To the Editor,
Pediatric nasopharyngeal carcinoma (NPC) is one of the most frequent epithelial tumors in children [Citation1]. Combination treatment of photon radiotherapy and chemotherapy is effective for pediatric nasopharyngeal cancer and overall survival has increased to 70–80% with advances of chemotherapy regimens and radiotherapy techniques. However, photon radiotherapy for pediatric NPC often causes facial deformity, pituitary dysfunction, and xerostomia, especially in younger children. Here, we report two cases of pediatric NPC treated with proton therapy as an alternative to photon radiotherapy.
Patient presentation
Case 1
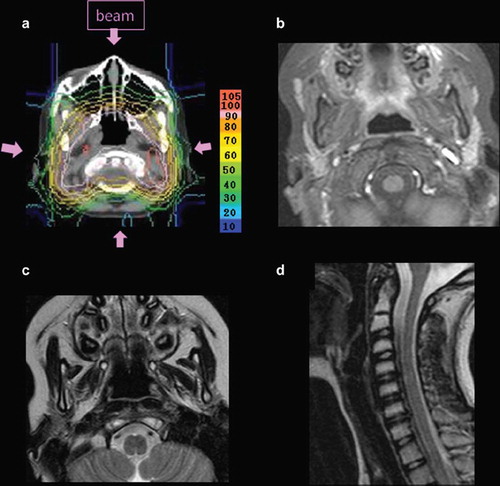
A 6-year-old girl with NPC of stage T2bN1M0 [Citation2] was referred to our institution in December 2005. The primary tumor was mainly at the right lateral wall with involvement of ipsilateral upper deep cervical lymph nodes. Pathological findings indicated undifferentiated carcinoma positive for latent membrane protein-1. The patient underwent chemotherapy with cisplatin (CDDP), methotrexate with leucovorin rescue, and 5-fluorouracil (5FU). After completion of four courses of chemotherapy, the tumor showed a partial response. Proton therapy was later administered. Treatment beams were delivered through anterior, posterior and lateral ports (). The photon equivalent dose (Gray equivalent dose; GyE) was defined as the physical dose × the relative biological effectiveness of the proton beam assigned a value of 1.1. A total dose of 59.4 GyE was applied to the tumor in 30 fractions over six weeks. The initial target included nasopharynx, base of the skull, posterior portion of the maxillary sinus and nasal cavity, and whole neck lymph nodes including the supraclavicular fossa. This treatment was successful and most of the tumor had disappeared after 22 fractions (43.56 GyE). Thereafter, the tumor and involved lymph nodes with coned-down fields up to a total dose of 59.4 GyE. The doses were felt off in the parotid glands: Over 30 Gy or more was irradiated to less than 40% volume of the left parotid gland, but more than 70% of the right.
Figure 1. The dose distribution and the MRIs after proton therapy: Proton beams were delivered via 3 ports (a) and the bilateral parotid glands (b), mandibular ramus (c), and cervical spine (d) in the treatment field showed retardation.
A grade 1 reaction of the pharyngeal mucosa and a skin reaction were observed at the end of proton therapy [Citation3], but not two months later. Slight neck edema was seen at two months after proton therapy, but not after seven months. Xerostomia and reduced taste sensation did not occur during treatment.
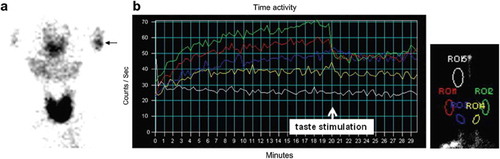
Four and a half years after proton therapy, the tumor was still undetectable. The MRI showed retardation of the bilateral parotid glands (), however, the patient has not experienced xerostomia and a salivary gland scintigram showed salivary secretion from both parotid glands, while right parotid function was depressed compared to the left side (). The mandibular ramus and cervical spine in the treatment field also showed retardation (). However, facial deformity and short neck were not noticeable.
Figure 2. A salivary scintigram of 4.5 years after proton therapy. (a): The accumulation in the left parotid gland was almost normal (arrow), but reduced in the right. Salivary secretion in the oral cavity was also shown. (b): The graph shows time-dependent change of salivary flow of each salivary gland; ROI 1–5 shows right and left parotid gland, right and left submandibular gland, and control, respectively. After 20 minutes from start of the study, patient licked tartaric acid for taste stimulation. Salivary flow was observed in both parotid glands after taste stimulation, while right salivary function was depressed. Both submandibular glands showed hypoaccumulation and loss of response to taste stimulation.
Case 2
A 13-year-old girl with NPC of stage T3N2M0 [Citation2] was referred to our hospital in December 2003. The primary tumor was extended to the right sphenoid sinus and parapharyngeal space with right upper deep cervical lymph nodes involvement. A biopsy of the nasopharynx showed poorly differentiated squamous cell carcinoma. Chemotherapy with CDDP and 5FU was started, and the tumor showed a partial response after three courses of chemotherapy. Thereafter the patient received proton therapy with concurrent CDDP and 5FU. Proton beams were delivered through anteroposterior and right ports (). A total dose of 71.28 GyE was given in 36 fractions. The initial target included the nasopharynx, base of the skull, posterior portion of the maxillary sinus and the nasal cavity, and the upper and lower cervical lymph nodes. After 61.38 GyE, the primary tumor and involved lymph nodes were treated with coned-down fields up to a total dose of 71.28 GyE.
Figure 3. Proton beams were delivered via 3 ports (a). The right parotid gland (b) and the right lower back teeth (Δ:c) in the treatment field showed atrophy on the MRI and the dental panoramic radiography.
