To establish the diagnosis either CT or ultrasound is recommended [Citation1–3]. Histopathological analysis is provided only postoperatively or post-mortem and is not suggested as part of the diagnostic criteria [Citation1,Citation2]. The histopathological picture is heterogeneous [Citation1,Citation2].
NE is a serious complication in the neutropenic patient. It is therefore of high importance to keep this diagnose in mind.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Ullery BW, Pieracci FM, Rodney JRM, Barie PS. Neutropenic enterocolitis. Surg Infect 2009;10:307–14.
- Gorschlüter M, Mey U, Strehl J, Ziske C, Schepke M, Schmidt-Wolf IGH, . Neutropenic enterocolitis in adults: Systematic analysis of evidence quality. Eur J Haematol 2005;75:1–13.
- Cloutier RL. Neutropenic enterocolitis. Emerg Med Clin North Am 2009;27:415–22.
- Shvartsbeyn M, Edelman MJ. Pemetrexed-induced typhlitis in non-small cell lung cancer. J Thorac Oncol 2008;3: 1188–90.
- Furonaka M, Miyazaki M, Nakajima M, Hirata S, Fujitaka K, Kondo K, . Neutropenic enterocolitis in lung cancer: A report of two cases and a review of the literature. Intern Med 2005;44:467–70.