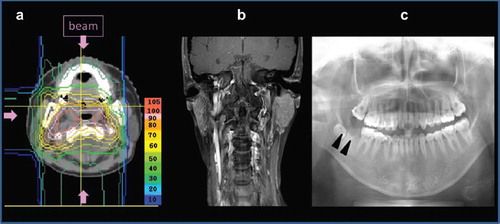
A grade 3 reaction of the pharyngeal mucosa and a grade 1 skin reaction were recorded during treatment [Citation3]. Proton therapy was suspended for ten days due to the mucositis, but these reactions were subsided three months later. Xerostomia and reduced taste sensation did not occur during treatment. The tumor showed a complete response on MRI at two months after completion of proton therapy.
Six years after proton therapy, no tumor was found. On imaging, the right parotid gland was smaller than the left gland, and the right lower back teeth showed atrophy (). However, the only clinical problem was grade 1 trismus. Facial deformation, xerostomia, skin pigmentation and short stature were not apparent.
Discussion
Pediatric patients with NPC are generally treated with chemotherapy and external beam photon radiotherapy with two lateral opposing fields and a single anterior field covering the entire nasopharynx, base of the skull, posterior portion of the orbit, paranasal sinus, nasal cavity, whole neck, and supraclavicular fossa. However, irradiation of these areas leads to a number of toxicities, including neuroendocrine sequelae, xerostomia, decreased taste, and facial bone retardation [Citation4–10]. Jaffe et al. found maxillofacial abnormalities in 82% of survivors of childhood cancer who received craniofacial radiation treatment, with an increase in severity with treatment at an earlier age and at higher radiation doses [Citation7]. Salivary function of the parotid gland is lost at a dose >26 Gy in an adult patient [Citation11]. Intensity modulated radiotherapy (IMRT) is a new technique that causes less xerostomia than previous radiotherapy. However, salivary flow only recovers to 25% of the preradiotherapy flow [Citation12].
In our cases, proton beams were used as an alternative to photon radiotherapy. Proton beams have a Bragg peak in which the dose rapidly falls off at the end of the beam range at a depth within the patient. This allows for excellent dose localization. And, when multi-portal proton beams are used, low dose area is smaller compared to photon radiotherapy including IMRT, which may produce regeneration as in the case above. Thus, we consider toxicity could be minimized in our cases using proton therapy. However, the reason of residual function of the retarded salivary gland in Case 1 was unclear. Recovery of the organ function in childhood may be a future problem.
For growing patients, quality of life is very important in later life. More patients and longer follow-up periods are needed to assess the long-term efficacy and complications of proton therapy, but we believe that this therapy can be used as a better alternative to photon radiotherapy to minimize toxicity and improve quality of life for patients with pediatric NPC.
Acknowledgments
We thank Dr. Noboru Oriuchi, department of diagnostic radiology and nuclear medicine of Gunma-University, for interpretation of scintigram of the manuscript. None of the authors have a conflict of interest regarding the work in the article.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Ayan I, Kaytan E, Ayan N. Childhood nasopharyngeal carcinoma: From biology to treatment. Lancet Oncol 2003; 4: 13–21.
- Sobin LH, Wittekind C. International Union Against Cancer, TNM classification of malignant tumors. Wiley-Liss, Oxford, UK; 2002.
- Trotti A, Colevas AD, Setser A, Rusch V, Jaques D, Budach V, . CTCAE v3.0: Development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol 2003;13:176–81.
- Denys D, Kaste SC, Kun LE, Chaudhary MA, Bowman LC, Robbins KT. The effects of radiation on craniofacial skeletal growth: A quantitative study. Int J Pediatr Otorhinolaryngol 1998;45:7–13.
- Fromm M, Littman P, Raney RB, Nelson L, Handler S, Diamond G, . Late effects after treatment of twenty children with soft tissue sarcomas of the head and neck. Experience at a single institution with a review of the literature. Cancer 1986;57:2070–6.
- Gevorgyan A, La Scala GC, Neligan PC, Pang CY, Forrest CR. Radiation-induced craniofacial bone growth disturbances. J Craniofac Surg 2007;18:1001–7.
- Jaffe N, Toth BB, Hoar RE, Ried HL, Sullivan MP, McNeese MD. Dental and maxillofacial abnormalities in long-term survivors of childhood cancer: Effects of treatment with chemotherapy and radiation to the head and neck. Pediatrics 1984;73:816–23.
- Larson DL, Kroll S, Jaffe N, Serure A, Goepfert H. Long-term effects of radiotherapy in childhood and adolescence. Am J Surg 1990;160:348–51.
- Rappaport R, Brauner R. Growth and endocrine disorders secondary to cranial irradiation. Pediatr Res 1989;25: 561–7.
- Imhof SM, Mourits MP, Hofman P, Zonneveld FW, Schipper J, Moll AC, . Quantification of orbital and mid-facial growth retardation after megavoltage external beam irradiation in children with retinoblastoma. Ophthalmology 1996;103:263–8.
- D'Angio GJ. Silhouette. Frank Ellis, M.S., M.D., FRCP, FRCR. Med Pediatr Oncol 1998;31:29–30.
- Pow EH, Kwong DL, McMillan AS, Wong MC, Sham JS, Leung LH, . Xerostomia and quality of life after intensity-modulated radiotherapy vs. conventional radiotherapy for early-stage nasopharyngeal carcinoma: Initial report on a randomized controlled clinical trial. Int J Radiat Oncol Biol Phys 2006;66:981–91.
